Abstract
One of the major clinical problems in the treatment of people with schizophrenia is suboptimal medication adherence. Most research focusing on determinants of nonadherence use quantitative research methods. These studies have some important limitations in exploring the decision-making process of patients concerning medication. In this study we explore factors influencing medication adherence behavior in people with schizophrenia using concept mapping. Concept mapping is a structured qualitative method and was performed in 4 European countries. Participants were 27 patients with schizophrenia, 29 carers, and 28 professionals of patients with schizophrenia. Five clinically relevant themes were identified that affect adherence: medication efficacy, external factors (such as patient support and therapeutic alliance), insight, side effects, and attitudes toward medication. Importance ratings of these factors differed significantly between professionals and carers and patients. Professionals, carers, and patients do not have a shared understanding of which factors are important in patients' medication adherence behavior. Adherence may be positively influenced if professionals focus on the positive aspects of medication, on enhancing insight, and on fostering a positive therapeutic relationship with patients and carers.
Keywords: medication adherence, schizophrenia, concept mapping
Introduction
Treatment nonadherence limits the clinical effectiveness of prescribed medication.1 Studies often report that about 50% of patients are treatment nonadherent across a range of disorders.2 Different authors, often using a quantitative approach, generally present a range of factors that influence treatment adherence with medication in patients with schizophrenia.3–7 Consistently reported factors include insight, beliefs about treatment, medication side effects, and treatment efficacy.3 Although research has improved our knowledge, adherence rates do not seem to have changed in the last 4 decades.8,9
More recently, interventions focused on nonadherence were developed. Several researchers have proposed that these adherence interventions should focus more on patients' decision-making process.6,10 For this, quantitative studies have some, but limited, value because they fail to adequately explain the complexity of medication-taking behavior and are only able to explore a limited number of variables.
Other more qualitative studies have tried to describe adherence behavior by focusing on the subjective responses or experiences of patients with antipsychotic medications and their decision-making process in relation to starting, continuing, or stopping medication. Conclusions regarding which factors influence adherence behavior are often based on either patients'11–14 or professionals' views.15 These views might differ as we know from research in other fields. Fischer et al,16 for instance, showed that patients', carers', and professionals' views concerning outcome and service priorities vary widely. Similar conclusions were drawn by Pope and Scott,17 studying main reasons to stop medication treatment in patients receiving lithium for an affective disorder. To increase our understanding of medication adherence, we should make use of the valuable expertise and experience of different stakeholder groups. Relying solely on one of these groups might give limited and unsatisfactory results.
The aim of this article is to learn more about (non)adherence in patients with schizophrenia. For this, we will use concept mapping, an established qualitative methodology, to explore factors that influence adherence behavior in patients with schizophrenia. We will include the opinions of patients, carers, and professionals from 4 countries.
MATERIALS AND METHODS
Setting
This study was conducted in 4 European Union countries: England, Germany, Italy and the Netherlands. It was part of the quality of life following adherence therapy for people disabled by schizophrenia and their carers (QUATRO) study, an international multisite randomized controlled trial assessing the effectiveness of adherence therapy in people with schizophrenia. All study sites gained full approval for the study from the appropriate local research ethics committee.
Participants
Participants were purposively selected out of the 3 stakeholder groups. Patients were meeting International Statistical Classification of Diseases and Related Health Problems, 10th Revision (ICD-10) criterion for schizophrenia. Carers and professionals were, respectively, caring for and working with patients with schizophrenia. All participants needed to be familiar with positive and negative consequences of antipsychotic medication. Therefore, patients needed to have had antipsychotic medication prescribed to them for at least 1 year. Carers and professionals needed to care for or work with patients with schizophrenia for a period of at least 2 years. Participants should have experience with nonadherence. Although the majority of patients and, consequently, their carers go through a nonadherent period during the course of their illness,6,18 patients were only included if they had been clinically instable in the previous year. This was defined by one or more of the following: at least one hospital admission on clinical (mental health) grounds, a change in antipsychotic medication, increased frequency of planned or actual contact, and indications of clinical instability from relatives, carers, or clinical team. These criteria were considered indicative of nonadherence. Carers were included if they were caring for patients fulfilling inclusion criteria. All participants were further expected to be able to adequately verbalize ideas and thoughts concerning medication adherence and perform the required tasks. A high-quality systematic review indicated that other sociodemographic characteristics have no influence on medication adherence3 and were therefore not assessed in this study. In order to increase variability of generated statements and generalizability of our results, stakeholder groups were unrelated. All participants gave written informed consent.
Procedure
To study variables or factors that (positively or negatively) influence patients, medication adherence behavior concept mapping was used. This method uses group discussions with patients, carers, and professionals to explore factors related to medication adherence. In contrast to other qualitative methods it also comprises a clustering and a prioritizing task. The clustering task allows for the participants to determine which factors or clusters emerge from the data and to what extent these clusters are related to each other. Therefore, compared with other qualitative research methods, the interpretation of the qualitative data might be less susceptible to the hypothesis that researchers may have. The prioritizing task enables, using a quantitative methodology, a comparison of the relative importance stakeholder groups address to the different factors or clusters.19,20
The procedure was administered by a trained facilitator and cofacilitator in each country. Concept mapping consists of 4 stages. For each stage, a written protocol was provided to make sure all sites followed the same procedure. A copy of the manual can be requested from the first author.
