Abstract
The purpose of this study was to assess how neurocognition and social cognition were associated with initial functional level and with rates of functional change in intensive community-based psychosocial rehabilitation interventions that have been shown to yield significant functional change for individuals diagnosed with schizophrenia. We also examined how service intensity was associated with rates of change and whether it served as a moderator of the relationship between functional change and both neurocognition and social cognition. The sample consisted of 125 individuals diagnosed with schizophrenia or schizoaffective disorder who were recruited upon admission to 1 of 4 community-based psychosocial rehabilitation facilities and were followed prospectively for 12 months. One hundred and two subjects completed the 12-month protocol. The findings suggested that (i) the initial level of psychosocial functioning was related to both social cognition and neurocognition at baseline, (ii) when significant rehabilitative change occurs, higher neurocognition and social cognition scores at baseline predicted higher rates of functional change over the subsequent 12 months, (iii) greater service intensity was related to higher rates of improvement in functional outcome over time, and (iv) service intensity moderated the relationship between neurocognition and initial functional level and moderated the relationship between social cognition and the rates of functional change at a trend level. These findings have relevance to our understanding of the heterogeneity in functional rehabilitative outcomes, to our understanding of the conditions of rehabilitative change and for the design of psychosocial interventions in the community.
Keywords: social cognition, neurocognition, schizophrenia, rehabilitation, outcome
Introduction
Many community-based rehabilitation programs for individuals with schizophrenia have developed intensive services designed to support and maintain changes in community functioning. 1–4 While findings from controlled effectiveness studies have led to optimism that we can develop community-based psychosocial interventions to improve the lives of individuals with schizophrenia, the most consistent success from these intervention models has been in the clinical outcomes of reducing relapse and hospitalization, as well as related improvements in housing stability.2,3,5–7 Rehabilitative success in other major psychosocial functioning areas such as social, vocational, and independent living domains has been limited in several ways. First, the functional changes do not consistently occur; second, there is wide individual variation and heterogeneity in rehabilitation outcomes from even effective programs; and third, most functional gains do not last when the intervention ends.2–14 Given our modest success in establishing and maintaining functional outcomes from community-based psychosocial rehabilitation services, it has been argued that we must increase our knowledge about individual responsiveness to psychosocial rehabilitation as well as the factors that underlay this heterogeneity in outcomes.2,6,15,16
In this regard, recent research has found a relationship between neurocognition and functional outcomes for individuals diagnosed with schizophrenia in both cross-sectional and longitudinal studies.17–19 Neurocognitive capacities, such as episodic memory, secondary/working memory, vigilance, and executive functioning in particular, have been related to social and work aspects of community functioning and to social skill acquisition in inpatient rehabilitation interventions. The findings are reasonably consistent in showing that neurocognition is a rate-limiting factor for functional change. One recent study20 also found that neurocognition was related to outpatient service use and suggested that service use might moderate the impact of neurocognition on functional outcomes. This moderation would be indicated by a change in the relationship between neurocognition and functional outcome contingent on different levels of service intensity.
Another underlying construct, social cognition, has recently emerged as a focus of interest in studying functional outcomes in schizophrenia.21–23 It has been shown to have both direct and indirect impact on cross-sectional and prospective functional outcomes.19,24 Its utility as a target for intervention has also been recently addressed.25 While its relationship to neurocognition is not yet fully understood, social cognition appears to be empirically linked to neurocognition, and it is emerging as an important factor in the understanding of functional outcome.
There are, however, some notable limitations in this literature. First, most of the research on neurocognition and responsiveness to psychosocial interventions has been done in inpatient settings.21 The generalization of this knowledge to community-based rehabilitation settings is needed as this is where most rehabilitation services are delivered. Second, a small number of studies have shown that posttreatment vocational success was correlated with baseline measures of neurocognition,26,27 but no studies have examined neurocognitive variables as predictors of the rate of functional rehabilitative change during community-based treatment. Third, social cognition has not been examined as a predictor of responsiveness to rehabilitative interventions. Therefore, missing from this literature is an examination of how social cognition and neurocognition contribute to change during intensive community-based psychosocial rehabilitation interventions that are designed to enhance functional outcomes in the community.
Fourth, given that the character of services (such as service intensity) has been related to functional rehabilitative outcomes, 28,29 there also needs to be an examination of whether service intensity influences the relationships between neurocognition, social cognition, and functional outcome so that the mechanisms and conditions of rehabilitative change can be better understood. For example, when significant rehabilitative change occurs, higher service intensity could mask the relationship between neurocognition and functional change, thus suggesting that rehabilitation services “work against” or neutralize the impact of neurocognitive deficits on functional outcome. On the other hand, higher service intensity could be associated with a stronger relationship between neurocognition and functional change, suggesting a mechanism whereby rehabilitation services potentiate or “work with” neurocognitive capacity to improve functional outcome. The moderating influences of service intensity could also apply to the relationship between social cognition and functional outcomes.
The purpose of this study was to assess how neurocognition and social cognition were associated with initial functional level and with rates of functional change in intensive community-based psychosocial rehabilitation interventions that have been shown to yield significant functional change for individuals diagnosed with schizophrenia. We also examined how service intensity was associated with rates of change and whether it served as a moderator of the relationship between functional change and both neurocognition and social cognition.
The following hypotheses were tested on a sample of individuals diagnosed in the schizophrenia spectrum, who were beginning intensive community-based psychosocial rehabilitation. (1) Better neurocognition and social cognition scores at baseline will be significantly associated with higher levels of initial functional status. (2) Better neurocognition and social cognition scores at baseline will be associated with higher rates of functional rehabilitative change over 12 months. (3) Higher service intensity will be related to higher rates of functional rehabilitative change. (4) Service intensity will moderate the relationship between both neurocognition and social cognition and subsequent functional change, with 2 competing types of moderation proposed: (a) a compensatory moderation where higher service intensity will be associated with a weaker relationship between baseline neurocognition, social cognition, and subsequent functional outcome or (b) a potentiating moderation where higher service intensity will be associated with a stronger relationship between baseline neurocognition, social cognition, and subsequent functional outcome.
