Abstract
Kraepelin said severe mental illness was due to 2 diseases subsequently characterized as disorders of thought vs disorders of mood, ie, the Kraepelinian dichotomy. Schizophrenia, traditionally considered the disorder of thought, has been defined by the presence of hallucinations, delusions, catatonia, and disorganization. Tangentiality, derailment, loose associations, and thought blocking are typically considered pathognomonic of schizophrenia. By contrast, the mood disorders have been characterized only as disorders of the emotions, though both depression and mania, when severe, are now recognized to include the same psychotic features traditionally considered diagnostic of schizophrenia. This article addresses disordered thinking in mania in order to clarify the relationship between schizophrenia and psychotic mood disorders. Normally, the brain's selective attention mechanism filters and prioritizes incoming stimuli by excluding from consciousness extraneous, low-priority stimuli and grading the importance of more relevant data. Because this “filter/prioritizer” becomes defective in mania, tangential stimuli are processed without appropriate prioritization. Observed as distractibility, this symptom is an index of the breakdown in selective attention and the severity of mania, accounting for the signs and symptoms of psychotic thinking. The zone of rarity between schizophrenia and psychotic mood disorders is blurred because severe disorders of mood are also disorders of thought. This relationship calls into question the tenet that schizophrenia is a disease separate from psychotic mood disorders. Patients whose case histories are discussed herein gave their written informed consent to participate in this institutional human subjects committee–approved protocol.
Keywords: psychosis, mania, schizophrenia, selective attention, Broadbent filter theory, Kraepelinian dichotomy
Questions About the Dichotomy of Disorders of Thought vs Disorders of Mood
Descriptions of the major psychiatric diseases were recorded in the 19th and early 20th centuries. Kraepelin described 2 distinct disorders (the Kraepelinian dichotomy), dementia praecox, renamed schizophrenia by Bleuler in 1911, and manic depressive insanity, now called bipolar disorder (tables 1 and 2).1,2 Kraepelin, Bleuler, Schneider, and others defined schizophrenia by the presence of disordered thought manifested in the psychotic symptoms of hallucinations, delusions, catatonia, and/or disorganization.1–3 Bleuler and Schneider equated psychosis with schizophrenia, regardless of prominent mood symptoms.2,3 The 1933 introduction of schizoaffective disorder by Kasanin recognized the importance of mood symptoms in psychotic patients, drew attention to similarities between bipolar and schizophrenia, and reflected an effort to erode the Kraepelinian dichotomy.4 Despite this, the concept of schizophrenia, promoted by Bleuler and Schneider, has been influential and resistant to change in the United States where academic psychiatry has differentiated the mood disorders as disorders of the emotions from the schizophrenias as disorders of thought. A growing literature is challenging this concept.
Table 1.
DSM-IV-TR Diagnostic Criteria for Schizophrenia (Modified)a
| A. Characteristic symptoms: patient must have 2 symptoms during a 1-month (active) phase (except as noted below) (only 1 symptom is required if delusions are bizarre or hallucinations are a voice commenting on one's behavior/thoughts or if 2 or more voices are conversing with each otherbc) |
| 1. Delusionsb |
| 2. Hallucinationsb |
| 3. Disorganized speech (frequent derailment, incoherence)b |
| 4. Grossly disorganizedb or catatonicb behavior |
| 5. Negative symptoms (affective flattening, alogia, and avolition)b |
| B. Social/occupational dysfunction: work, interpersonal relations, or self-care have markedly deterioratedb |
| C. Duration: continuous signs for 6 months with 1-month active-phase symptoms and may include prodromal or residual symptomsb |
| D. Exclude schizoaffective and mood D/Od with psychotic featurese |
| E. Exclude substance and general medical conditionb |
| F. Exclude preexisting pervasive developmental D/Ob |
Abbreviated format without change in meaning or substance. DSM-IV-TR, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision.
These symptoms/criteria are disease nonspecific and occur frequently in mood D/O, severe with psychotic features.
These qualifications that allow a diagnosis of schizophrenia with only 1 of the characteristic symptoms in “A” are from K. Schneider's3 first-rank symptoms.
D/O, disorders.
This criterion is often underemphasized or ignored; a diagnosis of schizophrenia is made before reaching criterion D.
Table 2.
DSM-IV-TR Diagnostic Criteria and Specifiers for Mania (modified for brevity)
| a. Diagnostic criteria for a manic episode (defines bipolar mood D/O) |
| A. Distinct period for at least 1 week (or inpatient hospitalization necessary) of abnormal and persistently elevated, expansive, or irritable mood |
| B. In the period, 3 symptoms (4 if mood is only irritable) persist to a significant degree |
| 1. Distractibility |
| 2. Insomnia with increased energy |
| 3. Grandiosity/increased self-esteem |
| 4. Flight of ideas |
| 5. Increased activities: including phoning, spending, travel, investing, gambling, sex; excessive involvement in pleasurable activities with high potential for negative outcome |
| 6. Speech: pressed to incoherenta |
| 7. Thoughts: racing, loose, tangentiala |
| C. Symptoms cause marked impairment in functioninga (job, social, family) or hospitalizationa warranted because of severity of symptoms |
| D. Symptoms not due to substance or general medical condition |
| b. Specifiers for mood D/O diagnoses: |
| A. Presenting state—for bipolar: manic, depressed, mixed; for unipolar: single episode or recurrent |
| B. Severity: mild, moderate, severe without, severe with psychotic featuresa; partial, full remission |
| C. Course/onset: chronic (symptoms over 2 years)a, seasonal affective D/O, rapid cyclinga (at least 4 episodes/year), postpartum onset (within 4 weeks), with or without full interepisode recoverya |
| D. Features: catatonica, melancholic, atypicala |
Note: DSM-IV-TR, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision; D/O, disorders.
