Abstract
Psychiatric research, including the search for predisposing genes, has tended to proceed under the assumptions that schizophrenia and bipolar disorder, as defined in Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, and International Statistical Classification of Diseases, 10th Revision, are discrete disease entities with distinct etiology and pathogenesis and that these disease entities can be identified by current “operational” diagnostic conventions. However, recent findings emerging from genetic studies show increasing evidence for an overlap in genetic susceptibility across the traditional binary classification of psychosis. Moreover, the emerging evidence suggests the possibility of relatively specific relationships between genotype and psychopathology. For example, variation in Disrupted in Schizophrenia 1 (DISC1) and Neuregulin 1 (NRG1) may confer susceptibility to a form of illness with mixed features of schizophrenia and mania. The elucidation of genotype-phenotype relationships is at an early stage, but current findings highlight the need to consider alternative approaches to classification and conceptualization for psychiatric research rather than continuing to rely heavily on the traditional categorical approach. We can expect that, over the coming years, molecular genetics will catalyze a reappraisal of psychiatric nosology as well as contribute in a major way to our understanding of pathophysiology and to the development of improved treatments. However, our understanding of the brain mechanisms that link specific gene actions and products to the subjective experience of psychopathological symptoms is likely to be bridged by employing intermediate (or endo-) phenotypes in the domains such as cognition, neurophysiology, or neuroanatomy rather than relying upon clinical measures alone.
Keywords: schizophrenia, bipolar disorder, genetics, nosology, psychosis
Introduction
The majority of genetic studies into the psychoses over the last 2 decades have been predicated on the double assumption that (a) schizophrenia and bipolar disorder, as defined in Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV),1 and International Statistical Classification of Diseases, 10th Revision2, are discrete, “natural” disease entities with distinct etiology and pathogenesis and (b) these disease entities can be identified by current operational diagnostic conventions, which are based on reported subjective symptoms and, to a lesser extent, on deteriorating performance of expected social roles. Data from genetic epidemiology have been called upon to justify the validity of this approach, often referred to as the “Kraepelinian dichotomy.”
It is important to note that this widely held notion is incorrect. Kraepelin's seminal work, which aggregated 3 previously described syndromes—hebephrenia, catatonia, and paranoid dementia—into the clinical entity of dementia praecox and delimited the latter from manic-depressive insanity, paranoia, and late paraphrenia introduced order in the previously chaotic field of nosology and laid down the foundation for the current classifications of psychotic disorders. It is not widely known that, in contrast to the narrowly defined manic-depressive psychosis, Kraepelin's dementia praecox was a broad clinical grouping, consisting of 9 clinical “forms,” also including what today would be termed schizoaffective disorder and mood-incongruent affective psychoses. However, in 1920, he wrote that “we cannot distinguish satisfactorily between these two illnesses and this brings home the suspicion that our formulation of the problem may be incorrect … the affective and schizophrenic forms of mental disorder do not represent the expression of particular pathological processes, but rather indicate the areas of our personality in which these processes unfold.”3
Thus, in his later years, Kraepelin continued to develop and refine his ideas about psychiatric diagnoses, and his thinking had in many ways moved on from the dichotomous classification by the end of his life. However, it is not the goal of this article to consider Kraepelin's views in relation to modern nosological practice. A discussion of this sort, although of historical interest, is not of direct relevance. Unfortunately, the dichotomous, categorical view of the psychoses has been reified in the Diagnostic and Statistical Manual of Mental Disorders, Third Edition, formulation (and its consequent versions), and most of the genetic, and other, research into psychoses has been based solely on the “given” diagnostic categories of schizophrenia and bipolar disorder as the phenotypes, notwithstanding the fact that their validity has been challenged by emerging data from many fields of psychiatric research.4–6
In this article, we will first review the key pieces of evidence from genetic epidemiology that there is in fact a genetic overlap between the psychopathological entities that we currently refer to as bipolar disorder and schizophrenia. We will then review emerging evidence that the 2 diagnostic categories share specific susceptibility genes and that particular risk alleles may be associated with specific aspects of the phenotype.
Genetic Epidemiology
Family Studies
The great majority of family studies have shown increased risks for schizophrenia, schizoaffective disorder, and schizotypal personality disorder in the relatives of probands with schizophrenia.7 Family studies of bipolar disorder, on the other hand, have shown increased familial risks of bipolar disorder, schizoaffective disorder, and unipolar depression.8 In contrast, the majority of studies have failed to find a familial relationship between schizophrenia and bipolar disorder.9–14 Thus, the weight of evidence has traditionally been interpreted to support the view that schizophrenia and bipolar disorder largely breed true.