Method
Participants in this study were recruited as they were admitted to 4 community-based psychosocial rehabilitation programs in urban Los Angeles. The programs were part of a county mandated mental health initiative and were designed to provide integrated and comprehensive rehabilitative services.30 The services provided included mental health treatment, housing services, social and vocational rehabilitation, substance abuse treatment, and 24-h crisis response. Sites were also selected on the basis of data showing that they were comprehensive service environments that yielded significant improvements in functional outcomes over time.19,28,31 Participants were assessed at baseline on all study variables and again 6 and 12 months later on the functional outcome variables. At baseline, psychosocial and functional status data were generally gathered within 2 weeks of the neuropsychological and social cognition testing. The psychosocial interviews were completed by trained research interviewers who were blind to the neuropsychological results. Neuropsychological testers were blind to the scores on the psychosocial measures.
Subjects
The sample consisted of 125 individuals diagnosed with schizophrenia or schizoaffective disorder who completed baseline test batteries including neurocognition, social cognition, and psychosocial functioning. Subjects were recruited and followed prospectively for 12 months from 1996 to 2000. Fifty-six percent of the subjects came from site 1, 16% from site 2, 16% from site 3, and 12% from site 4. Diagnoses were determined using clinical records, a Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition checklist, and collateral reports from the admitting clinician and on-site psychiatrist. Subjects were excluded if they met the criteria for alcohol or drug dependence in the previous 6 months or if they had an identified neurological disorder. One hundred and two subjects completed the 12-month protocol on the study variables (82% completion rate at 12 months). There was no statistically significant differential attrition across the program sites.
Descriptive data on the sample are reported in table 1. Over 65% of the sample is male, but this is similar to a sample of over 1750 adults with serious mental illness receiving outpatient rehabilitation services in Los Angeles in similar programs. There were no statistically significant differences between the completers and noncompleters on the variables in table 1 or were there statistically significant differences across sites on those variables. According to data presented below, over 93% of the subjects' total outpatient services during the study year were received from the agency from which they were recruited. To our knowledge, there was no site cross-over among subjects during the study period. All subjects signed an informed consent under protocols approved by the Institutional Review Boards at the University of Southern California, University of California Los Angeles, and VA Greater Los Angeles Healthcare System.
Table 1.
Characteristics of the Samples at Baseline: Full Baseline Sample vs 12-month Completers
| Baseline (N = 125) | 12 Month (N = 102) | |
| Gender (%) | ||
| Male | 86 (68.8) | 70 (68.6) |
| Female | 39 (31.2) | 32 (31.4) |
| Age | ||
| Range (y) | 18–62 | 21–62 |
| Mean | 38.01 | 38.22 |
| SD | 9.15 | 9.35 |
| Ethnicity (%) | ||
| White | 55 (44.0) | 47 (46.1) |
| African American | 49 (39.2) | 37 (36.3) |
| Latino | 14 (11.2) | 12 (11.8) |
| Asian | 4 (3.2) | 4 (3.9) |
| Other | 3 (2.4) | 2 (2.0) |
| Mean (SD) | Mean (SD) | |
| Education | 11.93 y (1.79)a | 12.06 y (1.86)b |
| Length of illness | 13.99 y (10.06)c | 13.73 y (10.18)d |
| Neurocognitive composite (sum of Z scores) | −0.35 (3.28) | −0.06 (3.07) |
| Perception of emotion | 37.85 (9.39) | 38.34 (9.32) |
| RFS totale | 8.32 (3.60) | 8.45 (3.71) |
| RFS social | 2.96 (1.56) | 3.00 (1.55) |
| RFS work | 2.00 (1.56) | 2.12 (1.66) |
| RFS independent | 3.37 (1.74) | 3.33 (1.74) |
| BPRSf | 39.16 (10.16) | 39.19 (10.51) |
Measures
All psychosocial variables came from data gathered in face-to-face interviews conducted at a place of the subject's choosing, typically at a program site or their residence. The interviewers were masters-level clinicians trained using a protocol described in detail elsewhere.32 They were trained on the Brief Psychiatric Rating Scale33 using a protocol described by Ventura et al.34 The neurocognitive and social cognition data came from laboratory-based assessments in a facility designed for this study. We used summary scores for the neurocognition, social cognition, and psychosocial variables because we were interested in global rather than specific effects in these analyses.
Psychosocial Measure.
The Role Functioning Scale (RFS),35 a scale of choice for this population,36 is a functional outcome measure that was administered during a semi-structured interview. Interviewer ratings of work, social functioning, and independent living from the RFS are used for this study, in accordance with procedures described by Brekke et al.32 The RFS provides anchored descriptions and captures both the quantity and quality of community-based functioning in that domain. After interview training, the intraclass correlation coefficient among 3 interviewers on the RFS items was >.8. In this study, we used the global score (ie, the sum of the 3 items). A principal components factor analysis of the 3 items found a single factor with eigenvalue greater than 1 that explained 55% of the item variance and supported the use of the global score.
Social Cognition Measures.
Social cognition is measured in various ways in schizophrenia research.19 For the current study, we assessed affect perception as measured by the sum of following 3 scales: (1) the Facial Emotion Identification Test,37 (2) the Voice Emotion Identification Test,37 and (3) the Videotape Affect Perception Test.38 These tests and the procedures for administering them are fully described by Kee et al.39 All 3 require the subject to select 1 of 6 basic emotions (ie, happy, angry, afraid, sad, surprised, and ashamed) that best describes the emotion presented in photographs, on audiotape, or in videotaped scenes of interpersonal situations.
