Abstract
Objective
Adolescence is an important period of risk for the development of lifelong smoking behaviors. Compelling, although inconsistent, evidence suggests a relation between parental smoking and the risk of smoking initiation during adolescence. This study investigates unresolved issues concerning the strength and nature of the association between parent smoking and offspring smoking initiation.
Methods
We enrolled 564 adolescents aged 12-17, along with one of their parents, into the New England Family Study between 2001-2004. Lifetime smoking histories were obtained from parents and their adolescent offspring. Discrete-time survival analysis was used to investigate the influence of parental smoking histories on the risk of adolescent smoking initiation.
Results
Parental smoking was associated with a significantly higher risk of smoking initiation in adolescent offspring (odds ratio=2.81, 95% CI=1.78, 4.41). In addition, the likelihood of offspring smoking initiation increased with the number of smoking parents and the duration of exposure to parental smoking, suggesting a dose-response relation between parental smoking and offspring smoking. Offspring of parents who had quit smoking were no more likely to smoke than offspring of parents who had never smoked. The effects of parental smoking on offspring initiation differed by sex (with a stronger effect of father's smoking on boys than girls), developmental period (with a stronger effect of parental smoking before the adolescent was age 13 than afterwards), and residence of parents (with effects of father's smoking being dependent on living in the same household as the adolescent). Parental smoking was also associated with stronger negative reactions to adolescents' first cigarette, a potential marker of the risk of progression to higher levels of use.
Conclusions
Parental smoking is an important source of vulnerability to smoking initiation among adolescents, and parental smoking cessation might attenuate this vulnerability.
Keywords: Smoking, adolescents, parent-offspring transmission
Most adult smokers began smoking during adolescence;1-3 preventing adolescent smoking initiation is therefore important for reducing the public health burden of smoking-related illnesses over the life course. There is accumulating evidence that parental smoking increases the risk for adolescent smoking initiation;4-19 however, unresolved issues persist concerning the strength and nature of the association between parent smoking and initiation of smoking in offspring.20 For example, while parental smoking and parental nicotine dependence have each been linked with an increased risk of offspring smoking,21,22 few studies of intergenerational transmission have addressed their comparative effects. Evidence from one such study suggests that the effect of maternal smoking on offspring smoking is largely irrespective of maternal nicotine dependence.18
Prior evidence of a dose-response relationship between parental smoking and offspring initiation is also mixed. In some studies, the risk of adolescent smoking increased with the number of smoking parents23,24 and the number of years exposed to parental smoking.25 In contrast, there are inconsistent reports showing that either maternal smoking alone is the key determinant of intergenerational transmission,26 maternal smoking and paternal smoking equally influence offspring smoking,8,22 and that maternal smoking has a stronger effect on offspring smoking than paternal smoking.26-28 Finally, there is mixed evidence regarding the stability of parental influences on adolescent smoking behaviors, indicating either that parental influences wane over the course of development as peer influences strengthen29,30 or that they endure throughout adolescence.31
This study investigates the relation between parental smoking and smoking initiation in adolescent offspring in a new generation of participants recruited into the New England Family Study. We address the following questions regarding the intergenerational transmission of smoking: 1) whether parental smoking increases the risk of offspring smoking initiation, and whether this increased risk persists even if parents quit smoking; 2) the effect of parental nicotine dependence on offspring initiation; 3) dose-response relations between parental smoking and offspring initiation; 4) gender-specificity of parental smoking effects on adolescent initiation; and 5) variation in parental smoking effects by age of the adolescent. We also examine subjective reactions to the 1st cigarette among adolescent smokers to determine if there are links with parental smoking. Enhancing our understanding of the intergenerational transmission of smoking will provide further insight into avenues of prevention, particularly with respect to the potential for smoking cessation interventions in adults to reduce smoking in subsequent generations.14,32-34
METHODS
Sample ascertainment and interview procedures
The New England Family Study (NEFS) was established to locate and interview the second-generation (G2) offspring of mothers enrolled in the Boston and Providence cohorts of the National Collaborative Perinatal Project35-39 and their third-generation (G3) adolescent grandchildren. As described previously,40,41 G2 participants were selected through a multi-stage sampling procedure. We mailed screening questionnaires to 4,579 of the 15,721 National Collaborative Perinatal Project G2 offspring who survived until age 7. Of the 3,121 questionnaires returned (68.2%), we identified 2,271 G2 offspring who were eligible for participation, and enrolled 1,674 (73.7%). Following the G2 interview, we obtained parental consent to invite their age-eligible biological children to participate in the study. Adolescents between ages 12 and 17 who were living within 100 miles of either study site in Providence or Boston were eligible for participation.
Measures
We obtained detailed information from the G2 parents' regarding their lifetime smoking history, including age at first cigarette, progression to regular smoking (defined as smoking weekly for ≥2 months), quit attempts, and periods of sustained abstinence. Lifetime history and age at onset of nicotine dependence based on Diagnostic and Statistical Manual-IVth Edition criteria42 were obtained from parents using a modified43 version of the Composite International Diagnostic Interview.44,45 We also obtained adolescents' reports of their exposure to maternal and paternal cigarette smoking.46,47 The intergenerational design allowed for matching the lifetime smoking history of biological parents to the age of offspring to determine the number of years of exposure to parental smoking and parental nicotine dependence.