Signs and symptoms associated or confused with schizophrenia.
By 1978, Pope and Lipinski observed that patients with severe mood disorders did experience hallucinations, delusions, catatonia, and disorganization, which are, in fact, disorders of thought.5 They and others have concluded that psychosis and disordered thought are common in severe bipolar and that many patients diagnosed with schizophrenia (because they experience hallucinations and/or delusions) are misdiagnosed and actually suffer from severe but unrecognized bipolar disorder.5–13 Furthermore, chronicity of course, treatment resistance, or cognitive deficits do not distinguish these 2 disorders.11,12,14–23 Persistent cognitive defects in executive function and working memory were initially associated with patients diagnosed with schizophrenia.17 However, severe bipolar patients can suffer a chronic deteriorating course with similar permanent cognitive impairment that worsens with increasing episodes and impairs executive function and memory, even during remissions.11,12,14,21 Similar neurodevelopmental defects have been suggested in the etiology of both bipolar disorder and schizophrenia.22,23 Another realm of overlap is sleep disturbances that are common to patients diagnosed with schizophrenia and bipolar disorder.24,25 Such phenotypic overlap supports the conclusion that schizophrenia may be the same disease as a psychotic mood disorder.5,13 Is one of these a more valid disorder?
In contrast to schizophrenia, bipolar disorder is scientifically grounded as a “bona fide” disease because its diagnostic criteria are unique. Classic bipolar patients are so different from normals and patients with other medical conditions and they demonstrate such a large variance in their thoughts and behavior between episodes of mania and depression, that selection confidence is high. Schizophrenia has no unique symptom or group of symptoms not accounted for by severe psychotic bipolar. Despite phenotypic similarities, further clarification of the relationship between schizophrenia and psychotic bipolar can be expected from the elucidation of mechanisms of psychotic thought, but such an understanding remains challenging and speculative.18–23,26–29
Selective Attention: the Brain's Filter/Prioritizer
The human brain possesses the ability to selectively process incoming information. Attention is part of this processing and is a multidimensional construct. Selective attention refers to those mechanisms which lead our consciousness to be dominated by 1 thing rather than another.26 Partly under voluntary control, partly subconscious, and partly dependent on stimulus salience, some stimuli are processed more thoroughly than others. Experimental models, including Donald Broadbent filter theory and various cognitive neuroscience techniques in psychiatric patients, have focused on selective attention and its malfunction.18–21,26–29 Selective attention appears to govern an initial filtration process that is linked with a prioritization mechanism before stimuli reach consciousness (figures 1–3). Stimuli that reach consciousness are the basis of thoughts, verbalizations, and actions. This filter/prioritizer enables one to screen out and avoid attending to extraneous distractions during a conversation or other focused activity such as an initial diagnostic interview. Although there is wide individual variability in what is likely to attract or distract one's attention, stimuli indicating emergency or life-threatening situations are universally given priority in euthymic individuals. For example, the smell of smoke appropriately overrides most conversations. By contrast, at a ball game, depending on their individual interests, a home run or touchdown might appropriately distract only some from a serious discussion.
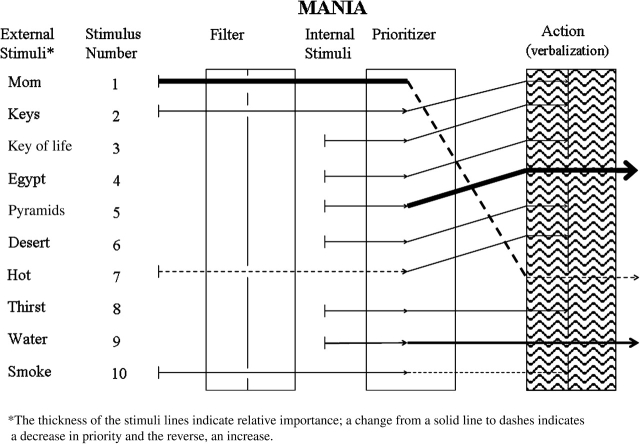
Fig. 1.
Selective Attention in Mood Disorders: Mania. In mania, the subject of “mom” is inappropriately lost when stimulus 2, the “keys”, is passed through the filter and prioritized, possibly due to it being the most recent stimulus. The keys idea is not verbalized because of a flurry of sequential internal stimuli based initially on keys and then on subsequent internal stimuli (see text). This series of internal stimuli includes items 3–9. Stimulus 7 is shown as a dashed line of external input because the room may have been warm. Only 5 and 9 are verbalized. Although there are connections to each thought based on the patient's report, the failure to filter and prioritize causes stimuli to come so fast and demand attention (apparently based on most recent order) that there is not enough time to verbalize all of them. An observer hears only “mom,” “pyramids,” and wanting water, concluding there has been a “blockage of thought.” The present explanation is predicated on the core manic symptoms of distractibility, flight of ideas, and racing thoughts. Manic thought is indeed disordered. The potentially critical external stimulus of “smoke” (item 10) may pass the filter but may not be adequately prioritized in mania to receive action. “Smoke” may be quickly overridden by the next stimulus such as “cigarettes are expensive” or “Smokey the Bear is cute.” The first 9 stimuli are actual thoughts of the patient as discussed in the text; stimulus 10 is hypothesized. This exchange and series of thoughts might occur in as little as 1 minute. Three areas of central nervous system data processing are denoted by each set of 3 boxes, each set representing 1 of 3 states of mood. The examples of the stimuli used in the figure derive from an actual patient interview during a student case conference (see text). Represented by the first box in each of the 3 sets, external stimuli appear to meet a filter that eliminates trivial data in euthymia while most or all stimuli pass through the filter in mania. Excessive stimuli may be stopped at the filter in depression. Internal stimuli are shown but their filtration is not indicated in the figure. Represented by the middle boxes, a second data-processing mechanism is a prioritizing function that can rearrange the importance of stimuli, diminishing or exaggerating attention to incoming data. The third boxes in each set represent action or verbalization. The time elapsed during processing of the interview material differs among mood states. In euthymia, the 8 stimuli take 2–5 minutes; the 10 stimuli in mania, less than a minute and 5 steps in depression, 5–10 minutes.