This conclusion has been challenged by family studies suggesting shared familial risk15,16 and by the observation that families exist in which some relatives have schizophrenia, some have bipolar disorder, and some have both psychosis and mood disorder.17 Moreover, the position of schizoaffective disorder has appeared somewhat anomalous in the context of a strict dichotomous view. Thus, schizoaffective disorder occurs at similarly increased rates both in families of probands with schizophrenia18 and in those of probands with bipolar disorder.19 Moreover, both schizophrenia and bipolar disorder have been shown to occur at increased rates in families of probands with schizoaffective disorder.19 This is supported by one of the largest family studies to date, which used the Swedish inpatient case register and obtained data on over 13 000 cases of schizophrenia and 5000 cases of bipolar disorder.20 The cross-disorder incidence ratios were robustly increased in siblings and half-siblings for both schizophrenia and bipolar disorder.
Twin Studies
Twin studies tend to be relatively small, given the difficulty in recruiting cases and the related arguments concerning their power can be made. In fact, the early, canonical twin study of Slater and Shields21 found that nearly as many of the co-twins of schizophrenic probands had affective disorder as had schizophrenia and that there were actually more parents with affective disorder than with schizophrenia. However, this, like other departures from the Kraepelinian model, was attributed to misdiagnosis.22 There have been few subsequent attempts to explore or challenge diagnostic boundaries using twin studies. An exception was the study by Farmer et al,23 who showed in a study of the first half of the Maudsley twin series that affective disorders, particularly those with mood-incongruent psychotic features, are genetically related to schizophrenia.
More recently, Cardno et al24 reasoned that overlap in genetic risk factors between schizophrenia and bipolar disorder might have been obscured in twin studies of psychosis because of the adoption of a hierarchical rule that requires that each individual be given a single lifetime diagnosis. Because schizophrenia was placed higher in terms of severity and “organicity,” schizophrenic symptoms tended to “trump” those of mood disorder. When Cardno et al24 defined syndromes nonhierarchically, they demonstrated a clear overlap in genetic liability between syndromically defined mania and schizophrenia.24 Their model fitting suggested that, whereas some susceptibility genes are specific to schizophrenia and some to bipolar disorder, there is a third group of genes, influencing across the board susceptibility to schizoaffective disorder, schizophrenia, and bipolar disorder. A graphic illustration of the varied expression of the same set of susceptibility genes is provided by the Maudsley triplets—a set of genetically identical triplets, 2 of whom had a lifetime diagnosis of schizophrenia and the third a lifetime diagnosis of bipolar disorder.25
Molecular Genetic Studies
Most molecular genetic studies of schizophrenia and bipolar disorder have been based upon the assumption that these constitute 2 independent disorders, with individual studies typically focusing on only one or the other disorder. Cases with a mix of mood and psychotic features, while common, have tended to be ignored or subsumed into some broader category of either schizophrenia or bipolar disorder.
Linkage Studies
Individual genetic linkage studies and meta-analyses have identified some chromosomal regions for which there is evidence of linkage in both schizophrenia and bipolar disorder. These include regions of 13q, 22q, 18,26,27 and 6q.28 The chromosomal regions implicated are wide and contain many genes, so it is not certain that the apparent overlaps reflect the existence of shared genes between the 2 disorders. We should also remember that it remains possible that any given linkage might be a false positive in at least one of the disorders.
However, the hypothesis that loci exist that influence susceptibility across the schizophrenia-bipolar divide has recently received further support from a genome-wide linkage scan using families selected on the basis of a member with DSM-IV schizoaffective disorder, bipolar type. This study demonstrated genome-wide significant linkage at 1q42 and suggestive linkage at 22q11, with evidence for linkage being contributed equally by “schizophrenia” families (ie, those where other members had predominantly schizophrenia) and “bipolar” families (ie, those where other members had predominantly bipolar disorder).29 It is of interest that 2 genes which have been implicated in schizophrenia, DISC1 and catechol-O-methyltransferase (COMT), map to 1q42 and 22q11, respectively, and this raises the question of whether either or both of these genes predispose to illness across the schizophrenia-bipolar divide. There is evidence to support this for both COMT30 and DISC1 (see below).
Studies of Individual Genes
Linkage studies can provide at best indirect evidence for shared genetic effects. More direct evidence has come from reports implicating variation in the same genes as influencing susceptibility to both schizophrenia and bipolar disorder. In most cases, the gene was first implicated in studies of schizophrenia, and the evidence in most cases is strongest for this phenotype. This could reflect the true contribution to the phenotype or may simply reflect the fact that substantially greater resources and samples have been used to date on studies of schizophrenia. We will consider the evidence for each gene in turn.