Adolescent smoking was defined as any lifetime history of cigarette use. Age at smoking initiation was assessed with the question, “How old were you the very first time you ever smoked even a puff of tobacco?” Adolescents who smoked were asked about negative and positive reactions to their first cigarette, which were measured by 4 items assessing negative symptoms (unpleasant sensations, nausea, dizziness, and coughing, α=0.75) and 3 items assessing positive symptoms (pleasant sensations, relaxation, pleasurable rush or buzz, α=0.66). These symptoms were recorded on a 4-point scale ranging from 1=none to 4=intense, which were summed together and then standardized to a mean of 0 and standard deviation of 1.48,49
Analysis methods
We used discrete-time survival analysis to investigate the intergenerational transmission of smoking.50 Regression coefficients from these models, when exponentiated, indicate the factor by which each dimension of parental smoking increases or decreases the odds of adolescent smoking initiation. The dependent variable in these analyses was the adolescents' age at smoking initiation, which for adolescents who had never smoked was censored at their current age. We coded parental smoking as a time-varying covariate, thereby overcoming limitations of prior work in which parental smoking was assumed to be present or absent for the child's entire lifespan. For example, consider a prototypical parent who began smoking when his or her child was age five, met diagnostic criteria for nicotine dependence when the child was age 8, and subsequently quit smoking when the child was age 11. Parental smoking for this individual would be coded as `none' in person-years 1-4, `regular smoker' in person-years 5-7, `nicotine dependent' in person-years 8-10, and `former smoker' thereafter.
Covariates included in all models were indicator variables representing the baseline rate of initiation in each person-year, sex, race/ethnicity, and age at interview. Among adolescents who smoked at least once in their lifetimes, we compared age-adjusted scores on the standardized scales of positive and negative reactions to their first cigarette according to whether or not either parent was smoking in the year they initiated. All variance estimates were adjusted for the presence of multiple siblings per family.51
RESULTS
Characteristics of the parent and offspring samples, and comparisons with non-interviewed subjects
We identified 726 adolescent offspring who were eligible for inclusion in NEFS-G3 cohort, and completed in-person interviews of 569 adolescents (78.4%). Five adolescents were excluded from the NEFS-G3 cohort because of problems with interview administration. Due to missing data on either adolescent or parental smoking, an additional five G3 adolescents were excluded from the current analyses, resulting in an analytic sample of 559 adolescents (180 singletons and 176 sibling sets).
The characteristics of the full NEFS-G2 sample (n=1,674), G2 parents with eligible offspring (n=466), and of G2 parents whose offspring were included in the current analysis (n=356) are shown in the first three columns of table 1. G2 parents with enrolled offspring were more likely to be female than the full NEFS sample; the age, race/ethnicity, and education distributions of the G2 parents were comparable across the groups of parents with eligible and enrolled adolescents. The distributions of lifetime regular smoking among parents with eligible and enrolled offspring were similar (64.1% and 62.4%, respectively), as were the distributions of lifetime nicotine dependence (46.1% and 46.0%, respectively). The mean (standard deviation) age of the adolescent sample was 14.0 (1.7) years (range=12-17); the sample was 52.2% female.
Table 1.
Characteristics of parents and adolescent offspring selected and enrolled into the NEFS-G3 cohort
| Parental Characteristics |
Adolescent Characteristics |
||||
|---|---|---|---|---|---|
| All NEFS G2's (n=1674) | G2's with eligible G3 offspringa (n=466) | G2's whose offspring were included in the analysis sample (n=356) | Eligible G3's (n=726) | Final analysis sample of G3 adolescents (n=559) | |
| Mean Age (SD) | 39.2 (1.9) | 40.0 (1.85) | 39.6 (1.9) | 14.0 (1.9) | 14.0 (1.7) |
| Percent female (n) | 59.2% (991) | 71.5% (333) | 77.8% (277) | 52.5% (379) | 52.2% (292) |
| G2 Race/ethnicity | |||||
| Percent white (n) | 83.5% (1354) | 81.8% (372) | 85.0% (301) | ||
| Percent non-white (n) | 16.5% (268) | 18.2% (83) | 15.7% (56) | ||
| G2 Education | |||||
| Percent college or more (n) | 57.7% (937) | 45.5% (208) | 49.0% (173) | ||
| Percent high school (n) | 36.4% (591) | 47.9% (219) | 46.4% (165) | ||
| Percent less than high school (n) | 6.0% (97) | 6.6% (30) | 5.1% (18) | ||
| G2 Smoking characteristics | |||||
| Percent lifetime regular smokers (n) | 58.5% (949) | 64.1% (293) | 62.4% (222) | ||
| Percent lifetime nicotine dependence (n) | 39.0% (625) | 46.1% (207) | 46.0% (161) | ||
Not included in this column are an additional 101 G2's whose adolescent children were ineligible for participation in the study based on living >100 miles from one of the study sites or not being a biological child. The prevalence of regular smoking among G2 parents whose children were ineligible for participation (66.7%) was similar to that among G2 parents with eligible children (64.1%).
Prevalence of smoking initiation in adolescent offspring
The prevalence of lifetime cigarette use was 27.8% (n=157), ranging from 7.2% among adolescents interviewed at age 12 to 61.3% among adolescents interviewed at age 17. The mean (SD) age of first smoking was 12.4 (2.4). The prevalence of lifetime cigarette use was 30.7% (n=83) among males, and 25.2% (n=74) among females.
