Abstract
Antistigma campaigns have been promoting a medical view of schizophrenia. Given the growing body of research finding negative associations between biogenetic (BG) causal attributions and stigmatizing attitudes, this approach must be reappraised. The present study investigates the impact of different psychoeducational interventions on the etiology of schizophrenia (BG and psychosocial [PS], vs a neutral condition) and on stigmatizing attitudes in medical (n = 60) and psychology students (n = 61). Information was presented via information brochures and a video presentation. Attitudes were assessed before and after the interventions on an explicit level using the stereotype questionnaire and the Social Distance Scale as well as on an implicit level, using the Implicit Association Test. Both educational interventions produced a significant decrease in several stereotype components, which was not the case in the neutral condition. The BG intervention decreased the attribution of blame in both groups. It also decreased the stereotype unpredictability/incompetence and social distance in the medical students but increased the negative outlook on prognosis in the psychology students. The PS intervention reduced the widespread stereotype of dangerousness as well as social distance in the group of medical students. While further research into antistigma interventions is necessary, the proposal for antistigma campaigns is to take a multidimensional and balanced approach, which is adapted to target groups and provides additional facts that challenge the myths maintaining stigma.
Keywords: stigmatization, psychoeducation, biogenetic, psychosocial
Introduction
“All my neighbours know that Tom is mentally ill. What I do not tell them is that he is schizophrenic, because a lot of nasty things are said about schizophrenic people.” Margaret, mother of Tom.1(p9)
Persons with schizophrenia are frequently seen as being unpredictable, incompetent and dangerous, being responsible for their disorder, and having a poor prognosis.2–8 These attitudes have been found to be related to a preference of social distance (eg, not accepting a person with schizophrenia as a neighbor) and acceptance of structural discrimination.2 For persons with schizophrenia, this kind of stigma is often described as worse than the main condition.1,9 It pervades every part of life, in particular work and social life,1 and negatively affects the motivation to cope with the disorder and adhere with treatment.9 Unfortunately, stigma does not halt before the opinion leaders in mental health who should be expected to bring about change. With few exceptions,10 most findings reveal mental health professionals’ attitudes to be comparable to those found in the general population.11–14
In the hope to reduce stigma, campaigns have been emphasizing biogenetic (BG) explanations of schizophrenia and have been promoting the concept of “schizophrenia is an illness like others.”15–17 For example, the “changing minds” program by the Royal College of Psychiatrists18 lists “changes in the structure of their brains,” “infections before they were born,” “disorder appears to run in families,” and “chemical messengers in the brain … are not working correctly” before mentioning any psychosocial (PS) cause. The National Alliance on Mental Illness19 lists no explicit PS causes of schizophrenia but states that “the brains of people with schizophrenia are different from the brains of people without the illness,” “schizophrenia seems to be caused by a combination of problems including genetic vulnerability and environmental factors that occur during a person's development,” and recent research has “identified certain genes that appear to increase risk for schizophrenia.” Similarly, the World Psychiatric Association antistigma initiative “Open the Doors”20 states that “a predisposition is inherited” but that an “environmental trigger,” such as “complications during the mother's pregnancy or labor,” “prenatal exposure to virus,” or “complications during pregnancy and delivery,” must also be present to bring on the “disease.”
There is reason to assume that antistigma programs might be improved by promoting a diathesis-stress model of schizophrenia.21,22 The diathesis-stress model, which is widely accepted in the scientific field, acknowledges genetic and early biologic developmental risks along with environmental stressors, such as life events, daily stressors, family communication, and trauma as relevant risk factors.23–29 Its potential usefulness as a means of reducing stigma seems to be supported not only by the theoretical reflections about the possible effects that varying information is going to have on illness attributions and stigma but also by an array of empirical findings. On the one hand, it seems reasonable to assume that if the causes of mental health problems are attributed to factors outside the control of individuals (eg, biological factors), people's reactions will be less negative and patients and families will experience less blame.30–32 So far, however, this assumption has only been supported in one experimental study carried out with male students by Mehta and Farina,33 who found a disease view to be associated with less blame. On the other hand, it has been argued that BG explanations might cause the disorder to be viewed as more fundamental and immutable,33,34 exacerbate the “stickiness” of the mental illness label, and strengthen links to other undesirable characteristics.31 In support of this, a large number of studies have found biological explanations to be associated with higher levels of stigma and social distance, while this has not been shown for PS explanations.7,15,35,36 For example, in representative population surveys carried out in Germany, Russia, and Mongolia, it was found that the more respondents endorsed a brain disease as a cause, the more dangerous they believed a person with schizophrenia to be and the more desire they showed for social distance.7,37 The analysis of data from 601 adult respondents to a US telephone survey revealed genetic attributions to be associated with decreased optimism that a mental health professional could help with the problem.38,39 In their experiment, Mehta and Farina33 found that students who were provided with a disease view were prepared to apply more electric shocks toward fellow students whom they believed to have a history of mental disorder than students provided with a PS view.33 Finally, in a trend analysis of data from 2498 participants in Germany, Angermeyer and Matschinger40 found that as biological causes are being more widely acknowledged by the public, the desire for social distance toward people with schizophrenia has increased.
In sum, these results challenge the existing 1-dimensional antistigma campaigns and seem to point to the necessity of promoting multifactorial etiological models. However, in order to develop better campaigns, researchers must go beyond the cross-sectional investigations to study the impact of forwarding different information on schizophrenia. So far, only very few studies have adopted this approach. While the interpretation of 2 older studies is hampered by a quasiexperimental approach41 or the compounding of information on etiology with appraisals,42 a more recent study by Walker and Read35 investigated the impact of 5-minute medical, PS, or combined intervention on the stereotypes of dangerousness and unpredictability as well as behavioral intention. They found a trend toward overall improvement of stereotypes in the PS and combined models, while the medical model increased the attitude that patients with schizophrenia are dangerous and unpredictable. This promising approach could be optimized by using a more intensive intervention. Also, in order to gain a differentiated picture, studies should adopt a more balanced approach and include stereotype components that might be positively influenced by medical models, such as the attitude that patients are responsible for their disorder. Finally, the sole use of explicit, direct measures of stereotypes, eg, via questionnaires, that are susceptible to socially and personally desirable answers can be considered a weakness of all the listed studies. This accounts in particular for those investigating mental health professionals, for whom stereotypes of mental illness are likely to be highly taboo.43 Implicit, indirect measures, eg, via reaction time paradigms, have been found to assess a different aspect of stereotypes than explicit ones and to be superior in predicting discriminating behavior44–46 (T. A. Poehlmann, E. L. Uhlmann, A. G. Greenwald, M. R. Banaji, unpublished data, 2005).