Neurocognitive Measures.
The neurocognitive measure in this study is a composite created to reflect verbal fluency, immediate (working) memory, secondary (episodic) memory, sustained attention, and mental flexibility. It was derived from 5 tests by summing the standardized scores. The 5 tests were the Controlled Oral Word Association Test,40 the Digit Span Distractibility Test,41 the California Verbal Learning Test,42 the Degraded-Stimulus Continuous Performance Test,43 and perseverative errors from the Wisconsin Card Sorting Test.44 Although these constructs are often represented as separate factors when multiple indicators are available,45 we represented the neurocognitive factor as a composite. A principal components factor analysis of the 5 scores revealed a single factor that accounted for over 53% of the total score variance.
Service Intensity.
Service intensity was measured with a method successfully used in a previous study of similar sites.28 Intensity was measured as the number of days that an individual received at least one service contact from the admitting rehabilitation agency in the 365 days subsequent to admission to the study. The service contact data were gathered by staff on a daily basis for billing and administrative purposes and are subject to utilization review by County auditors. The units of service data are uploaded to a billing program that generates units of service billing data in 15-min increments. The service intensity data for this study came from the programs' service data that is eventually transferred to the County billing system. In addition, we retrieved data on all mental health contacts from throughout the County mental health system for the study period on all study subjects. These data suggest that the vast majority (over 93%) of all outpatient service contacts from County and County-contracted agencies during the study year came from the rehabilitation agency to which the subject was admitted when they were recruited into this study. As expected, there was wide individual variation in the days and minutes of rehabilitation contact, with minutes and days of treatment received being highly correlated (Pearson's r = .7). On average, clients were seen about twice a week, with an average treatment day representing over 2 h of service contact which is in line with our pilot data which showed that the sites were service intensive, and which validated our site selection protocol.
Statistical Analyses
Hierarchical Linear Modeling (HLM) was used to test the study hypotheses. Advances in longitudinal research suggest that modeling should begin on the individual subject level. This allows for the assessment of both intraindividual and interindividual differences in change.46–48 The recommended approach is to model individual change across time and then examine the effects of covariates (eg, individual factors) to see if there are systematic differences in rate (ie, slope) of change. This 2-fold aim can be accomplished using growth curves and HLM.49–51
HLM involves modeling at 2 levels. At Level 1, a least-squares regression equation is fit to each individual's data across all time points (this equation is the growth curve). Each individual's scores on the criterion (functional outcome) are regressed on time or a transformation of time. At Level 2, the Level 1 parameter estimates of the slope (in this case the linear slope) are treated as criterion scores and each is regressed on the covariate (in this study, neurocognition, social cognition, and service intensity). Final estimates of the growth curve parameters for each individual are derived via empirical Bayes estimation.52 Empirical Bayes estimation provides a composite procedure that uses both the information from each subjects' data and the information from the covariate in determining final parameter estimates. That is, each individual's growth curve parameters are estimated with a weighted combination of the Level 1 and Level 2 estimates (see Bryk and Raudenbush49 and Raudenbush and Bryk53). After individual curve parameters are estimated, hypothesis testing can be used to assess the fit of the group linear curves in the population, as well as the significance of the covariate interaction (for a detailed discussion, see Bryk and Raudenbush50 and Raudenbush and Bryk51).
In this study, there was interest in 3 covariates, neurocognition scores, social cognition scores, and service intensity. The central questions were whether these covariates were responsible for systematic differences in the intercept (the initial functional level at baseline) and in the growth curve rate (the magnitude of the slope of functional change over 12 months). All analyses were carried out with the HLM 6 software.54
For each hypothesis, the Level 1 model was the same,
where yij is the RFS total score for the ith participant (i = 1, … N) at time j (j = 1, …, J), β0i is the ith participant's intercept term, β1i is their linear slope, tij is the linear coefficient (t = [0, 6, 12]), and eij is the Level 1 residual. Various Level 2 models were specified to test the study hypotheses. Hypotheses 1 and 2 had the Level 2 model
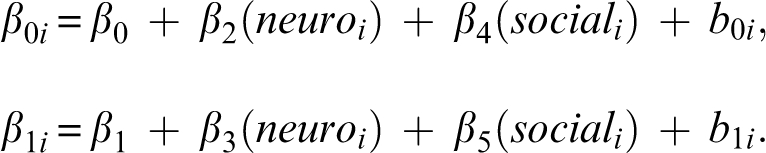 |
In the above equations, β0 and β1 are the fixed effects for the intercept and linear slope, respectively, β2 and β4 are the fixed effects of neurocognition and social cognition on the Level 1 intercepts, β3 and β5 are the fixed effects of neurocognition and social cognition on the Level 1 slopes, and b0i and b1i are Level 2 residuals (also known as random effects). Hypothesis 1 focuses on β2 and β4 whereas Hypothesis 2 focused on β3 and β5. Hypothesis 3 was similar in form using only service intensity to predict the Level 1 intercepts and slopes. Hypothesis 4 had the 2 predictors as shown above and added service intensity as a main effect and as an interaction with the other 2 predictors. For Hypotheses 1–3, omnibus tests were followed by univariate tests only if the omnibus null hypothesis was rejected. For Hypothesis 4, the interaction terms were tested jointly first, followed by univariate tests.