During the first stage, brainstorming sessions were held separately for patients, carers, and professionals in each of the 4 sites. According to Concept Mapping protocol,21 each of these 12 sessions were attended by 6–9 participants and took approximately 1.5 hours. Due to having 12 sessions, our study sample exceeded that of typical concept-mapping studies in which it is between 10 and 20.19 Patients were invited to generate statements focusing on “all factors that influence whether you take or not take antipsychotic medication.” Carers and professionals were asked to generate statements on “all factors influencing the start and continued use of antipsychotic medication.” If patients were inhibited to verbalize their thoughts, they were invited to submit statements in writing or on a one-to-one basis after the session finished.
In the second stage, the number of generated statements had to be reduced to below 100 in order to control the complexity of the following steps. After translation into English, 5 researchers (not involved in the brainstorming sessions) independently reviewed all generated statements. Statements that were not understandable, not singular, too specific, or too abstract were removed. Next, repetitive or overlapping statements were combined into single statements. Finally, in each country, the remaining statements were reviewed and rated by researchers according to how well each related to the topic of medication adherence on a 3-point scale. Those rated least relevant were excluded, leaving a final list of statements. These were back-translated into German, Italian, and Dutch. Translations were conducted according to WHO guidelines.22
Finally, in the third and fourth stage of the concept-mapping procedure, statements had to be clustered and prioritized. Groups were reconvened, and participants were asked to individually perform the remaining tasks. First, participants had to organize the statements they thought belonged to the same category into clusters (stage three). Clustering could be done in any way the participant thought was logical. Each cluster had to contain between 5 and 40 statements. In addition, individual participants were asked to prioritize the statements (stage four) by sorting them into 5 equal piles, ranging from least to most important. Patients were asked how important each aspect was for their decision to take or not take antipsychotic medication, and carers and professionals were asked to rate how important they thought each aspect was for patients.
Data Analysis
The “Ariadne” software package was used to perform 2 types of analysis.21 The first, a principal component analysis, positions the statements on a concept map. Here the distance between statements represents how often they have been sorted together. Secondly, a cluster analysis grouped statements in clusters. This analysis produced between 2 and 18 clusters. Three researchers independently reviewed each of these 17 computer-generated cluster solutions starting with the simplest (ie, 2 clusters) and ending with the most complex (ie, 18 clusters). The cluster solution that was most understandable and meaningful was selected.
Finally, the relative importance of each cluster was calculated using the prioritizing data. For each participant, the percentage of statements, in each cluster, rated 4 or 5 (important) was calculated. Differences in means were tested using analysis of variance.
Results
Brainstorming sessions were attended by 91 participants (41% male) and the prioritizing and clustering sessions by 89 participants (44% male), approximately equally divided over the 4 sites (table 1). Results of 4 patients and 1 carer across 3 sites were removed from the data set. These participants indicated they found the clustering and/or prioritizing task too complicated. They also did not profit from support, and their results clearly demonstrated their lack of understanding (eg, statements clustered according to card number instead of contents).
Table 1.
Participants in Brainstorming Session (BS) and Clustering and Prioritizing Tasks (CP)
| Patients |
Carers |
Professionals |
Total |
|||||
| BS | CP | BS | CP | BS | CP | BS | CP | |
| Amsterdam | 6 | 6 | 6 | 7 | 8 | 8 | 20 | 21 |
| Leipzig | 9 | 6 | 7 | 7 | 6 | 4 | 22 | 17 |
| London | 7 | 7 | 8 | 7 | 9 | 8 | 24 | 22 |
| Verona | 8 | 8 | 8 | 8 | 9 | 8 | 25 | 24 |
| Total | 30 | 27 | 29 | 29 | 32 | 28 | 91 | 84 |
On average, patients (n = 27; 59% male) had been prescribed antipsychotic medication for a period of 8.6 years (SD = 8.2). Carers (n = 29; 28% male) had been caring for someone with schizophrenia for an average of 12.6 (SD = 7.4) years, and professionals (n = 28; 46% male) had been working with patients with schizophrenia for an average of 11.4 (SD = 11.1) years.
Brainstorming
The 12 brainstorming sessions produced a total of 769 statements relating to factors influencing medication adherence for patients with schizophrenia. Generated statements confirmed that participants were familiar with both positive and negative aspects of antipsychotic medication. Out of all the statements generated by patients, carers, and professionals, respectively, 48%, 42%, and 51% were negative aspects of medication use. Following translation, researchers reached consensus on the elimination of 141 statements not meeting the criteria and combined 424 statements with other statements because they were repetitive or overlapping. The amount of overlap indicated issues reaching a point of saturation. The remaining 204 statements were rated, resulting in a final set of 82 statements, of which approximately equal numbers of statements were found to be produced by the 3 stakeholder groups (56% of statements were mentioned by patients, 56% by carers, and 66% by professionals) and across the 4 sites.
