Abstract
Early intervention is assumed to improve outcome in first-episode psychosis, but this has not been proven. Objective: To study whether 1-year outcome will be better in a health care sector with early detection (ED) of psychosis compared with sectors with no early detection (no-ED). Design: a quasi-experimental study with ED in 2 experimental sectors and no-ED in 2 control sectors. ED was achieved through low-threshold ED teams and information campaigns about psychosis for the public, schools, and primary health care providers. The ED and no-ED health care areas offered an equivalent assessment and treatment program during the first year. Two hundred and eighty-one patients were included; 88% were reassessed after 1 year. Results: The ED-area patients (N = 141) had a median duration of untreated psychosis of 5 weeks at baseline compared with 16 weeks for patients in the no-ED area (N = 140). Positive and general symptoms, global assessment of functioning, quality of life, time to remission, and course of psychosis at 1 year after the start of treatment were not different between ED and no-ED groups. Outcome was significantly better for the ED area for negative symptoms. Conclusions: The ED, no-ED differences at baseline become attenuated by 1 year but not the difference in negative symptoms, suggesting secondary prevention in this domain of psychopathology. However, this possibility requires further testing by follow-up and replication.
Keywords: psychosis, schizophrenia, early detection, outcome
Early intervention in first-episode psychosis has gained increasing attention during the last decade.1 Duration of untreated psychosis (DUP) in most studies is reported to be long with a mean of around 1–2 years and a median of about 6 months,2 and it is suggested that DUP is a prognostic factor that can be influenced by changes in the organization of the mental health services. A number of studies find a significant association between long DUP and poorer outcome, but some do not replicate this finding.3–6 In a recent meta-analysis on the relationship between DUP and outcome in prospective cohorts with first-episode schizophrenia spectrum psychosis, 26 studies were identified,7 and the conclusion was that “convincing evidence for a modest association between DUP and outcome was found.”
All these studies, however, remain correlational in nature. We do not know whether this association is causal or whether long DUP is a marker of other known or unknown factors that contribute to a poorer outcome.2,8,9 To separate the effects of the DUP from confounding factors, we will need to modify the DUP in one patient group but not in another. An experimental delay of treatment for a random subgroup of first-episode patients is the best design but would be clearly unethical. The next best way to demonstrate causality between reduced DUP and better outcome would be to introduce early detection (ED) programs into clinical services in a quasi-experimental design with reduction of DUP in one of the sites. Here patients from one health care sector serving an entire population should receive an experimental approach, in this case the sector-wide ED program, and then be compared with patients from another health care sector who do not receive the experimental approach.10
This has been the strategy of the TIPS (early Treatment and Intervention in Psychosis) study. We developed early intervention strategies in the health care sectors of Rogaland County, Norway (ED area). The ED program consisted of intensive information campaigns in local media together with seminars for teachers, pupils, and health professionals working in the primary health services and low-threshold ED teams that carried out assessment on all possible first-episode psychosis cases.11 Consecutive first-episode patients from the ED area over 4 years were compared with consecutive first-episode patients from 2 comparable health care sectors with parallel treatment and assessment programs but without the ED program (no-ED area). At baseline we found that ED patients had significantly shorter DUP (median 5 vs 16 weeks) than patients from the no-ED area.12 ED patients also had less severe positive, negative, and general symptoms at start of treatment, and with the exception of positive symptoms this difference was still present after 3 months. To our knowledge, this study is the first to demonstrate a reduction of DUP in a representative sample of patients with first-episode psychosis.
The key question of this study is whether intervening earlier in the course of psychosis achieves secondary prevention, ie, not only reduces symptoms but also improves prognosis (long-term course and outcome). This would be demonstrated if the ED group's advantages seen at baseline are seen at 1 year, suggesting that typical schizophrenic deterioration over time has not occurred. Based on previously observed associations between DUP and different aspects of outcome, we hypothesize that if there is a causal relationship between earlier treatment and better outcome, then the ED group will have a better outcome in regard to level of symptoms (positive, negative, and general), time to remission, quality of life (QoL), and social functioning. The null hypothesis is that the ED, no-ED difference will attenuate over time.