The present study adopts an experimental approach comparing the effects of a detailed BG and PS and a neutral control intervention on various components of implicit and explicit stereotypes and on social distance. Targets were undergraduate psychology and medical students because they are expected to differ in their preexisting causal models and represent the health professionals of the future, while yet being sensitive to change by a brief educational intervention.
Method
Participants
Psychology students (n = 61) were recruited by advertisements in the faculty building and were able to fulfill study requirements by participating. Their mean age was 21.2 (SD = 3.4) years, 91.8% were female and 86.9% were of German nationality. Medical students (n = 60) were recruited by advertisements in the medical faculty building and announcements in the cafeteria. Because participation in experiments is not obligatory for medical students, they were paid for participating. The mean age of the medical students was 22.5 (SD = 3.4) years, 65.0% were female and 95.0% were of German nationality.
Measures
Preexisting subjective models on the etiology of schizophrenia were assessed by a questionnaire in which the participant was asked to respond to 9 potential causes of schizophrenia on a 5-point Likert scale ranging from 1 (certainly a cause) to 5 (certainly not a cause). The 9 causes represented in equal proportions (1) BG causes: brain disease (transmitter disorder and morphological anomalies), brain damage (eg, poisoning or injuries), inheritance; (2) PS causes: stressors and strain (eg, loss of job, partner problems, and financial worries), trauma (eg, death of close person, sexual abuse), problematic childhood (eg, unloving parents, too strict, or inconsequent upbringing); and (3) other causes: coincidence or fate, self-induced (eg, weak will, impulsiveness, or immoral behavior), God's will (eg, punishment or test). The questionnaire was developed for the purpose of this study, based on items that had been used in other investigations of causal attributions40 and were provided, on request, by the authors of these studies. In order to test the validity of the items selected for this study, 6 experts on schizophrenia were asked to allocate the items to the categories. All items were correctly allocated. Cronbach α was satisfying for the 3 items on “PS causes” (.78). However, it was low for the items on “BG causes” (.32), although it could be substantially improved by excluding the item on “genetics” (.59).
Explicit Attitudes and Social Distance
Explicit attitudes toward schizophrenia were assessed using an adaptation of a scale developed by Angermeyer and Matschinger,2 which consists of 33 statements on schizophrenia stereotypes for which agreement or disagreement is rated on a 5-point Likert scale. The authors found a 5-factor solution for a large representative sample from the German population, labeled as dangerousness (eg, “Most sex crimes are committed by people with schizophrenia”), attribution of responsibility (eg, “Anyone who gets schizophrenia is a failure”), creativity (eg, “People with schizophrenia are usually highly intelligent”), unpredictability/incompetence (eg, “People with schizophrenia are completely unpredictable”), and poor prognosis (eg, “Schizophrenia takes its tragic course, there is no point in treating it”). With exception of poor prognosis (Cronbach α = .62), all factors revealed sufficient internal consistency, with Cronbach α’s varying from .70 to .87. In the present study, the Likert scale was extended to a 9-point scale on which 3 points were described (1 = totally agree, 5 = neither-nor, and 9 = totally disagree). This adaptation was made in order to capture smaller changes in attitude change and to reduce the impact of memory effects that are likely to occur as a consequence of the retest design. We used the same factors that were identified by Angermeyer and Matschinger but added some items to the scales that had been excluded from the factors in the original version because we found them to improve the Cronbach α’s. Items belonging to each factor are depicted in Appendix 1. Cronbach α ranged from .55 (creativity), .63 (responsibility and poor prognosis), .75, and (unpredictability/incompetence) to .80 (dangerousness). Due to the low internal consistency of the “creativity” subscale and problems interpreting this factor, we omitted it from further calculations.
A behavioral intention to distance oneself from persons with schizophrenia was assessed by adapting the 7-item Social Distance Scale by Link et al.47 Specifically, respondents are asked whether they would either accept or recommend someone with schizophrenia as a lodger, coworker, neighbor, member of the same social circle, employee, in-law, or child-care provider (eg, “If you had a room to let out, would you let it out to a person with schizophrenia?”). Again, the original 5-point Likert scale was extended to a 9-point scale, with a description of points 1 (certainly), 5 (undecided), and 9 (certainly not).
Implicit Attitudes
Implicit attitudes to schizophrenia were assessed using a reaction time paradigm, the Implicit Association Test (IAT).48 The IAT is a method developed in social psychology to assess implicit (unadmitted, hidden) attitudes by measuring the strength of the associations between mental representations from different categories of objects in memory. The theory is that the faster a person reacts to combinations of words from different semantic categories, the stronger his or her semantic association of these categories is. The IAT has been broadly utilized to measure attitudes, such as prejudice, which an individual might seek to conceal due to social norms or is not able to name or willing to accept.43,49–51 It has been shown to have superior reliability and internal consistency in comparison to other implicit measures and a satisfactory retest reliability with a median of r = 0.56.46
The experiment is introduced as a computerized reaction time task. The participant responds to a series of items to be classified into 4 categories—2 representing a concept discrimination (in this case schizophrenia vs depression) and 2 representing an attribute discrimination (eg, dangerous vs safe). Subjects are asked to respond rapidly with a right-hand key press to stimuli representing one concept and one attribute (eg, schizophrenia and dangerous) and with a left-hand key press to stimuli from the remaining 2 categories (eg, depression and safe). Subjects then perform a second task in which the key assignments for one of the pairs are switched (such that schizophrenia and safe share a response, likewise depression and dangerous). The logic of the IAT is that sorting should be easier, and thus faster, when the 2 concepts that share a response are implicitly associated.
Depression was chosen as contrast category to schizophrenia because it has been found to be associated with less stigma.3,11,30 Five stimuli related to each category were derived from the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, criteria for these disorders. Three different attribution discriminations were extracted from the assessment of explicit stereotypes2: culprit vs victim, cureless vs healable, and dangerous vs safe. The 5 stimuli related to each attribute discrimination were derived from the terms used in the explicit stereotype questionnaire and by discussion and consensus among the authors. The IAT was tested in a pilot trial with 12 participants, and some of the original stimuli were replaced because they produced outliers in reaction times. A translation of the German stimuli for the concept and attribution discriminations is presented in Appendix 2.