Clustering
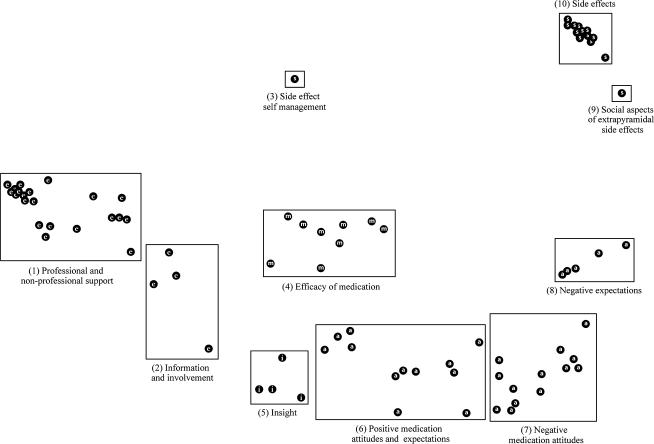
All statements are presented as dots on the concept map in figure 1. Their spatial position is based on the clustering results. Statements that the participants sorted together more frequently are positioned closer to each other on the concept map. Consequently, the distances between the statements in figure 1 indicate to what extent, according to the participants, statements and, consequently, clusters are related to each other. On the basis of these interstatement distances, cluster are defined. A 10-cluster solution was considered to be most understandable and meaningful. A cluster solution with fewer clusters resulted in the loss of clinically relevant clusters. Cluster solutions with more clusters were difficult to interpret and resulted in clusters that were considered less meaningful. Clusters that were located close to each other referred to distinct but clinically related topics. Clusters on the map were numbered from left to right and labeled. Examples of statements are shown in table 2.
Fig. 1.
Concept map of factors influencing medication adherence for patients with schizophrenia. The map displays the 82 statements as dots, the 10 clusters, and 5 clinical themes; medication efficacy (m), external factors (e), insight (i), side effects (s), and medication attitudes (a). Distance between statements indicates how often they have been sorted together.
Table 2.
Cluster Number, Cluster Label, and Examples of Statements
| Cluster Number and Label | Examples of Statements |
| 1: Professional and nonprofessional support | “being accurately informed about the potential side effects of the medication” |
| “the doctor asking you how you feel, being understanding and listening to your concerns” | |
| “family, friends remind you to take your medication” | |
| “accessibility of the medication (getting the prescription and medication on time)” | |
| 2: Information and involvement | “being given the choice whether or not to take medication” |
| “listening to other patients experiences of taking medication” | |
| “not being told what your diagnosis is” | |
| “having an understanding of the illness” | |
| 3: Side effect self-management | “knowing how to manage the side effects” |
| 4: Efficacy of medication | “being able to function better due to the medication” |
| “the medication is effective in reducing the hallucinations” | |
| “the medication keeps you from feeling ill/ relapsing” | |
| 5: Insight | “having insight into the illness” |
| “accepting that medication is needed” | |
| “your cultural beliefs fit in with medical advice” | |
| 6: Positive medication attitudes and expectations | “having faith that the medication is effective” |
| “taking medication to avoid going back into hospital” | |
| “good previous experiences with medication” | |
| 7: Negative medication attitudes | “feeling suspicious about the medication” |
| “believe that the medication will harm you” | |
| “the voices telling you not to take the medication” | |
| “believe that taking medication is unnatural” | |
| 8: Negative expectations | “feeling better when you stop taking it” |
| “a traumatic experience the first time you were given medication” | |
| “preferring the symptoms to the side effects” | |
| 9: Social aspects of extrapyramidal side effects | “being embarrassed about movement disorders because people can see it” |
| 10: Side effects | “obesity/weight gain due to the medication” |
| “sexual problems due to the medication” | |
| “feeling tired due to the medication” |
Prioritizing
Table 3 shows the average percentages of statements in each cluster which were rated as important by patients, carers, and professionals. There was general agreement between patient and carer ratings of the relative importance of each cluster. However, there were a number of significant differences between patient and/or carer and professional ratings. The latter rated the efficacy of medication (cluster 4) as significantly less important and negative medication attitudes and beliefs (cluster 7) as more important cluster than carers and patients. The professional and nonprofessional support cluster (cluster 1) was rated as less important and the side effect cluster (cluster 10) as more important by professionals compared with carers.
Table 3.