METHOD
The study was carried out on the basis of the specialist psychiatric services in 4 Scandinavian health care sectors (2 health care sectors in Rogaland County, Norway, with a total of 370 000 inhabitants and the Ullevaal health care sector, Oslo County, Norway, and the midsector, Roskilde County, Denmark, with a combined total of 295 000 inhabitants). Rogaland County comprised the ED sector and the combined Ullevaal and Roskilde sites comprised the no-ED sector. Both sectors had urban and suburban elements with 84% of the ED population living in urban areas vs 96% of the no-ED population (P = .001, the Fisher exact test). There were no differences in age and sex distribution between the 2 areas and no differences in main income levels and unemployment rates in the total population. Patients from the no-ED area were more often immigrants from a nonwestern country (12% vs 4%) and had more education after high school (31% vs 21%) (P = .001 for both, the Fisher exact test).
All 4 health care sectors are part of a national health care system. In Norway and Denmark, these are essentially the only systems available for the treatment of psychotic disorders, and the samples collected represent most, if not all, cases of psychosis ascertained and treated. As such, these are clinical epidemiologic samples.
In all 4 health care sectors, the treatment systems were catchment area based and publicly funded. The core basis of the psychiatric specialist treatment system was the subsector catchment area-based outpatient units, with the addition of short-term, acute-care inpatient units and a restricted number of specialized long-term wards (4 different outpatient units and 2 hospitals in the ED area and 5 outpatient units and 2 hospitals in the no-ED area). The treatment system was based on referral from general practitioners, but the assessment and treatment of first-episode psychosis was considered a task for the specialized psychiatric treatment system, with immediate transfer of recognized cases as standard practice. There were no differences in the use of inpatient psychiatric services across the areas.
From January 1, 1997, the specialized psychiatric services of the 4 health care sectors established equivalent treatment programs for patients with first-episode psychosis. All first-episode patients from all 4 sectors underwent assessment by trained personnel as soon as possible after first contact with the specialized treatment system and were assigned to the treatment program without delay. The program consisted of defined treatment algorithms for antipsychotic medication (low-dose second-generation antipsychotic medication), individual psychosocial treatment (a trained psychiatric case worker offering weekly sessions), and psychoeducational family work (multifamily groups). The program was based on experiences from other first-episode treatment programs and the recommendations of the Schizophrenia Patients Outcomes Research Team.13
In 2 of the health care sectors (Rogaland County), an extensive ED program was added that was not present in the 2 other participating health care sectors (Oslo and Roskilde counties). The ED program consisted of educational campaigns about psychotic symptoms and their treatment directed at the general population through newspaper, radio, and cinema advertisements and targeted information campaigns directed at general practitioners, social workers, and high school health care personnel. In addition, specialized low-threshold ED teams were established that could be reached by a single telephone call from potential patients, family, and friends, and the telephone number was made part of the information campaign. The organization of the ED program was based on the idea that treatment could be delayed owing to lack of awareness or to prejudices about psychotic disorders and their treatments in the psychotic person, in the person's network, and/or among first-line health care and social welfare personnel. Treatment could secondarily be delayed owing to difficulties in accessing psychiatric services. A tertiary delaying factor could be delays in identifying cases and/or resource limitations in assigning adequate treatment for first-episode patients at the level of the specialized psychiatric services. The ED program addressed the first 2 factors, with the intention of bringing first-episode patients earlier into the specialized psychiatric services assessment and treatment programs. Establishing equivalent treatment programs in the ED and no-ED areas would necessarily reduce delays on the level of the specialized services equally and thus carried the possibility of shortening the DUP in the no-ED area.
The study included all eligible patients meeting study criteria for the period of January 1, 1997, through December 31, 2000. Participants were followed up with personal interviews after 3 months and 1, 2, and 5 years. This communication reports the 1-year results.
The Regional Committee for Research Ethics approved the study. All patients entering the study gave written informed consent. Information regarding nonparticipants is based on data gathered anonymously for the purpose of bias testing.