NRG1
NRG1 was first implicated in schizophrenia in the Icelandic population after a systematic study of 8p21-22 revealed association between schizophrenia and a multimarker haplotype at the 5′ end of NRG1.31 Strong evidence for association with the same haplotype, known as HAPICE, was subsequently found in a large sample from Scotland,32 with further support coming from our own UK sample.33 These and subsequent studies of NRG1 in schizophrenia have been reviewed recently.34 Overall, there is strong evidence from several studies that genetic variation in NRG1 confers risk to schizophrenia, but not all studies have found the same haplotype to be associated and, as yet, specific susceptibility and protective variants have not been identified. NRG1 has not yet been extensively studied in bipolar disorder. However, in the only published study to date, we found significant evidence for association of HAPICE with susceptibility to bipolar disorder of a similar magnitude to that seen by us in schizophrenia (OR = 1.3).35 In the bipolar cases with predominantly mood-incongruent psychotic features, the effect was greater (OR = 1.7), as was the case in the subset of schizophrenia patients who had experienced mania (OR = 1.6). Pending replication, these findings should be treated with caution, but they suggest that NRG1 plays a role in influencing susceptibility to both bipolar disorder and schizophrenia and that it may exert a specific effect in the subset of functional psychoses characterized by both manic and mood-incongruent psychotic features.
Dysbindin
Evidence implicating dystrobrevin-binding protein 1 (DTNBP1), also known as dysbindin, in schizophrenia was first reported by Straub et al,36 and there is now quite impressive support from a number of studies reviewed recently.37 However, once again various markers and haplotypes have been associated, and the actual susceptibility variants have yet to be identified. Raybould and colleagues38 reported the first study of single-nucleotide polymorphisms (SNPs) from dysbindin in bipolar disorder. They found no significant associations in bipolar disorder as a whole but found modestly significant evidence for association in a subset of bipolar cases with predominantly psychotic episodes. This finding suggests that variation in dysbindin confers risk to some aspect of the psychotic syndrome rather than to the DSM-IV schizophrenia phenotype per se, although replication is required. More recently, Breen et al39 reported evidence for association with dysbidin SNPs in a small sample of bipolar patients, though no analyses stratified by phenotype were conducted. Recent work in the Irish Study of High-Density Schizophrenia Families has shown that schizophrenic patients with negative symptoms were more likely to inherit the dysbindin risk haplotype,40 raising the possibility that negative symptoms might also be part of the clinical presentation of the subgroup of psychotic bipolar cases that are particularly likely to carry the dysbindin risk haplotype.
G72 (DAOA)/G30
This locus was first implicated in studies of schizophrenia by Chumakov and colleagues41 who undertook association mapping in the linkage region on chromosome 13q22-34. They found associations in French Canadian and Russian populations in markers around 2 novel, putative genes, G72 and G30, which are overlapping but transcribed in opposite directions. Both G72 and G30 are apparently transcribed in brain, but in vitro translation experiments only resulted in production of protein for G72. Yeast 2-hybrid analysis of experimentally produced protein provided evidence for physical interaction between G72 and D-amino acid oxidase (DAO). DAO is expressed in human brain where it oxidizes D-serine, a potent activator of N-methyl-D-aspartate glutamate receptor. Coincubation of G72 and DAO in vitro revealed a functional interaction with G72 enhancing the activity of DAO. Consequently, G72 has now been named D-amino acid oxidase activator (DAOA). However, it should be noted that the existence of native G72 protein has not been demonstrated and there have been, as yet, no reports replicating the physical interaction with DAO. Associations between schizophrenia and markers in and around DAOA have subsequently been reported by a number of groups and supported by recent meta-analysis,42 although once again there is no consensus concerning the specific risk alleles or haplotypes across studies. Moreover, unlike NRG1 and DTNBP1, this locus has been quite extensively studied in bipolar disorder, for which it is now arguably the best-supported locus. Support for association with bipolar disorder has been reported from at least 5 independent datasets, and, as for schizophrenia, the presence of association is supported by meta-analysis without clear implication of specific alleles or haplotypes.42 No pathologically relevant variant has yet been identified, and the biological mechanism remains to be elucidated.
The largest study to date, and the only one which has attempted to tag all common genetic variation at this locus, was published after the meta-analysis of Detera-Wadleigh and McMahon42 was completed. This included 2831 individuals of whom 709 had DSM-IV schizophrenia, 706 had bipolar I disorder, and 1416 were ethnically matched controls.43 The authors identified significant association with bipolar disorder but failed to find association with schizophrenia. Analyses across the traditional diagnostic categories revealed significant evidence for association in the subset of cases (n = 818) in which episodes of major mood disorder had occurred. A similar pattern of association was observed in both bipolar cases and schizophrenia cases in which individuals had experienced major mood disorder. In contrast, there was no evidence for association in the subset of cases (n = 1153) in which psychotic features occurred. This finding requires replication, but the data as they stand suggest that, despite being originally reported as a schizophrenia susceptibility locus, variation in DAOA/G30 does not primarily increase susceptibility for prototypical schizophrenia or psychosis. Instead, it appears that variation in DAOA/G30 influences susceptibility to episodes of mood disorder across the traditional bipolar and schizophrenia categories. Importantly, these findings also imply that whether or not significant associations are seen in schizophrenia will depend upon the proportion of cases that have suffered from episodes of mood disorder and remind us of the potential importance of sample differences in determining the reproducibility of genetic association studies.
