Abstract
Previous evidence reviewed in Schizophrenia Bulletin suggests the importance of a range of different environmental factors in the development of psychotic illness. It is unlikely, however, that the diversity of environmental influences associated with schizophrenia can be linked to as many different underlying mechanisms. There is evidence that environmental exposures may induce, in interaction with (epi)genetic factors, psychological or physiological alterations that can be traced to a final common pathway of cognitive biases and/or altered dopamine neurotransmission, broadly referred to as “sensitization,” facilitating the onset and persistence of psychotic symptoms. At the population level, the behavioral phenotype for sensitization may be examined by quantifying, in populations exposed to environmental risk factors associated with stress or dopamine-agonist drugs, (1) the increased rate of persistence (indicating lasting sensitization) of normally transient developmental expressions of subclinical psychotic experiences and (2) the subsequent increased rate of transition to clinical psychotic disorder.
Keywords: environment, psychosis, schizophrenia, mechanisms, mediators
Introduction
In previous issues of Schizophrenia Bulletin,1–9 evidence has been presented suggesting that environmental risk factors (prenatal stress/malnutrition/infection/hypoxia, paternal age, developmental trauma, urbanicity, cannabis, ethnic minority group, social fragmentation) may be associated with an increased risk for schizophrenia and psychotic symptoms, resulting in widespread geographical variation in incidence and prevalence.10 These studies have several themes in common that are summarized in box 1. It is clear that much remains to be clarified. For example, although the research on individual environmental risk factors is mostly consistent, effect sizes have been derived from bias and confounding-prone observational research. Also, none of the hypothesized factors are likely necessary or sufficient nor are they specific for psychosis outcomes. Finally, variables such as ethnic group, urbanicity, or prenatal maternal malnutrition merely represent proxies for one or more nongenetic factors that remain to be identified.
Box 1. Common Themes of Recent Reviews on the Link Between the Environment and Schizophrenia.
1. Most findings are derived from observational studies that can never conclusively exclude bias and confounding.
2. It is not clear to what degree genetic liability for psychosis is the origin of the environmental influence (eg, psychosis liability contributing to later cannabis use or maternal psychosis liability giving rise to pregnancy complications).
3. For the majority of environmental risk factors, the increase in risk is associated with exposure before adulthood, suggesting an interaction with developmental processes. For example, the risk-increasing effects of urbanicity, trauma, and cannabis use are limited to exposure during childhood and adolescence, suggesting they may create enduring liabilities that, in interaction with other factors, bring about psychotic disorder in adulthood.
4. Relative risks associated with environmental exposures are modest and none are likely necessary or sufficient. Indeed, for most, interactions with genetic risk factors are hypothesized and some gene-environment interactions using direct or indirect measures of genes and environments have been reported.
5. Many, if not most, of the environmental candidate factors represent proxies for as yet unidentified nongenetic effects. For example, while ethnic group and urbanicity can be readily used as categorical variables in statistical analyses, it is not known what underlying true environmental effect they may represent.
6. The evidence for a link between the environment and psychosis is for many risk factors, at least where this has been studied, not limited to the narrow syndrome of schizophrenia, but extending to broader psychometric expressions of psychosis in the form of psychotic-like symptoms or schizotypy.
7. None of the reported risk factors can claim a specific link to psychosis-all have been associated with a range of other psychiatric and somatic disorders.
Given these uncertainties, relatively little attention has been paid to what arguably constitutes the most challenging issue: is there any evidence for a plausible mechanism linking exposure to the environment to psychosis outcomes? How does the environment induce change in human beings so that enduring risk states or psychopathological outcomes may result? Rutter11 has argued that there are a number of ways in which the environment can impact on the individual to increase the risk for psychopathology, including effects on gene expression, effects on developmental programming of the brain, effects on neuroendocrine and neurotransmitter functioning, effects on patterns of interpersonal interactions that may shape risk for later psychopathology, and effects on affective and cognitive processing. Therefore, one way to validate the hypothesis of a link between the environment and psychosis is to examine to what degree the two may be plausibly linked to any of the above-mentioned cognitive or biological mechanisms. Given the fact that (1) it is unlikely that the extreme diversity of environmental influences associated with schizophrenia can be linked to as many different underlying mechanisms and (2) it has been suggested that environmental exposures in schizophrenia may induce psychological or physiological alterations that can be traced to a final common pathway of cognitive biases and/or altered dopamine neurotransmission,12–15 this particular suggestion will be examined in more detail, subsumed under the broad header of “sensitization.”