Mean Percentage of Items Per Cluster Rated 4 or 5 (important), Stratified by Patients (Pa), Carers (Ca) and Professionals (Pr)
| Cluster Number and Label | Number of Statements | Pa (n = 27) |
Ca (n = 29) |
Pr (n = 28) |
p < 0.05c | |||
| Meana (%) (SD) | rb | Meana (%) (SD) | rb | Meana (%) (SD) | rb | |||
| 4: Efficacy of medication | 9 | 54 (20) | 1 | 64 (23) | 1 | 40 (21) | 5 | Pa-Pr; Ca-Pr |
| 3: Side effect self-management | 1 | 48 (51) | 2 | 34 (48) | 6 | 39 (50) | 6/7 | |
| 5: Insight | 4 | 44 (19) | 3 | 54 (21) | 2 | 52 (23) | 1 | |
| 1: Professional and nonprofessional support | 21 | 42 (12) | 4/5 | 52 (16) | 3 | 37 (15) | 8/9 | Ca-Pr |
| 6: Positive medication attitudes and expectations | 12 | 42 (14) | 4/5 | 36 (14) | 4/5 | 36 (12) | 10 | |
| 10: Side effects | 12 | 40 (21) | 6 | 28 (19) | 8/9 | 46 (24) | 2 | Ca-Pr |
| 2: Information and involvement | 4 | 39 (22) | 7 | 36 (21) | 4/5 | 37 (24) | 8/9 | |
| 8: Negative expectations | 5 | 36 (22) | 8 | 32 (18) | 7 | 43 (22) | 3 | |
| 7: Negative medication attitudes | 13 | 30 (13) | 9 | 25 (16) | 10 | 42 (14) | 4 | Pa-Pr; Ca-Pr |
| 9: Social aspects of extrapyramidal side effects | 1 | 22 (42) | 10 | 28 (45) | 8/9 | 39 (50) | 6/7 | |
For each participant, the percentage of statements rated 4 or 5 (important) in each cluster was calculated. The mean percentages over raters are reported in the table (eg, patients rated on average 54% of the nine statements in cluster 4 as important).
Rank order of cluster based on mean percentage.
Analysis of variance, multiple comparisons (Tukey's honestly significant difference test).
Discussion
In this study, we used concept mapping to explore “all factors influencing the start and continued use of antipsychotic medication” comprehensively by including 3 different and independent groups of stakeholders, all familiar with schizophrenia for many years, from 4 different countries. In this discussion, we will interpret our results and describe its clinical and research implications.
Content and spatial location of the clusters are used to interpret the concept map and identify clinically relevant themes (figure 1). Statements, except those in clusters 1, 2, and 5, referred to perceived advantages or disadvantages of medication use and were divided into 3 themes; right in the middle we identified medication efficacy (cluster 4), surrounded clockwise by issues related to side effects (clusters 3, 9, and 10) and attitudes (clusters 6, 7, and 8). Although closely located, due to the content of the statements, insight (cluster 5) is considered a separate theme in this concept map. The remaining clusters 1 and 2, both distant from the other clusters, referred to external factors.
Efficacy
Cluster 4 represents the subjective efficacy of medication due to a relief of symptoms. Patients and carers both rated this cluster as the most important for medication adherence. This is in line with authors showing that the beneficial effects of medication on well-being have a major influence on adherence behavior.14,23–25 Accordingly, studies showed that patients who have the experience of their medications having no benefit, not being helpful, or being ineffective and unnecessary more often do not comply.18,26–29
Professionals in our study surprisingly rated efficacy significantly less important than patients and carers. Professionals should (re)value efficacy as more important and are advised to closely monitor and discuss medication efficacy, from the patients perspective, as well as the perceived degree (or absence) of adverse symptoms, in order to understand and manage medication adherence.
External Factors
Clusters 1 (professional and nonprofessional support) and 2 (information and involvement) contain statements that refer to factors which contribute to establishing favorable conditions for adherence behavior by different means, such as increasing patients understanding, alliance, or trust with clinician; social support; and reduction of practical medication barriers. These factors can be labeled as external because they refer to influences from outside by important others, not directly under the control of the patient. Both clusters adjoin but are distant from the other clusters in the concept map, suggesting that they are not strongly related to the other clusters.
Nonprofessional (or professional) support, information, and involvement have been studied as important predictors of treatment adherence in people with schizophrenia.30–34 Some psychological approaches enhancing treatment adherence have placed them at the heart of the intervention,10,35 which is in accordance with our finding that patients and, in particular, carers rated support, information, and involvement as rather important. So far, compliance interventions focused on education and information have not been found to be effective in improving adherence.10 This might explain why professionals rate these issues as less important.36
Insight
The map shows that insight (cluster 5) is closely related to positive expectations and attitudes toward the use of antipsychotic medication (cluster 6). All groups rated the insight cluster as important, which is in line with studies describing insight as a strong predictor of medication adherence.3,37–39 This effect of insight has been addressed to an improvement in understanding illness and medication consequences. The spatial locations of clusters 4 and 5 show that a clear relation with medication efficacy (cluster 4) is, however, lacking. Insight seems less important for appreciating subjective symptom relief due to medication than for indirect treatment benefit such as hospitalization or coercion. A patient who uses his or her medication because it improves well-being does not necessarily need to have insight into the disorder. This might also explain why Nageotte et al40 found that 38% of patients were compliant despite the fact that they did not believe themselves to be ill.
Side Effects
Statements related to side effects that referred to objective perceived side effects of medication (cluster 10), the social aspects of side effects (in particular, movement disorders) (cluster 9), and self-management of side effects (cluster 3). The latter cluster referred to a positive characteristic, which patients rated as very important.