Disrupted in Schizophrenia 1
This gene was implicated through studies of an extended pedigree in which a balanced chromosomal translocation (1;11)(q42;q14.3) showed strong evidence for linkage to a fairly broad phenotype comprising schizophrenia, bipolar disorder, and recurrent depression.44 The translocation was found to disrupt 2 genes on chromosome 1: DISC1 and DISC2.44,45 DISC2 contains no open reading frame and may regulate DISC1 expression via antisense RNA.45 A small pedigree has recently been reported in which a 4-bp deletion in exon 12 of DISC1 cosegregates with schizophrenia and schizoaffective disorder,46 although independent evidence suggests that the deletion is unlikely to be a highly penetrant risk allele for psychosis.47 Interestingly, DISC1 and DISC2 are located close to the chromosome 1 markers implicated in 2 Finnish linkage studies of schizophrenia.48,49 The Edinburgh group which identified DISC1 found no linkage evidence in their own schizophrenia sample but did find suggestive evidence for linkage in bipolar disorder.50 More recently, Hamshere and colleagues29 reported genome-wide significant evidence for linkage at this locus in a linkage study of schizoaffective disorder, bipolar type. DISC1 is certainly an interesting candidate gene for mental disorder, but it is important to remember that translocations exert effects on genes other than those directly disrupted. For example, there are several mechanisms by which a translocation can influence the expression of neighboring genes. In order to unequivocally implicate DISC1 and/or DISC2 in the pathogenesis of psychosis, it is necessary to identify mutations or polymorphisms that are associated with psychosis in nondeleted cases and are not in linkage disequilibrium with neighboring genes. Negative studies in schizophrenia samples were initially reported by the Edinburgh group with a small number of markers51 and by a group who focused on the 5′ end of the gene in a large Japanese sample.52 More recently, several groups have reported positive findings,53–56 although in no case are the results compelling and there is little agreement as to the specific markers or haplotypes showing association. Interestingly, in 3 of these studies, associations were observed with bipolar disorder as well as schizophrenia,53–55 and in one the strongest association was observed with schizoaffective disorder.54
While no consistent pattern of association has yet emerged and no pathogenically relevant variants have been established, the convergence of the linkage data is strongly suggestive that variation in DISC1 or another gene in this region influences susceptibility to mood-psychosis phenotypes that cut across the traditional Kraepelinian divide.
Conclusions
Genetic epidemiological data are beginning to favor the view that schizophrenia, bipolar disorder, and schizoaffective disorders share at least some genetic liability, although more work aimed at exploring these issues in adequately powered and suitably designed family and twin studies is clearly needed. Recent work on specific candidate genes supports this view and suggests that the genetic associations are strongest with clinical syndromes that do not map directly onto either or both of the 2 hypothetical disease entities proposed by Kraepelin. This is not surprising, given the frequency with which clinicians encounter mixed forms and the absence of a clear demarcation or “zone of rarity” between the 2 syndromes.57 It also seems congruent with the evidence that schizophrenia and bipolar disorder share a range of other risk factors.6 Moreover, general medicine provides multiple examples of genetically complex disorders where distinct diagnostic categories (eg hypertension, hemorrhagic stroke, myocardial infarction, and hypertensive cardiomyopathy) share genetic risk factors.58
The comparative work on candidate genes in the major psychiatric disorders is still in its early stages and the findings should be treated with caution until further studies have been reported, given the difficulties in establishing unequivocal evidence for genetic association in complex diseases and the fact that for none of the genes implicated have specific risk variants so far been established. Indeed, it may turn out that many of the candidate genes currently discussed contain multiple risk (and protective) variants with effects on different aspects of psychopathology. A more parsimonious interpretation of the existing data is that variation in DISC1/DISC 2 and NRG1 can confer predisposition to illness in individuals on either side of the Kraepelinian divide and that the effects of both genes will be felt most strongly in disorders with features of both schizophrenia and bipolar disorder. Variation in DTNBP1 seems to predominantly predispose to schizophrenia and negative symptoms, with an effect on bipolar disorder confined to those cases with prominent psychotic features. In contrast, DAOA/G30 appears to be more strongly associated with mood disorder, and the extent to which associations with schizophrenia are seen may depend upon the proportion of cases with prominent mood disorder features.