Subjects
Inclusion criteria consisted of living in the catchment area of 1 of the 4 health care areas; age 18–65 years; meeting the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for schizophrenia, schizophreniform disorder, schizoaffective disorder (narrow schizophrenia spectrum disorders) or brief psychotic episode, delusional disorder, affective psychosis with mood-incongruent delusions, or psychotic disorder not otherwise specified; being actively psychotic, as measured by the Positive and Negative Syndrome Scale (PANSS)14 score of 4 or more on at least 1 of positive subscale items for delusions, hallucinatory behavior, grandiosity, or suspiciousness/persecution or general subscale item unusual thought content; not receiving previous adequate treatment for psychosis (defined as antipsychotic medication of 3.5 haloperidol equivalents for 12 weeks or until remission of the psychotic symptoms); having no neurological or endocrine disorders with relationship to the psychosis; having no contraindications to antipsychotic medication; understanding and/or speaking a Scandinavian language; having an IQ score of above 70; and being willing and able to give informed consent.
During the 4-year period, 380 patients were identified, and 284 gave informed consent to enter the study. The refuser rate for study inclusion was 23%, and no major differences for key characteristics were found when compared with the included sample. For details see previous publications.12 Three patients withdrew consent during the first year, leaving 281. These 281 patients were distributed with 141 in the ED area and 140 in the no-ED area. From the initial sample of 281 patients, we were able to reassess diagnosis in 272 cases (97%) and to carry out complete assessments of 239 (85%) at 1-year follow-up. The patients lost to follow-up did not differ from the original sample on any major characteristics such as gender, age, diagnosis, premorbid functioning, or symptom level at baseline.
Measures
The assessment team at all sites consisted of clinically experienced and trained research personnel who performed all evaluations.9 The Structured Clinical Interview for the DSM-IV Axis I Disorders (SCID) was used for diagnostic purposes.15 If patients abused drugs, we would initiate a longer period (> 4 weeks) of drug-free observation (mostly involuntarily) before a diagnostic conclusion was made. Symptom levels were measured by means of the PANSS.14 Global functioning was measured by the Global Assessment of Functioning Scale (GAF),16 and the scores were split into symptom (GAFs) and function (GAFf) scores to improve psychometric properties. QoL was measured with the Lehman Quality of Life Interview, brief version.17 Misuse of alcohol and other drugs was measured by the Drake Scale.18 The DUP was measured as the time from the onset of psychosis until the start of adequate treatment; for details see previous publications.12
After 3 months, we repeated PANSS, GAF, and deficit assessment. At 1 year, all assessments were repeated including SCID. For the 1-year follow-up, a separate summary interview was conducted in which we gathered information regarding 3 different outcome domains: (1) psychosis development: time to remission, duration and number of relapses, and remission status at follow-up; (2) use of treatment offered in weeks of participation: hospitalizations, individual supportive psychotherapy (at least weekly sessions), family work, and use of antipsychotic medication; and (3) use of rehabilitation services. All major baseline assessments such as diagnosis, PANSS, GAF, drug abuse, and DUP underwent tests of intra- and intersite reliability with satisfactory results. The definition of remission at follow-up was equal to the definition of DUP at baseline; retrospective estimation of time period with or without positive symptoms defined as a rating of four or more on specific PANSS items. Raters trained to reliability for DUP made assessment of remission at follow-up. For details see previous publications.9 Regarding reliability for the follow-up, 31 vignettes were randomly selected from 1- and 2-year follow-ups and rated by 2 experienced psychiatrists on the following variables: diagnosis, GAFs, GAFf, and alcohol and drug scores. For all dimensions the reliability was clearly satisfactory. For diagnosis, kappa = 0.81; for the other dimensions, Intra Class Correlation (1.1) were GAFf: 0.86, GAFs: 0.91, alcohol: 0.75, and drugs: 0.86.
Statistical Procedures
Analyses were performed with the statistical package SPSS (version 12.0; SPSS Inc., Chicago, Ill). The applied methods are reported for all group comparisons. All tests were 2-tailed. We used nonparametric tests for data without normal distribution. As noted in several other studies, the DUP does not seem to have a normal distribution, whereas its natural logarithm does. In multiple linear regression analyses, DUP was transformed to its natural logarithm.