Medication side effects have often been associated with nonadherence,24,41,42 although a consistent correlation between the presence or severity of these and the degree of adherence could not be found in a recent systematic review.3 Side effects might not be the most important factor in determining adherence behavior25,39–43 and may have less impact than the efficacy of medication44–46 or expressed beliefs concerning susceptibility to relapse.26
Our results confirm this and show that patients and carers prioritized side effects relatively low compared with positive medication aspects. In comparison, professionals prioritized side effects as the second most important cluster and, consequently, seem to overestimate the relative importance of side effects on adherence behavior. Although discussing side effects is essential during treatment because it is the most important disadvantage of medication use for patients, professionals might, however, understand the relative importance better in relation to other factors such as perceived advantages of medication, and coping strategies are taken into account.
Medication Attitudes
Finally, the clusters 6, 7, and 8 represent not only beliefs and attitudes concerning medication but also previous experiences with these agents. Statements of cluster 6 represent positive aspects or benefits of medication (eg, reducing adverse consequences of being ill such as hospitalization or coercion). Clusters 7 and 8 refer to negative attitudes and beliefs concerning medication and feeling better without medication. Different authors have stressed that both attitudes to medication and side effects have to be openly discussed with patients.25,47
Prioritizing
Patients were instructed to rate the importance of statements based on their own experiences. Carers and professionals rated statements based on their observations of, and experiences with, patients. Two points are of interest. First, professionals, in general, rated negative aspects (side effects and negative medication attitudes) as more important than patients and carers, while patients and carers, more than professionals, stressed the positive aspects (efficacy and support). Secondly, the fact that carers and patients in our study prioritized clusters in a similar way indicates that carers can be well aware of patients' considerations concerning medication. Our results underline that professionals need to carefully assess patients' beliefs and experiences of treatment with antipsychotic medication in order to understand patients' perspectives. They also, if possible, should involve carers in treatment planning and evaluation. Not only will it improve patients' support, which was found to be an important issue, but also carers might be able to provide professionals with valuable information.
Models for Understanding Adherence
Our results correspond with the Health Belief Model, often used to explain adherence behavior.48 According to this model, individuals' readiness to take action depends on their “perceived seriousness and susceptibility of illness” (such as belief in the accuracy of the diagnosis and subjective vulnerability to relapse) and “perceived benefits and barriers of medication use.” This is reflected in the themes insight, efficacy of medication, side effects, and medication attitudes. These themes demonstrate patients' considerations concerning advantages and disadvantages of medication use. Contrary to the Health Belief Model, we did not find perceived illness severity and medication benefit to be separate themes (eg, “the medication is effective in reducing the hallucinations”).
We argue that patients are most motivated to use medication if they experience direct beneficial effects such as a reduction of adverse symptoms and/or because they realize it has indirect, long-term benefits such as preventing relapse. Although illness insight is not clearly positioned in the Health Belief Model, our results seem to indicate that insight is particularly important for patients to understand and appreciate the indirect benefit of medication. Therefore, patients who experience no direct subjective benefit from medication are most likely to benefit from psychoeducation or brief cognitive behavioral therapy to enhance insight.49
The external factors show us that there are a number of factors which are not under patient control, but which might affect adherent behavior. These factors include the alliance between carers and their key worker, the information given to patients, actively involving patients in treatment, and practical medication barriers. These factors are similar to “cues to action” in the Health Belief Model. Clinicians should therefore make every effort to inform patients concerning their illness and medication, increase patients understanding, their alliance with their patient, the provision of social support, and reduction of practical medication barriers.
Results of this study might be useful in screening patients with schizophrenia. Discussing the topics that were found in this study should help professionals to detect patients likely to be nonadherent.
Limitations
This study has some limitations. First, it should be noted that results are limited to issues which were involved in the decision-making process of patients. Therefore, factors which have been found to correlate with adherent behavior such as sociodemographic characteristics and previous nonadherence are not reported in this study. Patient reports are limited to issues they are aware of and they are prepared to mention.
We included a heterogeneous sample of 91 participants. Although this is in accordance with the concept map protocol, this number is relatively low for analysis of between-group differences. However, differences were significant even with this low numbers per group.
Patients were selected if they had been clinically instable for some period of time within the previous year. This inclusion criterion might have influenced our results because these patients may have stressed the importance of factors that negatively influence medication adherence.
Conclusion
In conclusion, this study has learned that concept mapping is a useful tool in exploring relevant issues for patients' decision to use or not use prescribed antipsychotic medication. The findings suggest that patients, carers, and professionals were able to identify and weigh up the factors that influence treatment adherence. Our findings provide a comprehensive overview of all relevant issues and how they relate to one another. Clusters could be organized into 5 clinically relevant themes: efficacy of medication, external factors, insight, side effects, and medication attitudes.
