Abstract
The TIPS early intervention program reduced the duration of untreated psychosis (DUP) in first-episode schizophrenia from 16 to 5 weeks in a health care sector using a combination of easy access detection teams (DTs) and a massive information campaign (IC) about the signs and symptoms of psychosis. This study reports what happens to DUP and presenting schizophrenia in the same health care sector when the IC is stopped. Methods: Using an historical control design, we compare 2 cohorts of patients with first-episode Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition, non-affective psychosis at admission to treatment. The first cohort (N = 108) was recruited from January 1997 to December 2000, using an IC to raise awareness about recognizing psychosis to the public, the schools, and to general practitioners. The second cohort (N = 75) was recruited from January 2002 to June 2004 with no-IC. Easy access DTs were available to both cohorts. Results: In the no-IC period, DUP increased back up to 15 weeks (median) and fewer patients came to clinical attention through the DTs. No-IC patients were diagnosed less frequently with schizophreniform disorder, more Positive and Negative Syndrome Scale positive and total symptoms, and poorer Global Assessment of Functioning (symptom) Scale scores. Conclusions: Intensive education campaigns toward the general public, the schools, and the primary health care services appear to be an important and necessary part of an early detection program. When such a campaign was stopped, there was a clear regressive change in help-seeking behavior with an increase in DUP and baseline symptoms.
Keywords: first-episode psychosis, early intervention, schizophrenia
Introduction
Duration of untreated psychosis (DUP) has emerged as an important parameter in studies of early detection of first-episode psychosis, insofar as long DUP appears to be a risk factor for poorer treatment response and outcome according to 2 recent meta-analyses.1,2
In the early Treatment and Intervention in Psychosis (TIPS) study of 1997–2000 (hereafter referred to as TIPS I), patients with first-episode psychosis were compared between 4 health care sectors in Norway and Denmark. Two of the health care sectors in Norway serving the county of Rogaland were early detection sectors. The TIPS I early detection program in Rogaland County consisted of 2 major elements. The first was intensive information campaigns (ICs) targeting the general public, schools, and general practitioners (GPs) with information about how to recognize the signs and symptoms of psychosis. The second was low-threshold early detection teams (DTs) that could be contacted directly by anyone. They were located within the county psychiatric system in order to facilitate case finding, evaluation, and triage. The 2 other health care sectors (Ullevaal sector in Oslo, Norway, and Roskilde in Denmark) were “control” sectors, recruiting patients in the usual fashion, meaning patients were most often triaged to inpatient or outpatient care via the GPs.
As previously reported,3 the TIPS I program successfully reduced DUP and the difference between experimental and control sites was significant (median 5 weeks vs median 16 weeks, respectively). Furthermore, at baseline the early detection patients presented with less severe psychotic symptoms and milder functional deficits (prior to treatment). Thus, the TIPS I study was the first to demonstrate that DUP could be reduced significantly and that this reduction was associated with clinical advantages at intake.
One question not addressed by the TIPS I study was which elements of the early detection program were particularly effective in reducing DUP. Specifically, was it the ICs or the DTs that were key? The cessation of the IC when the TIPS I study was finished in 2000 provided an opportunity to test this question. Specifically, on January 1, 2001, the TIPS I study, and thereby also the intensive IC, came to an end in Rogaland County. One DT, however, was maintained in the southern sector of Rogaland County. This dismantling of the IC but not the DT offered an opportunity to estimate the contribution of the IC to the early detection effect achieved in TIPS I, provided that the first-episode psychosis patients continued to be recruited for research assessment.
On January 1, 2002, 1 year after the IC in the TIPS I project had been stopped, a new sample of first-episode psychiatric patients began to be recruited (TIPS II). The intake criteria, assessment methodology, standard treatment package, DT, and follow-along protocol3 were identical with TIPS I, and the overlap of staff research and clinical personnel was substantial.
Our hypothesis was that discontinuing the IC would lead to recruiting a first-episode sample with longer DUP and more psychopathology at baseline.