The use of 3 attribute discriminations resulted in 3 different IATs. The variation of the order of the potentially congruent vs incongruent category-attribute combinations as well as the 3 IATs resulted in a total of 12 different IAT versions, which were evenly assigned to the 3 experimental groups.
Prior to the actual IAT experiment and each block, test instructions were displayed on the screen and the assignment of categories and stimuli were practiced (eg, schizophrenia-paranoia, hallucinations, etc—vs depression-suicide, loss of interest, etc). Stimuli were presented in random order, the response-stimulus interval was 150 ms. An error message appeared on the screen after a wrong classification, and the stimuli remained on the screen until the participant had responded correctly. The IAT effects were calculated using the D-measure, the difference between the compatible and the incompatible condition, corrected by the SD of the reaction times.52 Thus, the larger the effect, the stronger the stereotyping of schizophrenia compared with depression.
Design
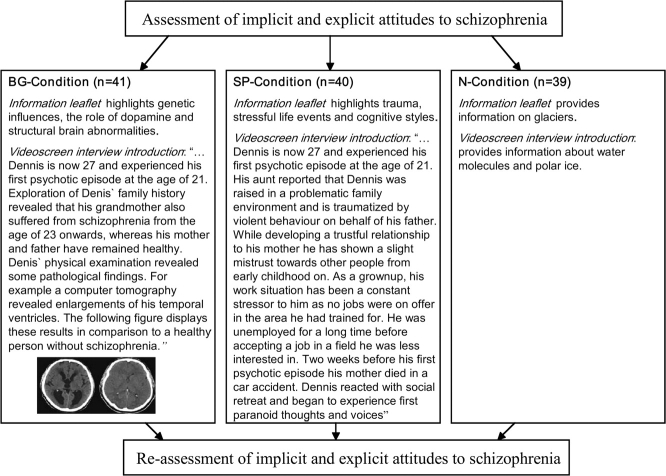
The design of the study was an experimental pre-post design using 3 experimental groups, for which either a BG, PS, or no intervention (N) was presented (see figure 1). Participants were allocated to one of 3 experimental groups and 12 different IAT versions by systematic variation.
Fig. 1.
Design.
Procedure
Participants were told that the experiment was being carried out to test the influence of information processing in knowledge transfer of psychological disorders. All participants completed the assessments of implicit and explicit attitudes, social distance, and preexisting models of explanation for schizophrenia at study entry. Then, they were allocated to one of the 3 interventions. The interventions began by handing out an information leaflet on the etiology of schizophrenia or—in the neutral condition—on water (compare figure 1). After the lecture of the leaflet, participants were questioned about its content and were later excluded from the analyses if they could not recall at least 2 of the 3 highlighted causal explanations. In a second step, the information provided in the leaflet was underlined by a video of a patient (played by an actor) being interviewed for a diagnostic assessment. The interview is introduced by a video screen text, stating that the interview section “shows one of our patients, Dennis, being interviewed by a clinical psychologist from our department” which is followed by an account of relevant factors for the development of schizophrenia in the case of Dennis. These were of BG nature (BG intervention) and PS nature (PS intervention). In the interview, the patient reports on a row of positive and negative symptoms of schizophrenia, such as delusions of reference, poor concentration, and thought disorder. The interview is the same in both interventions. Again, the subsequent recall of at least 2 of the highlighted etiological factors was required for inclusion. Following the film, implicit and explicit attitudes were reassessed. Finally, participants were asked to indicate on a 5-point Likert scale (1) how convincing they found the model of explanation, (2) how much the film had helped them toward a better understanding of schizophrenia, and (3) how much they liked the patient. After completion of the experiment, participants were fully disclosed and provided with the additional scientific information on the etiology of schizophrenia.
Results
Preexisting Explicit and Implicit Stereotypes and Social Distance
There were no significant differences in the mean stereotype scores between the medical students (3.78, SD = 0.80) and the psychology students (3.77, SD = 0.64; T = −0.115, df = 119, P = .909). The groups did also not differ in the specific stereotype factors. However, psychology students revealed more desire for social distance (mean = 4.42) than medical students (mean = 3.88; T = −2.147, P = .034).
Social distance was significantly correlated with the total stereotype score (r = 0.60), dangerousness (r = 0.58), responsibility (r = 0.41), unpredictability/incompetence (r = 0.43), and poor prognosis (r = 0.20) in the complete sample, controlling for group.
Overall, endorsement rates were high, although slightly lower than those found by Angermeyer and Matschinger2 for the general population, in particular with regard to dangerousness and social distance (Arens, Berger, and Lincoln, unpublished data).
Psychology and medical students did also not differ in their level of implicit stereotypes as assessed with the IAT. Both groups showed significantly higher levels of negative stereotypes for schizophrenia as compared with depression. In the group of psychology students, the D-score differed significantly from zero for dangerousness (0.17, SD = 0.31, df = 56, P = .00) and responsibility (0.15, SD = 0.29, df = 56, P = .00) but not with regard to poor prognosis (0.07, SD = 0.35, df = 57, P = .15). The same pattern was found for the group of medical students, with significant effects for dangerousness (0.11, SD = 0.33, df = 57, P = .02) and responsibility (0.14, SD = 0.27, df = 57, P = .00) but not for poor prognosis (0.02, SD = 0.30, df = 57, P = .68).
There were no significant positive correlations between the IATs and the explicit measure of stereotypes; the IAT for dangerousness was even negatively associated with the explicit stereotype responsibility (r = −0.21, P = .023).
Association of Preexisting Causal Explanations and Stereotypes
First, we tested whether psychology and medical students differed in the relevance they ascribed to each causal explanation but found no significant differences. Second, we tested each of the causal explanations for significant correlations with each of the stereotypes and with social distance. In addition, we calculated a score to assess the “favor of biological explanations over psychosocial ones” by calculating the difference between the total psychological score and the total biological score (higher values indicate favor of biological explanations). This score was also tested for significant associations with stereotypes. The correlations are depicted in table 1. The psychology and medical students differed in some of the correlations between causal explanations and explicit stereotypes. In these cases, correlations are presented for each group separately. Nonscientific causal explanations, such as schizophrenia being due to fate, being self-induced, or God's will, were generally most strongly associated with stereotypes, in particular with responsibility, dangerousness, and unpredictability/incompetence. Medical students who believed that schizophrenia has a genetic cause were less likely to judge persons with schizophrenia as dangerous, responsible, and unpredictable or incompetent. Psychology students who endorsed PS factors, such as trauma and upbringing, were more likely to have a positive attitude toward prognosis. Medical students who favored BG explanations over PS ones showed less attribution of responsibility, whereas psychology students who favored BG explanations over PS ones had a more negative view on prognosis.