Multiple linear regression analyses with different aspects of 1-year outcome as dependent variables were performed to check the influence of possible confounders such as sampling effects. The selection of variables to be included in the regression model was based on a forward selection procedure, in addition to a set of variables based on assumed clinical importance through reviews of relevant studies and a set of variables comprising measures of differences between the areas. These last sets of variables were included in the model prior to the stepwise procedure. Candidate variables to the forward selection procedure were found by choosing those that showed at least a moderate association with the dependent variable (P value ≤ .25) in a regression analysis with only that variable as covariate in addition to coming from the ED sites. In the resulting multivariate analyses, “Coming from the ED sector” was included in the last step. The final model was examined for interaction effects and the effects of outliers and influential observations, including leverages. In order to study time to remission, we used Kaplan-Meier survival analysis, and the groups were compared using the log rank test.
Results
Treatment
In order to study the effect of ED on outcome, we aimed to provide similar treatment at all sites. In general we achieved this goal. Even though ED patients did receive significantly fewer weeks of psychotherapy and fewer weeks of medication during the first year, the differences were only 3–4 weeks and should probably not be regarded as clinically significant (table 1). No differences were found for weeks of hospitalization or participation in family work.
Table 1.
Treatment Provided During the First Year
| N | No-ED Area | ED Area | |
| Weeks of psychotherapy, mean (SD)* | 138/140 | 45.5 (12.0) | 42.0 (14.9) |
| Weeks of medication, mean (SD)* | 138/139 | 41.7 (14.9) | 37.3 (17.4) |
| Weeks of first hospitalization, mean (SD) | 138/140 | 11.8 (14.5) | 11.9 (14.8) |
| Weeks of total hospitalization, mean (SD) | 138/140 | 15.5 (15.9) | 16.4 (16.6) |
| Family work participation (%) | 38 | 40 |
P < .05, 2-tailed unpaired t test.
Clinical Status at 1 Year
Findings were similar for the course of psychotic symptoms during the first year (table 2). In the no-ED groups, 68% were in remission compared with 64% in the ED area. Remission was defined as having a score of PANSS positive symptoms below 4 that had lasted at least 1 week. Twenty-one percent were continuously psychotic in the no-ED groups compared with 26% in the ED area. The total duration of psychosis defined as the sum of DUP and time to remission was significantly shorter in the ED sectors.
Table 2.
Clinical Status at 1-Year Follow-up
| N | No-ED Area | ED Area | |
| Course during 1-year follow-up (% yes) | 133/139 | ||
| In remission (> 1 week) | 68 | 64 | |
| In relapse | 12 | 10 | |
| Continuously psychotic | 21 | 26 | |
| Total duration of psychosis (DUP + time to remission) (median weeks)* | 138/140 | 44 | 22 |
| PANSS | 124/124 | ||
| Positive symptoms | 11.8 (4.8) | 11.8 (5.7) | |
| Negative*** | 14.6 (6.4) | 12.3 (5.9) | |
| General | 26.2 (7.3) | 25.1 (10.1) | |
| Substance abuse | |||
| Drugs**** | 1.3 (0.8) | 1.7 (1.0) | |
| Alcohol | 1.9 (0.6) | 1.9 (0.5) | |
| Weeks of psychosis first year mean (SD) | 133/139 | 23.2 (18.9) | 23.0 (19.7) |
| GAF | 127/132 | ||
| Symptoms | 50.6 (14.0) | 52.0 (16.2) | |
| Function | 49.2 (14.0) | 51.5 (16.2) | |
| Strauss-Carpenter mean (SD) score | 124/127 | ||
| Work last year | 1.1 (1.5) | 1.3 (1.6) | |
| Friends last year | 2.7 (1.4) | 3.0 (1.4) | |
| Symptoms last month | 2.2 (1.2) | 2.2 (1.3) | |
| QoL subjective scale | 116/108 | ||
| Daily activities/social relations** | 4.2 (1.0) | 4.6 (1.1) | |
| Legal and safety issues | 5.7 (1.0) | 5.8 (1.2) | |
| Economy | 3.8 (1.6) | 3.8 (1.8) | |
| Family | 5.3 (1.4) | 5.2 (1.4) | |
| QoL objective scale | 116/108 | ||
| Social activity* | 3.2 (1.0) | 3.5 (1.0) | |
| Daily activity | 1.1 (0.3) | 1.1 (0.3) | |
| Economy | 0.8 (0.3) | 0.7 (0.3) | |
| Family | 3.9 (0.8) | 4.1 (0.8) |
Note: All values are mean and standard deviation when not otherwise specified.