Defective Selective Attention Is Observed as Manic Distractibility
Distractibility is a recognized core diagnostic symptom of mania (table 2).30 In mania, the selective attention function deteriorates and the filter/prioritizer becomes more porous allowing inappropriate and irrelevant stimuli to gain attention and focus (figure 1). This defect is observed clinically as manic distractibility, poor judgment, and lack of insight. The level of distractibility provides a clinical index reflecting the severity of the information-processing defect in manic patients.18,28,29 Increasing distractibility in mania leads to disorganization of thought and behavior and to psychosis. Although disorganization is still considered diagnostic of schizophrenia according to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR),30 it is a prominent characteristic of severe mania, likely exacerbated by failure of the selective attention function and increasing distractibility.18 There are a number of symptoms of disordered thinking that are traditionally considered pathognomonic for schizophrenia such as tangentiality, derailment, loose associations, ideas of reference/influence, blocking, rhyming, punning, echolalia, clanging, word salad, paranoia, disorganization, and incoherence (table 3). How this set of symptoms derives instead from manic distractibility is considered below (figure 1).
Table 3.
Symptoms of Disordered Thought and Speech Traditionally Indicative of Schizophrenia or Mania
| Schizophreniaa | Mania |
| A disorder of thought | A disorder of mood |
| Delusions | Distractibility |
| Hallucinations | Racing thoughts |
| Disorganized speech | Flight of ideas |
| Disorganized behavior | Pressure of speech |
| Incoherence | Grandiosity |
| Paranoia | |
| Catatonia | |
| Tangentiality | |
| Circumstantiality | |
| Loose associations | |
| Derailment | |
| Blocking | |
| Echolalia | |
| Echopraxia | |
| Clanging | |
| Rhyming | |
| Punning | |
| Word salad | |
| Ideas of reference | |
| Ideas of influence |
Note that no single symptom or combination of symptoms is disease specific for schizophrenia, and all are more likely explained by the core manic symptom of distractibility.
In mild mania, the defect in the filter/prioritizer system is modest, allowing fairly appropriate evaluation of incoming data, but with reduced dampening of ideas and more activity than are usual for that individual. During this state, new ideas are triggered more readily and are expressed with less restriction and more confidence. Hypomanic patients typically become more productive in their areas of endeavor as well as in additional ventures. History demonstrates that some of the most famous and successful writers, composers, musicians, artists, generals, and politicians have suffered from bipolar mood disorder. When the filter/prioritizer mechanism becomes less discriminating, however, rationality and the quality of productivity decrease.
In moderately severe mania, sequential stimuli demand attention even though they are tangential, loose, or seemingly unrelated to the subject of a conversation. For example, during an initial diagnostic interview, a patient with moderate mania may attend to irrelevant stimuli from pictures on the wall, a clock, noises outside, the interviewer's tie, and other inappropriate distractions rather than the interviewer's questions. Redirection of the patient may become difficult due to increasing distractibility and irritability.
In severe mania, the brain's filter/prioritizer is very porous to inappropriate distractions. The ability to distinguish and thus to discard trivial sensory input is lost, and the manic brain seems to attempt to process and vocalize myriad stimuli (figure 1). This defect results in the experience of racing thoughts, flight of ideas, and confusion, typically described by manic patients and observed by the interviewer as a pressure of speech extending to disorganization and incoherence. New ideas and thoughts come so fast that even speaking as rapidly as possible, a patient may be able to express only a small percentage of them. Conversely, critical stimuli may be overlooked. Rational conversation becomes difficult because such patients are confused by sensory and thought overload, as demonstrated below.
Student Case Conference
The case of a 56-year-old married male, recently readmitted to the acute inpatient unit, was presented in a weekly student conference. He carried the diagnosis of schizophrenia, disorganized type. The student reported his presenting symptoms of derailment, loose associations, blocking, delusions, and gross disorganization of thoughts, speech, and behavior for over 6 months (table 1). He fulfilled DSM criteria for schizophrenia and demonstrated additional signs and symptoms usually associated with this diagnosis (table 4). After the student's presentation, the patient was invited into the conference room for an interview with the attending professor. About 2 minutes into the interview, as the patient answered a question about his mother, with a normal rhythm but a modest pressure, the professor “accidentally” knocked his key chain off the table. The patient stopped talking, remained silent for about 15 seconds, and then said, with appropriate emotion, “The pyramids are magnificent structures.” After another unusual pause, the patient said, “May I have a glass of water?” These appear to be textbook examples of “schizophrenic thought blocking,” understood as the sudden obstruction in or loss of a thought during a flow of speech, and observed as an unusual silence followed by the emergence of a totally unrelated subject. There is no apparent association between “mother,” “pyramids,” and wanting water. This presentation appeared to meet all the DSM criteria for schizophrenia, but the rule out for psychotic mood disorder had been overlooked.
Table 4.