Results
Preliminary Analyses
Before testing the study hypotheses, a number of preliminary analyses were completed. First, this study was predicated on the presence of rehabilitative change; therefore, unconditional HLM models were run to examine the rate of change in global psychosocial functioning over 12 months. The unconditional HLM models have no predictors in the Level 2 equations. There was a statistically significant rate of rehabilitative change (β = .77, t = 5.2, df = 124, P < .000). Given that a one-point change in the RFS score is considered clinically significant,35 this rate of change over 12 months is clinically significant (.77 × 2). Importantly, each of the 4 sites showed statistically and clinically significant rates of change. Second, we wanted to examine the degree to which baseline scores on psychosocial functioning, social cognition, and neurocognition were related to days of treatment. This was to assess the degree to which certain clients select into more days of treatment or the degree to which staff differentially target certain clients for more treatment. None of these relationships was statistically significant (bivariate Pearson r ranged from .05 to .12, P > .15 in all cases). This is in line with the treatment philosophy of the sites, which states that all clients should be given equal opportunities for change regardless of their level of functioning or existing deficits.
Third, we used an intent-to-treat method for all analyses by retaining clients in the sample if they had received more than 1 day of treatment over the 12-month study period. Twenty subjects who were consented and tested at basline were eliminated from the analyses because they had no subsequent days of treatment. A comparison of the treated (n = 125) with the untreated sample (n = 20) on all baseline variables in table 1 revealed 2 statistically significant differences. The untreated group was higher than the treated group on independent living and neurocognition.
Fourth, we also wanted to examine whether each site had comparable levels of treatment intensity. While there was notable individual variation in the number of days of treatment received by clients (average no. of days = 89; SD = 56 days), the between-site variation in days treated was not statistically significant, although there was a trend for one site to be less intensive. In spite of this, even the least intensive site saw its clients on average of more than once a week, and the top 50% of treatment utilizers at that site were seen more than 2 days a week over the 12-month study period.
Hypothesis Testing
The first step in testing Hypotheses 1 and 2 was to do an omnibus multivariate test of the 4 parameters (2 intercepts and 2 slopes). This test was statistically significant (see table 2). The second step in testing the hypotheses involved univariate tests of significance. Hypothesis 1 proposed that better neurocognition and social cognition scores at baseline would be significantly associated with higher levels of initial functional status (the intercept hypothesis). Table 2 shows that both neurocognition and social cognition scores were significantly related to baseline level of psychosocial functioning in the predicted direction. Specifically, better neurocognition and social cognition at baseline were associated with higher psychosocial functioning at baseline.
Table 2.
Neurocognition and Social Cognition as Predictors of Change in Functional Outcome (FO) over 12 Months of Rehabilitation
| χ2 | df | P | ||
| 61.6 | 4 | .0000 | ||
| Omnibus Test | β | SE | t | Effect Size, r |
| Level 2 Covariate | ||||
| Neurocognition | ||||
| Intercept (FO) | .255 | 0.086 | 2.96** | .26 |
| Linear slope (FO) | .107 | 0.039 | 2.72** | .24 |
| Social cognition | ||||
| Intercept (FO) | .134 | 0.033 | 4.12*** | .35 |
| Linear slope (FO) | .024 | 0.015 | 1.63* | .15 |
P < .05
P < .01
P < .001; 1-tailed tests.
Hypothesis 2 stated that better neurocognition and social cognition scores at baseline would be associated with higher rates of functional rehabilitative change over 12 months (the slope hypothesis). The results in table 2 show that this hypothesis was supported. Higher neurocognition and social cognition scores at baseline predicted higher rates of rehabilitative change over the 12-month follow-along period. Hypothesis 3 states that more days of treatment will be related to higher rates of functional change. The results supported this hypothesis (see table 3). It should also be noted that neurocognition and social cognition are not related to the number of treatment days but that neurocognition, social cognition, and treatment days are all related to rates of functional change. This suggests that the effects on outcome from these individual and service indicators are independent.
Table 3.
Service Intensity as Predictor of Change in Functional Outcome (FO) over 12 months of Rehabilitation
| χ2 | df | P | ||
| 6.12 | 2 | .04 | ||
| Omnibus Test | β | SE | t | Effect Size, r |
| Level 2 Covariate | ||||
| Service intensity | ||||
| Intercept (FO) | −.008 | 0.005 | −1.59 | |
| Linear slope (FO) | .006 | 0.003 | 2.15* | .19 |
P < .025; 1-tailed test.
The final hypothesis proposed a moderator effect, such that treatment intensity would alter the relationship between social cognition, neurocognition, and rates of rehabilitative change. Prior to testing this hypothesis, we used the median to split the sample into high- and low-service intensity groups and then to compare the 2 groups to see if there might be sample characteristics that would confound interpretation of any moderator results. In terms of the variables in table 1, there were no statistically significant differences between the high- and low-service intensity groups (results available upon request). In testing this moderator hypothesis, we used days treated as a continuous variable when creating the interaction terms in order to preserve statistical power. Table 4 shows that the omnibus test was significant. From table 4 only the interaction terms are relevant to the moderation hypothesis, and the other results replicate the findings reported above. Concerning the moderation hypothesis, there are 2 notable results. First, as days of treatment decreased across subjects, the relationship between neurocognition and initial level of psychosocial functioning increased. Second, as the days of treatment decreased, the influence of social cognition on the rate of rehabilitative change increased at a trend level (P = .06). The second result provides some support for the compensatory moderation mechanism.
Table 4.