P < .05,
P < .01,
P < .005,
P < .001.
We found no significant differences for PANSS scores on the positive and general scale, but patients from the ED area had less severe negative symptoms. The ED patients had more drug abuse but not more alcohol abuse, and GAF scores were quite similar. Regarding social functioning no significant differences were found. For QoL measures, the ED patients had better scores on daily activities/social relations both on the subjective and the objective scale. No differences were reported on other QoL measures such as economy, feeling of safety, or family relations.
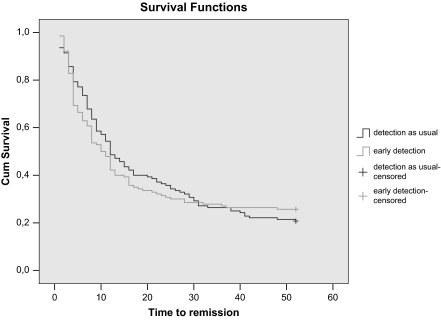
Regarding time to remission, a Kaplan-Meier analysis revealed no significant differences. Figure 1 illustrates the similar survival curves.
Fig. 1.
Kaplan-Meier analyses of time to remission.
For negative symptoms, we conducted a multiple linear regression analysis to test whether coming from the DUP-reducing ED sites predicted the negative symptom differences after adjusting for possible confounding variables. In this analysis, we did not include baseline scores for positive or negative symptoms because we were testing whether or not baseline differences remained at follow-up. For this we regarded gender, age, diagnosis, and DUP (log transformed) to be clinically important variables to be fixed in the regression model. Candidate variables to the forward selection procedure were years of education, all premorbid factors (childhood level and change), and drug/alcohol abuse. The results for the final multiple regression model are presented in table 3.
Table 3.
Multiple Linear Regression Analysis of the Effect of Possible Confounder Variables on the Level of Negative Symptoms at 1 Year
| Variables | Coefficients | Confidence Intervals | P Value |
| Constant | 19.2 | 14.0 to 24.3 | .0000 |
| Age in years | 0.02 | −0.06 to 0.1 | .5780 |
| Gender | −1.7 | −3.3 to −0.08 | .0390 |
| Diagnosis (schizophrenia spectrum yes or no) | 0.8 | −0.9 to 2.5 | .3560 |
| DUP (log transformed) | 0.09 | −0.3 to 0.5 | .6960 |
| Years of education | −0.6 | −1.0 to −0.3 | .0000 |
| Premorbid social functioning childhood | 1.5 | 0.8 to 2.3 | .0000 |
| Premorbid social functioning change scores | 0.9 | 0.3 to 1.5 | .0020 |
| ED reduction in DUP | −2.0 | −3.6 to −0 | .0150 |
Note: Model summary—R2 = .242, adjusted R2 = .214.
Gender, years of education, premorbid social functioning during childhood, premorbid social functioning change scores, and coming from the ED sites each had a significant relationship to level of negative symptoms. DUP (log transformed) did not contribute significantly to the model. The directions of the relationships were that being male, having fewer years of education, having a poorer childhood level of premorbid social functioning with changes in social functioning for the worse during development, and coming from the no-ED sites (ie, longer DUP) were associated with more negative symptoms.
For QoL daily activity scores as the dependent variable, similar analysis was carried out, and coming from the ED sites contributed significantly to better QoL scores. The explained variance was, however, so low (10%) that we assume that the level of negative symptoms are accounting for most of these differences.
Discussion
The first question regarding early intervention in psychosis is whether health care systems can be developed that is able to bring patients with first-episode psychosis into treatment earlier. Our project has been successful in that we have an ED sector with a median DUP of 5 weeks compared with 16 weeks in a health care sector without ED. Furthermore, the lower DUP is associated with psychoses that are less symptomatic and functionally disabling. The second question is whether early treatment confers secondary prevention meaning that the initial clinical/functional advantage of the earlier detected sample is maintained over time. Our findings support this idea but only to a limited degree, ie, we find that coming from the ED sectors is associated with less negative symptoms at 1-year follow-up. This association is retained also when effects of possible confounders are adjusted for through multivariate regression analysis. The effect size, however, is small, and further research will be required to confirm that the ED program produced a true secondary prevention.