METHODS
Setting
We compare 2 samples of first-episode nonaffective psychosis from the same geographical area (south sector of Rogaland County, Norway). The sector population of 290 000 lives mainly in urban and suburban areas. All first-episode patients were assessed by trained personnel within a week of contact and assigned without delay to the standard treatment program (consisting of standardized antipsychotic medication, multifamily work, and active outreach-supportive psychotherapy). Recruitment of patients in the TIPS II no-IC time period (January 1, 2002, to June 30, 2004) was conducted in the south sector of the Rogaland County health care system where the DT still existed. This consecutive sample (N = 75) is compared with the patients from the south sector of Rogaland TIPS I project when the IC was active (N = 108).
Information Campaigns
The public mass media campaign had 3 aims: teaching the general public about early signs of first psychosis, informing the public about the importance of getting help early, and educating the public about the existence of the DTs. The IC program tried to enhance the public's knowledge of psychiatric disorders in general and on early signs of psychotic disorders in particular and to change the help-seeking behavior of the population. The IC program consisted of multifaceted educational campaigns about psychotic symptoms and their treatment aimed at the general population, schools (teachers and pupils), and health professionals. Newspapers advertisements, intensively used, have been the most important message carrier. In addition to use of local newspapers, we also produced brochures, posters, commercials on cinema, local TV, and local radio stations. A web page was designed primarily as service to other professionals and as a base where people could get information about the project. Prior to the launch of the study in January 1997, an advertising campaign consisting of full-page advertisements in the local newspapers was carried out in December 1996. In addition to this, 80% (N = 300) of the county's GPs underwent a special educational program (4 hours) about diagnostics of early signs of psychosis and the structures available for early triage and easy access. In the second campaign which consisted of 6 whole-page newspaper advertisements during the period of January to May 1997, we introduced the “slogan,” which has followed the marketing campaigns the entire period; “Seek help as early as possible and you have the best chance to recover.” In January 1997, a brochure was distributed to all households in the county. This contained a presentation of all the topics from the advertisements, with emphasis on symptoms, available treatment, and the importance of seeking help at an early stage. A small brochure, the size of a business card, was disturbed to GPs, health workers, schools, and other places where it was natural to hand them out. In the autumn of 1997, we launched a school campaign. The main objective of this campaign was to provide knowledge about psychosis to teachers in the high schools. This has mainly been done through courses and lectures supported with advertisements and other material to support. The county's 45 high schools (approximately 1000 teachers) have all been visited on an annual basis and offered a special educational program of lectures and videos during the project period. A brochure and special designed posters were made for distribution to schools. The brochure contained a list of symptoms and comparison between warning signs and passing problems typical for adolescence. Specially designed newspaper advertisements aimed at teachers and pupils were provided. This campaign was repeated on a yearly basis during the years of 1997–2000. In addition, other public relation strategies such as free postcards in restaurants, flyers, car stickers, t-shirts, and other brochures were made available to collaborate partners. In the experimental period, a total of 26 whole-page newspaper advertisements were provided. Social workers, local community psychiatric nurses, and GPs were all offered a yearly seminar, either in their own locations or at the hospital with focus on early intervention and information about the project status.
Detection Teams
The second component in the early detection program was the low-threshold DTs. Each team consisted of 5 full-time professionals (1 psychiatrist, 1 psychologist, 2 psychiatric nurses, and 1 social worker) who were on call from 8:00 AM till 3:30 PM Monday through Friday. The teams were mobile and worked with an active outreach esprit. For any referral suspected of being in a first psychosis, a face-to-face interview was conducted within 24 hours and individuals with manifest psychosis would be referred to start treatment right away. The early detection program is described in detail elsewhere.4,5
The TIPS II program continued the DT but discontinued the IC. From the year 2001, a favorable contract was made with the largest newspaper in the sector making it possible to offer a small advertisement, size 5 × 10 cm, with text only trying to draw the attention of the general public if someone suspected a family member or themselves of suffering of possible psychosis to make contact with the DT. The advertisements provided telephone number to the DT. These advertisements were provided on an irregular basis when the paper had available advertisement space in the pages. There were no structured educational activities toward GPs or schools in the no-IC.
Subjects
The study includes all eligible patients meeting study criteria and signing informed consent. Participants agreed to undergo clinical assessment at baseline and to be followed up after 3 months and 1, 2, and 5 years. This article reports on the admission (baseline) data.