Survival analysis of smoking initiation in adolescent offspring
Incidence rates of adolescent smoking initiation were calculated: 1) during person-years prior to the onset of regular parental smoking; 2) during person-years of exposure to active parental regular smoking; and 3) during person-years following parental smoking cessation. These rates were 1.35, 2.84, and 2.23 (per 100 person-years), respectively, indicating a higher likelihood of initiation in the context of exposure to active parental smoking. A similar pattern emerged in the survival analysis of smoking initiation. Exposure to active parental smoking was strongly related to offspring initiation (adjusted odds ratio=2.81; CI=1.78, 4.41), in contrast to former parental smoking, which was not related to offspring initiation (OR=1.03; CI=0.61, 1.74).
Active parental smoking—either with or without exposure to parental nicotine dependence—was associated with an elevated risk of offspring initiation. Table 2 presents the distribution of adolescent smoking initiation according to the G2 parent's smoking status, with a separate category for exposure to parental nicotine dependence. There was no difference in the likelihood of initiation between adolescents whose G2 parent was a nicotine dependent smoker and adolescents whose G2 parent was a regular smoker without symptoms of nicotine dependence. Therefore, the remaining analyses focus on active parental smoking alone, and do not distinguish between former versus never parental smoking, nor between parental smoking and nicotine dependence.
Table 2.
Parental smoking status in each person-year and the risk of smoking initiation among their adolescent offspring
| Person-years | Number of adolescents initiating | Rate of smoking initiation per 100 person-years | Odds ratioa | 95% CI | |
|---|---|---|---|---|---|
| Parental smoking status | |||||
| Active smoking with nicotine dependence | 1,502 | 51 | 3.40 | 3.06 | 1.90,4.91 |
| Active smoking without nicotine dependence | 924 | 20 | 2.16 | 2.30 | 1.21,4.39 |
| Quit smoking, former nicotine dependence | 972 | 22 | 2.26 | 1.13 | 0.65, 1.98 |
| Quit smoking, never dependent | 540 | 6 | 1.11 | 0.77 | 0.30, 1.96 |
| Never a weekly smoker | 2,960 | 40 | 1.35 | 1 | referent |
Odds ratios estimated from a discrete-time survival analysis of the age at smoking initiation also adjusting for the G2 parent's sex, adolescent sex, age at interview, and the baseline hazard of initiation in each year of life.
Using the life-chart method,52 adolescents were asked to indicate the years of their life in which their mother and father smoked; this information enabled us to determine the duration of exposure to both biological parents' smoking. Adolescents' reports were highly correlated with their G2 parents' own reports: the correlation between the number of years of mothers' self-reported smoking and adolescent reports of maternal smoking was 0.89; the correlation between fathers' self-reported smoking and adolescent reports of paternal smoking was 0.88.
We tested for a dose-response relation between parent smoking and offspring smoking by comparing the risk of initiation according to the number of smoking parents and according to the duration of exposure to parental smoking. Exposure to one parent's smoking was associated with a 1.45 times higher odds of initiation (CI=0.82, 2.59), and exposure to both parents' smoking raised the odds of offspring initiation almost threefold (OR=2.75; CI=1.48, 5.08). In addition, a prolonged duration of exposure to parental smoking was associated with a higher risk of offspring initiation; we observed a threshold effect of duration, in that adolescents exposed to 4 (OR=3.29; CI=1.28, 8.46) or ≥5 (OR=1.82; CI=0.95, 3.51) years of parental smoking, compared to 0 years, exhibited elevated risks of initiation.
In gender-specific analyses, mother's (OR=2.34; CI=1.57, 3.51) and father's (OR=1.67; CI=1.12, 2.48) smoking independently raised the risk of offspring smoking initiation, and overall, the effects of mother's smoking and father's smoking were not significantly different from one another (χ2=1.1, df=1, p=0.307). However, there was evidence of a differential effect of father's smoking according to offspring sex (χ2 for the interaction between father's smoking and offspring sex=4.5, df=1, p=0.034), indicating a stronger effect of father's smoking on boys than girls. We also observed a stronger effect of parental smoking prior to the teen years than at age 13 or after (χ2 for the interaction between parental smoking and adolescent age=4.2, df=1, p=0.042). Finally, incorporating information from adolescents' reports of which years of their lives they were living with each biological parent into the analysis, we observed a differential effect of paternal smoking depending on the presence of the father in the household (χ2 for the interaction between paternal smoking and father's presence in the household=5.0, df=1, p=0.026). Adolescents living with smoking fathers were more than three times as likely to initiate smoking; in contrast, non-resident father's smoking had no effect on the risk of their offspring's initiation. Odds ratios for the differential effects of parental smoking according to offspring sex, offspring age, and the presence of the father in the household, are presented in table 3.
Table 3.
Differential effects of parental smoking according to offspring sex, age, and the presence of the father in the household
| Odds Ratio | 95% CI | Odds Ratio | 95% CI | |
|---|---|---|---|---|
| Differential effects according to offspring sex |
||||
| Girlsa |
Boysa |
|||
| Mother's Smoking | 2.73 | 1.50,4.98 | 2.29 | 1.39,3.77 |
| Father's Smoking | 1.06 | 0.59, 1.89 | 2.39 | 1.45,3.92 |
| Differential effects according to offspring age |
||||
| ≤Age 12b |
≥Age 13b |
|||
| Mother's or Father's Smoking | 3.63 | 2.07, 6.36 | 1.71 | 1.06,2.76 |
| Differential effects according to father's presence in the household |
||||
| Father at homec |
Father not at homec |
|||
| Father's Smoking | 3.18 | 1.93,5.23 | 1.13 | 0.59,2.17 |
Results of two discrete-time survival models of the age at smoking initiation, one estimated for girls and one for boys. Models also adjusted for age at interview and the baseline hazard of initiation in each year of life.