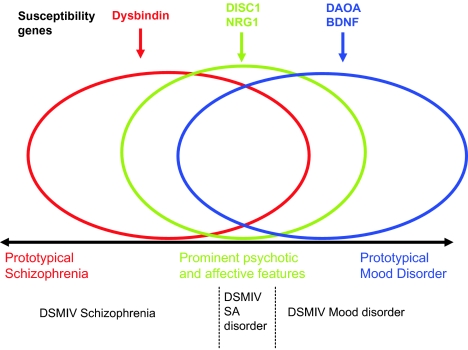
Such findings will have important implications for future classifications of the major psychiatric disorders because they suggest an overlap in the biological basis of disorders that have, over the last 100 years, been regarded as distinct entities.4 We predict that, over the coming years, molecular genetics will catalyze a reappraisal of psychiatric nosology as well as contribute in a major way to our understanding of the pathophysiology and the development of improved treatments. Current genetic findings suggest that rather than classifying psychosis as a dichotomy, a more useful formulation may be to conceptualize alternative categories or a spectrum of clinical phenotypes with susceptibility conferred by overlapping sets of genes4 (figure 1).
Fig. 1.
Simplified hypothesized relationship between specific susceptibility genes (above the black line) and clinical phenotype (below the line) using the model outlined in Craddock and Owen4. The overlapping ellipses represent overlapping sets of genes: red influencing susceptibility to phenotypes with prominent schizophrenia-like features, blue to prominent mood features, and green to phenotypes with a prominent mix of both types of feature. These assignments are based on current data and are likely to require revision as more data accumulate.
For the time being, however, such interpretations remain largely speculative as our understanding of the brain mechanisms linking specific gene actions and products to the subjective experience of psychopathological symptoms, such as delusions, hallucinations, or thought disorder is at best rudimentary. There is an “explanatory gap” between the findings of statistical association of a gene variant with the disorder and the demonstration of causality with regard to specific illness phenomena. This gap might be easier to bridge by employing intermediate (or endo-) phenotypes in the domains of cognition, neurophysiology, or neuroanatomy. As objectively measurable quantitative traits, endophenotypes are better anchored in brain biology than clinical symptoms and can help delineate subtypes of disorder with likely distinct genetic basis.59,60 The dissection of the syndromes of psychosis into “modular” endophenotypes with specific neurocognitive or neurophysiological underpinnings, cutting across the conventional diagnostic boundaries, is beginning to be perceived as a promising approach in the genetics of the major psychiatric disorders.61
It is important that researchers are willing to embrace and explore such alternative approaches to the phenotype of psychosis in order to interpret the accumulating data and design new research. This will be an iterative process with identified genetic signals allowing refinement of the phenotype and the refined phenotype allowing increased power to detect further genetic signals. To facilitate this approach, it will be important to collect large samples that have a full representation of phenotypes across the mood-psychosis spectrum and detailed, high-quality phenotypic assessments, preferably including dimensional measures (eg, Levinson et al62, Craddock et al63).
In conclusion, accumulating evidence supports the existence of an overlap in genetic susceptibility across the traditional Kraepelinian divide with studies of several genes providing to date the most compelling such evidence. This work is at an early stage but has the potential to change our conception of psychiatric nosology as well as our understanding of the pathogenesis of psychopathology.
Acknowledgments
Owen's and Craddock's work on the genetics of psychosis and mood disorders is funded through grants from the Wellcome Trust and the Medical Research Council. Jablensky's work on the genetics of cognitive deficit in schizophrenia is funded by the National Health and Medical Research Council of Australia. The authors are indebted to all the participants in our studies.