Sensitization
Sensitization refers to the observation that individuals who are exposed repeatedly to an environmental risk factor may develop progressively greater responses over time, finally resulting in a lasting change in response amplitude. It has been hypothesized that the process of sensitization is the substrate for the susceptibility to the psychosis-inducing effects of stress and dopamine-agonist drugs observed in patients with schizophrenia.13,16 Given the fact that many environmental exposures associated with schizophrenia may be linked to stress or dopamine-agonist drugs, sensitization may represent a common mechanism linking multiple environmental influences.
Sensitization: Cognitive and Affective Processing
Although the precise exposure under most environmental risk factors associated with schizophrenia remains unknown, many, including trauma, ethnic minority group, urbanicity, and social fragmentation, can be plausibly traced to “social defeat”–type psychological effects17 in the realm of interpersonal interactions. Such effects play a key role in recent cognitive models of psychosis.12,18–23 Early exposure to environmental risk factors such as developmental trauma and discrimination may shape specific negative beliefs about the self and about others. It has been hypothesized that such negative schemas and self-beliefs may predispose individuals to employ external attributions for negative events, possibly in order to protect the self from negative self-evaluative beliefs (delusion-as-a-defense theory).18,20,24 Indeed, studies have confirmed that psychotic individuals likely attribute negative events to external causes.18 Accordingly, dysfunctional beliefs and schemas may moderate the psychotogenic effect of later environmental risk factors, such as adverse life events, for psychosis. It has been argued that stressful events trigger particular emotional and cognitive changes, including automatic cognitive processes and maladaptive conscious appraisals. These, in combination with cognitive biases induced by earlier exposures, may be crucial in the formation and maintenance of positive symptoms of psychosis.12,25 Recent work examining these hypotheses has yielded some evidence that the path from childhood abuse or trauma to adult psychosis is mediated by disrupted self-representations and negative beliefs about others, as well as by alterations in meta-cognition that may predispose to psychosis.26–28 With the advent of sophisticated virtual reality (VR) techniques, researchers now can conduct controlled experiments in order to study, eg, how paranoia may arise from cognitive biases by observing how people interact with one another and interpret interpersonal behavior in controlled social situations. Early results show that people with paranoid thinking patterns interpret social signals abnormally.29 These VR experiments can be extended to test whether certain environmental exposures or, indeed, certain genotypes are associated with psychotic interpretations. If ethically acceptable, similar controlled experiments can be conducted using actual environmental exposures. For example, a recent experimental study showed that in individuals with a liability for psychosis, paranoid thoughts were exacerbated by a deprived urban environment.30
Sensitization: Behavioral Stress Sensitivity
It has been demonstrated that persons with a higher than average liability to psychosis are overreactive to small stressors, displaying an exaggerated affective response31 and increases in the intensity of subtle psychotic experiences associated with minor stresses in the flow of daily life.32 This effect may be described as behavioral sensitization because it has been shown to result, at least in part, from a sensitization process by which previous exposures to severe stress, such as childhood trauma33 or stressful life events,34 increase the sensitivity to small stresses in daily life, the cumulative impact of which might lead to the development of impairment and need for care.35 These findings therefore suggest that the effects of early stress may give rise to a lasting liability in the form of emotional and psychotic reactivity.
Sensitization: Dopamine Neurotransmission
Research has revealed that dopamine is released in response to stress in both animals36–38 and humans,39,40 although not all studies agree.41 Because dopamine is often regarded as the final common pathway of the factors involved in the causation of psychosis,13,42 it is attractive to speculate that dopamine plays a role in the pathway from environmental risk exposure to psychosis.