Results of two discrete-time survival models of the age at smoking initiation, one estimate for person-years through age 12, and one for person-years 13 and above. Models also adjusted for adolescent sex, age at interview, and the baseline hazard of initiation in each year of life.
Results of two discrete-time survival models of the age at smoking initiation, one estimate for person-years in which the father was living at home, and one for person-years when father was not living at home. Models also adjusted for adolescent sex, age at interview, and the baseline hazard of initiation in each year of life.
Parental smoking status and adolescents' first smoking experiences
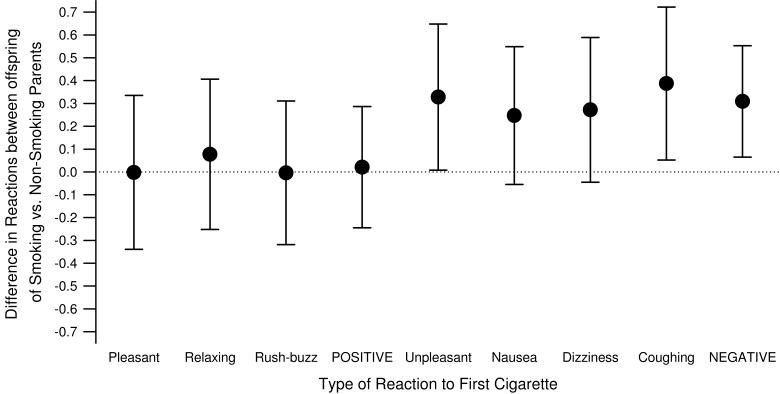
First smoking reactions are a potential marker of the risk of progression, and therefore we compared adolescents' reactions to their first cigarette according to parental smoking status in the year of initiation. Offspring of current smokers reported significantly stronger negative reactions (unpleasant sensations, coughing, and overall negative reactions) to their first cigarette than offspring of non-smoking parents (Figure 1). There were no differences in the level of adolescents' positive reactions to their first cigarette across categories of parental smoking status.
Figure 1. Reactions to first smoking experience associated with parental smoking in the year of adolescent smoking initiation (n=157).
Differences (and 95% confidence intervals) in age-adjusted standardized scores of negative and positive reactions to adolescents' first cigarette between offspring of smoking versus non-smoking parents.48,49 Means are shown for the individual items and also the summary scores of POSITIVE and NEGATIVE reactions.
DISCUSSION
We investigated the intergenerational transmission of smoking in the adolescent cohort of the New England Family Study. The dimensions of parents' smoking that were most strongly predictive of smoking initiation were active regular smoking, as opposed to prior smoking or nicotine dependence, and the number of smoking parents. We also observed differential effects according to sex (with a stronger effect of father's smoking on boys), developmental period (with a stronger effect of parental smoking before age 13 than afterwards), and residence of parents (with resident fathers' smoking predictive of offspring initiation, but not non-resident fathers' smoking).
Distinguishing the effects of current and former parental smoking has direct implications for prevention insofar as parental cessation may reduce the risk of adolescent smoking initiation.17,33 Our results demonstrated that only active parental smoking was associated with an increased risk of smoking initiation in offspring, and that children whose parents had quit smoking were no more likely to begin smoking than children whose parents had never smoked. These findings are consistent with a social learning model of smoking initiation, which posits that attitudes, beliefs, and behaviors toward cigarette use are learned through modeling.17,33,53,54 Adolescents may therefore observe smoking, imitate smoking, and absorb favorable outcome expectations over time with repeated exposure. The findings for resident fathers' smoking are also consistent with a social learning model, in that a custodial father who smokes has a greater influence on smoking initiation than a non-custodial father who smokes, by virtue of his greater contact with the adolescent. The absence of an elevated risk of initiation associated with former parental smoking implies that not only do adolescents imitate their parents' smoking behaviors, but potentially their parents' cessation behaviors as well; however, we did not directly analyze adolescents' cessation behaviors in this study.
Nicotine dependence may represent more intense and persistent parental smoking,55-57 and may also be indicative of a broader constellation of parental psychopathology,58 both of which would be expected to increase the risk of offspring initiation. However, we observed no difference in the risk of smoking initiation between person-years of exposure to active parental smoking (without nicotine dependence) and person-years of exposure to parental nicotine dependence. Although our study might have lacked the temporal precision needed to distinguish between parental smoking and parental nicotine dependence, our results are consistent with prior evidence that parental nicotine dependence does not increase the risk of adolescent smoking beyond the risk conferred by parental smoking.18
We found that each additional smoking parent was associated with an increased risk of adolescent initiation, as was exposure to ≥4 years of exposure to parental smoking. In addition, maternal and paternal smoking were both related to the risk of offspring smoking initiation. While maternal smoking predicted smoking initiation among sons and daughters, paternal smoking was predictive only among sons. Considering the strong effect of custodial parent's smoking that we observed, it is conceivable that these gender differences in the effects of parental smoking reflect the gender of the custodial parent rather than inherent differences in the effects of mothers' versus fathers' smoking. We also observed that parental smoking was more strongly predictive of offspring smoking initiation prior to age 13 than at age 13 and beyond.