Inclusion criteria were identical to the TIPS I criteria and consisted of living in the catchment area (south sector, Rogaland County); age 15–65 years; meeting the Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV), criteria for schizophrenia, schizophreniform disorder, schizoaffective disorder (core schizophrenia-spectrum disorders) or brief psychotic episode, delusional disorder, affective psychosis with mood-incongruent delusions, or psychotic disorder not otherwise specified; being actively psychotic, as measured by a Positive and Negative Syndrome Scale (PANSS) score6 of 4 or more on at least one of the following PANSS items—P1 (delusions), P3 (hallucinations), P5 (grandiose thinking), P6 (suspiciousness), and A9 (unusual thought content); not previously receiving adequate treatment for psychosis (defined as antipsychotic medication of 3.5 haloperidol equivalents for 12 weeks or until remission of the psychotic symptoms); no neurological or endocrine disorders with relationship to the psychosis; no contraindications to antipsychotic medication; understands/speaks one of the Scandinavian languages; IQ over 70 (Wechsler Adult Intelligence Scale); willing and able to give informed consent.
Assessment Instruments
The Structured Clinical Interview for the DSM-IV Axis I Disorders7 was used for diagnostic purposes. Symptom levels were measured by means of the PANSS. Global functioning was measured by the Global Assessment of Functioning (GAF) Scale,8 and the scores were split into symptom (GAFs) and function (GAFf) scores. Misuse of alcohol and other drugs was measured by the Drake Scale.9 The DUP was measured as the time from onset of psychosis until the start of adequate treatment. Onset of psychosis was equated with the first appearance of positive psychotic symptoms, defined as the first week with symptoms corresponding to a PANSS score of 4 or more on positive subscale items 1, 3, 5, or 6 or on general subscale item 9. When we were measuring long DUP cases, all available data sources were used to ascertain the length of this period to the best achievable level, including semi-structured personal interviews with patients and relatives. Adequate treatment was defined as the start of structured treatment with antipsychotic medications, start of hospitalization, or the start of outpatient clinic psychotherapy designed to manage psychotic symptoms. Premorbid functioning was measured by the Premorbid Adjustment Scale,10 covering 2 areas of functioning—school adaptation and socialization—described as initial childhood level and subsequent change.11
Assessment Raters
The assessment team for the no-IC sample almost completely overlapped with the team for the original TIPS project, with the exception of one new psychologist. The team consisted of clinically experienced and trained research personnel who performed all evaluations.12
The raters for the IC sample were all previously trained to reliability in the use of the study instruments. Reliability of measurements for that sample ranged from fair to very good (DUP, 0.99; GAFs score, 0.63; GAFf score, 0.75; drug abuse, 0.88; alcohol abuse, 0.88; PANSS positive sum score, 0.88; PANSS negative sum score, 0.76; and PANSS general sum score, 0.56 [all intraclass correlations, 1.1]; for diagnostic categories, K = 0.76).3,12 In the no-IC period (2002–2004), a new interrater reliability scores were obtained for central measures from 17 randomly selected clinical vignettes from the baseline data. Reliability of measurements ranged from poor to very good (DUP, 0.99; GAFs score, 0.68; GAFf score, 0.45; drug abuse, 0.67; alcohol abuse, 0.81 [all intraclass correlations, 1.1]; for diagnostic categories, K = 0.58). The GAFf score was removed from further analyses due to poor reliability.
The study was approved by the regional ethical committee. After completely describing the study to the subjects, written informed consent was obtained. Demographic and diagnostic information regarding nonparticipants was gathered anonymously for the purpose of bias testing.
Statistical Analyses
Analyses were performed with the statistical package SPSS (version 13.0; SPSS Inc, Chicago, IL). Continuous data were represented as mean with SD and analyzed using Student t test. Categorical variables were analyzed using chi-square or Fisher exact test. All tests were 2 tailed, and statistical significance was defined as P ≤ .05. As noted in several studies, the DUP does not seem to have a normal distribution, and all analyses that included the DUP were nonparametric using Wilcoxon-Mann-Whitney test if possible. Log-transformed DUP was used in the regression analyses.