Other Signs and Symptoms Often Thought Indicative of Schizophreniaa
| 1. Loner; poor premorbid personalityb |
| 2. Onset of psychotic illness in late adolescence or early adulthood |
| 3. Disorder of thought, formal thought disorder |
| 4. Derailment, tangentiality, loose associations, disorganization, blocking, incoherence, word salad, clanging, echolalia, echopraxia, speaking in tongues |
| 5. Catatonia |
| 6. Coprophagia, coprophilia |
| 7. Downward drift in society and employmentb |
| 8. Multiple, brief jobsb |
| 9. Street personb |
| 10. Ideas of control or reference, paranoiab |
| 11. Mood incongruent hallucinations and/or delusions |
None of these symptoms or combinations are disease specific for schizophrenia, and all occur frequently in severe mood disorders with psychotic features.
These signs and symptoms can overlap with the fringes of normal behavior or be caused by multiple circumstances.
The patient was asked by the attending professor to focus his attention and try to explain how his thoughts had jumped from discussing his mother to pyramids to wanting water. With some redirection, he was able to maintain focus to say that the key chain stimulated the thought of “the key of life” leading to the idea that life began in Egypt's Nile River valley. “Egypt” brought him to pyramids and how “magnificent” they must be. Egypt also stimulated the thought of a desert, of feeling hot and then thirsty, so he asked for a glass of water. This sequence of thoughts occurred in a matter of seconds.
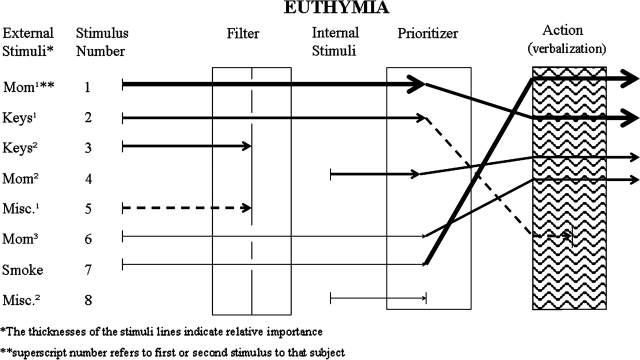
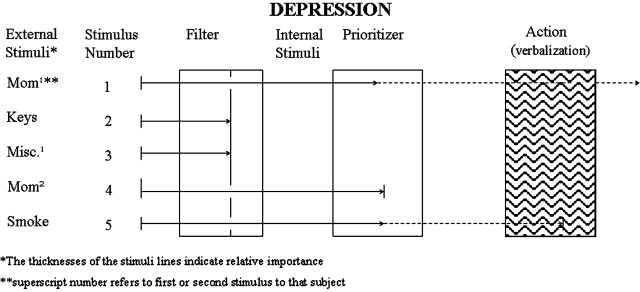
An analysis of what transpired in this interaction demonstrates distractibility, flight of ideas, and racing thoughts and may be explained by a defect in the selective attention function typical to mania (figure 1). The patient's filter/prioritizer failed to prevent his inappropriate distraction to and processing of “keys.” Because he was unable to maintain appropriate focus on the interviewer's questions about his mom, this theme was lost. Including the initial subject of “mom,” the extraneous stimulus of the attending professor's keys led to a cascade of at least 9 internally generated loosely associated ideas: (1) mom, (2) the professor's keys, (3) the key of life, (4) Egypt, (5) the magnificent pyramids, (6) the desert, (7) feeling hot, (8) being thirsty, and (9) wanting water. The patient's mind was racing to such an extent that he only had time to verbalize “pyramids are magnificent” and wanting water, items 5 and 9 (figure 1). Such a breakdown apparently allows so many thoughts to reach consciousness that there is no time to say them all. By the patient's report, there are connections to all his thoughts, but an observer is oblivious to the connections because only about 20% of his thoughts are verbalized, and none have any relationship to the subject of “mom.” During euthymia, distraction to the keys falling to the floor would usually be blocked at the filter or given such low priority that the interview subject of “mom” would continue appropriately and uninterrupted (figure 2). In depression, exclusion of stimuli may be increased (figure 3).
Fig. 2.
Selective Attention in Mood Disorders: Euthymia. In euthymia, the psychiatrist's questions about “mom” are prioritized and are not overridden by the “keys” (neither of the 2 keys stimuli 1 or 2) or by miscellaneous stimuli, 1 or 2. The first “keys (1)” stimulus is impactful enough to pass the filter but is shown as downgraded by the prioritizer function (second box), and there is no action or verbalization. A second “keys (2)” stimulus when the professor picked up his keys does not pass filtration. Internal stimulus 4 (mom 2) and external stimulus 6 (“mom 3” as in the form of another question from the interviewer) are appropriately prioritized and verbalized in continuing with the psychiatric interview. The dialogue about the topic of “mom” may last 5 minutes and is only overridden by a hypothetical stimulus, “smoke.” The sight or smell of smoke (stimulus 7) readily passes the filter and is highly prioritized. Note increase in line thickness and elevation to the top of the “action” box, receiving immediate attention above the “mom” topic.
Fig. 3.
Selective Attention in Mood Disorders: Depression. In depression, all cognitive processes appear to be slowed. A depressed patient may have difficulty maintaining focus on “mom” not because of subsequent interrupting stimuli but because of a defect in concentration associated with depression. Other stimuli may be inappropriately filtered out or receive an unwarranted reduction in prioritization. Stimulus 5, “smoke,” is shown as passing the filter but not receiving a high enough prioritization rank to produce an action. No internal stimuli are generated, in sharp contrast to the manic state where an excessive number of internal stimuli reach consciousness. In depression, only 5 stimuli may require 5–10 minutes with less comprehension than 8 stimuli in euthymia in the same time.
Bleuler and Schneider would interpret this interchange as thought blocking, loose associations, derailment, disorganization, and incoherence of thought and speech, leading to a diagnosis of schizophrenia,2,3 but these signs are also compatible with manic distractibility. Upon additional inquiry, the patient under discussion endorsed the DSM, disease-specific symptoms diagnostic of a manic episode (table 2).30 The significant other of the patient confirmed his manic symptoms.