Finally, we observed stronger negative reactions to smoking among adolescents whose parents were currently smoking at the time of their first cigarette. Prior evidence relates both positive and negative initial smoking experiences to the development of regular smoking and nicotine dependence.48,49,59-62 The counterintuitive finding of aversive reactions to initial smoking predicting escalating levels of use has been hypothesized to reflect a heightened sensitivity to nicotine, and consequently a heightened vulnerability to the reinforcing effects of nicotine.62 If this is the case, then our findings suggest a correlation between parental smoking and offspring sensitivity to nicotine. We could not, however, differentiate adolescents' reactions to nicotine from their reactions to other constituents in cigarette smoke.
Limitations of this study include the use of parents' retrospective reports of lifetime smoking to establish patterns of cigarette smoking, symptoms of nicotine dependence, and ages at smoking onset and offset. Adolescents' ages at smoking initiation were also reported retrospectively. Inaccuracies in these reports may have weakened our ability to distinguish between various aspects of intergenerational transmission. In addition, information on parental smoking was obtained partly by self-report and partly by adolescent report, giving rise to the possibility of overestimating the intergenerational transmission if there were systematic reporting biases. We found a high degree of correspondence between parent-reported and child-reported parental smoking, and no systematic difference in concordance for mother versus father smoking.63 Consistent with this, the intergenerational transmission models that relied exclusively on parents' self-reported smoking were similar to those that included parental smoking information obtained from parents and adolescents. Finally, we emphasize that our current findings are specific to smoking initiation defined as first puff of a cigarette. However, prior research has shown that smoking just once is associated with a higher risk of subsequent regular smoking.64
CONCLUSIONS
The results of this study expand our understanding of the intergenerational transmission of smoking. With respect to smoking initiation during adolescence, the aspects of parental smoking that emerged as most important were active parental smoking, number of smoking parents, maternal smoking (and for boys, paternal smoking), and exposure to parental smoking prior to adolescence. There was no elevated risk of smoking initiation among adolescents whose parents were former smokers. Future work with the NEFS-G3 sample includes examining hypothesized mechanisms of intergenerational transmission such as parental socioeconomic status and parental psychopathology;29,65,66 how peer and sibling smoking interact with parental smoking;16 effects of non-biological parents on offspring smoking;6 and the ways in which parental smoking impacts their offspring's progression to regular smoking, nicotine dependence, and likelihood of smoking cessation in adulthood.9,67 A deeper understanding of the intergenerational transmission of cigarette smoking will provide further insight into avenues of prevention, in particular family-based interventions and those that emphasize assisting parents in cessation efforts that will not only reduce the parent's smoking but likely reduce smoking uptake in subsequent generations.
ACKNOWLEDGEMENTS
This research was supported in part by grants from the National Institutes of Health (Transdisciplinary Tobacco Use Research Center Award P50 CA084719; K07 CA95623 (Stanton)) and from the Robert Wood Johnson Foundation. The authors sincerely appreciate the contribution of Ms. Kathleen McGaffigan for statistical programming and data management.
Abbreviations
- (NEFS)
New England Family Study
- (G2)
second-generation
- (G3)
third-generation
Footnotes
Financial disclosure and conflicts of interest: None
REFERENCES
- 1.Giovino GA, Henningfield JE, Tomar SL, Escobedo LG, Slade J. Epidemiology of tobacco use and dependence. Epidemiologic Reviews. 1995;17(1):48–65. doi: 10.1093/oxfordjournals.epirev.a036185. [DOI] [PubMed] [Google Scholar]
- 2.Escobedo LG, Anda RF, Smith PF, Remington PL, Mast EE. Sociodemographic characteristics of cigarette smoking initiation in the United States. Implications for smoking prevention policy. Jama. 1990;264(12):1550–1555. [PubMed] [Google Scholar]
- 3.Gilpin EA, Lee L, Evans N, Pierce JP. Smoking initiation rates in adults and minors: United States, 1944-1988. American Journal of Epidemiology. 1994;140(6):535–543. doi: 10.1093/oxfordjournals.aje.a117280. [DOI] [PubMed] [Google Scholar]