References
- 1.American Psychiatric Association. 4th ed text revised. Washington, DC: American Psychiatric Press; 1994. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 2.WHO. Geneva, Ill: World Health Organization; 1993. The ICD10 Classification of Mental and Behavioural Disorders. Diagnostic Criteria for Research. [Google Scholar]
- 3.Kraepelin E. Patterns of mental disorders. In: Hirsch SR, editor. Themes and Variations in European Psychiatry. Bristol, England: John Wright & Sons; 1974. pp. 7–30. [Google Scholar]
- 4.Craddock N. The beginning of the end for the Kraepelinian dichotomy. Br J Psychiatry. 2005;186:364–366. doi: 10.1192/bjp.186.5.364. [DOI] [PubMed] [Google Scholar]
- 5.Van Os J, et al. A comparison of the utility of dimensional and categorical representations of psychosis. UK700 group. Psychol Med. 1999;29:595–606. doi: 10.1017/s0033291798008162. [DOI] [PubMed] [Google Scholar]
- 6.Murray RM. A developmental model for similarities and dissimilarities between schizophrenia and bipolar disorder. Schizophr Res. 2004;71:405–416. doi: 10.1016/j.schres.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 7.Gottesman II. Schizophrenia Genesis: The Origins of Madness. New York, NY: Freeman; 1991. [Google Scholar]
- 8.Tsuang MT. The Genetics of Mood Disorders. Baltimore, Md: The Johns Hopkins University Press; 1990. [Google Scholar]
- 9.Baron M, et al. Schizoaffective illness, schizophrenia and affective disorders: morbidity risk and genetic transmission. Acta Psychiatr Scand. 1982;65:253–262. doi: 10.1111/j.1600-0447.1982.tb00845.x. [DOI] [PubMed] [Google Scholar]
- 10.Gershon ES, et al. A family study of schizoaffective, bipolar I, bipolar II, unipolar, and normal control probands. Arch Gen Psychiatry. 1982;39:1157–1167. doi: 10.1001/archpsyc.1982.04290100031006. [DOI] [PubMed] [Google Scholar]
- 11.Frangos E, et al. Prevalence of DSM III schizophrenia among the first-degree relatives of schizophrenic probands. Acta Psychiatr Scand. 1985;72:382–386. doi: 10.1111/j.1600-0447.1985.tb02625.x. [DOI] [PubMed] [Google Scholar]
- 12.Gershon ES. A controlled family study of chronic psychoses: schizophrenia and schizoaffective disorder. Arch Gen Psychiatry. 1988;45:328–336. doi: 10.1001/archpsyc.1988.01800280038006. [DOI] [PubMed] [Google Scholar]
- 13.Kendler KS, et al. The Roscommon family study: affective-illness, anxiety disorder, andalcoholism in relatives. Arch Gen Psychiatry. 1993;50:952–960. doi: 10.1001/archpsyc.1993.01820240036005. [DOI] [PubMed] [Google Scholar]
- 14.Maier W, et al. Continuity and discontinuity of affective-disorders and schizophrenia: results of a controlled family study. Arch Gen Psychiatry. 1993;50:871–883. doi: 10.1001/archpsyc.1993.01820230041004. [DOI] [PubMed] [Google Scholar]
- 15.Tsuang MT. Morbidity risks of schizophrenia and affective disorders among first degree relatives of patients with schizophrenia, mania, depression and surgical conditions. Br J Psychiatry. 1980;137:497–504. doi: 10.1192/bjp.137.6.497. [DOI] [PubMed] [Google Scholar]
- 16.Valles V, et al. Increased morbid risk for schizophrenia in families of in-patients with bipolar illness. Schizophr Res. 2000;42:83–90. doi: 10.1016/s0920-9964(99)00117-6. [DOI] [PubMed] [Google Scholar]
- 17.Pope HG., Jr Schizophrenic individuals with bipolar first-degree relatives: analysis of two pedigrees. J Clin Psychiatry. 1990;51:97–101. [PubMed] [Google Scholar]
- 18.Kendler KS. The structure of psychosis: latent class analysis of probands from the Roscommon family study. Arch Gen Psychiatry. 1998;55:492–499. doi: 10.1001/archpsyc.55.6.492. [DOI] [PubMed] [Google Scholar]
- 19.Rice J, et al. The familial transmission of bipolar illness. Arch Gen Psychiatry. 1987;44:441–447. doi: 10.1001/archpsyc.1987.01800170063009. [DOI] [PubMed] [Google Scholar]
- 20.Ősby U. The risk for schizophrenia and bipolar disorder in siblings to probands with schizophrenia and bipolar disorder. Am J Med Genet. 2001;105:O56. [Google Scholar]
- 21.Slater E. Psychotic and Neurotic Illnesses in Twins. Medical Research Council Special Report 278. London, England: Her Majesty's Stationery Office; 1953. [PubMed] [Google Scholar]
- 22.Slater E. The Genetics of Mental Disorders. London, England: Oxford University Press; 1971. [Google Scholar]
- 23.Farmer AE. Twin concordance for DSM-III schizophrenia: scrutinizing the validity of the definition. Arch Gen Psychiatry. 1987;44:634–641. doi: 10.1001/archpsyc.1987.01800190054009. [DOI] [PubMed] [Google Scholar]