In animals, there is compelling evidence that disruptions in postnatal rearing conditions can lead to profound and lasting changes in the responsiveness of mesocorticolimbic dopamine neurons to stress and psychostimulants.43–45 A similar mechanism may exist in humans as well and provide an explanation for differential dopamine reactivity in those with and without psychosis liability.32,46 For example, a recent human study reported that mesolimbic dopamine release in response to psychosocial stress depended on low early life maternal care.40 In rodents, there is evidence that not only early life stress but also use of agonist drugs may induce sensitization of dopamine systems.44 Not only is there evidence for similar mechanisms in humans,47 studies also indicate that schizophrenia is associated with increased amphetamine-induced dopamine release.48
While these findings go some way toward validating the link between environmental exposures and psychosis, the precise mechanisms and neurocircuitry underlying stress-dopamine interactions and sensitization in schizophrenia remain unknown. There is evidence that mesocortical dopaminergic innervation of the prefrontal cortex (PFC) may regulate the activity of mesolimbic subcortical DA innervations and that the impact of environmental risk factors may result in taking the PFC “off-line,” resulting in altered responsiveness of subcortical dopaminergic innervations.49 Thus, when dopamine transmission is increased by exposure to stress or agonist drugs, there may be a shift in the balance of the system away from prefrontal cortical control and toward limbic predominance, facilitating the onset of psychotic symptoms.44,50 Genetic variation may act synergistically with environmental risk factors in shifting the balance between mesocortical and mesolimbic dopamine neurotransmission, explaining interactions between, eg, cannabis and the catechol-O-methyltransferaseval158met polymorphism.51,52 Other models for gene-environment interactions have been proposed. For example, it has been suggested that excessive levels of catecholamine release during stress impair PFC cognitive function through intracellular signaling pathways; schizophrenia may arise in individuals with mutations in DISC1 and RGS4, who may have weaker regulation of these intracellular stress pathways.53 Other factors may also play a role. For example, there is animal evidence that glucocorticoids may control stress-induced sensitization by changing the sensitivity of mesencephalic dopaminergic transmission to drugs of abuse.54 Similarly, prenatal stress, associated with schizophrenia,55 may induce changes in dopamine sensitivity of the nucleus accumbens and in the capacity to develop amphetamine-induced sensitization in adulthood, which may be mediated by impaired control of corticosterone secretion in the prenatally stressed animal.56 Finally, neurotransmitter sensitization may be associated with epigenetic mechanisms. Epigenetic factors are inherited and acquired modifications of DNA (eg, DNA methylation) and histones that occur without a change in nuclear DNA sequence but may impact on gene expression. The epigenetic state of a gene may be influenced by stress and drugs among other things and thus be considered a priori as an important factor mediating environment-schizophrenia relationships.57 Many studies have identified changes in mRNA levels in key areas involved in dopaminergic neurotransmission including the ventral tegmental area and the nucleus accumbens induced by dopamine-agonist drugs (including cannabis).58–61 Similarly, an epigenetic mechanism has been shown to mediate the relationship between variations in mother-infant interactions and the development of individual differences in behavioral and endocrine responses to stress in adulthood.62
Sensitization: Epidemiological Predictions
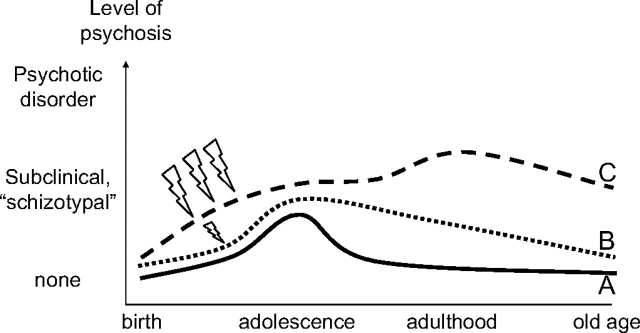
If environmental risk factors are causally associated with psychotic disorder and sensitization is the mechanism linking risk and outcome, then the challenge is to find a way to measure its behavioral phenotype and demonstrate epidemiological evidence that matches the hypothesis. Cougnard and colleagues63 suggested that the behavioral phenotype for sensitization may be examined at the population level by quantifying, in populations exposed to environmental risk factors associated with stress or dopamine-agonist drugs, (1) the increased rate of persistence (indicating lasting sensitization) of normally transient64–66 developmental expressions of subclinical psychotic experiences and (2) the subsequent increased rate of transition to clinical psychotic disorder (Fig. 1). In 2 large, prospective independent general population studies (Netherlands Mental Health Survey and Incidence Study [NEMESIS], n = 7076, and Early Developmental Stages of Psychopathology Study [EDSP], n = 3021), they examined the hypothesis that relatively common, subclinical developmental psychotic experiences would become abnormally persistent when synergistically combined with developmental exposures that may impact on sensitization such as cannabis, developmental trauma, and urbanicity. The authors found that the 3-year persistence rates of psychotic experiences were low at 26% in NEMESIS and 31% in EDSP. However, persistence rates were progressively higher with greater baseline number of environmental exposures in predicting follow-up psychotic experiences. The authors concluded that level of environmental risk combines synergistically with subclinical developmental expression of psychosis to cause abnormal persistence, reflecting a mechanism of sensitization.