We did not, however, find any association between coming from the ED sectors and fewer positive or general symptoms or higher remission rates over time. We found that a few aspects of QoL (daily activities) were significantly correlated with ED, the other measures were not. However, the effect of QoL (daily activities) was mainly accounted for by differences in negative symptoms at follow-up. We did not find the expected association between ED and shorter time to remission, earlier studies had indicated that this might be an effect of reduced DUP.19 The DUP in the control sites was, however, very low compared with international studies and may increase the risk of type II errors.
ED does not raise the incidence of schizophrenia in the sector. Rather, it seems to lower the threshold for identifying psychopathology and for starting treatment. That is, it starts treatment at an earlier stage of the psychotic disorder when it is milder and less disabling. If earlier treatment has no effect on the underlying pathophysiology of psychosis, then the ED sample should with time “catch up” with the no-ED sample in severity and deficit. We see this happen in our study between experimental and control samples for positive symptoms, general symptoms, and time to remission.
The “catch up” does not happen in the experimental sample with regard to negative symptoms. This may be important because negative symptoms form a core element of deficit psychopathology in schizophrenia that is both treatment resistant and associated with poor functional outcome. If early intervention provides secondary prevention here, the baseline and 1-year follow-up differences in negative symptoms between experimental and control sectors should endure and be apparent at subsequent follow-ups. We might also expect to see differences in phenomenologies associated with negative symptoms such as social functioning and instrumental capacity. We measured negative symptoms as subscore of the PANSS. A limitation of our study is that we did not attempt to disentangle primary from secondary negative symptoms.20
We conclude that ED of psychosis is both possible and important even though we found no obvious effect on positive symptoms during the first year of treatment. The fact that the suffering and danger associated with psychosis can be reduced through a shortening of the time ill has its own value and supports the development of systems of ED.21
Acknowledgments
This research was supported by the Norwegian National Research Council (# 133897/320 and #154642/320), the Norwegian Department of Health and Social Affairs, the National Council for Mental Health/Health and Rehabilitation (#1997/41 and #2002/306), Rogaland County, and Oslo County (Drs Vaglum, Johannessen, Friis, Larsen, Melle, and Opjordsmoen). It was also funded by the Theodore and Vada Stanley Foundation; the Regional Health Research Foundation for Eastern Region, Denmark; Roskilde County, Denmark; Helsefonden Lundbeck Pharma; Eli Lilly; and Janssen-Cilag Pharmaceuticals (Drs Simonsen and Haahr). It was also supported by a National Alliance for Research on Schizophrenia and Depression (NARSAD) Distinguished Investigator Award and National Institute of Mental Health grant MH-01654 (Dr McGlashan) and a NARSAD Young Investigator Award (Dr Larsen).