- 4.Bricker JB, Peterson AV, Jr., Sarason IG, Andersen MR, Rajan KB. Changes in the influence of parents' and close friends' smoking on adolescent smoking transitions. Addict Behav. 2007;32(4):740–757. doi: 10.1016/j.addbeh.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 5.Otten R, Engels RC, van de Ven MO, Bricker JB. Parental smoking and adolescent smoking stages: the role of parents' current and former smoking, and family structure. J Behav Med. 2007;30(2):143–154. doi: 10.1007/s10865-006-9090-3. [DOI] [PubMed] [Google Scholar]
- 6.Fidler JA, West R, van Jaarsveld CH, Jarvis MJ, Wardle J. Smoking status of step-parents as a risk factor for smoking in adolescence. Addiction. 2008;1033:496–501. doi: 10.1111/j.1360-0443.2007.02086.x. [DOI] [PubMed] [Google Scholar]
- 7.Volk HE, Scherrer JF, Bucholz KK, et al. Evidence for specificity of transmission of alcohol and nicotine dependence in an offspring of twins design. Drug Alcohol Depend. 2007;87(23):225–232. doi: 10.1016/j.drugalcdep.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 8.Peterson AV, Jr., Leroux BG, Bricker J, et al. Nine-year prediction of adolescent smoking by number of smoking parents. Addict Behav. 2006;31(5):788–801. doi: 10.1016/j.addbeh.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 9.McGee R, Williams S, Reeder A. Parental tobacco smoking behaviour and their children's smoking and cessation in adulthood. Addiction. 2006;101(8):1193–1201. doi: 10.1111/j.1360-0443.2006.01486.x. [DOI] [PubMed] [Google Scholar]
- 10.Bricker JB, Peterson AV, Jr., Leroux BG, Andersen MR, Rajan KB, Sarason IG. Prospective prediction of children's smoking transitions: role of parents' and older siblings' smoking. Addiction. 2006;101(1):128–136. doi: 10.1111/j.1360-0443.2005.01297.x. [DOI] [PubMed] [Google Scholar]
- 11.Shakib S, Zheng H, Johnson CA, et al. Family characteristics and smoking among urban and rural adolescents living in China. Preventive Medicine. 2005;40(1):83–91. doi: 10.1016/j.ypmed.2004.05.029. [DOI] [PubMed] [Google Scholar]
- 12.Hill KG, Hawkins JD, Catalano RF, Abbott RD, Guo J. Family influences on the risk of daily smoking initiation. Journal of Adolescent Health. 2005;37(3):202–210. doi: 10.1016/j.jadohealth.2004.08.014. [DOI] [PubMed] [Google Scholar]
- 13.Chassin L, Presson CC, Rose J, Sherman SJ, Davis MJ, Gonzalez JL. Parenting style and smoking-specific parenting practices as predictors of adolescent smoking onset. J Pediatr Psychol. 2005;30(4):333–344. doi: 10.1093/jpepsy/jsi028. [DOI] [PubMed] [Google Scholar]
- 14.Bricker JB, Rajan KB, Andersen MR, Peterson AV., Jr. Does parental smoking cessation encourage their young adult children to quit smoking? A prospective study. Addiction. 2005;100(3):379–386. doi: 10.1111/j.1360-0443.2005.00997.x. [DOI] [PubMed] [Google Scholar]
- 15.Kodl MM, Mermelstein R. Beyond modeling: Parenting practices, parental smoking history, and adolescent cigarette smoking. Addictive Behaviors. 2004;29(1):17–32. doi: 10.1016/s0306-4603(03)00087-x. [DOI] [PubMed] [Google Scholar]
- 16.Engels RC, Vitaro F, Blokland ED, de Kemp R, Scholte RH. Influence and selection processes in friendships and adolescent smoking behaviour: the role of parental smoking. J Adolesc. 2004;27(5):531–544. doi: 10.1016/j.adolescence.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 17.den Exter Blokland EA, Engels RC, Hale WW, 3rd, Meeus W, Willemsen MC. Lifetime parental smoking history and cessation and early adolescent smoking behavior. Prev Med. 2004;38(3):359–368. doi: 10.1016/j.ypmed.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 18.Lieb R, Schreier A, Pfister H, Wittchen HU. Maternal smoking and smoking in adolescents: a prospective community study of adolescents and their mothers. Eur Addict Res. 2003;9(3):120–130. doi: 10.1159/000070980. [DOI] [PubMed] [Google Scholar]
- 19.Bricker JB, Leroux BG, Peterson AV, Jr., et al. Nine-year prospective relationship between parental smoking cessation and children's daily smoking. Addiction. 2003;98(5):585–593. doi: 10.1046/j.1360-0443.2003.00343.x. [DOI] [PubMed] [Google Scholar]
- 20.Avenevoli S, Merikangas KR. Familial influences on adolescent smoking. Addiction. 2003;98(Suppl 1):1–20. doi: 10.1046/j.1360-0443.98.s1.2.x. [DOI] [PubMed] [Google Scholar]
- 21.Dierker LC, Canino G, Merikangas KR. Association between parental and individual psychiatric/substance use disorders and smoking stages among Puerto Rican adolescents. Drug Alcohol Depend. 2006;84(2):144–153. doi: 10.1016/j.drugalcdep.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 22.Hu MC, Davies M, Kandel DB. Epidemiology and correlates of daily smoking and nicotine dependence among young adults in the United States. Am J Public Health. 2006;96(2):299–308. doi: 10.2105/AJPH.2004.057232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kardia SL, Pomerleau CS, Rozek LS, Marks JL. Association of parental smoking history with nicotine dependence, smoking rate, and psychological cofactors in adult smokers. Addict Behav. 2003;28(8):1447–1452. doi: 10.1016/s0306-4603(02)00245-9. [DOI] [PubMed] [Google Scholar]