Fig. 1.
Sensitization Behavioral Phenotype. Person A has “normal” developmental expression of subclinical psychotic experiences that are mild and transient. Person B has similar expression but longer persistence due to additional but mild environmental exposure. Person C has prolonged persistence due to severe repeated environmental exposure and subsequent transition to clinical psychotic disorder.
In a subsequent study, M. Dominguez, M. Wichers, R. Lieb, H.-U. Wittchen, J. van Os (unpublished data) went 1 step further and examined the hypothesis that the probability of poor outcome (in the sense of clinical psychotic disorder) of the normally transitory developmental expression of subclinical psychosis in the general population becomes progressively greater with more tendency to persistence over time. Expression of psychosis was assessed 4 times (T0–T3) over a period of 8.4 years in a sample of 845 adolescents from the general population. Transition from subclinical psychosis at T0–T2 to clinical psychosis at T3 was examined as a function of the level of prior persistence of the subclinical phenotype over T0–T2 (subclinical psychosis present never, once, twice, or thrice at T0, T1, and T2). The authors found that the more subclinical psychosis persisted over the period T0–T2, the greater the risk of transition to clinical psychosis at T3 in a dose-response fashion.
Conclusion
Although many questions remain, there is some evidence that environmental exposures may induce, in interaction with (epi)genetic factors, psychological or physiological alterations that can be traced to a final common pathway of cognitive biases and/or altered dopamine neurotransmission, broadly referred to as “sensitization,” facilitating the onset and persistence of psychotic symptoms. The behavioral phenotype for sensitization may be examined at the population level by quantifying, in populations exposed to environmental risk factors associated with stress or dopamine-agonist drugs, (1) the increased rate of persistence (indicating lasting sensitization) of normally transient developmental expressions of subclinical psychotic experiences and (2) the subsequent increased rate of transition to clinical psychotic disorder.
Funding
NWO VIDI grant to I. M.-G.; NWO Geestkracht grant to D. C.
References
- 1.Henquet C, Murray R, Linszen D, van Os J. The environment and schizophrenia: the role of cannabis use. Schizophr Bull. 2005;31:608–612. doi: 10.1093/schbul/sbi027. [DOI] [PubMed] [Google Scholar]
- 2.Morgan C, Fisher H. Environmental factors in schizophrenia: childhood trauma—a critical review. Schizophr Bull. 2007;33:3–10. doi: 10.1093/schbul/sbl053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fearon P, Morgan C. Environmental factors in schizophrenia: the role of migrant studies. Schizophr Bull. 2006;32:405–408. doi: 10.1093/schbul/sbj076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Allardyce J, Boydell J. Review: the wider social environment and schizophrenia. Schizophr Bull. 2006;32:592–598. doi: 10.1093/schbul/sbl008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Clarke MC, Harley M, Cannon M. The role of obstetric events in schizophrenia. Schizophr Bull. 2006;32:3–8. doi: 10.1093/schbul/sbj028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krabbendam L, van Os J. Schizophrenia and urbanicity: a major environmental influence—conditional on genetic risk. Schizophr Bull. 2005;31:795–799. doi: 10.1093/schbul/sbi060. [DOI] [PubMed] [Google Scholar]