A multiple linear regression analysis was performed in order to investigate the prediction of symptoms and to investigate whether differences between the TIPS I IC and TIPS II no-IC samples were due to confounding factors at baseline. The multiple linear regression analyses were performed hierarchically in several steps. First, all variables were entered that previously had showed group differences, that had a significant bivariate relationship to the dependent variable in the IC sample, or that demonstrated potential predictive power.3 Because the multivariate procedures included a large number of variables (eg, demographics, premorbid academic and social adjustment, diagnostics, core schizophrenia-spectrum disorders, schizophrenia, schizophreniform disorder, schizoaffective disorder, drug abuse, and DUP), these variables were entered in a forward procedure in the first block. The IC vs no-IC variable was entered in a forward procedure in a second block. Only the final model is presented herein. The GAFs score was chosen as the dependent variable representing clinical status. There were no differences regarding main results if the GAFs score was exchanged with the PANSS positive or the PANSS total symptom scores in complementary analyses. These analyses are not presented herein.
Results
Persons with psychosis-like symptoms seeking help from the specialized psychiatric services underwent screening by the study's assessment team (36/100 000 per year). There were 229 study-appropriate patients for both samples (IC = 135, no-IC = 94). There were no significant differences between IC study–appropriate and no-IC–study appropriate patient samples for age, gender, and fraction of the sample receiving a core schizophrenia diagnosis. Of the study-appropriate patients, 46 refused to enter the study (IC = 27, no-IC = 19). There was no significant difference in the rate of refusal or in DUP between the IC and no-IC refusal samples.
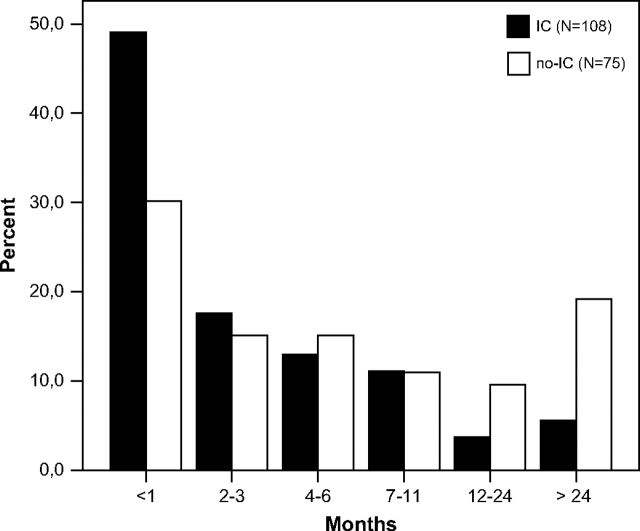
The TIPS I IC sample (N = 108) was recruited over a period of 48 months, and the TIPS II no-IC sample (N = 75) was recruited over a period of 30 months. DUP was longer in the no-IC period (table 1 and figure 1). There were no differences between the samples regarding incidence, age, gender distribution, cultural background, marital status, and length of education. The fraction of included patients first identified by the DT was less in the no-IC period.
Table 1.
Patient Characteristics at Start of First Treatment
| No-IC (n = 75) | IC (n = 108) | |
| Recruitment period, mo | 30 | 48 |
| DUP, wk mean/median (SD) | 105/15(275.8) | 26/5 (58.6)** |
| Incidence first-episode psychosis (n/100 000 per year) | 10.5 | 9.3 |
| Age, mean (SD), y | 26.4 (10.8) | 24.4 (7.5) |
| Females, No. (%) | 28 (37.0) | 42 (39.0) |
| Scandinavian background, No. (%) | 68 (94.0) | 104 (96.0) |
| Marital status, No. (%)a | ||
| Single | 52 (75.5) | 83 (80.6) |
| Divorced, separated, or widowed | 6 (7.6) | 4 (3.8) |
| Married or cohabiting | 11 (15.9) | 16 (15.6) |
| Educationb | ||
| Length, mean (SD), y | 11.7 (2.7) | 11.9 (2.1) |
| High school, No. (%) | 36 (53.7) | 62 (62.6) |
| College, No. (%) | 4 (6.0) | 10 (10.3) |
| University, No. (%) | 4 (6.1) | 7 (7.2) |
| Referred by detection team, No. (%) | 11 (14.7) | 34 (31.5)* |
Note: No-IC, no information campaigns; IC, information campaigns; DUP, duration of untreated psychosis.
*P = .009, Pearson chi-square test; **P < .005, Mann-Whitney U test. (2 tailed).
For the IC sample, n = 102; for the no-IC sample, n = 70.
For the IC sample, n = 100, for the no-IC sample n = 70.
Fig. 1.
Distribution of Duration of Untreated Psychosis (DUP). The bars presented in the figure represents different values for time. The figure represents percentage of cases over the 2 periods for different DUP categories.