- 24.Rossow I, Rise J. Concordance of parental and adolescent health behaviors. Soc Sci Med. 1994;38(9):1299–1305. doi: 10.1016/0277-9536(94)90193-7. [DOI] [PubMed] [Google Scholar]
- 25.Fergusson DM, Horwood LJ, Boden JM, Jenkin G. Childhood social disadvantage and smoking in adulthood: results of a 25-year longitudinal study. Addiction. 2007;102(3):475–482. doi: 10.1111/j.1360-0443.2006.01729.x. [DOI] [PubMed] [Google Scholar]
- 26.Kandel DB, Wu P. The contributions of mothers and fathers to the intergenerational transmission of cigarette smoking in adolescence. Journal of Research on Adolescence. 1995;5(2):225–252. [Google Scholar]
- 27.Rohde P, Lewinsohn PM, Brown RA, Gau JM, Kahler CW. Psychiatric disorders, familial factors and cigarette smoking: I. Associations with smoking initiation. Nicotine Tob Res. 2003;5(1):85–98. doi: 10.1080/1462220031000070507. [DOI] [PubMed] [Google Scholar]
- 28.Swan AV, Creeser R, Murray M. When and why children first start to smoke. Int J Epidemiol. 1990;19(2):323–330. doi: 10.1093/ije/19.2.323. [DOI] [PubMed] [Google Scholar]
- 29.Turner L, Mermelstein R, Flay B. Individual and contextual influences on adolescent smoking. Ann N Y Acad Sci. 2004;1021:175–197. doi: 10.1196/annals.1308.023. [DOI] [PubMed] [Google Scholar]
- 30.Wilkinson AV, Schabath MB, Prokhorov AV, Spitz MR. Age-related differences in factors associated with smoking initiation. Cancer Causes Control. 2007;18(6):635–644. doi: 10.1007/s10552-007-9008-6. [DOI] [PubMed] [Google Scholar]
- 31.Bricker JB, Peterson AV, Jr., Andersen MR, Sarason IG, Rajan KB, Leroux BG. Parents' and older siblings' smoking during childhood: changing influences on smoking acquisition and escalation over the course of adolescence. Nicotine Tob Res. 2007;9(9):915–926. doi: 10.1080/14622200701488400. [DOI] [PubMed] [Google Scholar]
- 32.Chassin L, Presson C, Rose J, Sherman SJ, Prost J. Parental smoking cessation and adolescent smoking. J Pediatr Psychol. 2002;27(6):485–496. doi: 10.1093/jpepsy/27.6.485. [DOI] [PubMed] [Google Scholar]
- 33.Farkas AJ, Distefan JM, Choi WS, Gilpin EA, Pierce JP. Does parental smoking cessation discourage adolescent smoking? Prev Med. 1999;28(3):213–218. doi: 10.1006/pmed.1998.0451. [DOI] [PubMed] [Google Scholar]
- 34.Jackson C, Henriksen L. Do as I say: Parent smoking, antismoking socialization, and smoking onset among children. Addictive Behaviors. 1997;22(1):107–114. doi: 10.1016/0306-4603(95)00108-5. [DOI] [PubMed] [Google Scholar]
- 35.Hardy JB. The Collaborative Perinatal Project: lessons and legacy. Ann Epidemiol. 2003;13(5):303–311. doi: 10.1016/s1047-2797(02)00479-9. [DOI] [PubMed] [Google Scholar]
- 36.Broman S. The Collaborative Perinatal Project: an Overview. In: Mednick SA, Harway M, Finello KM, editors. Handbook of Longitudinal Research. Praeger; New York: 1984. pp. 185–215. [Google Scholar]
- 37.Nichols PL, Chen T-C. Minimal brain dysfunction: a prospective study. Lawrence Erlbaum Associates; Hillsdale, N.J.: 1981. [Google Scholar]
- 38.Broman SH, Nichols PL, Kennedy WA. Preschool IQ: prenatal and early developmental correlates. L. Erlbaum Associates; Hillsdale, N.J.: 1975. distributed by the Halsted Press Division of Wiley. [Google Scholar]
- 39.Niswander KR, Gordon M. The women and their pregnancies: the Collaborative Perinatal Study of the National Institute of Neurological Diseases and Stroke. National Institute of Health; Washington: 1972. [Google Scholar]
- 40.Gilman SE, Martin LT, Abrams DB, et al. Educational attainment and cigarette smoking: a causal association? Int J Epidemiol. 2008;37(3):615–624. doi: 10.1093/ije/dym250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Graham AL, Papandonatos GD, Depue JD, et al. Lifetime Characteristics of Participants and Non-participants in a Smoking Cessation Trial: Implications for External Validity and Public Health Impact. Ann Behav Med. 2008 doi: 10.1007/s12160-008-9031-1. [DOI] [PubMed] [Google Scholar]
- 42.American Psychiatric Association . Diagnostic and statistical manual of mental disorders: DSM-IV-TR. 4th ed. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- 43.Dierker LC, Donny E, Tiffany S, Colby SM, Perrine N, Clayton RR. The association between cigarette smoking and DSM-IV nicotine dependence among first year college students. Drug Alcohol Depend. 2007;86(23):106–114. doi: 10.1016/j.drugalcdep.2006.05.025. [DOI] [PubMed] [Google Scholar]
- 44.Wittchen HU. Reliability and validity studies of the WHO--Composite International Diagnostic Interview (CIDI): a critical review. J Psychiatr Res. 1994;28(1):57–84. doi: 10.1016/0022-3956(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 45.Cottler LB, Robins LN, Grant BF, et al. The CIDI-core substance abuse and dependence questions: cross-cultural and nosological issues. The WHO/ADAMHA Field Trial. Br J Psychiatry. 1991;159:653–658. doi: 10.1192/bjp.159.5.653. [DOI] [PubMed] [Google Scholar]