In severe psychotic mania with more extensive damage to the filter/prioritizer mechanism, patients may only focus on words or sounds that rhyme or may only be able to say words or make sounds with no apparent relationship to one another. These disorganized and incoherent patterns of speech, called rhyming, punning, clanging, echolalia, and word salad, are traditionally associated with schizophrenia and not mania (table 3). An example of such manic incoherence comes from a recovered patient who said that, when manic, he had been able to focus on the first letter of each word spoken by others and to “make entire sentences beginning with each of those letters.” His speech had been incoherent (word salad) and his behavior, disorganized, delusional, and psychotic, yet he had felt organized. He met disease-specific DSM criteria for mania.30
Another extremely disorganized patient was brought to the emergency department (ED) by the police. He had been in the middle of a busy intersection gesturing frantically and speaking rapidly, nonstop in a “foreign language” or “in tongues” to any one or no one. In the ED, he continued to speak rapidly without pause but with a rhythm that indicated a potential for meaning. No English words were discernable. His affect was of extreme excitement and agitation. His wife denied that he spoke a foreign language and said that he had been in this mental state for 2 days without sleep or food. In retrospect, his initial diagnosis of disorganized schizophrenia was likely incorrect because he probably suffered from excited mania, severe with psychotic features. Such a presentation can be understood as a severe disintegration in the filter/prioritizer function. This case emphasizes the importance of considering a diagnosis of mania in disorganized individuals observed to be “speaking in tongues” and inappropriately “preaching.”
Defective Manic Sensory Processing Predisposes Grandiosity and Paranoia
The disease-specific manic symptom of grandiosity may also relate to this filter/prioritizer defect. In mania with psychotic features, the filter/prioritizer is so defective that judgment, insight, and the ability to discriminate reality from misperceptions and illusions are lost. Without adequate mechanisms to filter and evaluate data, illusions or misperceptions can be exaggerated to delusional fame, knowledge, and wealth. The occurrence of one such thought can stimulate an unfiltered sequence of progressively more grandiose delusions. Once manic patients are convinced they have special abilities, powers, ideas, knowledge, or wealth, the natural consequence is the occurrence of “paranoid delusions” that others want these possessions. Called “ideas of reference,” unrelated conversations or gestures by others in public, on television or radio, are personalized and are similarly misinterpreted and exaggerated as threatening. Such patients are dangerous because they may strike first, convinced they are in mortal danger. Because survival becomes the dominant focus, overriding and obscuring their grandiosity, patients' presenting complaints in the ED are fear and paranoia, not the grandiose delusions.31Ideas of reference and influence, held as pathognomonic of schizophrenia by Schneider3 and the current DSM (table 1),30 have been discounted as disease-specific symptoms because they occur frequently in psychotic bipolar patients.32–36 Pursuit of mood symptoms in such patients is critical because interviewer focus on the paranoid, psychotic symptoms can lead to the misdiagnosis of manic patients as schizophrenic, resulting in mismanagement.
Detrimental Effects of Misdiagnosis
Further confusing accurate diagnoses in psychotic patient is the observation that bipolar patients can suffer such severe and chronic psychotic symptoms that disturbances of mood are hidden for weeks at a time.11,12 Some physicians, assuming that psychosis means schizophrenia, may not aggressively pursue mood symptoms. The author concurs with Pope who said, “To misdiagnose schizophrenia as bipolar rarely does harm; to misdiagnose bipolar disorder as schizophrenia may adversely affect a patient's entire future.”32,33 The misdiagnosis of schizophrenia in patients with bipolar causes substantial negative outcomes, including pharmacological mismanagement. Once misdiagnosed as schizophrenic, the concept that schizophrenia is a lifelong disease inhibits reconsideration of both the diagnosis and a reduction in dosage of neurotoxic, antipsychotic medications.32,33 Most critical, bipolar patients misdiagnosed with schizophrenia are unlikely to receive mood-stabilizing medicines; without these, the rate of cycling increases and patients deteriorate related to kindling and excitotoxicity.11,12,34 The high rate of suicide in patients diagnosed with schizophrenia (misdiagnosed), because of psychotic symptoms, may reflect a lack of a trial on lithium, an effective antisuicide and antikindling medication. The potential for neurotoxic effects from antipsychotic medications is greater in patients diagnosed with schizophrenia because the antipsychotics are given in higher dosages and for longer periods of time than in patients diagnosed with bipolar.37 The impact of the stigma of the “schizo” prefix is substantial and lifelong. For psychotic patients who do not experience obvious mood symptoms, a temporary DSM diagnosis of psychotic disorder, Not Otherwise Specified,30 is recommended while obscure mood and/or organic explanations are explored further. There are many subtle organic causes of psychosis.37–39
Summary
Distractibility is an index of the severity of a core defect in information processing in the manic brain involving selective attention.18 This breakdown in mania leads to gross disorganization of thought and behavior, hallucinations, delusions, and incoherence and seems to explain most of, if not all, the signs and symptoms of disturbed thought, traditionally attributed to schizophrenia (tables 1, 3, and 4). The cognitive deficits in schizophrenia and bipolar share commonalities and overlap.18–21,28,29 Adding further doubt to the dichotomy of schizophrenia and bipolar and suggesting common neuropathology is a rapidly growing body of phenotypic and genotypic data from a wide array of basic science and preclinical fields such as neurochemistry,40–42 brain metabolism,43,44 imaging,45,46 epidemiology,47 cognitive function (selective attention/insight),14–23,28,29,48 and genetics49–59 that show considerable similarities and overlap. Molecular genetic results reveal 5–9 shared susceptibility loci.49,50,54–59 “The beginning of the end of the Kraepelinian dichotomy” has been predicted based on the phenotypic and genotypic overlap.57 Data that have supported the dichotomy or shown a bimodal distribution of discriminate scores with a natural discontinuity might be explained by differences between psychotic and nonpsychotic mood disorders, not 2 separate disorders. As recently stated, “ … the validity of the diagnostic distinction between schizophrenia and bipolar disorder is increasingly challenged …. The diagnostic split between schizophrenia and bipolar disorder is unable to define distinct etiological and/or pathophysiological entities.”60 and “Unfortunately, once a diagnostic concept such as schizophrenia … has come into general use, it tends to become reified. That is, people too easily assume that it is an entity of some kind that can be evoked to explain the patient's symptoms and whose validity need not be questioned.”61 Disordered thought and the functional psychoses can be accounted for by a single disorder, the disorder we currently diagnose as bipolar disorder. A correct differential diagnosis is critical because psychotic bipolar patients misdiagnosed with schizophrenia or schizoaffective disorder do not receive standard of care treatment.