Clinical status at the start of first treatment is shown in table 2. There were no differences between IC and no-IC patients in terms of diagnostic distribution, except that a significantly smaller proportion of the no-IC patients had schizophreniform disorder. The no-IC patients had significantly greater severity of positive PANSS symptoms, a higher total PANSS score, and a lower GAFs level (ie, more severe) than the IC patients. For the premorbid domains, no significant differences between IC and no-IC were found.
Table 2.
Clinical Status at Start of First Treatment
| No-IC (n = 75) | IC (n = 108) | |||
| Diagnostic distribution, No. (%) | ||||
| Schizophrenia | 24 | (32.0) | 29 | (26.9) |
| Schizophreniform disorder | 6 | (8.0) | 27 | (25.0)* |
| Others | 45 | (60) | 52 | (48) |
| Alcohol abuse, No. (%)a | 5 | (7.0) | 16 | (14.8) |
| Drug abuse, No. (%)a | 13 | (18.3) | 32 | (29.6) |
| Baseline symptoms | ||||
| PANSS positive symptom, mean (SD) | 20.3 | (4.9) | 18.7 | (5.3)** |
| PANSS negative symptom, mean (SD) | 15.8 | (7.2) | 14.1 | (6.2) |
| PANSS general symptom, mean (SD) | 33.1 | (7.9) | 31.6 | (8.6) |
| PANSS total symptom, mean (SD) | 69.3 | (14.9) | 64.6 | (15.9)** |
| GAF symptom, mean (SD) | 28.5 | (7.1) | 30.6 | (6.5)** |
| Premorbid Adjustment Scale (PAS), developmental period; childhood (up to 11 y) (mean) (SD)b | ||||
| Sociability and withdrawal | 0.9 | (1.5) | 1.0 | (1.5) |
| Peer relationships | 1.2 | (1.4) | 1.1 | (1.3) |
| Scholastic performance | 2.5 | (1.3) | 2.2 | (1.3) |
| Adaption to school | 0.9 | (1.3) | 1.1 | (1.2) |
| PAS, developmental change scores (mean) (SD)c | ||||
| Sociability and withdrawal | 1.2 | (2.0) | 1.0 | (1.9) |
| Peer relationships | 1.0 | (1.9) | 0.6 | (1.8) |
| Scholastic performance | 0.7 | (1.3) | 0.5 | (1.3) |
| Adaption to school | 1.1 | (1.7) | 0.7 | (1.6) |
*P = .013, Pearson chi-square test, df = 2; **P < .05, 2-tailed, unpaired t test. No-IC, no information campaigns; IC, information campaigns; PANSS, Positive and Negative Syndrome Scale; GAF, Global Assessment of Functioning Scale.
For the IC sample, n = 108, for the no-IC sample n = 72. Best level of functioning, 6; worst level, 0.
For the IC sample, n = 106, for the no-IC sample n = 64.
For the IC sample, n = 78, for the no-IC sample n = 51.
In order to determine if the difference in symptoms at baseline between the 2 samples was explained by variables other than IC, we did a multiple linear regression analyses with GAFs as the outcome variable (table 3). A shorter DUP, a higher level of drug abuse, and belonging to the IC sample were associated with a better clinical status at start of treatment. Coming from the IC sample was a strong predictor, even when entered as the last step.
Table 3.
Multiple Linear Regression Analysis of the Effect of Independent Variables on Clinical Status (GAF Symptoms) at Start of First Treatmenta
| Block Model Summary for Each Step |
Contribution of Separate Variables for Last Step |
||||||
| Block No., Variable | R2 Change | F Change | β | SD | T | P Value | 95% CI |
| Constant | 28.15 | (0.8) | 35.00 | <.001 | (26.56 to 29.73) | ||
| 1 | |||||||
| DUPb | 0.041 | 6.69 | .202 | (0.61) | 2.59 | .011 | (0.38 to 2.82) |
| 2 | |||||||
| Drug abuse | 0.026 | 4.42 | −.16 | (0.49) | −2.10 | 0.037 | (−2.03 to −0.06) |
| 3 | |||||||
| IC vs no-IC period | 0.055 | 9.7 | −.24 | (1.0) | −3.16 | .002 | (−5.52 to −1.23) |
Note: GAF, Global Assessment of Functioning Scale; CI, confidence interval; DUP, duration of untreated psychosis; IC, Information Campaigns; no-IC, no Information Campaigns.7
Final model, R2 = 0.11; F = 9,71; P = .002.