References
- 1.McGorry PD, Yung AR. Early intervention in psychosis: an overdue reform. Aust N Z J Psychiatry. 2003;37:393–398. doi: 10.1046/j.1440-1614.2003.01192.x. [DOI] [PubMed] [Google Scholar]
- 2.McGlashan TH. Duration of untreated psychosis in first-episode schizophrenia: marker or determinant of course? Biol Psychiatry. 1999;46:899–907. doi: 10.1016/s0006-3223(99)00084-0. [DOI] [PubMed] [Google Scholar]
- 3.Ho BC, Alicata D, Ward J, et al. Untreated initial psychosis: relation to cognitive deficits and brain morphology in first-episode schizophrenia. Am J Psychiatry. 2003;160:142–148. doi: 10.1176/appi.ajp.160.1.142. [DOI] [PubMed] [Google Scholar]
- 4.Craig TJ, Bromet EJ, Fennig S, Tanenberg-Karant M, Lavelle J, Galambos N. Is there an association between duration of untreated psychosis and 24-month clinical outcome in a first-admission series? Am J Psychiatry. 2000;157:60–66. doi: 10.1176/ajp.157.1.60. [DOI] [PubMed] [Google Scholar]
- 5.Hoff AL, Sakuma M, Razi K, Heydebrand G, Csernansky JG, DeLisi LE. Lack of association between duration of untreated illness and severity of cognitive and structural brain deficits at the first episode of schizophrenia. Am J Psychiatry. 2000;157:1824–1828. doi: 10.1176/appi.ajp.157.11.1824. [DOI] [PubMed] [Google Scholar]
- 6.Barnes TR, Hutton SB, Chapman MJ, Mutsatsa S, Puri BK, Joyce EM. West London first-episode study of schizophrenia. Clinical correlates of duration of untreated psychosis. Br J Psychiatry. 2000;177:207–211. doi: 10.1192/bjp.177.3.207. [DOI] [PubMed] [Google Scholar]
- 7.Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry. 2005;62:975–983. doi: 10.1001/archpsyc.62.9.975. [DOI] [PubMed] [Google Scholar]
- 8.Norman RM, Malla AK. Duration of untreated psychosis: a critical examination of the concept and its importance. Psychol Med. 2001;31:381–400. doi: 10.1017/s0033291701003488. [DOI] [PubMed] [Google Scholar]
- 9.Friis S, Larsen TK, Melle I, et al. Methodological pitfalls in early detection studies—the NAPE Lecture 2002. Nordic Association for Psychiatric Epidemiology. Acta Psychiatr Scand. 2003;107:3–9. doi: 10.1034/j.1600-0447.2003.02600.x. [DOI] [PubMed] [Google Scholar]
- 10.McGlashan TH, Johannessen JO. Early detection and intervention with schizophrenia: rationale. Schizophr Bull. 1996;22:201–222. doi: 10.1093/schbul/22.2.201. [DOI] [PubMed] [Google Scholar]
- 11.Johannessen JO, McGlashan TH, Larsen TK, et al. Early detection strategies for untreated first-episode psychosis. Schizophr Res. 2001;51:39–46. doi: 10.1016/s0920-9964(01)00237-7. [DOI] [PubMed] [Google Scholar]
- 12.Melle I, Larsen TK, Haahr U, et al. Reducing the duration of untreated psychosis in first episode psychosis: effects on clinical presentation. Arch Gen Psychiatry. 2004;61:143–150. doi: 10.1001/archpsyc.61.2.143. [DOI] [PubMed] [Google Scholar]
- 13.Lehman AF, Steinwachs DM. Evidence-based psychosocial treatment practices in schizophrenia: lessons from the patient outcomes research team (PORT) project. J Am Acad Psychoanal Dyn Psychiatry. 2003;31:141–154. doi: 10.1521/jaap.31.1.141.21939. [DOI] [PubMed] [Google Scholar]
- 14.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 15.Spitzer RL, Williams JB, Gibbon M, First MB. The structured clinical interview for DSM-III-R (SCID). I: history, rationale, and description. Arch Gen Psychiatry. 1992;49:624–629. doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- 16.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- 17.Lehman AF. A quality of life interview for the chronically mentally-ill. Eval Program Plann. 1988;11:51–62. [Google Scholar]
- 18.Drake RE, Osher FC, Noordsy DL, Hurlbut SC, Teague GB, Beaudett MS. Diagnosis of alcohol use disorders in schizophrenia. Schizophr Bull. 1990;16:57–67. doi: 10.1093/schbul/16.1.57. [DOI] [PubMed] [Google Scholar]
- 19.Loebel AD, Lieberman JA, Alvir JM, Mayerhoff DI, Geisler SH, Szymanski SR. Duration of psychosis and outcome in first-episode schizophrenia. Am J Psychiatry. 1992;149:1183–1188. doi: 10.1176/ajp.149.9.1183. [DOI] [PubMed] [Google Scholar]
- 20.Kirkpatrick B, Buchanan RW, McKenney PD, Alphs LD, Carpenter WT., Jr The schedule for the deficit syndrome: an instrument for research in schizophrenia. Psychiatry Res. 1989;30:119–123. doi: 10.1016/0165-1781(89)90153-4. [DOI] [PubMed] [Google Scholar]
- 21.UK Department of Health. The NHS Plan—A Plan for Investment, a Plan for Reform. London, England: Author; 2000. [Google Scholar]