Interactions Between Service Intensity and Both Neurocognition and Social Cognition in Predicting Change in Functional Outcome (FO)
| χ2 | df | P | ||
| 10.51 | 4 | .03 | ||
| Omnibus Test | β | SE | t | Effect Size, r |
| Level 2 Covariate | ||||
| Neurocognition | ||||
| Intercept (FO) | .52 | 0.15 | 3.44*** | .30 |
| Linear (FO) | .12 | 0.06 | 1.86** | .17 |
| Service intensity | ||||
| Intercept (FO) | −.009 | 0.005 | −1.81* | .16 |
| Linear (FO) | .006 | 0.003 | 1.95* | .17 |
| Neurocognition × service | ||||
| Intercept (FO) | −.003 | 0.001 | −2.34* | .20 |
| Linear (FO) | −.00008 | 0.0006 | −0.13 | |
| Social Cognition | ||||
| Intercept (FO) | .153 | 0.059 | 2.59** | .23 |
| Linear (FO) | .067 | 0.025 | 2.71** | .24 |
| Service intensity | ||||
| Intercept (FO) | .003 | 0.021 | 0.15 | |
| Linear (FO) | .026 | 0.012 | 2.21* | .20 |
| Social cognition × service | ||||
| Intercept (FO) | −.0002 | 0.0006 | −0.51 | |
| Linear (FO) | −.0005 | 0.0003 | −1.88* | .17 |
P < .05
P < .01
P < .001
P = .06; 2-tailed tests.
Discussion
This study examined the relationships between neurocognition, social cognition, and initial functional level and the rates of functional rehabilitative change in community-based psychosocial rehabilitation interventions for individuals diagnosed with schizophrenia. We also tested a moderator hypothesis about service intensity. These findings have relevance to our understanding of the heterogeneity in functional rehabilitative outcomes, to our understanding of the conditions of rehabilitative change, and for the design of psychosocial interventions in the community.
Our first finding was that the initial level of psychosocial functioning was related to both social cognition and neurocognition at baseline. This cross-sectional finding corroborates a large body of literature showing that better neurocognition is associated with higher levels of psychosocial functioning in schizophrenia across a range of settings and outcomes.55 There is much less research on social cognition, but this finding corroborates those few studies as well.23 The effect size for social cognition was in the medium range, and for neurocognition, it was near the medium range. The magnitude of the effects are notable given that it has been argued that the impact of neurocognitive and social cognitive factors will attenuate as the outcomes become closer to real world functioning which is what was measured in this study21,23. These findings further establish the ecological validity of the impact of neurocognition and social cognition on functional status and support notions that both capacities underlay successful functioning in the community for individuals diagnosed with schizophrenia. Cross-sectional relationships, however, do not suggest that any factor will actually influence rates of change in desired outcomes during an intervention. Change rate was the focus of the second study hypothesis.
While change in functional outcome is not consistently achieved in randomized studies of community-based psychosocial interventions for schizophrenia, when they do occur, there is large between-individual heterogeneity in the occurrence and rates of change in even the most effective interventions.2–14 The present findings suggest that when significant rehabilitative change occurs, pretreatment levels of neurocognition and social cognition both significantly influence the rate of functional rehabilitative change over 12 months. Specifically, higher neurocognition and social cognition scores at baseline predicted higher rates of functional change over the subsequent 12 months. This suggests that these are rate-limiting factors for rehabilitative change and must be considered when understanding the factors responsible for promoting change in psychosocial rehabilitation, and, further, that they offer one explanation for the wide heterogeneity in functional change for individuals who participate in effective community-based interventions. This study also provides support for the ecological validity of the relationship between neurocognition and functional rehabilitative change. While previous studies have identified neurocognition as a rate-limiting factor for aspects of behavioral change in the hospital, this influence has rarely been examined in the community-based contexts where most rehabilitation occurs.
Our findings on social cognition are the first to establish it as a rate-limiting factor for rehabilitative change. This suggests that better social cognition is important to improving rates of functional rehabilitative change in community-based interventions. In a previous study,19 neurocognition and social cognition combined in a causal model to influence community-based psychosocial functioning. Our present findings suggest that understanding how these factors interact in treatment to influence rehabilitative change could be a useful line of research.
We also found that greater service intensity was related to higher rates of improvement in functional outcome over time. This finding replicates earlier studies28,29 and lays the foundation for examining whether service intensity moderates the relationships between neurocognition and functional outcome, and social cognition and functional outcome.
Once a rate-limiting factor like neurocognition or social cognition is identified, it is important to understand the conditions under which it exerts its influence and also the degree to which the existing interventions can be altered to influence its impact. One of these moderating conditions is the character of the services delivered and, in particular, the intensity of service that has been suggested as a moderator of the rate-limiting influence of neurocognition.20 We tested for 2 possible moderating dynamics. Our results offered some limited support for the compensatory hypothesis where higher service intensity will be associated with a weaker relationship between baseline neurocognition, social cognition, and subsequent functional outcome. First, the relationship between neurocognition and initial functional status is weaker for individuals who had more subsequent days of treatment. This could be because individuals self-select into fewer treatment days when they experience greater rate-limiting impacts or practitioners decrease the intensity of their services when this relationship is palpable to them. Second, there was a trend (P = .06) for more treatment days to be associated with a weaker influence of social cognition on rehabilitative change. This has more direct relevance to our moderator hypothesis and could suggest that increased practitioner activity reflected in more days of treatment compensates or overrides the rate-limiting impact of social cognition on functional change. Further research is needed to understand the conditions that facilitate the integration of neurocognition and social cognition and how treatment variables and rate-limiting variables interact.56
Overall, our results suggest that neurocognition and social cognition influence the initial functional level and the rates of rehabilitative change and that models of community-based psychosocial rehabilitation need to begin to integrate these factors into their services in several ways. First, practitioners and consumers could benefit from understanding that these factors do impact rates of functional rehabilitative change and that service factors alone cannot account for the individual heterogeneity in treatment outcomes. Second, this knowledge could be used as a foundation for service activities. For example, with relevant assessment, these factors could be used to identify individuals for whom functional change might be easier or more challenging. This can be used to educate both consumers and practitioners so that interventions can be more individually tailored and realistic change goals can be set. Rather than being used to delimit the rates of possible functional change, these assessments can be used to maximize individual change rates by minimizing practitioner and consumer frustration due to inaccurate goal setting and inappropriately low or high expectations for change. Third, there are psychosocial interventions available that are designed to compensate for neuropsychological deficits that have shown effectiveness in improving functional outcomes. Errorless learning57 and Cognitive Adaptation Training58 are central examples. Strategies for transporting and integrating these interventions into existing community-based rehabilitation services are needed.