Table 1.
Correlations Between Causal Explanations and Explicit Stereotypes and Social Distance
| Score in Stereotype Components and Social Distance |
|||||||||||||||
| Dangerousness | Responsibility | Unpredictability/Incompetence | Poor Prognosis | Social Distance | |||||||||||
| Relevance ascribed to causal explanations | Total | Med | Psy | Total | Med | Psy | Total | Med | Psy | Total | Med | Psy | Total | Med | Psy |
| Brain disease | .00 | −.15 | .07 | −.01 | .01 | ||||||||||
| Brain damage | .02 | .00 | .09 | .03 | .07 | ||||||||||
| Inheritance | −.28** | −.37** | NS | −.32** | −.46** | NS | −.16 | −.28* | NS | .02 | −.02 | ||||
| Favor of biogenetic factors | −.12 | −.23** | −.32* | NS | −.07 | .12 | NS | .36** | −.01 | ||||||
| Stresses and strains | −.01 | −10 | .04 | −.09 | .09 | ||||||||||
| Trauma | .05 | .07 | .10 | −.11 | NS | −.40** | .09 | ||||||||
| Childhood/upbringing | .05 | .08 | .05 | −.17 | NS | −.33** | −.11 | ||||||||
| Coincidence/fate | .17 | .22* | .35** | NS | .16 | .05 | .18 | ||||||||
| Self-induced | .31** | NS | .41** | .50** | .39** | .60** | .23** | NS | .39** | .04 | .10 | ||||
| God's will | .34** | .39** | .30* | .48** | .57** | .41** | .26** | .38** | NS | .05 | .30** | .42** | NS | ||
Note: Pearson correlations, 2 tailed; total, total sample; med, medical students; psy, psychology students. *P ≤ .05; **P ≤ .01.
Implicit stereotypes were not associated with preexisting causal explanations in either of the groups.
Impact of the Interventions on Changes in Stereotypes
Three participants in the BG condition and 2 participants from the PS condition were excluded because they could not recall at least 2 relevant causal facts from either the text or the film or both. Both interventions were rated as equally convincing (BG: 4.0, SD = 0.75; PS: 4.0, SD = 0.89) and useful for conveying information about schizophrenia (BG: 4.0, SD = 0.92; PS: 4.0, SD = 1.24). However, the patient was rated as more likable (4.3, SD = 0.74) in the BG than in the PS condition (3.8, SD = 0.77; T = 2.77, df = 73, P = .007).
To test the impact of the interventions on explicit stereotypes, we conducted a multivariate linear model of variance with the difference scores in the explicit stereotype factors and social distance (with negative difference scores implying a reduction of stereotypes or social distance) as dependent variables and interventions (BG vs PS vs N) and group (psychology vs medical students) as fixed factors and tested for main effects (condition, group) and interaction effects.
A separate multivariate linear model of variance was conducted with the difference scores in the 3 IATs because it has been advised to use moderately intercorrelated dependent variables in multivariate analyses of variance53 and this was not the case for the implicit and explicit stereotypes.
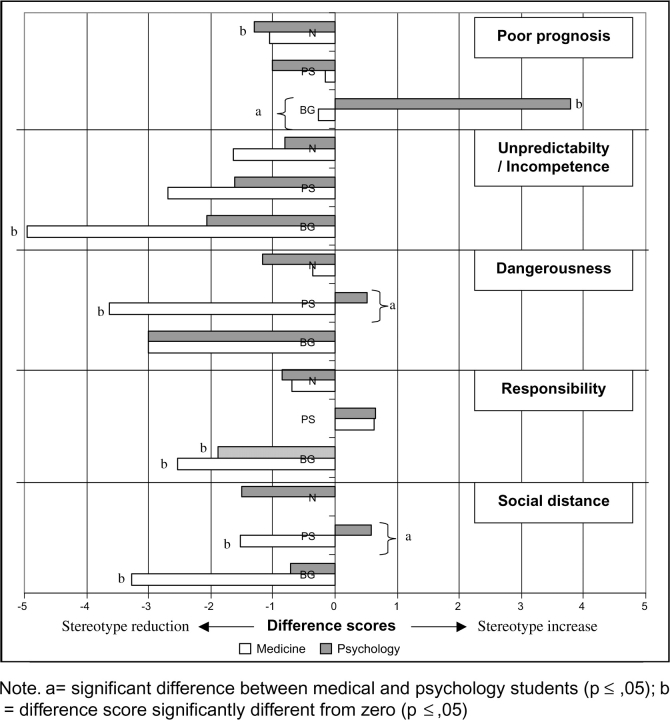
The results of both analyses are depicted in table 2. For the changes in explicit stereotypes and social distance, there was a significant effect for time, indicating an overall reduction in stereotype scores across the 2 measurements. There was also a significant effect for intervention. Least significant difference post hoc univariate tests revealed a significant reduction of the stereotype responsibility in the BG intervention compared with PS (P = .000) or N (P = .035) and a significant increase in the stereotype poor prognosis for the BG intervention in comparison to PS (P = .019) and N (P = .003). There was no significant group effect but a trend to a significant interaction effect between intervention and group. Figure 2 shows the difference scores in each combination of explicit stereotype component, group, and intervention. Post hoc t tests were conducted to test for significant difference scores and group differences. Significant reductions of stereotypes by the BG intervention occurred with regard to unpredictability/incompetence, responsibility, and social distance, but the BG intervention produced an increase of the stereotype poor prognosis. The PS condition led to a decrease in the stereotype dangerousness as well as social distance. Figure 2 also points to some relevant group differences. For example, the BG condition produced a significantly larger increase with regard to poor prognosis in the psychology students than in the medical students, whereas the PS intervention reduced the stigma of dangerousness significantly more in the medical students. However, these interactions should be interpreted with caution because the interaction for group × intervention in the model was not significant.
Table 2.