- 24.Cardno AG, et al. A twin study of genetic relationships between psychotic symptoms. Am J Psychiatry. 2002;159:539–545. doi: 10.1176/appi.ajp.159.4.539. [DOI] [PubMed] [Google Scholar]
- 25.McGuffin P. Identical triplets: non-identical psychosis? Br J Psychiatry. 1982;140:1–6. doi: 10.1192/bjp.140.1.1. [DOI] [PubMed] [Google Scholar]
- 26.Badner JA. Meta-analysis of whole-genome linkage scans of bipolar disorder and schizophrenia. Mol Psychiatry. 2002;7:405–411. doi: 10.1038/sj.mp.4001012. [DOI] [PubMed] [Google Scholar]
- 27.Berrettini W. Evidence for shared susceptibility in bipolar disorder and schizophrenia. Am J Med Genet. 2003;123C:59–64. doi: 10.1002/ajmg.c.20014. [DOI] [PubMed] [Google Scholar]
- 28.Craddock N. The genetics of schizophrenia and bipolar disorder: dissecting psychosis. J Med Genet. 2005;42:193–204. doi: 10.1136/jmg.2005.030718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hamshere ML, et al. Genome-wide linkage scan in schizoaffective disorder: significant evidence for linkage (LOD = 3.54) at 1q42 close to DISC1, and suggestive evidence at 22q11 and 19q13. Arch Gen Psychiatry. 2005;62:1081–1088. doi: 10.1001/archpsyc.62.10.1081. [DOI] [PubMed] [Google Scholar]
- 30.Craddock N. The catechol-O-methyltransferase gene (COMT) as a candidate for psychiatric phenotypes: evidence and lessons. Mol Psychiatry. 2006;11:446–458. doi: 10.1038/sj.mp.4001808. [DOI] [PubMed] [Google Scholar]
- 31.Stefansson H, et al. Neuregulin 1 and susceptibility to schizophrenia. Am J Hum Genet. 2002;71:877–892. doi: 10.1086/342734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stefansson H, et al. Association of neuregulin 1 with schizophrenia confirmed in a Scottish population. Am J Hum Genet. 2003;72:83–87. doi: 10.1086/345442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Williams NM, et al. A systematic genomewide linkage study in 353 sib pairs with schizophrenia. Am J Hum Genet. 2003;73:1355–1367. doi: 10.1086/380206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tosato S. Association between the neuregulin 1 gene and schizophrenia: a systematic review. Schizophr Bull. 2005;31:613–617. doi: 10.1093/schbul/sbi043. [DOI] [PubMed] [Google Scholar]
- 35.Green E, et al. The operation of the schizophrenia susceptibility gene, neuregulin 1 (NRG1) across traditional diagnostic boundaries to increase risk for bipolar disorder. Arch Gen Psychiatry. 2005;62:642–648. doi: 10.1001/archpsyc.62.6.642. [DOI] [PubMed] [Google Scholar]
- 36.Straub RE, et al. Genetic variation in the 6p22.3 gene DTNBP1, the human ortholog of the mouse dysbindin gene, is associated with schizophrenia. Am J Hum Genet. 2002;71:337–348. doi: 10.1086/341750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Williams NM. Is the dysbindin gene (DTNBP1) a susceptibility gene for schizophrenia? Schizophr Bull. 2005;31:800–805. doi: 10.1093/schbul/sbi061. [DOI] [PubMed] [Google Scholar]
- 38.Raybould R, et al. Bipolar disorder and polymorphisms in the dysbindin (dystrobrevin binding protein 1) gene (DTNBP1) Biol Psychiatry. 2005;57:696–701. doi: 10.1016/j.biopsych.2005.01.018. [DOI] [PubMed] [Google Scholar]
- 39.Breen G, et al. Association of the dysbindin gene with bipolar affective disorder. Am J Psychiatry. 2006;163:1636–1638. doi: 10.1176/ajp.2006.163.9.1636. [DOI] [PubMed] [Google Scholar]
- 40.Fanous AH, et al. Relationship between a high-risk haplotype in the DTNBP1 (dysbindin) gene and clinical features of schizophrenia. Am J Psychiatry. 2005;162:1824–1832. doi: 10.1176/appi.ajp.162.10.1824. [DOI] [PubMed] [Google Scholar]
- 41.Chumakov I, et al. Genetic and physiological data implicating the new human gene G72 and the gene for D-amino acid oxidase in schizophrenia. Proc Natl Acad Sci USA. 2002;99:13675–13680. doi: 10.1073/pnas.182412499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Detera-Wadleigh SD. G72/G30 in schizophrenia and bipolar disorder: review and meta-analysis. Biol Psychiatry. 2006;60:106–114. doi: 10.1016/j.biopsych.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 43.Williams NM, et al. Variation at the DAOA/G30 locus influences susceptibility to major mood episodes but not psychosis in schizophrenia and bipolar disorder. Arch Gen Psychiatry. 2006;63:366–373. doi: 10.1001/archpsyc.63.4.366. [DOI] [PubMed] [Google Scholar]