Transformed to its natural logarithm.
Discussion
The major finding in this study is that DUP lengthens when ICs about psychosis cease. Coming to first psychosis treatment during the no-IC period is associated with less schizophreniform disorder and more positive and total symptoms. ICs thus appear to be a critical element for the reduction of DUP such that when the campaigns are stopped we observe a reversal of such reduction.
The DUP in the TIPS II no-IC sample is comparable to the DUP in the no–early detection site of the TIPS I parallel control study,3 but the TIPS II no-IC DUP is not as lengthy as in the pre-TIPS period 1993–1994.13
In a first-episode psychosis study in Denmark (the OPUS study) carried out during 1998–1999, DUP was not measured against a non-OPUS comparison sample.14 The Median DUP in the Integrated Treatment site was 46 weeks. In OPUS, early DTs were established with a low threshold to treatment. The project offered no intensive IC aimed at the general public and no educational program aimed toward teachers and pupils. Information about the project and the DT was mainly provided to the GPs and health/social professionals working in the local communities. An Australian study15 found that adding a community development campaign to DTs in one county did not clearly reduce DUP. Compared with the TIPS IC sector the Australian project was shorter (12 months) and did not include IC to the general public but instead concentrated on schools and GPs. The common factor for these 2 studies is that their campaigns did not target multiple community groups, particularly the general public. We conclude that our study shows that an effective early detection program in first-episode psychosis requires educating the public as well as school personnel and primary health care professionals. In addition, the program included low-threshold DTs that were able to detect some patients with poor prognostic features (including those with long DUP).
A methodological weakness of our study is that it uses a quasi-experimental, historical control design that theoretically cannot control for major sources of population, measurement, and treatment variance between groups. At the same time the quasi-experimental design is the only design that can ethically test the effects of later vs earlier treatment of first-break schizophrenia. Furthermore, we believe we have minimized differences in the sources of variance between the IC and no-IC groups by selecting samples from the same health care sector with only 1 year separating them, by using the same assessment instruments and virtually the same raters, and by limiting group comparisons to baseline measures that are unaffected by treatment differences. The fact that the study used the overlapping raters also implies that they would have known whether the patient was being seen during the IC period or during the no-IC period. This may have led to potential bias in ratings. An additional weakness is that the estimate of DUP for obvious reasons had to be made retrospectively. However, we built upon all available information in making the estimate, and the reliability scores for DUP and other central measures have remained acceptable.
Selecting samples with only 1-year difference means that a substantial proportion of the no-IC sample became psychotic in the IC period. That they avoided recognition and treatment in the midst of an IC blitz demonstrates how robust denial and the impairment in insight can be. If becoming psychotic in the IC period had any effect on the no-IC sample, we think it probably was in the direction of bringing such persons to treatment somewhat earlier than if there had been no IC at all. Indeed, without this overlap, the IC/no-IC difference we found in DUP may have actually been greater.
The major strength of this study is that, at least for the foreseeable future, it is the only place where such a study can be done at all given that the TIPS project is the first (and so far the only) project to engineer changes in DUP. All other studies have simply reported DUP, not changed it in ways that the effects of such change can be measured. Another strength of the study is its location in a publicly paid catchment area treatment system that provides all possible treatment services for first-episode patients and recruits virtually all such patients from that particular geographical area. The study sample is thus clinically an incidence sample.
In conclusion, our study indicates that well-planned educational campaigns toward the general public and targeted groups, combined with low-threshold DTs, are key components of early detection efforts that successfully bring patients with first-episode psychosis into treatment earlier than otherwise.