Change in Stereotype Components by Varying Causal Explanation Models: Results of the Multiple Linear Models
| F (Pillai-Spur) | df (Hypothesis/Error) | P | Wilks λ | Partial η2 | |
| Explicit stereotypes and social distance | |||||
| Time (fixed factor) | 6.65 | 5/102 | .000 | 0.754 | 0.246 |
| Intervention | 3.37 | 10/206 | .000 | 0.728 | 0.141 |
| Group | 1.03 | 5/102 | .403 | 0.972 | 0.048 |
| Intervention × group | 1.73 | 10/206 | .077 | 0.851 | 0.077 |
| Implicit stereotypes | |||||
| Time (fixed factor) | 1.26 | 3/102 | .291 | 0.964 | 0.036 |
| Intervention | 1.33 | 6/206 | .247 | 0.927 | 0.037 |
| Group | 0.53 | 3/102 | .661 | 0.985 | 0.015 |
| Intervention × group | 0.35 | 6/206 | .908 | 0.980 | 0.010 |
Note: Partial η2 is an estimate of the effect size.53
Fig. 2.
Difference Scores Between Explicit Stereotypes and Social Distance Before and After the Intervention. Note: a = significant difference between medical and psychology students (P ≤ .05); b = difference score significantly different from zero (P ≤ .05).
There were no changes in implicit stereotypes across the 2 measurements (compare table 2).
Discussion
Preexisting Causal Beliefs and Stereotypes
Psychology and medical students were found to express significant levels of explicit stereotypes. Moreover, the implicit assessment of stereotypes via the IAT revealed a stronger implicit stereotyping of persons with schizophrenia than of persons with depression with regard to dangerousness and responsibility. Contrary to our expectation, medical and psychology students did not differ in their preexisting causal explanations for schizophrenia. However, medical students who believed genetics to be involved were less likely to see persons with schizophrenia as being responsible for their disorder or as being dangerous and unpredictable. In contrast, psychology students who favored BG factors over PS ones were more likely to have a negative view on the prognosis of schizophrenia. Encouragingly, neither BG nor PS causal beliefs were strongly associated with stigmatizing attitudes. This was much more the case for “unscientific” causal beliefs, such as seeing schizophrenia as being self-induced or God's will, which supports the approach of forwarding scientific facts to combat stigma.
The positive association of preexisting PS models on estimates of prognosis in the psychology students could be explicable by their better knowledge and understanding of PS problems (either as a consequence of or even as a personal prerequisite for studying psychology) and thus greater belief in their changeability. On the other hand, genetics and in particular brain damage or disorder might seem more alien and less changeable to psychology students. In contrast, BG explanations might be more readily understood by medical students and judged less fundamental and immutable. This might also explain part of the motivation among the medically dominated psychiatric associations to combat stigma by promoting BG explanations. Obviously, this strategy might be less successful in the more psychosocially dominated general population.8,15,54–56
Impact of Varying Interventions
Here too, our results do not provide a simple answer. Again, it is reassuring to find that both educational interventions produced a significant decrease of several stereotype components, which was not the case in the neutral condition. This finding is in line with other studies finding educational interventions to be a promising approach in reducing psychiatric stigma.17,57 However, it seems that different approaches produce different results in different groups and, in particular, for different components of stereotypes. The PS intervention had significant impact on the most widespread and problematic stereotype of dangerousness, and it reduced social distance in the group of medical students. It also had the advantage of not increasing any stereotype components. The BG model decreased the stereotype unpredictability/incompetence and social distance in the medical students, while increasing the stereotype poor prognosis in the psychology students. In line with assumptions on positive effects of a medical view30,31 and the finding by Mehta and Farina,33 the BG model decreased the attribution of responsibility for the disorder in both groups. These results underline the assumption that it would be better to combine the various elements of the diathesis-stress model in an antistigma intervention rather than providing a 1-dimensional view.
One concern is that there seem to be some disparate elements between not holding people responsible for their disorder and having an optimistic outlook on prognosis and treatment possibilities, the latter implying that patients have a certain amount of control over the course of the disorder. Because the stereotype of responsibility is a less frequent one,2,3 antistigma interventions should focus on combating the more widespread negative views on prognosis. This is likely to have more impact on structural discrimination. The hope that people will adapt a more optimistic view on schizophrenia if they are better informed about treatment possibilities is supported by the results of a cross-sectional population survey by Angermeyer and Matschinger55 comparing prognosis estimates of treated vs untreated psychosis.
Our interventions generally produced more significant attitude change than the ones employed by Walker and Read.35 This might be due to the longer and more detailed intervention and the premise of correct recall. One concern with the Walker and Read35 study is the use of the word “schizophrenia” in the title of their BG intervention but not in the PS intervention. This might have biased the results toward the PS model because the label schizophrenia as such seems to produce a negative evaluation.15
Strengths and Limitations
The use of 2 different mental health professional groups and diverse components of stereotypes as well as the strict experimental design, separating information from appraisal and employing a neutral condition, can be considered as major strengths of the present study. The application of an additional, implicit measure to assess negative attitudes toward schizophrenia presents an advantage of the present methodology over previous investigations. However, in spite of finding significant IAT effects in this study, the interventions did not produce changes in implicit stereotypes. Possibly, the short intervention did not have enough impact to produce changes at this less conscious level of processing in such a short time. Possible too, that the category dimensions used in the IATs in the effort to make them more directly comparable to the explicit measures were too complex to reveal small changes in attitudes at a more basic level. Also, as relative measures, the IATs in our study could only capture stereotypes to schizophrenia beyond and above stereotypes of depression.3,30 They thus assessed only part of the complete stereotyped thinking, possibly rendering them less sensitive to change.
The absence of associations between the implicit and explicit attitudes might raise doubt with regard to the validity of the IATs.58 On the other hand, we took into account all relevant recommendations for programming and applying the IAT.46,52 Correlations between implicit and explicit attitudes were also absent in the study by Teachman et al51 investigating stereotypes of mental illness. The generally low associations have been argued to be explicable by the lack of introspection into hidden attitudes, nonadmittance of unwanted attitudes, or social desire.59
Although there was no significant main group effect, medical students tended to be influenced more by the models. This might be explained by the fact that they were more attentive because they were being paid for participation, whereas psychology students were merely fulfilling ordinary and bothersome curriculum requirements. On the other hand, participants who could not reproduce the conveyed information were excluded, and this was not the case for more psychology than medical students.
The use of a new measure for the assessment of beliefs about etiology is a limitation. More work is needed to improve the reliability of this measure and test its validity.
Finally, it should be noted that the educational interventions focused solely on etiological models and did not provide additional information likely to reduce stigma (eg, facts about treatment effectiveness) and are, as such, not intended to be sufficient models for antistigma campaigns. However, in order to improve campaigns, it is important to be able to estimate the impact each information is going to have on its own before studying “packages” of information.