- 44.Blackwood DH, et al. Schizophrenia and affective disorders—cosegregation with a translocation at chromosome 1q42 that directly disrupts brain-expressed genes: clinical and P300 findings in a family. Am J Hum Genet. 2001;69:428–433. doi: 10.1086/321969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Millar JK, et al. Disruption of two novel genes by a translocation co-segregating with schizophrenia. Hum Mol Genet. 2000;9:1415–1423. doi: 10.1093/hmg/9.9.1415. [DOI] [PubMed] [Google Scholar]
- 46.Sachs NA. A frameshift mutation in Disrupted in Schizophrenia 1 in an American family with schizophrenia and schizoaffective disorder. Mol Psychiatry. 2005;10:758–764. doi: 10.1038/sj.mp.4001667. [DOI] [PubMed] [Google Scholar]
- 47.Green E, et al. Evidence that a DISC1 frame-shift deletion associated with psychosis in a single family may not be a pathogenic mutation. Mol Psychiatry. 2006;11:798–799. doi: 10.1038/sj.mp.4001853. [DOI] [PubMed] [Google Scholar]
- 48.Ekelund J, et al. Chromosome 1 loci in Finnish schizophrenia families. Hum Mol Genet. 2001;10:1611–1617. doi: 10.1093/hmg/10.15.1611. [DOI] [PubMed] [Google Scholar]
- 49.Ekelund J, et al. Replication of 1q42 linkage in Finnish schizophrenia pedigrees. Mol Psychiatry. 2004;9:1037–1041. doi: 10.1038/sj.mp.4001536. [DOI] [PubMed] [Google Scholar]
- 50.Macgregor S, et al. A genome scan and follow-up study identify a bipolar disorder susceptibility locus on chromosome 1q42. Mol Psychiatry. 2004;9:1083–1090. doi: 10.1038/sj.mp.4001544. [DOI] [PubMed] [Google Scholar]
- 51.Devon RS, et al. Identification of polymorphisms within Disrupted in Schizophrenia 1 and Disrupted in Schizophrenia 2, and an investigation of their association with schizophrenia and bipolar disorder. Psychiatr Genet. 2002;11:71–78. doi: 10.1097/00041444-200106000-00003. [DOI] [PubMed] [Google Scholar]
- 52.Kockelkorn TT, et al. Association study of polymorphisms in the 5′ upstream region of human DISC1 gene with schizophrenia. Neurosci Lett. 2004;368:41–45. doi: 10.1016/j.neulet.2004.06.048. [DOI] [PubMed] [Google Scholar]
- 53.Hennah W, et al. Haplotype transmission analysis provides evidence of association for DISC1 to schizophrenia and suggests sex-dependent effects. Hum Mol Genet. 2003;12:3151–3159. doi: 10.1093/hmg/ddg341. [DOI] [PubMed] [Google Scholar]
- 54.Hodgkinson CA, et al. Disrupted in schizophrenia 1 (DISC1): association with schizophrenia, schizoaffective disorder, and bipolar disorder. Am J Hum Genet. 2004;75:862–872. doi: 10.1086/425586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thomson PA, et al. Association between the TRAX/DISC locus and both bipolar disorder and schizophrenia in the Scottish population. Mol Psychiatry. 2005;10:657–668. doi: 10.1038/sj.mp.4001669. 616. [DOI] [PubMed] [Google Scholar]
- 56.Callicott JH, et al. Variation in DISC1 affects hippocampal structure and function and increases risk for schizophrenia. Proc Natl Acad Sci USA. 2005;102:8627–8632. doi: 10.1073/pnas.0500515102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kendell R. Distinguishing between the validity and utility of psychiatric diagnoses. Am J Psychiatry. 2003;160:4–12. doi: 10.1176/appi.ajp.160.1.4. [DOI] [PubMed] [Google Scholar]
- 58.Kendler KS. Reflections on the relationship between psychiatric genetics and psychiatric nosology. Am J Psychiatry. 2006;163:1138–1146. doi: 10.1176/ajp.2006.163.7.1138. [DOI] [PubMed] [Google Scholar]
- 59.Hallmayer JF, et al. Genetic evidence for a distinct subtype of schizophrenia characterized by pervasive cognitive deficit. Am J Hum Genet. 2005;77:468–476. doi: 10.1086/432816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jablensky A. Subtyping schizophrenia: implications for genetic research. Mol Psychiatry. 2006;11:815–836. doi: 10.1038/sj.mp.4001857. [DOI] [PubMed] [Google Scholar]
- 61.Harrison PJ. Genes for schizophrenia? Recent findings and their pathophysiological implications. Lancet. 2003;361:417–419. doi: 10.1016/S0140-6736(03)12379-3. [DOI] [PubMed] [Google Scholar]
- 62.Levinson DF. The Lifetime Dimensions of Psychosis Scale (LDPS): description and interrater reliability. Schizophr Bull. 2002;28:683–695. doi: 10.1093/oxfordjournals.schbul.a006972. [DOI] [PubMed] [Google Scholar]
- 63.Craddock N, et al. The Bipolar Affective Disorder Dimension Scale (BADDS)—a dimensional scale for rating lifetime psychopathology in bipolar spectrum disorders. BMC Psychiatry. 2004;4:19. doi: 10.1186/1471-244X-4-19. [DOI] [PMC free article] [PubMed] [Google Scholar]