Funding
Helse Vest trust, Stavanger, Norway (200202797-65 to I.J.). The TIPS study was supported by Norwegian National Research Council, Oslo (grant 133897/320); the Norwegian Department of Health and Social Affairs, Oslo; National Council for Mental Health/Health and Rehabilitation, Oslo (grant 1997/41); Rogaland County, Stavanger, Norway, and Oslo County, Oslo (P.V., J.J., S.F., T.L., I.M., S.O.); Theodore and Vada Stanley Foundation, Bethesda, MD; Regional Health Research Foundation for Eastern Region, Hilleroed, Denmark; Roskilde County, Roskilde, Denmark; Helsefonden Lundbeck Pharma, Hellerup, Denmark; Eli Lilly, Lyngby, Denmark; Janssen-Cilag Pharmaceuticals, Birkeroed, Denmark (E.S.); National Alliance for Research on Schizophrenia and Depression Great Neck, NY; Distinguished Investigator Award, National Institute of Mental Health, Rockville, MD (grant MH-01654 to T.M.); National Alliance for Research on Schizophrenia and Depression (Young Investigator Award to T.L.).
References
- 1.Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry. 2005;62:975–983. doi: 10.1001/archpsyc.62.9.975. [DOI] [PubMed] [Google Scholar]
- 2.Perkins DO, Gu H, Boteva K, Lieberman JA. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry. 2005;162:1785–1804. doi: 10.1176/appi.ajp.162.10.1785. [DOI] [PubMed] [Google Scholar]
- 3.Melle I, Larsen TK, Haahr U, et al. Reducing the duration of untreated first-episode psychosis: effects on clinical presentation. Arch Gen Psychiatry. 2004;61:143–150. doi: 10.1001/archpsyc.61.2.143. [DOI] [PubMed] [Google Scholar]
- 4.Johannessen JO, McGlashan TH, Larsen TK, et al. Early detection strategies for untreated first-episode psychosis. Schizophr Res. 2001;51:39–46. doi: 10.1016/s0920-9964(01)00237-7. [DOI] [PubMed] [Google Scholar]
- 5.Johannessen J, Larsen TK, Horneland M, et al. The TIPS project; a systematized program to reduce duration of untreated psychosis in first episode schizophrenia. In: Miller T, Mednick SA, McGlashan ThH, Libiger J, Johannessen JO, editors. Early Intervention in Psychotic Disorders. The Netherlands: Kluwer Academic Publishers; 2001. pp. 151–161. [Google Scholar]
- 6.Kay SR, Fiszbein A, Opler LA. The Positive and Negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 7.First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders-Patient Edition (SCID I/P, Version 2.0) New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- 8.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed, revised. Washington, DC: American Psychiatric Assosiation; 1987. [Google Scholar]
- 9.Drake RE, Osher FC, Noordsy DL, Hurlbut SC, Teague GB, Beaudett MS. Diagnosis of alcohol use disorders in schizophrenia. Schizophr Bull. 1990;16:57–67. doi: 10.1093/schbul/16.1.57. [DOI] [PubMed] [Google Scholar]
- 10.Cannon-Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull. 1982;8:470–484. doi: 10.1093/schbul/8.3.470. [DOI] [PubMed] [Google Scholar]
- 11.Larsen TK, Friis S, Haahr U, et al. Premorbid adjustment in first-episode non-affective psychosis: distinct patterns of pre-onset course. Br J Psychiatry. 2004;185:108–115. doi: 10.1192/bjp.185.2.108. [DOI] [PubMed] [Google Scholar]
- 12.Friis S, Larsen TK, Melle I, et al. Methodological pitfalls in early detection studies—the NAPE Lecture 2002. Nordic Association for Psychiatric Epidemiology. Acta Psychiatr Scand. 2003;107:3–9. doi: 10.1034/j.1600-0447.2003.02600.x. [DOI] [PubMed] [Google Scholar]
- 13.Larsen TK, McGlashan TH, Johannessen JO, et al. Shortened duration of untreated first episode of psychosis: changes in patient characteristics at treatment. Am J Psychiatry. 2001;158:1917–1919. doi: 10.1176/appi.ajp.158.11.1917. [DOI] [PubMed] [Google Scholar]
- 14.Petersen L, Jeppesen P, Thorup A, et al. A randomised multicentre trial of integrated versus standard treatment for patients with a first episode of psychotic illness. BMJ. 2005;331:602. doi: 10.1136/bmj.38565.415000.E01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krstev H, Carbone S, Harrigan SM, Curry C, Elkins K, McGorry PD. Early intervention in first-episode psychosis—the impact of a community development campaign. Soc Psychiatry Psychiatr Epidemiol. 2004o;39:711–719. doi: 10.1007/s00127-004-0798-5. [DOI] [PubMed] [Google Scholar]