- 46.Coultas DB, Peake GT, Samet JM. Questionnaire assessment of lifetime and recent exposure to environmental tobacco smoke. Am J Epidemiol. 1989;130(2):338–347. doi: 10.1093/oxfordjournals.aje.a115340. [DOI] [PubMed] [Google Scholar]
- 47.Sandler DP, Shore DL. Quality of data on parents' smoking and drinking provided by adult offspring. Am J Epidemiol. 1986;124(5):768–778. doi: 10.1093/oxfordjournals.aje.a114453. [DOI] [PubMed] [Google Scholar]
- 48.Pomerleau OF, Pomerleau CS, Namenek RJ. Early experiences with tobacco among women smokers, ex-smokers, and never-smokers. Addiction. 1998;93(4):595–599. doi: 10.1046/j.1360-0443.1998.93459515.x. [DOI] [PubMed] [Google Scholar]
- 49.Pomerleau CS, Pomerleau OF, Namenek RJ, Marks JL. Initial exposure to nicotine in college-age women smokers and never-smokers: a replication and extension. J Addict Dis. 1999;18(3):13–19. doi: 10.1300/J069v18n03_02. [DOI] [PubMed] [Google Scholar]
- 50.Cox DR. Regression models and life-tables. Journal of the Royal Statistical Society, Series B (Methodological) 1972;34(2):187–220. [Google Scholar]
- 51.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42(1):121–130. [PubMed] [Google Scholar]
- 52.Lewis-Esquerre JM, Colby SM, Tevyaw TO, Eaton CA, Kahler CW, Monti PM. Validation of the timeline follow-back in the assessment of adolescent smoking. Drug Alcohol Depend. 2005;79(1):33–43. doi: 10.1016/j.drugalcdep.2004.12.007. [DOI] [PubMed] [Google Scholar]
- 53.Akers RL. Deviant behavior: a social learning approach. 3rd ed. Wadsworth Pub. Co.; Belmont, Calif.: 1985. [Google Scholar]
- 54.Bandura A. Social foundations of thought and action: a social cognitive theory. Prentice-Hall; Englewood Cliffs, N.J.: 1986. [Google Scholar]
- 55.Hughes JR. Distinguishing nicotine dependence from smoking: why it matters to tobacco control and psychiatry. Arch Gen Psychiatry. 2001;58(9):817–818. doi: 10.1001/archpsyc.58.9.817. [DOI] [PubMed] [Google Scholar]
- 56.Breslau N, Johnson EO, Hiripi E, Kessler R. Nicotine dependence in the United States: prevalence, trends, and smoking persistence. Arch Gen Psychiatry. 2001;58(9):810–816. doi: 10.1001/archpsyc.58.9.810. [DOI] [PubMed] [Google Scholar]
- 57.Fagerstrom KO, Kunze M, Schoberberger R, et al. Nicotine dependence versus smoking prevalence: comparisons among countries and categories of smokers. Tob Control. 1996;5(1):52–56. doi: 10.1136/tc.5.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Grant BF, Hasin DS, Chou SP, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61(11):1107–1115. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- 59.Shiffman S. Tobacco “chippers”--individual differences in tobacco dependence. Psychopharmacology (Berl) 1989;97(4):539–547. doi: 10.1007/BF00439561. [DOI] [PubMed] [Google Scholar]
- 60.Pomerleau OF, Collins AC, Shiffman S, Pomerleau CS. Why some people smoke and others do not: new perspectives. J Consult Clin Psychol. 1993;61(5):723–731. doi: 10.1037//0022-006x.61.5.723. [DOI] [PubMed] [Google Scholar]
- 61.Chen X, Stacy A, Zheng H, et al. Sensations from initial exposure to nicotine predicting adolescent smoking in China: a potential measure of vulnerability to nicotine. Nicotine Tob Res. 2003;5(4):455–463. doi: 10.1080/14622200307239. [DOI] [PubMed] [Google Scholar]
- 62.DiFranza JR, Savageau JA, Fletcher K, et al. Recollections and repercussions of the first inhaled cigarette. Addict Behav. 2004;29(2):261–272. doi: 10.1016/j.addbeh.2003.08.002. [DOI] [PubMed] [Google Scholar]
- 63.Marks JL, Swan GE, Pomerleau CS, Pomerleau OF. Agreement between proband and parental self-report of smoking behavior and nicotine dependence. Nicotine & Tobacco Research. 2003;5(4):527–533. doi: 10.1080/1462220031000118630. [DOI] [PubMed] [Google Scholar]
- 64.Fidler JA, Wardle J, Brodersen NH, Jarvis MJ, West R. Vulnerability to smoking after trying a single cigarette can lie dormant for three years or more. Tobacco Control. 2006;15(3):205–209. doi: 10.1136/tc.2005.014894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Conrad KM, Flay BR, Hill D. Why children start smoking cigarettes: predictors of onset. Br J Addict. 1992;87(12):1711–1724. doi: 10.1111/j.1360-0443.1992.tb02684.x. [DOI] [PubMed] [Google Scholar]
- 66.Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob Control. 1998;7(4):409–420. doi: 10.1136/tc.7.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mayhew KP, Flay BR, Mott JA. Stages in the development of adolescent smoking. Drug and Alcohol Dependence. 2000;59(Suppl 1):S61–81. doi: 10.1016/s0376-8716(99)00165-9. [DOI] [PubMed] [Google Scholar]