- 7.Zammit S, Lewis S, Gunnell D, Smith GD. Schizophrenia and neural tube defects: comparisons from an epidemiological perspective. Schizophr Bull. 2007;33:853–858. doi: 10.1093/schbul/sbl041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown AS. Prenatal infection as a risk factor for schizophrenia. Schizophr Bull. 2006;32:200–202. doi: 10.1093/schbul/sbj052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Perrin MC, Brown AS, Malaspina D. Aberrant epigenetic regulation could explain the relationship of paternal age to schizophrenia. Schizophr Bull. 2007;33:1270–1273. doi: 10.1093/schbul/sbm093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McGrath JJ. Variations in the incidence of schizophrenia: data versus dogma. Schizophr Bull. 2006;32:195–197. doi: 10.1093/schbul/sbi052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rutter M. How the environment affects mental health. Br J Psychiatry. 2005;186:4–6. doi: 10.1192/bjp.186.1.4. [DOI] [PubMed] [Google Scholar]
- 12.Garety PA, Kuipers E, Fowler D, Freeman D, Bebbington PE. A cognitive model of the positive symptoms of psychosis. Psychol Med. 2001;31:189–195. doi: 10.1017/s0033291701003312. [DOI] [PubMed] [Google Scholar]
- 13.Howes OD, McDonald C, Cannon M, Arseneault L, Boydell J, Murray RM. Pathways to schizophrenia: the impact of environmental factors. Int J Neuropsychopharmacol. 2004;7:S7–S13. doi: 10.1017/S1461145704004122. [DOI] [PubMed] [Google Scholar]
- 14.Selten J-P, Cantor-Graaf E. Social defeat: risk factor for schizophrenia? Br J Psychiatry. 2005;187:101–102. doi: 10.1192/bjp.187.2.101. [DOI] [PubMed] [Google Scholar]
- 15.Myin-Germeys I, van Os J. Stress-reactivity in psychosis: evidence for an affective pathway to psychosis. Clin Psychol Rev. 2007;27:409–424. doi: 10.1016/j.cpr.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 16.Lieberman JA, Sheitman BB, Kinon BJ. Neurochemical sensitization in the pathophysiology of schizophrenia: deficits and dysfunction in neuronal regulation and plasticity. Neuropsychopharmacology. 1997;17:205–229. doi: 10.1016/S0893-133X(97)00045-6. [DOI] [PubMed] [Google Scholar]
- 17.Bjorkqvist K. Social defeat as a stressor in humans. Physiol Behav. 2001;73:435–442. doi: 10.1016/s0031-9384(01)00490-5. [DOI] [PubMed] [Google Scholar]
- 18.Bentall RP, Taylor JL. Psychological processes and paranoia: implications for forensic behavioral science. Behav Sci Law. 2006;24:277–294. doi: 10.1002/bsl.718. [DOI] [PubMed] [Google Scholar]
- 19.Fowler D, Freeman D, Smith B, et al. The Brief Core Schema Scales (BCSS): psychometric properties and associations with paranoia and grandiosity in non-clinical and psychosis samples. Psychol Med. 2006;36:749–759. doi: 10.1017/S0033291706007355. [DOI] [PubMed] [Google Scholar]
- 20.Freeman D. Suspicious minds: the psychology of persecutory delusions. Clin Psychol Rev. 2007;27:425–457. doi: 10.1016/j.cpr.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 21.Hacker D, Birchwood M, Tudway J, Meaden A, Amphlett C. Acting on voices: omnipotence, sources of threat, and safety-seeking behaviours. Br J Clin Psychol. [Epub ahead of print] October 23, 2007;10.1348/014466507X249093 doi: 10.1348/014466507X249093. [DOI] [PubMed] [Google Scholar]
- 22.Morrison AP, Wells A, Nothard S. Cognitive and emotional predictors of predisposition to hallucinations in non-patients. Br J Clin Psychol. 2002;41(pt 3):259–270. doi: 10.1348/014466502760379127. [DOI] [PubMed] [Google Scholar]
- 23.Peters ER, Joseph SA, Garety PA. Measurement of delusional ideation in the normal population: introducing the PDI (Peters et al. Delusions Inventory) Schizophr Bull. 1999;25:553–576. doi: 10.1093/oxfordjournals.schbul.a033401. [DOI] [PubMed] [Google Scholar]