Another issue with rate-limiting factors is whether they can be directly improved through treatment or intervention. In addition to compensatory interventions that are designed to take cognitive deficits into account, restorative interventions such as cognitive remediation are designed to improve underlying cognitive functions. Such approaches use systematically graded cognitive exercises and have shown some success in improving basic cognitive functions in the serious mentally ill.59,60 In combination with other psychosocial interventions, cognitive interventions have yielded improved processing of social information.56,61 Cognitive remediation approaches are complementary to psychopharmacological approaches intended to identify and evaluate potential cognition-enhancing drugs for schizophrenia and other major mental illnesses, as illustrated by the National Institute of Mental Health-Measurement and Treatment Research to Improve Cognition in Schizophrenia Initiative.55,62 Two recent studies on vocational intervention have shown that modest cognitive change is possible from remediation approaches and that combining cognitive remediation with psychosocial interventions is more effective in improving vocational outcomes than psychosocial intervention alone.20,60 However, it is not yet clear to what degree cognitive change is linked to treatment effects. This is a critical question for future experimental and observational studies.
Concerning social cognition, it is not yet clear whether compensatory or remediation strategies are best suited. There is early work suggesting that some aspects of social cognition respond to remediation strategies.63 It is clear, however, that social cognition must be a topic of investigation in terms of rehabilitation interventions, much as was begun with neurocognition over a decade ago.
There are several limitations to this study. First, there is a wide range of community-based psychosocial interventions. The generalizability of these findings across different models is unknown. Second, we did not test for specificity effects between distinct neurocognitive factors and discrete domains of functional outcome. Future research should address the specificity of effects between specific domains of neurocognition (eg, immediate memory) and distinct functional outcomes (eg, work or social functioning). Third, our measure of social cognition only reflects one aspect of the larger construct. Other aspects of social cognition such as theory of mind and attributional style were not reflected in our measure. Fourth, while we did not find site effects largely because our extensive pilot data gathering allowed us to select homogenous program sites, it is possible that some site effects were undetected. Fifth, there are other moderators that could be investigated in terms of their influence on the relationship between neurocognition, social cognition, and functional outcomes. Certain type of services, such as rehabilitation or case management, might have differential effects. Similarly, the character of the alliance between consumer and practitioner is also a potentially important moderator. Better understanding of these moderators could be integrated into service design and intervention development in order to facilitate rehabilitative change. Finally, Spaulding et al64 found a nonspecific impact of intensive rehabilitation on neurocognitive performance. Prospective measures of neurocognition and social cognition would allow for a test of these effects, and they would also allow for an examination of the degree to which changes in neurocognition and social cognition are linked to changes in functional outcome which is a critical area for future investigation.
References
- 1.Drake RE. Recent research on vocational rehabilitation for persons with severe mental illness. Curr Opin Psychiatr. 2003;16:451–455. [Google Scholar]
- 2.Mueser KT. Models of community care for severe mental illness: a review of research on case management. Schizophr Bull. 1998;24:37–74. doi: 10.1093/oxfordjournals.schbul.a033314. [DOI] [PubMed] [Google Scholar]
- 3.Scott SE. Assertive community treatment and case management for schizophrenia. Schizophr Bull. 1995;24:657–667. doi: 10.1093/schbul/21.4.657. [DOI] [PubMed] [Google Scholar]
- 4.Solomon P. The efficacy of case management services for severely mentally disabled clients. Community Ment Health J. 1992;28:163–180. doi: 10.1007/BF00756815. [DOI] [PubMed] [Google Scholar]
- 5.Bustillo JR. The psychosocial treatment of schizophrenia: an update. Am J Psychiatry. 2001;158:163–175. doi: 10.1176/appi.ajp.158.2.163. [DOI] [PubMed] [Google Scholar]
- 6.Penn DL. Information processing, social skill, and gender in schizophrenia. Psychiatry Res. 1996;59:213–220. doi: 10.1016/0165-1781(95)02768-8. [DOI] [PubMed] [Google Scholar]
- 7.Group for the Advancement of Psychiatry. Beyond Symptom Suppression: Improving Long-Term Outcomes of Schizophrenia. Washington, DC: American Psychiatric Press, Inc.; 1992. [PubMed] [Google Scholar]
- 8.Bond GR. Assertive outreach for frequent users of psychiatric hospitals: a meta-analysis. J Ment Health Adm. 1995;22:4–16. doi: 10.1007/BF02519193. [DOI] [PubMed] [Google Scholar]
- 9.Test MA. Community support programs. In: Bellack AS, editor. Treatment and Care for Schizophrenia. New York: Grune and Stratton; 1984. pp. 347–373. [Google Scholar]