Implications for Future Research and Antistigmatization Programs
While there is clearly more to fighting stigma than improving antistigma campaigns (eg, by providing state of the art treatment to every patient), educating people about schizophrenia via scientific knowledge can be considered a helpful approach. In spite of this, 1-sided or biased explanations seem to have limited benefits. As a consequence, we argue that rather than excluding relevant scientific facts from educational interventions,31 it seems more sensible to take a multidimensional and balanced approach.34 These interventions could use the positive effect that BG explanations produce with regard to some stereotypes, in particular responsibility, while actively seeking to counterbalance the negative effects, in particular the view about prognosis, by providing specific information on outcome and treatment effectiveness. Furthermore, our data seem to imply that information that makes schizophrenia more understandable is most helpful in reducing stigma. In addition, campaigns might need to place more emphasis on the frequent stereotypes and provide information that actively negates false assumptions about schizophrenia. The findings also suggest that it might be advantageous to adapt antistigma campaigns to target groups, aligning them with preexisting knowledge and targeting the specific components of stereotypes that are predominant in a particular group. Nevertheless, the attitude change toward persons with schizophrenia must occur first in the opinion leaders in science and mental health professions in order to spread to other target groups, such as patients, relatives, and the general population. Furthermore, it might prove helpful to make use of factors known to reduce stereotypes, such as positive models or contact,4,6 and to provide patient examples suited to the target groups, eg, a mental health professional with schizophrenia.
In order to evaluate these suggestions, a whole array of empirical studies is needed, replicating current findings and investigating and comparing the impact of different interventions for varying target groups and on varying components of stereotypes (see also recommendations by Angermeyer and Dietrich,4 Phelan,31 and Corrigan and Watson34). This might seem toilsome in comparison to the good-willed but unproven approaches taken so far. On the other hand, for those recovering from schizophrenia, there is nothing more devastating and disabling than stigma and discrimination.1,9,60 Scientific knowledge could be used more rigorously in order to improve this situation.
Appendix 1: Factors Derived From the Explicit Stereotype Questionnaire
Dangerousness. Only a few dangerous criminals have schizophrenia (s.); the number of violent crimes committed by people with s. has been increasing; people with s. are a great threat to small children; people with s. commit particularly brutal crimes; most sex crimes are committed by people with s.; the only thing you can do with patients with s. is put them in a hospital for a long time; by admitting all patients with s. to closed wards, one could significantly reduce the number of violent crimes; patients with s. do not commit violent crimes more often than the rest of the population.
Attribution of responsibility. Anyone who gets s. is a failure; s. is a penalty for bad deeds; whether you get s. is a question of willpower and self-discipline; successful people rarely get s.; you can get s. if you lead an immoral life.
Unpredictability and incompetence. People with s. cannot think logically; people with s. definitely need a guardian; people with s. are completely unpredictable; you never know what a patient with s. is going to do next; people with s. are quick to lose their self-control; people with s. are not capable about making important decisions about their lives; s. leads to complete stupidity; people with s. are completely unpredictable.
Poor prognosis. Nowadays, treatment for s. is just as good as it is for diabetes; with modern treatment methods these days, many people with s. can be cured; there is still no effective treatment for s.; s. takes its tragic course, there is no point in treating it; rehabilitation schemes designed to get patients back to work are usually doomed to failure.
Appendix 2: Concepts, Attributes, and Stimuli Used in the Implicit Association Tests
Concepts. Schizophrenia (paranoia, hallucinations, thought insertion, disorganization, and bizarre behavior) vs depression (suicide, loss of interest, slowed down, loss of pleasure, and agitation).
Attributes. Threatening (criminal, dangerous, brutal, uncontrollable, and inscrutable) vs safe (trustworthy, harmless, peaceful, controlled, and predictable); Culprit (active, guilty, punishment, responsible, and involved) vs victim (passive, innocent, pity, helpless, at so's mercy); Healable (recovery, treatable, optimistic, outlook, and hopeful) vs unhealable (chronic, untreatable, pessimistic, resignation, and hopeless).
References
- 1.Thornicroft G. Shunned. Discrimination Against People with Mental Illness. Oxford, UK: Oxford University Press; 2006. [Google Scholar]
- 2.Angermeyer MC, Matschinger H. The stereotype of schizophrenia and its impact on discrimination against people with schizophrenia: results from a representative survey in Germany. Schizophr Bull. 2004;30:1049–1061. doi: 10.1093/oxfordjournals.schbul.a007120. [DOI] [PubMed] [Google Scholar]
- 3.Crisp AH, Gelder MG, Rix S, Meltzer HI, Rowlands OJ. Stigmatisation of people with mental illnesses. Br J Psychiatry. 2000;177:4–7. doi: 10.1192/bjp.177.1.4. [DOI] [PubMed] [Google Scholar]
- 4.Angermeyer MC, Dietrich S. Public beliefs about and attitudes towards people with mental illness: a review of population studies. Acta Psychiatr Scand. 2006;113:163–179. doi: 10.1111/j.1600-0447.2005.00699.x. [DOI] [PubMed] [Google Scholar]