The discrepancies between patients' and professionals' views on the importance of clusters should be further explored in future research. Professionals need to be aware of patients' considerations concerning their antipsychotic medication, in particular positive aspects of medication use, in order to provide effective support and guidance. Consequently, strengthening mutual understanding and alliance could improve adherence or make it easier to come to agreements on individually tailored medication regimens. Therefore, closing the gap between patients' and professionals' views on the importance of medication-related aspects seems vital.
Acknowledgments
The QUATRO study is a multicentre collaboration between the Health Services Research Department, Institute of Psychiatry, King's College London; the Department of Medicine and Public Health, Section of Psychiatry and Clinical Psychology; University of Verona, Italy; the Department of Psychiatry, Leipzig University, the Department of Psychiatry II, Ulm University, Germany, and the Department of Psychiatry, Academic Medical Center, University of Amsterdam, the Netherlands. The study was funded by a grant from the Quality of Life and Management of Living Resources Programme of the European Union (QLG4-CT-2001-01734). The views expressed in this article are those of the authors and not necessarily those of the funders. We also wish to acknowledge the contributions of the patients, carers, and staff who have taken part in this study. We would like to acknowledge the contributions to this study of the following colleagues—Amsterdam site: Aart Schene, Annemarie Fouwels, Martijn Kikkert, Maarten Koeter, and Carin Meijer; Leipzig/Ulm site: Thomas Becker, Matthias Angermeyer, Anja Born, Anne Gießler, Hedda Helm, and Bernd Puschner; London site: Jonathan Bindman, Jayne Camara, Anthony David, Kevin Gournay, Richard Gray, Martin Knapp, Morven Leese, Paul McCrone, Mauricio Moreno, Anita Patel, Debbie Robson, Graham Thornicroft, and Ian White; and Verona site: Michele Tansella, Francesco Amaddeo, Corrado Barbui, Lorenzo Burti, Daniela Celani, Doriana Cristofalo, Claudia Goss, Antonio Lasalvia, Giovanna Marrella, Mariangela Mazzi, Michela Nosè, Mirella Ruggeri, and Marta Solfa. We also like to thank Carin Meijer, Emile Barkhof, and Udo Nabitz for their contributions to this article.
References
- 1.Haynes RB, McDonald HP, Garg AX. Interventions for Helping Patients to Follow Prescriptions for Medications. Issue 2. Oxford: Cochrane Library Update Software; 2002. [DOI] [PubMed] [Google Scholar]
- 2.World Health Report. The magnitude of the problem of poor adherence. In: Sabaté E, editor. Adherence to Long Term Therapies: Evidence for Action. Geneva: World Health Organization; 2003. pp. 7–10. [Google Scholar]
- 3.Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: A comprehensive review of recent literature. J Clin Psychiat. 2002;63:892–909. doi: 10.4088/jcp.v63n1007. [DOI] [PubMed] [Google Scholar]
- 4.Lindstrom E, Bingefors K. Patient compliance with drug therapy in schizophrenia: economic and clinical issues. Pharmacoeconomics. 2000;18:105–124. doi: 10.2165/00019053-200018020-00002. [DOI] [PubMed] [Google Scholar]
- 5.Oehl M, Hummer M, Fleischhacker WW. Compliance with antipsychotic treatment. Acta Psychiatr Scand. 2000;102:83–86. doi: 10.1034/j.1600-0447.2000.00016.x. [DOI] [PubMed] [Google Scholar]
- 6.Fenton WS, Blyler CR, Heinssen RK. Determinants of medication compliance in schizophrenia: empirical and clinical findings. Schizophr Bull. 1997;23:637–651. doi: 10.1093/schbul/23.4.637. [DOI] [PubMed] [Google Scholar]
- 7.Hughes I, Hill B, Budd R. Characteristics of schizophrenic and schizoaffective compliers and noncompliers with psychiatric medication. Diss Abstr Int Sect B Sci Eng. 1997;57:6584. [Google Scholar]
- 8.Parkes CM, Brown GW, Monck EM. The general practitioner and the schizophrenic patient. Br Med J. 1962;5283:972–976. doi: 10.1136/bmj.1.5283.972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Renton CA, Affleck FW, Carstairs GM, Forrest AD. A follow-up of schizophrenic patients in Edinburgh. Acta Psychiat Scand. 1963;39:548–600. doi: 10.1111/j.1600-0447.1963.tb07482.x. [DOI] [PubMed] [Google Scholar]