- 24.Garety PA, Freeman D. Cognitive approaches to delusions: a critical review of theories and evidence. Br J Clin Psychol. 1999;38:113–154. doi: 10.1348/014466599162700. [DOI] [PubMed] [Google Scholar]
- 25.Garety PA, Bebbington P, Fowler D, Freeman D, Kuipers E. Implications for neurobiological research of cognitive models of psychosis: a theoretical paper. Psychol Med. 2007;37:1377–1391. doi: 10.1017/S003329170700013X. [DOI] [PubMed] [Google Scholar]
- 26.Finzi-Dottan R, Karu T. From emotional abuse in childhood to psychopathology in adulthood. J NervMent Dis. 2006;194:616–621. doi: 10.1097/01.nmd.0000230654.49933.23. [DOI] [PubMed] [Google Scholar]
- 27.Gracie A, Freeman D, Green S, et al. The association between traumatic experience, paranoia and hallucinations: a test of the predictions of psychological models. Acta Psychiatr Scand. 2007;116:280–289. doi: 10.1111/j.1600-0447.2007.01011.x. [DOI] [PubMed] [Google Scholar]
- 28.Bak M, Krabbendam L, Janssen I, de Graaf R, Vollebergh W, van Os J. Early trauma may increase the risk for psychotic experiences by impacting on emotional response and perception of control. Acta Psychiatr Scand. 2005;112:360–366. doi: 10.1111/j.1600-0447.2005.00646.x. [DOI] [PubMed] [Google Scholar]
- 29.Freeman D, Garety PA, Bebbington P, et al. The psychology of persecutory ideation II: a virtual reality experimental study. J Nerv Ment Dis. 2005;193:309–315. doi: 10.1097/01.nmd.0000161686.53245.70. [DOI] [PubMed] [Google Scholar]
- 30.Ellett L, Freeman D, Garety PA. The psychological effect of an urban environment on individuals with persecutory delusions: the Camberwell walk study. Schizophr Res. [Epub ahead of print] November 29, 2007 doi: 10.1016/j.schres.2007.10.027. 10.1016/j.schres.2007.10.027. [DOI] [PubMed] [Google Scholar]
- 31.Myin-Germeys I, Van Os J, Schwartz JE, Stone AA, Delespaul PA. Emotional reactivity to daily life stress in psychosis. Arch Gen Psychiatry. 2001;58:1137–1144. doi: 10.1001/archpsyc.58.12.1137. [DOI] [PubMed] [Google Scholar]
- 32.Myin-Germeys I, Marcelis M, Krabbendam L, Delespaul P, van Os J. Subtle fluctuations in psychotic phenomena as functional states of abnormal dopamine reactivity in individuals at risk. Biol Psychiatry. 2005;58:105–110. doi: 10.1016/j.biopsych.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 33.Glaser JP, van Os J, Portegijs PJ, Myin-Germeys I. Childhood trauma and emotional reactivity to daily life stress in adult frequent attenders of general practitioners. J Psychosom Res. 2006;61:229–236. doi: 10.1016/j.jpsychores.2006.04.014. [DOI] [PubMed] [Google Scholar]
- 34.Myin-Germeys I, Krabbendam L, Delespaul PA, Van Os J. Do life events have their effect on psychosis by influencing the emotional reactivity to daily life stress? Psychol Med. 2003;33:327–333. doi: 10.1017/s0033291702006785. [DOI] [PubMed] [Google Scholar]
- 35.Myin-Germeys I, van Os J. Stress-reactivity in psychosis: evidence for an affective pathway to psychosis. Clin Psychol Rev. 2007;27(4):409–424. doi: 10.1016/j.cpr.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 36.Abercrombie ED, Keefe KA, DiFrischia DS, Zigmond MJ. Differential effect of stress on in vivo dopamine release in striatum, nucleus accumbens, and medial frontal cortex. J Neurochem. 1989;52:1655–1658. doi: 10.1111/j.1471-4159.1989.tb09224.x. [DOI] [PubMed] [Google Scholar]
- 37.Tidey JW, Miczek KA. Social defeat stress selectively alters medocorticolimbic release: an in vivo microdialysis study. Brain Res. 1996;721:140–149. doi: 10.1016/0006-8993(96)00159-x. [DOI] [PubMed] [Google Scholar]
- 38.Gresch PJ, Sved AF, Zigmond MJ, Finlay JM. Stress-induced sensitization of dopamine and norepinephrine efflux in medial prefrontal cortex of the rat. J Neurochem. 1994;63:575–583. doi: 10.1046/j.1471-4159.1994.63020575.x. [DOI] [PubMed] [Google Scholar]