- 10.Test MA. Long-term community care through an assertive continuous treatment team. In: Tamminga CA, editor. Schizophrenia Research. 1. 1 ed. New York: Raven Press; 1991. pp. 239–246. [Google Scholar]
- 11.Hargreaves WA. Effectiveness of services for the severely mentally ill. In: Taube CA, editor. The Future of Mental Health Services Research. Washington, DC: U.S. Department of Health and Human Services; 1989. [Google Scholar]
- 12.Olfson M. Assertive community treatment: an evaluation of the experimental evidence. Hosp Community Psychiatry. 1990;41:634–651. doi: 10.1176/ps.41.6.634. [DOI] [PubMed] [Google Scholar]
- 13.Wallace CJ. Washington, DC: Department of Health and Human Services; 1993. Psychiatric Rehabilitation. Health Care Reform for Americans with Severe Mental Illnesses: Report of the National Advisory Mental Health Council. [DOI] [PubMed] [Google Scholar]
- 14.Burns BJ. Assertive community treatment: an update of randomized trials. Psychiatr Serv. 1995;46:669–675. doi: 10.1176/ps.46.7.669. [DOI] [PubMed] [Google Scholar]
- 15.Lehman AF. Vocational rehabilitation in schizophrenia. Schizophr Bull. 1995;21:645–656. doi: 10.1093/schbul/21.4.645. [DOI] [PubMed] [Google Scholar]
- 16.Bellack AS. Psychosocial treatment for schizophrenia. Schizophr Bull. 1993;19:317–336. doi: 10.1093/schbul/19.2.317. [DOI] [PubMed] [Google Scholar]
- 17.Green MF. What are the functional consequences of neurocognitive deficits in schizophrenia? Am J Psychiatry. 1996;153:321–330. doi: 10.1176/ajp.153.3.321. [DOI] [PubMed] [Google Scholar]
- 18.Green MF. Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the “Right Stuff?”. Schizophr Bull. 2000;26:119–136. doi: 10.1093/oxfordjournals.schbul.a033430. [DOI] [PubMed] [Google Scholar]
- 19.Brekke JS. Biosocial pathways to functional outcome in schizophrenia. Schizophr Res. 2005;80:213–235. doi: 10.1016/j.schres.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 20.McGurk SR. Cognitive training and supported employment for persons with severe mental illness: one-year results from a randomized controlled trial. Schizophr Bull. 2005;31:898–909. doi: 10.1093/schbul/sbi037. [DOI] [PubMed] [Google Scholar]
- 21.Green MF. Longitudinal studies of cognition and functional outcome in schizophrenia: implications for Matrics. Schizophr Res. 2004;72:41–51. doi: 10.1016/j.schres.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 22.Pinkham AE. Implications for the neural basis of social cognition for the study of schizophrenia. Am J Psychiatry. 2003;160:815–824. doi: 10.1176/appi.ajp.160.5.815. [DOI] [PubMed] [Google Scholar]
- 23.Couture SM. The functional significance of social cognition in schizophrenia: a review. Schizophr Bull. 2006;443:1–20. doi: 10.1093/schbul/sbl029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vauth R. Does social cognition influence the relation between neurocognitive deficits and vocational functioning in schizophrenia? Psychiatry Res. 2004;128:155–165. doi: 10.1016/j.psychres.2004.05.018. [DOI] [PubMed] [Google Scholar]
- 25.Green MF. Social cognition in schizophrenia: recommendations from the measurement and treatment research to improve cognition in schizophrenia new approaches conference. Schizophr Bull. 2005;31:882–887. doi: 10.1093/schbul/sbi049. [DOI] [PubMed] [Google Scholar]
- 26.Evans JD, et al. Cognitive and clinical predictors of success in vocational rehabilitation in schizophrenia. Schizophr Res. 2004;70:331–342. doi: 10.1016/j.schres.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 27.McGurk SR. The role of cognition in vocational functioning in schizophrenia. Schizophr Res. 2000;45:175–184. doi: 10.1016/s0920-9964(99)00198-x. [DOI] [PubMed] [Google Scholar]
- 28.Brekke JS. The impact of service characteristics on functional outcomes from community support programs for persons with schizophrenia: a growth curve analysis. J Consult Clin Psychol. 1997;65:464–475. doi: 10.1037//0022-006x.65.3.464. [DOI] [PubMed] [Google Scholar]
- 29.Brekke JS. Intensity and continuity of services and functional outcomes in the rehabilitation of persons with schizophrenia. Psychiatr Serv. 1999;50:248–256. doi: 10.1176/ps.50.2.248. [DOI] [PubMed] [Google Scholar]
- 30.Young AS. Implementing publicly funded risk contracts with community mental health organizations. Psychiatr Serv. 1998;49:1579–1584. doi: 10.1176/ps.49.12.1579. [DOI] [PubMed] [Google Scholar]
- 31.Bae S-W. Ethnicity and treatment outcome variation in schizophrenia: a longitudinal study of community based psychosocial rehabilitation interventions. J Nerv Ment Dis. 2004;192:623–628. doi: 10.1097/01.nmd.0000140035.36075.7f. [DOI] [PubMed] [Google Scholar]
- 32.Brekke JS. Psychosocial functioning and subjective experience in schizophrenia. Schizophr Bull. 1993;19:599–608. doi: 10.1093/schbul/19.3.599. [DOI] [PubMed] [Google Scholar]
- 33.Lukoff D. Manual for the expanded Brief Psychiatric Rating Scale. Schizophr Bull. 1986;12:594–602. [Google Scholar]
- 34.Ventura J. Training and quality assurance with the Brief Psychiatric Rating Scale: the drift busters. Int J Method Psych. 1995;3:221–244. [Google Scholar]
- 35.Goodman SH. Assessing levels of adaptive functioning: the Role Functioning Scale. Community Ment Health J. 1993;29:119–131. doi: 10.1007/BF00756338. [DOI] [PubMed] [Google Scholar]