- 10.Gray R, Wykes T, Gournay K. From compliance to concordance: a review of the literature on interventions to enhance compliance with antipsychotic medication. J Psychiatr Ment Health Nurs. 2002;9:277–284. doi: 10.1046/j.1365-2850.2002.00474.x. [DOI] [PubMed] [Google Scholar]
- 11.Carder PC, Vuckovic N, Green CA. Negotiating medications: patient perceptions of long-term medication use. J Clin Pharm Ther. 2003;28:409–417. doi: 10.1046/j.0269-4727.2003.00511.x. [DOI] [PubMed] [Google Scholar]
- 12.Carrick R, Mitchell A, Powell RA, Lloyd K. The quest for well-being: A qualitative study of the experience of taking antipsychotic medication. Psychol Psychother. 2004;77:19–33. doi: 10.1348/147608304322874236. [DOI] [PubMed] [Google Scholar]
- 13.Holzinger A, Loffler W, Muller P, Priebe S, Angermeyer MC. Subjective illness theory and antipsychotic medication compliance by patients with schizophrenia. J Nerv Ment Dis. 2002;190:597–603. doi: 10.1097/01.NMD.0000030524.45210.FD. [DOI] [PubMed] [Google Scholar]
- 14.Rogers A, Day J, Williams B, et al. The meaning and management of neuroleptic medication: a study of patients with a diagnosis of schizophrenia. Soc Sci Med. 1998;47:1313–1323. doi: 10.1016/s0277-9536(98)00209-3. [DOI] [PubMed] [Google Scholar]
- 15.Weiden P, Rapkin B, Mott T, et al. Rating of Medication Influences (ROMI) scale in schizophrenia. Schizophr Bull. 1994;20:297–310. doi: 10.1093/schbul/20.2.297. [DOI] [PubMed] [Google Scholar]
- 16.Fischer EP, Shumway M, Owen RR. Priorities of consumers, providers, and family members in the treatment of schizophrenia. Psychiatr Serv. 2002;53:724–729. doi: 10.1176/appi.ps.53.6.724. [DOI] [PubMed] [Google Scholar]
- 17.Pope M, Scott J. Do clinicians understand why individuals stop taking lithium? Affect Disord. 2003;74:287–291. doi: 10.1016/s0165-0327(02)00341-5. [DOI] [PubMed] [Google Scholar]
- 18.Lieberman JA, Stroup TS, McEvoy JP, et al. Effectiveness of antipsychotic drugs in patients with schizophrenia. N Engl J Med. 2005;353:1209–1223. doi: 10.1056/NEJMoa051688. [DOI] [PubMed] [Google Scholar]
- 19.Southern DM, Batterham RW, Appleby NJ, Young D, Dunt D, Guibert R. The concept mapping method: An alternative to focus group inquiry in general practice. Aust Fam Physician. 1998;28:S35–S40. [PubMed] [Google Scholar]
- 20.Trochim WMK. An introduction to concept mapping for planning and evaluation. Eval Program Plann. 1989;12:1–16. [Google Scholar]
- 21.Severens P. Handbook Concept Mapping. Amsterdam: Talcott. National Centre for Mental Health; 1995. [Google Scholar]
- 22.Sartorius N, Kuyken W. Translation of health status instruments. In: Orley J, Kuyken W, editors. Proceedings of the Joint Meeting Organised by the World Health Organization and the Foundation IPSEN. Paris: Springer; 1994. pp. 3–18. [Google Scholar]
- 23.Freudenreich O, Cather C, Evins AE, Henderson DC, Goff DC. Attitudes of schizophrenia outpatients towards psychiatric medications: Relationship to clinical variables and insight. J Clin Psychiat. 2004;65:1372–1376. doi: 10.4088/jcp.v65n1012. [DOI] [PubMed] [Google Scholar]
- 24.Rettenbacher M, Hofer A, Eder U, et al. Compliance in schizophrenia: psychopathology, side effects, and patient's attitudes toward the illness and medication. J Clin Psychiat. 2004;65:1211–1218. doi: 10.4088/jcp.v65n0908. [DOI] [PubMed] [Google Scholar]
- 25.Adams SG, Howe JT. Predicting medication compliance in a psychotic population. J Nerv Ment Dis. 1993;181:558–560. doi: 10.1097/00005053-199309000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Nelson AA, Jr, Gold BH, Hutchinson RA, Benezra E. Drug default among schizophrenic patients. Am J Hosp Pharm. 1975;32:1237–1242. [PubMed] [Google Scholar]
- 27.Ruscher SM, de WR, Mazmanian D. Psychiatric patients' attitudes about medication and factors affecting noncompliance. Psychiatr Serv. 1997;48:82–85. doi: 10.1176/ps.48.1.82. [DOI] [PubMed] [Google Scholar]
- 28.Hertz M, Melville C. Relapse in schizophrenia. Am J Psychiatry. 1980;137:801–805. doi: 10.1176/ajp.137.7.801. [DOI] [PubMed] [Google Scholar]
- 29.Gasquet I, Haro JM, Novick D, et al. Pharmacological treatment and other predictors of treatment outcomes in previously untreated patients with schizophrenia: results from the European Schizophrenia Outpatient Health Outcomes (SOHO) study. Int Clin Psychopharmacol. 2005;20:199–205. doi: 10.1097/00004850-200507000-00002. [DOI] [PubMed] [Google Scholar]