- 5.Pescosolido BA, Monahan J, Link BG, Stueve A, Kikuzawa S. The public's view of the competence, dangerousness, and need for legal coercion of persons with mental health problems. Am J Public Health. 1999;89:1339–1345. doi: 10.2105/ajph.89.9.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Corrigan PW, Green A, Lundin R, Kubiak AA, Penn DL. Familiarity with and social distance from people who have serious mental illness. Psychiatr Serv. 2001;52:953–958. doi: 10.1176/appi.ps.52.7.953. [DOI] [PubMed] [Google Scholar]
- 7.Dietrich S, Beck M, Bujantugs B, Kenzine D, Matschinger H, Angermeyer MC. The relationship between public causal beliefs and social distance toward mentally ill people. Aust N Z J Psychiatry. 2004;38:348–354. doi: 10.1080/j.1440-1614.2004.01363.x. [DOI] [PubMed] [Google Scholar]
- 8.Link BG, Phelan JC, Bresnahan M, Stueve A, Pescosolido BA. Public conceptions of mental illness: labels, Causes, Dangerousness. and Social Distance. Am J Public Health. 1999;89:1328–1333. doi: 10.2105/ajph.89.9.1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meise U, Sulzenbacher H, Hinterhuber H. Das Stigma der Schizophrenie: versuche zu dessen Überwindung [The stigma of schizophrenia: attempts to overcoming it] Fortschr Neurol Psychiatr. 2001;69:75–80. doi: 10.1055/s-2001-16534. [DOI] [PubMed] [Google Scholar]
- 10.Kingdon D, Sharma T, Hart D. What attitudes do psychiatrists hold towards people with mental illness? Psychiatr Bull. 2004;28:401–406. [Google Scholar]
- 11.Nordt C, Rössler W, Lauber C. Attitudes of mental health professionals toward people with schizophrenia and major depression. Schizophr Bull. 2006;32:709–714. doi: 10.1093/schbul/sbj065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lauber C, Anthony M, Ajdacic-Gross V, Rössler W. What about psychiatrists’ attitude to mentally ill people? Eur Psychiatry. 2004;19:423–427. doi: 10.1016/j.eurpsy.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 13.Mukherjee R, Fialho A, Wijetunge K, Checinski K, Surgenor T. The stigamtisation of psychiatric illness: the attitudes of medical students and doctors in a London teaching hospital. Psychiatr Bull. 2002;26:171–181. [Google Scholar]
- 14.Rössler W, Salize HJ, Trunk V, Voges B. Die Einstellungen von Medizinstudenten gegenüber psychisch Kranken [Attitudes of medical students towards the mentally ill] Nervenarzt. 1996;67:757–764. doi: 10.1007/s001150050050. [DOI] [PubMed] [Google Scholar]
- 15.Read J, Haslam N, Sayce L, Davies E. Prejudice and schizophrenia: a review of the ‘mental illness is an illness like any other’ approach. Acta Psychiatr Scand. 2006;114:303–318. doi: 10.1111/j.1600-0447.2006.00824.x. [DOI] [PubMed] [Google Scholar]
- 16.Thompson AH, Stuart H, Bland RC, Arboleda-Florez J, Warner R, Dickson RA. Attitudes about schizophrenia from the pilot site of the WPA worldwide campaign against the stigma of schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2002;37:475–482. doi: 10.1007/s00127-002-0583-2. [DOI] [PubMed] [Google Scholar]
- 17.Watson AC, Otey E, Westbrook AL, et al. Changing middle schoolers’ attitudes about mental illness through education. Schizophr Bull. 2004;30:563–572. doi: 10.1093/oxfordjournals.schbul.a007100. [DOI] [PubMed] [Google Scholar]
- 18.Royal College of Psychiatrists. Changing minds. Schizophrenia. Available at: http://www.rcpsych.ac.uk/campaigns/changingminds/mentaldisorders/schizophrenia.aspx. 2005. Accessed August 2007. [Google Scholar]
- 19.National Alliance on Mental Illness. About mental illness. Schizophrenia. 2007 Available at: http://www.nami.org/Template.cfm?Section=By_Illness. 2007. Accessed November 22, 2007. [Google Scholar]
- 20.World Psychiatric Association. Open the doors. Available at: http://www.openthedoors.com/english/03_07.html, 2007. Accessed August 2007. [Google Scholar]
- 21.Zubin J, Spring B. Vulnerability—a new view of schizophrenia. J Abnorm Psychol. 1977;86:103–126. doi: 10.1037//0021-843x.86.2.103. [DOI] [PubMed] [Google Scholar]
- 22.Nuechterlein KH, Dawson ME. A heuristic vulnerability/stress model of schizophrenic episodes. Schizophr Bull. 1984;10:300–312. doi: 10.1093/schbul/10.2.300. [DOI] [PubMed] [Google Scholar]
- 23.Myin-Germeys I, Krabbendam L, Delespaul PAEG, Van Os J. Do life events have their effect on psychosis by influencing the emotional reactivity to daily life stress? Psychol Med. 2003;33:327–333. doi: 10.1017/s0033291702006785. [DOI] [PubMed] [Google Scholar]
- 24.Butzlaff RL, Hooley JM. Expressed emotion and psychiatric relapse. A meta-analysis. Arch Gen Psychiatry. 1998;55:547–552. doi: 10.1001/archpsyc.55.6.547. [DOI] [PubMed] [Google Scholar]
- 25.Cantor-Graae ES, J-P Schizophrenia and Migration: a meta-analysis and review. Am J Psychiatry. 2005;162:12–24. doi: 10.1176/appi.ajp.162.1.12. [DOI] [PubMed] [Google Scholar]
- 26.Norman RMG, Malla AK. Stressful life events and schizophrenia I: a review of the research. Br J Psychiatry. 1993;162:161–166. doi: 10.1192/bjp.162.2.161. [DOI] [PubMed] [Google Scholar]
- 27.Morgan C, Fisher H. Environmental factors in schizophrenia: childhood trauma—a critical review. Schizophr Bull. 2007;33:3–10. doi: 10.1093/schbul/sbl053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lataster T, Van Os J, Drukker M, et al. Childhood victimization and developmental expression of non-clinical delusional ideation and hallucinatory experiences. Soc Psychiatry Psychiatr Epidemiol. 2006;41:423–428. doi: 10.1007/s00127-006-0060-4. [DOI] [PubMed] [Google Scholar]
- 29.Cougnard A, Marcels M, Myin-Germeys I, et al. Does normal developmental expression of psychosis combine with environmental risk to cause persistence of psychosis? A psychosis proneness-persistence model. Psychol Med. 2007;37:513–527. doi: 10.1017/S0033291706009731. [DOI] [PubMed] [Google Scholar]
- 30.Corrigan PW, River LP, Lundin RK, et al. Stigmatizing attributions about mental illness. J Community Psychol. 2000;28:91–102. [Google Scholar]
- 31.Phelan JC. Genetic bases of mental illness—a cure for stigma? Trends Neurosci. 2002;25:430–431. doi: 10.1016/s0166-2236(02)02209-9. [DOI] [PubMed] [Google Scholar]