Acknowledgments
The author would like to acknowledge Heather Nachbar, Martha Mundis, and Anita Swisher for technical support.
References
- 1.Kraepelin E. Clinical Psychiatry. New York, NY: William Wood Company; 1913. [Google Scholar]
- 2.Bleuler E. Dementia Praecox or the Group of Schizophrenias. New York, NY: International Universities Press; 1911. /1950. [Google Scholar]
- 3.Schneider K. Clinical Psychopathology. New York, NY: Grune & Stratton, Inc; 1959. [Google Scholar]
- 4.Kasanin J. The acute schizoaffective psychoses. Am J Psychiatry. 1933;13:97–126. [Google Scholar]
- 5.Pope HG, Lipinski JF. Diagnosis in schizophrenia and manic-depressive illness, a reassessment of the specificity of “schizophrenic” symptoms in the light of current research. Arch Gen Psychiatry. 1978;35:811–828. doi: 10.1001/archpsyc.1978.01770310017001. [DOI] [PubMed] [Google Scholar]
- 6.Lake CR, Hurwitz N. Schizoaffective disorders are psychotic mood disorders; there are no schizoaffective disorders. Psychiatry Res. 2006;143:255–287. doi: 10.1016/j.psychres.2005.08.012. [DOI] [PubMed] [Google Scholar]
- 7.Kendell RE, Gourlay J. The clinical distinction between the affective psychoses and schizophrenia. Br J Psychiatry. 1970;117:261–266. [PubMed] [Google Scholar]
- 8.Fowler RC, McCabe MS, Cadoret RJ, Winokur G. The validity of good prognosis schizophrenia. Arch Gen Psychiatry. 1972;26:182–185. doi: 10.1001/archpsyc.1972.01750200086018. [DOI] [PubMed] [Google Scholar]
- 9.Thomas P. The many forms of bipolar disorder: a modern look at an old illness. J Affect Disord. 2004;79:S3–S8. doi: 10.1016/j.jad.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 10.Abrams R, Taylor MA, Gaztanaga P. Manic-depressive illness and paranoid schizophrenia. Arch Gen Psychiatry. 1974;31:640–642. doi: 10.1001/archpsyc.1974.01760170040006. [DOI] [PubMed] [Google Scholar]
- 11.Goodwin FK. The biology of recurrence: new directions for the pharmacologic bridge. J Clin Psychiatry. 1989;50:40–44. [PubMed] [Google Scholar]
- 12.Post RM. Transduction of psychosocial stress into the neurobiology of recurrent affective disorder. Am J Psychiatry. 1992;149:999–1010. doi: 10.1176/ajp.149.8.999. [DOI] [PubMed] [Google Scholar]
- 13.Dieperink ME, Sands JR. Bipolar mania with psychotic features: diagnosis and treatment. Psychiatr Ann. 1996;26:633–637. [Google Scholar]
- 14.Zuibieta JK, Huguelet P, O'Neil RL, Giordani BJ. Cognitive function in euthymic bipolar I disorder. Psychiatry Res. 2001;102:9–20. doi: 10.1016/s0165-1781(01)00242-6. [DOI] [PubMed] [Google Scholar]
- 15.Martinez-Aran A, Vieta E, Reinares M, et al. Cognitive function across manic or hypomanic, depressed and euthymic states in bipolar disorder. Am J Psychiatry. 2004;161:262–270. doi: 10.1176/appi.ajp.161.2.262. [DOI] [PubMed] [Google Scholar]
- 16.Sweeney JA, Kmiec JA, Kupfer DJ. Neuropsychologic impairments in bipolar and unipolar mood disorders on the CANTAB neurocognitive battery. Biol Psychiatry. 2000;48:674–684. doi: 10.1016/s0006-3223(00)00910-0. [DOI] [PubMed] [Google Scholar]
- 17.Harvey PD, Docherty N, Serper MR, Rasmussen M. Cognitive deficits and thought disorder: II. An eight-month follow-up study. Schizophr Bull. 1990;16:147–156. doi: 10.1093/schbul/16.1.147. [DOI] [PubMed] [Google Scholar]
- 18.Oltmanns TF. Selective attention in schizophrenic and manic psychoses: the effect of distraction on information processing. J Abnorm Psychol. 1978;87:212–225. doi: 10.1037//0021-843x.87.2.212. [DOI] [PubMed] [Google Scholar]
- 19.Olincy A, Martin L. Diminished suppression of the P50 auditory evoked potential in bipolar disorder subjects with a history of psychosis. Am J Psychiatry. 2005;162:43–49. doi: 10.1176/appi.ajp.162.1.43. [DOI] [PubMed] [Google Scholar]
- 20.Politis A, Lykouras L, Mourtzouchou P, Christodoulou GN. Attentional disturbances in patients with unipolar psychotic depression: a selective and sustained attention study. Compr Psychiatry. 2004;45:452–459. doi: 10.1016/j.comppsych.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 21.Addington J, Addington D. Attentional vulnerability indicators in schizophrenia and bipolar disorder. Schizophr Res. 1997;23:197–204. doi: 10.1016/s0920-9964(96)00105-3. [DOI] [PubMed] [Google Scholar]