- 30.Agarwal MR, Sharma VK, Kishore Kumar KV, Lowe D. Non-compliance with treatment in patients suffering from schizophrenia: a study to evaluate possible contributing factors. Int J Soc Psychiart. 1998;44:92–106. doi: 10.1177/002076409804400202. [DOI] [PubMed] [Google Scholar]
- 31.Frank AF, Gunderson JG. The role of the therapeutic alliance in the treatment of schizophrenia. Relationship to course and outcome. Arch Gen Psychiatry. 1990;47:228–236. doi: 10.1001/archpsyc.1990.01810150028006. [DOI] [PubMed] [Google Scholar]
- 32.Kelly GR, Scott JE, Mamon J. Medication compliance and health education among outpatients with chronic mental disorders. Med Care. 1990;28:1181–1197. doi: 10.1097/00005650-199012000-00006. [DOI] [PubMed] [Google Scholar]
- 33.Olfson M, Mechanic D, Hansell S, Boyer CA, Walkup J, Weiden PJ. Predicting medication noncompliance after hospital discharge among patients with schizophrenia. Psychiat Serv. 2000;51:216–222. doi: 10.1176/appi.ps.51.2.216. [DOI] [PubMed] [Google Scholar]
- 34.Sullivan G, Wells KB, Morgenstern H, Leake B. Issues in drug administration in a psychiatric rehabilitation unit. Int J Soc Psychiat. 1995;41:174–179. doi: 10.1177/002076409504100302. [DOI] [PubMed] [Google Scholar]
- 35.Nose M, Barbui C, Gray R, Tansella M. Clinical interventions for treatment non-adherence in psychosis: meta analysis. Br J Psychiat. 2003;183:197–206. doi: 10.1192/bjp.183.3.197. [DOI] [PubMed] [Google Scholar]
- 36.Paccaloni M, Pozzan T, Zimmerman C. Le informazioni ricevute e il coinvolgimento nella cura in psichiatria:cosa pensano i pazienti? Una revisione della letteratura [Being informed and involved in treatment: what do psychiatric patients think? A review] Epidemiol Psichiatr Soc. 2004;13:270–283. doi: 10.1017/s1121189x00001792. [DOI] [PubMed] [Google Scholar]
- 37.Bartko G, Herczeg I, Zador G. Clinical symptomatology and drug compliance in schizophrenic patients. Acta Psychiatr Scand. 1988;77:74–76. doi: 10.1111/j.1600-0447.1988.tb05080.x. [DOI] [PubMed] [Google Scholar]
- 38.Kampman O, Laippala P, Vaananen J, et al. Indicators of medication compliance in first-episode psychosis. Psychiatry Res. 2002;110:39–48. doi: 10.1016/s0165-1781(02)00030-6. [DOI] [PubMed] [Google Scholar]
- 39.Marder SR, Mebane A, Chien CP, Winslade WJ, Swann E, Van Putten T. A comparison of patients who refuse and consent to neuroleptic treatment. Am J Psychiat. 1983;140:470–472. doi: 10.1176/ajp.140.4.470. [DOI] [PubMed] [Google Scholar]
- 40.Nageotte C, Sullivan G, Duan N, Camp PL. Medication compliance among the seriously mentally ill in a public mental health system. Soc Psych Psych Epid. 1997;32:49–56. doi: 10.1007/BF00788920. [DOI] [PubMed] [Google Scholar]
- 41.Fleischhacker WW, Meise U, Gunther V, Kurz M. Compliance with antipsychotic drug treatment: Influence of side effects. Acta Psychiatr Scand. 1994;S89:11–15. [PubMed] [Google Scholar]
- 42.Weiden PJ, Shaw E, Mann J. Causes of neuroleptic noncompliance. Psychiatr Ann. 1986;16:571–575. [Google Scholar]
- 43.Mutsatsa SH, Joyce EM, Hutton SB, et al. Clinical correlates of early medication adherence: West London first episode schizophrenia study. Acta Psychiatr Scand. 2003;108:439–446. doi: 10.1046/j.0001-690x.2003.00193.x. [DOI] [PubMed] [Google Scholar]
- 44.Kampman O, Lehtinen K. Compliance in psychoses. Acta Psychiatr Scand. 1999;100:167–175. doi: 10.1111/j.1600-0447.1999.tb10842.x. [DOI] [PubMed] [Google Scholar]
- 45.Buchanan A. A two-year prospective study of treatment compliance in patients with schizophrenia. Psychol Med. 1992;22:787–797. doi: 10.1017/s0033291700038228. [DOI] [PubMed] [Google Scholar]
- 46.Linden M. Negative vs. positive therapy expectations and compliance vs. noncompliance. Psychiatr Prax. 1987;14:132–136. [PubMed] [Google Scholar]
- 47.Chan DW. Medication compliance in a Chinese psychiatric out-patient setting. Br J Med Psychol. 1984;57:81–89. doi: 10.1111/j.2044-8341.1984.tb01585.x. [DOI] [PubMed] [Google Scholar]
- 48.Becker MH, Maiman LA. Sociobehavioural determinants of compliance with health and medical care recommendations. Med Care. 1975;13:10–24. doi: 10.1097/00005650-197501000-00002. [DOI] [PubMed] [Google Scholar]
- 49.Turkington D, Kingdon D. Cognitive-behavioural techniques for general psychiatrists in the management of patients with psychoses. Br J Psychiatry. 2000;177:101–106. doi: 10.1192/bjp.177.2.101. [DOI] [PubMed] [Google Scholar]