- 39.Wand GS, Oswald LM, McCaul ME, et al. Association of amphetamine-induced striatal dopamine release and cortisol responses to psychological stress. Neuropsychopharmacology. 2007;32:2310–2320. doi: 10.1038/sj.npp.1301373. [DOI] [PubMed] [Google Scholar]
- 40.Pruessner JC, Champagne F, Meaney MJ, Dagher A. Dopamine release in response to a psychological stress in humans and its relationship to early life maternal care: a positron emission tomography study using [11C]raclopride. J Neurosci. 2004;24:2825–2831. doi: 10.1523/JNEUROSCI.3422-03.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Montgomery AJ, Mehta MA, Grasby PM. Is psychological stress in man associated with increased striatal dopamine levels?: a [11C]raclopride PET study. Synapse. 2006;60:124–131. doi: 10.1002/syn.20282. [DOI] [PubMed] [Google Scholar]
- 42.Kapur S. Psychosis as a state of aberrant salience: a framework linking biology, phenomenology, and pharmacology in schizophrenia. Am J Psychiatry. 2003;160:13–24. doi: 10.1176/appi.ajp.160.1.13. [DOI] [PubMed] [Google Scholar]
- 43.Brake WG, Zhang TY, Diorio J, Meaney MJ, Gratton A. Influence of early postnatal rearing conditions on mesocorticolimbic dopamine and behavioural responses to psychostimulants and stressors in adult rats. Eur J Neurosci. 2004;19:1863–1874. doi: 10.1111/j.1460-9568.2004.03286.x. [DOI] [PubMed] [Google Scholar]
- 44.Pani L, Porcella A, Gessa GL. The role of stress in the pathophysiology of the dopaminergic system. Mol Psychiatry. 2000;5:14–21. doi: 10.1038/sj.mp.4000589. [DOI] [PubMed] [Google Scholar]
- 45.Hall FS, Wilkinson LS, Humby T, Robbins TW. Maternal deprivation of neonatal rats produces enduring changes in dopamine function. Synapse. 1999;32:37–43. doi: 10.1002/(SICI)1098-2396(199904)32:1<37::AID-SYN5>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 46.Soliman A, O'Driscoll GA, Pruessner JC, Holahan AL, Boileau I, Gagnon D, et al. Stress-induced dopamine release in humans at risk of psychosis: a [(11)C]raclopride PET study. Neuropsychopharmacology. Advance Online publication October 24, 2007 doi: 10.1038/sj.npp.1301597. 10.1038/sj.npp.1301597. [DOI] [PubMed] [Google Scholar]
- 47.Boileau I, Dagher A, Leyton M, et al. Modeling sensitization to stimulants in humans: an [11C]raclopride/positron emission tomography study in healthy men. Arch Gen Psychiatry. 2006;63:1386–1395. doi: 10.1001/archpsyc.63.12.1386. [DOI] [PubMed] [Google Scholar]
- 48.Laruelle M. The role of endogenous sensitization in the pathophysiology of schizophrenia: implications from recent brain imaging studies. Brain Res Rev. 2000;31:371–384. doi: 10.1016/s0165-0173(99)00054-5. [DOI] [PubMed] [Google Scholar]
- 49.Deutch AY, Clark WA, Roth RH. Prefrontal cortical dopamine depletion enhances the responsiveness of mesolimbic dopamine neurons to stress. Brain Res. 1990;521:311–315. doi: 10.1016/0006-8993(90)91557-w. [DOI] [PubMed] [Google Scholar]
- 50.Goto Y, Otani S, Grace AA. The Yin and Yang of dopamine release: a new perspective. Neuropharmacology. 2007;53:583–587. doi: 10.1016/j.neuropharm.2007.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Caspi A, Moffitt TE, Cannon M, et al. Moderation of the effect of adolescent-onset cannabis use on adult psychosis by a functional polymorphism in the catechol-O-methyltransferase gene: longitudinal evidence of a gene X environment interaction. Biol Psychiatry. 2005;57:1117–1127. doi: 10.1016/j.biopsych.2005.01.026. [DOI] [PubMed] [Google Scholar]