- 36.Green RS. Selecting a rating scale for evaluating services to the chronically mentally ill. Community Ment Health J. 1987;23:91–102. doi: 10.1007/BF00757163. [DOI] [PubMed] [Google Scholar]
- 37.Kerr SL. Emotion perception in schizophrenia: specific deficit or further evidence of generalized poor performance? J Abnorm Psychol. 1993;102:312–318. doi: 10.1037//0021-843x.102.2.312. [DOI] [PubMed] [Google Scholar]
- 38.Bellack AS. Cue availability and affect perception in schizophrenia. Schizophr Bull. 1996;22:535–544. doi: 10.1093/schbul/22.3.535. [DOI] [PubMed] [Google Scholar]
- 39.Kee KS. Perception of emotion and neurocognitive functioning in schizophrenia: what's the link? Psychiatry Res. 1998;81:57–65. doi: 10.1016/s0165-1781(98)00083-3. [DOI] [PubMed] [Google Scholar]
- 40.Lezak MD. New York: Oxford University Press; 1995. Neuropsychological Assessment. [Google Scholar]
- 41.Oltmanns TF. Schizophrenic performance when distractors are present: attentional deficit or differential task difficulty? J Abnorm Psychol. 1975;84:205–209. doi: 10.1037/h0076721. [DOI] [PubMed] [Google Scholar]
- 42.Delis DC. New York: Psychological Corporation; 1987. The California Verbal Learning Test. [Google Scholar]
- 43.Nuechterlein KH. Los Angeles: University of California, Los Angeles; 1992. UCLA Continuous Performance Test [manual and computer program]. Version 4. [Google Scholar]
- 44.Heaton RK. Odessa, Fla: Psychological Assessment Resources; 1981. A Manual for the Wisconsin Card Sorting Task. [Google Scholar]
- 45.Nuechterlein KH. Identification of separable cognitive factors in schizophrenia. Schizophr Res. 2004;72:29–39. doi: 10.1016/j.schres.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 46.Rogosa DR. A growth curve approach to the measurement of change. Psychol Bull. 1982;90:726–748. [Google Scholar]
- 47.Rogosa DR. Understanding correlates of change by modeling individual differences in growth. Psychometrika. 1985;50:203–228. [Google Scholar]
- 48.Willett JB. Questions and answers in the measurement of change. In: Rothkopf E, editor. Review of Research in Education 1988–1989. Washington, DC: American Educational Research Association; 1988–1989. pp. 345–422. [Google Scholar]
- 49.Bryk AS. Application of hierarchical linear models to assessing change. Psychol Bull. 1987;101:147–158. [Google Scholar]
- 50.Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. Newbury Park, Calif: Sage; 1992. [Google Scholar]
- 51.Raudenbush SW. Thousand Oaks, Calif: Sage; 2002. Hierarchical Linear Models: Applications and Data Analysis Methods. [Google Scholar]
- 52.Strenio JL. Empirical Bayes estimation of individual growth curve parameters and their relationship to covariates. Biometrics. 1983;39:71–86. [PubMed] [Google Scholar]
- 53.Raudenbush SW. Empirical Bayes meta-analysis. J Educ Stat. 1985;10:75–98. [Google Scholar]
- 54.Raudenbush SW. Lincolnwood, Ill: Scientific Software International; 2004. Hlm 6: Hierarchical Linear and Nonlinear Modeling. [Google Scholar]
- 55.Green MF, et al. Approaching a consensus cognitive battery for clinical trials in schizophrenia: the NIMH-Matrics conference to select cognitive domains and test criteria. Biol Psychiatry. 2004;56:301–307. doi: 10.1016/j.biopsych.2004.06.023. [DOI] [PubMed] [Google Scholar]
- 56.Medalia A. What predicts a good response to cognitive remediation interventions? Schizophr Bull. 2005;31:942–953. doi: 10.1093/schbul/sbi045. [DOI] [PubMed] [Google Scholar]
- 57.Kern RS. Does ‘errorless learning’ compensate for neurocognitive impairments in the work rehabilitation of persons with schizophrenia? Psychol Med. 2003;33:433–442. doi: 10.1017/s0033291702007298. [DOI] [PubMed] [Google Scholar]
- 58.Velligan DI. Rehab rounds: two case studies of cognitive adaptation training for outpatients with schizophrenia. Psychiatr Serv. 2000;51:25–29. doi: 10.1176/ps.51.1.25. [DOI] [PubMed] [Google Scholar]
- 59.Bell M. Neurocognitive enhancement therapy with work therapy: effects on neuropsychological test performance. Arch Gen Psychiatry. 2001;58:763–768. doi: 10.1001/archpsyc.58.8.763. [DOI] [PubMed] [Google Scholar]
- 60.Bell M. Cognitive remediation of working memory deficits: durability of training effects in severely impaired and less severely impaired schizophrenia. Acta Psychiatr Scand. 2003;108:101–109. doi: 10.1034/j.1600-0447.2003.00090.x. [DOI] [PubMed] [Google Scholar]
- 61.Hogarty GE, et al. Cognitive enhancement therapy for schizophrenia: effects of a 2-year randomized trial on cognition and behavior. Arch Gen Psychiatry. 2004;61:866–876. doi: 10.1001/archpsyc.61.9.866. [DOI] [PubMed] [Google Scholar]
- 62.Marder SR. Measurement and treatment research to improve cognition in schizophrenia: NIMH Matrics initiative to support the development of agents for improving cognition in schizophrenia. Schizophr Res. 2004;72:5–9. doi: 10.1016/j.schres.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 63.Penn D. A pilot study of social cognition and interaction training (Scit) for schizophrenia. Schizophr Res. 2005;80:357–359. doi: 10.1016/j.schres.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 64.Spaulding WD. Effects of cognitive treatment in psychiatric rehabilitation. Schizophr Bull. 1999;25:657–676. doi: 10.1093/oxfordjournals.schbul.a033409. [DOI] [PubMed] [Google Scholar]
- 65.Overall JE. The Brief Psychiatric Rating Scale. Psychol Rep. 1962;10:799–812. [Google Scholar]