- 32.Weiner B, Perry RP, Magnusson J. An attributional analysis of reactions to stigmas. J Pers Soc Psychol. 1988;55:738–748. doi: 10.1037//0022-3514.55.5.738. [DOI] [PubMed] [Google Scholar]
- 33.Mehta S, Farina A. Is being “sick” really better? Effect of the disease view of mental disorders on stigma. J Soc Clin Psychol. 1997;16:405–419. [Google Scholar]
- 34.Corrigan PW, Watson AC. At issue: stop the stigma: call mental illness a brain disease. Schizophr Bull. 2004;30:477–479. doi: 10.1093/oxfordjournals.schbul.a007095. [DOI] [PubMed] [Google Scholar]
- 35.Walker I, Read J. The differential effectiveness of psychosocial and biogenetic causal explanations in reducing negative attitudes towards “mental illness”. Psychiatry. 2002;65:313–325. doi: 10.1521/psyc.65.4.313.20238. [DOI] [PubMed] [Google Scholar]
- 36.Read J, Harré N. The role of biological and genetic causal beliefs in the stigmatization of ‘mental patients’. J Ment Health. 2001;10:223–235. [Google Scholar]
- 37.Dietrich S, Matschinger H, Angermeyer MC. The relationship between biogenetic causal explanations and social distance toward people with mental disorders: results from a population survey in Germany. Int J Soc Psychiatry. 2006;52:166–174. doi: 10.1177/0020764006061246. [DOI] [PubMed] [Google Scholar]
- 38.Phelan JC, Yang LH, Cruz-Rojas R. Effects of attributing serious mental illnesses to genetic causes on orientations to treatment. Psychiatr Serv. 2006;57:382–387. doi: 10.1176/appi.ps.57.3.382. [DOI] [PubMed] [Google Scholar]
- 39.Kuppin S, Carpiano RM. Public conceptions of serious mental illness and substance abuse, their causes and treatments: findings from the 1996 General Social Survey. Am J Public Health. 2006;96:1766–1771. doi: 10.2105/AJPH.2004.060855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Angermeyer MC, Matschinger H. Causal beliefs and attitudes to people with schizophrenia. Trend analysis based on data from two population surveys in Germany. Br J Psychiatry. 2005;186:331–334. doi: 10.1192/bjp.186.4.331. [DOI] [PubMed] [Google Scholar]
- 41.Fisher JD, Farina A. Consequences of beliefs about the nature of mental disorders. J Abnorm Psychol. 1979;88:320–327. doi: 10.1037//0021-843x.88.3.320. [DOI] [PubMed] [Google Scholar]
- 42.Farina A, JDF, Getter H, Fischer EH. Some consequences of changing people's views regarding the nature of mental illness. J Abnorm Psychol. 1978;87:272–279. doi: 10.1037//0021-843x.87.2.272. [DOI] [PubMed] [Google Scholar]
- 43.Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: is anyone immune? Int J Obes. 2001;25:1525–1531. doi: 10.1038/sj.ijo.0801745. [DOI] [PubMed] [Google Scholar]
- 44.Sekaquaptewa D, Espinoza P, Thompson M, Vargas P, von Hippel W. Stereotypic explanatory bias: implicit stereotyping as a predictor of discrimination. J Exp Soc Psychol. 2003;39:75–82. [Google Scholar]
- 45.Dovidio JF, Kawakami K, Johnson C, Johnson B, Howard A. On the nature of prejudice: automatic and controlled processes. J Exp Soc Psychol. 1997;33:510–540. [Google Scholar]
- 46.Nosek BA, Greenwald AG, Banaji MR. The Implicit Association Test at age 7: a methological and conceptual review. In: Bargh JA, editor. Social Psychology and the Unconscious: The Automaticy of Higher Mental Processes. New York, NY: Psychology Press; 2007. [Google Scholar]
- 47.Link BG, Cullen FT, Frank J, Wozniak JF. The social rejection of former mental patients: understanding why labels matter. Am J Sociol. 1987;92:1461–1500. [Google Scholar]
- 48.Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: The Implicit Association Test. J Pers Soc Psychol. 1998;74:1464–1480. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- 49.Greenwald AG, Banaji MR. Implicit social cognition: attitudes, self-esteem, and stereotypes. Psychol Rev. 1995;102:4–27. doi: 10.1037/0033-295x.102.1.4. [DOI] [PubMed] [Google Scholar]
- 50.White MJ, White GB. Implicit and explicit occupational gender stereotypes. Sex Roles. 2006;55:259–266. [Google Scholar]
- 51.Teachman BA, Wilson JG, Komarovskaya AI. Implicit and explicit stigma of mental illness in diagnosed and healthy samples. J Soc Clin Psychol. 2006;25:75–95. [Google Scholar]
- 52.Greenwald AG, Nosek BA, Banaji MR. Understanding and using the Implicit Association Test: 1. An improved scoring algorithm. J Pers Soc Psychol. 2003;85:197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- 53.Tabachnick BG, Fidell LS. Using Multivariate Statistics (5) Boston, Mass: Pearson and Allyn & Bacon; 2007. [Google Scholar]
- 54.Jorm AF, Korten AE, Jacomb PA, Christensen H, Rodgers B, Pollitt P. Public beliefs about causes and risk factors for depression and schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 1997;32:143–148. doi: 10.1007/BF00794613. [DOI] [PubMed] [Google Scholar]
- 55.Angermeyer MC, Matschinger H. Lay beliefs about schizophrenic disorder: the results of a population survey in Germany. Acta Psychiatr Scand. 1994;89:39–45. doi: 10.1111/j.1600-0447.1994.tb05864.x. [DOI] [PubMed] [Google Scholar]
- 56.Furnham A, Bower P. A comparison of academic and lay theories of schizophrenia. Br J Psychiatry. 1992;161:201–210. doi: 10.1192/bjp.161.2.201. [DOI] [PubMed] [Google Scholar]
- 57.Pinfold V, Toulmin H, Thornicroft G, Huxley P, Farmer P, Graham T. Reducing psychiatric stigma and discrimination: evaluation of educational interventions in UK secondary schools. Br J Psychiatry. 2003;182:342–346. doi: 10.1192/bjp.182.4.342. [DOI] [PubMed] [Google Scholar]
- 58.Blanton H, Jaccard J. Arbitrary metrics in psychology. Am Psychol. 2006;61:27–41. doi: 10.1037/0003-066X.61.1.27. [DOI] [PubMed] [Google Scholar]
- 59.Hofmann W, Gawronski B, Geschwendner T, Le H, Schmitt M. A meta-analysis of the correlation between the Implicit Association Test and explicit self-report measures. Pers Soc Psychol Bull. 2005;31:1369–1386. doi: 10.1177/0146167205275613. [DOI] [PubMed] [Google Scholar]
- 60.Leete E. How I perceive and manage my illness. Schizophr Bull. 1989;15:197–200. doi: 10.1093/schbul/15.2.197. [DOI] [PubMed] [Google Scholar]