- 52.Henquet C, Rosa A, Krabbendam L, et al. An experimental study of catechol-o-methyltransferase Val(158)Met moderation of delta-9-tetrahydrocannabinol-induced effects on psychosis and cognition. Neuropsychopharmacology. 2006;31(12):2748–2757. doi: 10.1038/sj.npp.1301197. [DOI] [PubMed] [Google Scholar]
- 53.Arnsten AF. Catecholamine and second messenger influences on prefrontal cortical networks of “representational knowledge”: a rational bridge between genetics and the symptoms of mental illness. Cereb Cortex. 2007;17(suppl 1):i6–15. doi: 10.1093/cercor/bhm033. [DOI] [PubMed] [Google Scholar]
- 54.Deroche V, Marinelli M, Maccari S, Le Moal M, Simon H, Piazza PV. Stress-induced sensitization and glucocorticoids. I. Sensitization of dopamine-dependent locomotor effects of amphetamine and morphine depends on stress-induced corticosterone secretion. J Neurosci. 1995;15:7181–7188. doi: 10.1523/JNEUROSCI.15-11-07181.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Van Os J, Selten J-P. Prenatal exposure to maternal stress and subsequent schizophrenia: the May 1940 invasion of The Netherlands. Br J Psychiatry. 1998;172:324–326. doi: 10.1192/bjp.172.4.324. [DOI] [PubMed] [Google Scholar]
- 56.Sorg BA, Kalivas PW. Effects of cocaine and footshock stress on extracellular dopamine levels in the ventral striatum. Brain Res. 1991;559:29–36. doi: 10.1016/0006-8993(91)90283-2. [DOI] [PubMed] [Google Scholar]
- 57.Tsankova N, Renthal W, Kumar A, Nestler EJ. Epigenetic regulation in psychiatric disorder. Nat Rev. 2007;8:355–367. doi: 10.1038/nrn2132. [DOI] [PubMed] [Google Scholar]
- 58.Freeman WM, Brebner K, Lynch WJ, et al. Changes in rat frontal cortex gene expression following chronic cocaine. Brain Res Mol Brain Res. 2002;104:11–20. doi: 10.1016/s0169-328x(02)00197-3. [DOI] [PubMed] [Google Scholar]
- 59.McClung CA, Nestler EJ. Regulation of gene expression and cocaine reward by CREB and DeltaFosB. Nat Neurosci. 2003;6:1208–1215. doi: 10.1038/nn1143. [DOI] [PubMed] [Google Scholar]
- 60.Villares J. Chronic use of marijuana decreases cannabinoid receptor binding and mRNA expression in the human brain. Neuroscience. 2007;145:323–334. doi: 10.1016/j.neuroscience.2006.11.012. [DOI] [PubMed] [Google Scholar]
- 61.Yao WD, Gainetdinov RR, Arbuckle MI, et al. Identification of PSD-95 as a regulator of dopamine-mediated synaptic and behavioral plasticity. Neuron. 2004;41:625–638. doi: 10.1016/s0896-6273(04)00048-0. [DOI] [PubMed] [Google Scholar]
- 62.Weaver IC, Cervoni N, Champagne FA, et al. Epigenetic programming by maternal behavior. Nat Neurosci. 2004;7:847–854. doi: 10.1038/nn1276. [DOI] [PubMed] [Google Scholar]
- 63.Cougnard A, Marcelis M, Myin-Germeys I, et al. Does normal developmental expression of psychosis combine with environmental risk to cause persistence of psychosis? A psychosis proneness-persistence model. Psychol Med. 2007;37:513–527. doi: 10.1017/S0033291706009731. [DOI] [PubMed] [Google Scholar]
- 64.Hanssen M, Bak M, Bijl R, Vollebergh W, van Os J. The incidence and outcome of subclinical psychotic experiences in the general population. Br J Clin Psychol. 2005;44(pt 2):181–191. doi: 10.1348/014466505X29611. [DOI] [PubMed] [Google Scholar]
- 65.Wiles NJ, Zammit S, Bebbington P, Singleton N, Meltzer H, Lewis G. Self-reported psychotic symptoms in the general population: results from the longitudinal study of the British National Psychiatric Morbidity Survey. Br J Psychiatry. 2006;188:519–526. doi: 10.1192/bjp.bp.105.012179. [DOI] [PubMed] [Google Scholar]
- 66.Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H. Children's self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch Gen Psychiatry. 2000;57:1053–1058. doi: 10.1001/archpsyc.57.11.1053. [DOI] [PubMed] [Google Scholar]