- 22.Tiihonen J, Haukka J, Henriksson M, et al. Premorbid intellectual functioning in bipolar disorder and schizophrenia: results from a cohort study of male conscripts. Am J Psychiatry. 2005;162:1904–1910. doi: 10.1176/appi.ajp.162.10.1904. [DOI] [PubMed] [Google Scholar]
- 23.McIntosh AM, Harrison LK, Forrester K, Lawrie SM, Johnstone EC. Neuropsychological impairments in people with schizophrenia or bipolar disorder and their unaffected relatives. Br J Psychiatry. 2005;186:378–385. doi: 10.1192/bjp.186.5.378. [DOI] [PubMed] [Google Scholar]
- 24.Benson KL. Sleep in schizophrenia: impairments, correlates, and treatment. Psychiatr Clin North Am. 2006;29:1033–1045. doi: 10.1016/j.psc.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 25.Costa e Silva JA. Sleep disorders in psychiatry. Metabolism. 2006;55:S40–S44. doi: 10.1016/j.metabol.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 26.Driver J. A selective review of selective attention research from the past century. Br J Psychiatry. 2001;92:53–78. [PubMed] [Google Scholar]
- 27.Posner ML, Petersen SE. The attention system of the human brain. Annu Rev Neurosci. 1990;13:25–42. doi: 10.1146/annurev.ne.13.030190.000325. [DOI] [PubMed] [Google Scholar]
- 28.Mialet JP, Pope HG. Impaired attention in depressive states: a non-specific deficit? Psychol Med. 1996;26:1009–1020. doi: 10.1017/s0033291700035339. [DOI] [PubMed] [Google Scholar]
- 29.David AS. Spatial and selective attention in the cerebral hemispheres in depression, mania, and schizophrenia. Brain Cogn. 1993;23:166–180. doi: 10.1006/brcg.1993.1053. [DOI] [PubMed] [Google Scholar]
- 30.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition-TR. Washington D.C.: American Psychiatric Association Press; 2000. [Google Scholar]
- 31.Lake CR. Paranoia hides grandiosity and guilt. Schizophr Bull. doi: 10.1093/schbul/sbm132. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pope HG. Distinguishing bipolar disorder from schizophrenia in clinical practice: guidelines and case reports. Hosp Community Psychiatry. 1983;34:322–328. doi: 10.1176/ps.34.4.322. [DOI] [PubMed] [Google Scholar]
- 33.Swartz CM. Schizophrenic schizophrenia. Psychiatr Times. 2002 Oct:47–51. [Google Scholar]
- 34.Carlson GA, Goodwin FK. The stages of mania. A longitudinal analysis of the manic episode. Arch Gen Psychiatry. 1973;28:221–228. doi: 10.1001/archpsyc.1973.01750320053009. [DOI] [PubMed] [Google Scholar]
- 35.Carpenter WT, Strauss JS. Are there pathognomonic symptoms in schizophrenia? An empiric investigation of Schneider's first-rank symptoms. Arch Gen Psychiatry. 1973;28:847–852. doi: 10.1001/archpsyc.1973.01750360069010. [DOI] [PubMed] [Google Scholar]
- 36.Gonzales-Pinto A, van Os J, Perez de Heredia JL, et al. Age-dependence of Schneiderian psychotic symptoms in bipolar patients. Schizophr Res. 2003;61:157–162. doi: 10.1016/s0920-9964(02)00320-1. [DOI] [PubMed] [Google Scholar]
- 37.Swartz CM. Tardive psychopathology. Neuropsychobiology. 1995;32:115–119. doi: 10.1159/000119222. [DOI] [PubMed] [Google Scholar]
- 38.Swartz CM. Misdiagnosis of schizophrenia for a patient with epilepsy. Psychiatr Serv. 2001;52:109–110. doi: 10.1176/appi.ps.52.1.109. [DOI] [PubMed] [Google Scholar]
- 39.Martin MJ. A brief review of organic diseases masquerading as functional illness. Hosp Community Psychiatry. 1983;34:328–332. doi: 10.1176/ps.34.4.328. [DOI] [PubMed] [Google Scholar]
- 40.Tkachev D, Minnack ML, Ryan MM, et al. Oligodendrocyte dysfunction in schizophrenia and bipolar disorder. Lancet. 2003;362:798–805. doi: 10.1016/S0140-6736(03)14289-4. [DOI] [PubMed] [Google Scholar]
- 41.McCullumsmith RE, Meador-Woodruff JH. Striatal excitatory amino acid transporter transcript expression in schizophrenia, bipolar disorder, and major depressive disorder. Neuropsychopharmacology. 2002;26:368–375. doi: 10.1016/S0893-133X(01)00370-0. [DOI] [PubMed] [Google Scholar]
- 42.Koh PO, Undie AS, Kabbani N, Levenson R, Goldman-Rakie PS, Lidow MS. Up-regulation of neuronal calcium sensor-1 (NCS-1) in the prefrontal cortex of schizophrenia and bipolar patients. Proc Natl Acad Sci USA. 2003;100:313–317. doi: 10.1073/pnas.232693499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.al-Mousawi AH, Evans N, Ebmeier KP, Roeda D, Chaloner F, Ashcroft GW. Limbic dysfunction in schizophrenia and mania. A study using 18F-labelled fluorodeoxyglucose and positron emission tomography. Br J Psychiatry. 1996;169:509–516. doi: 10.1192/bjp.169.4.509. [DOI] [PubMed] [Google Scholar]
- 44.Cohen RM, Semple WE, Gross M, et al. Evidence for common alterations in cerebral glucose metabolism in major affective disorders and schizophrenia. Neuropsychopharmacology. 1989;2:241–254. doi: 10.1016/0893-133x(89)90028-6. [DOI] [PubMed] [Google Scholar]
- 45.Bilder RM, Wu H, Bogerts B, et al. Cerebral volume asymmetries in schizophrenia and mood disorders: a quantitative magnetic resonance imaging study. Int J Psychophysiol. 1999;34:197–205. doi: 10.1016/s0167-8760(99)00077-x. [DOI] [PubMed] [Google Scholar]
- 46.Roy PD, Zipursky RB, Saint-Cyr JA, Bury A, Langevin R, Seeman MV. Temporal horn enlargement is present in schizophrenia and bipolar disorder. Biol Psychiatry. 1998;44:418–422. doi: 10.1016/s0006-3223(98)00105-x. [DOI] [PubMed] [Google Scholar]
- 47.Berrettini WH. Are schizophrenic and bipolar disorders related? A review of family and molecular studies. Biol Psychiatry. 2000;48:531–558. doi: 10.1016/s0006-3223(00)00883-0. [DOI] [PubMed] [Google Scholar]
- 48.Pini S, Cassano GB, Dell ‘Osso L, Amador XF. Insight into illness in schizophrenia, schizoaffective disorder, and mood disorders with psychotic features. Am J Psychiatry. 2001;158:122–125. doi: 10.1176/appi.ajp.158.1.122. [DOI] [PubMed] [Google Scholar]
- 49.Berrettini WH. Molecular linkage studies of bipolar disorders. Bipolar Disord. 2001;3:276–283. doi: 10.1034/j.1399-5618.2001.30603.x. [DOI] [PubMed] [Google Scholar]
- 50.Berrettini W. Evidence for shared susceptibility in bipolar disorder and schizophrenia. Am J Med Genet. 2003;123:59–64. doi: 10.1002/ajmg.c.20014. [DOI] [PubMed] [Google Scholar]
- 51.Schurhoff F, Szoke A, Meary A, et al. Familial aggregation of delusional proneness in schizophrenia and bipolar pedigrees. Am J Psychiatry. 2003;160:1313–1319. doi: 10.1176/appi.ajp.160.7.1313. [DOI] [PubMed] [Google Scholar]
- 52.Cardno AG, Rysdijk FV, Sham PC, Murray RM, McGuffin P. A twin study of genetic relationships between psychotic symptoms. Am J Psychiatry. 2002;159:539–545. doi: 10.1176/appi.ajp.159.4.539. [DOI] [PubMed] [Google Scholar]
- 53.Valles V, Van Os J, Guillamat R, et al. Increased morbid risk for schizophrenia in families of in-patients with bipolar illness. Schizophr Res. 2000;42:83–90. doi: 10.1016/s0920-9964(99)00117-6. [DOI] [PubMed] [Google Scholar]
- 54.Schulze TG, Ohlraun S, Czerski P, et al. Genotype-phenotype studies in bipolar disorder showing association between the DAOA/G30 locus and persecutory delusions: a first step toward a molecular genetic classification of psychiatric phenotypes. Am J Psychiatry. 2005;162:2101–2108. doi: 10.1176/appi.ajp.162.11.2101. [DOI] [PubMed] [Google Scholar]
- 55.Schumacher J, Jamra RA, Freudenberg J, et al. Examination f G72 and D-amino-acid oxidase as genetic risk factors for schizophrenia and bipolar affective disorder. Mol Psychiatry. 2004;9:203–207. doi: 10.1038/sj.mp.4001421. [DOI] [PubMed] [Google Scholar]
- 56.Hodgkinson CA, Goldman D, Jaeger J, et al. Disrupted in schizophrenia 1 (DISC1): association with schizophrenia, schizoaffective disorder and bipolar disorder. Am J Hum Genet. 2004;75:862–872. doi: 10.1086/425586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Craddock N, Owen MJ. The beginning of the end for the Kraepelinian dichotomy. Br J Psychiatry. 2005;184:384–386. doi: 10.1192/bjp.186.5.364. [DOI] [PubMed] [Google Scholar]
- 58.Craddock N, O'Donovan MC, Owen M. The genetics of schizophrenia and bipolar disorder dissecting psychosis. J MedGenet. 2005;42:193–204. doi: 10.1136/jmg.2005.030718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Park N, Juo SH, Cheng R, et al. Linkage analysis of psychosis in bipolar pedigrees suggests novel putative loci for bipolar disorder and shared susceptibility with schizophrenia. Mol Psychiatry. 2004;9:1091–1099. doi: 10.1038/sj.mp.4001541. [DOI] [PubMed] [Google Scholar]
- 60.Maier W, Zobel A, Wagner M. Schizophrenia and bipolar disorder: differences and overlaps. Curr Opinion Psychiatry. 2006;19:165–170. doi: 10.1097/01.yco.0000214342.52249.82. [DOI] [PubMed] [Google Scholar]
- 61.Kendell R, Jablensky A. Distinguishing between the validity and utility of psychiatric diagnoses. Am J Psychiatry. 2003;160:4–12. doi: 10.1176/appi.ajp.160.1.4. [DOI] [PubMed] [Google Scholar]