Researchers from a wide array of disciplines have investigated ancient “plagues”, from fields as diverse as microbiology, ancient history, epidemiology, zoology, palaeopathology and archaeology, both independently from each other or in collaborative multidisciplinary teams. This paper aims to discuss the role of archaeology within such investigations and, perhaps more significantly, to highlight some of the limitations of the archaeological data on which many such studies are based. Non-archaeologists may not fully appreciate these limitations, as archaeology invariably operates under the constraints of an incomplete, biased, poorly preserved and often problematic sample. Only once these limitations are taken into account can the archaeological record be used to its “full” potential. Applying scientific methods to, and developing elaborate theories from, archaeological material without taking such shortcomings into account can seriously affect academic validity. Nonetheless, archaeology has a role to play in the study of ancient “plagues”. Archaeological methods from a wide range of sub-disciplines can offer additional or alternative avenues of research that may help us identify and understand the diseases behind ancient “plagues”. The Black Death burial site at East Smithfield, London, will provide a background to the discussion.1
The Black Death in London
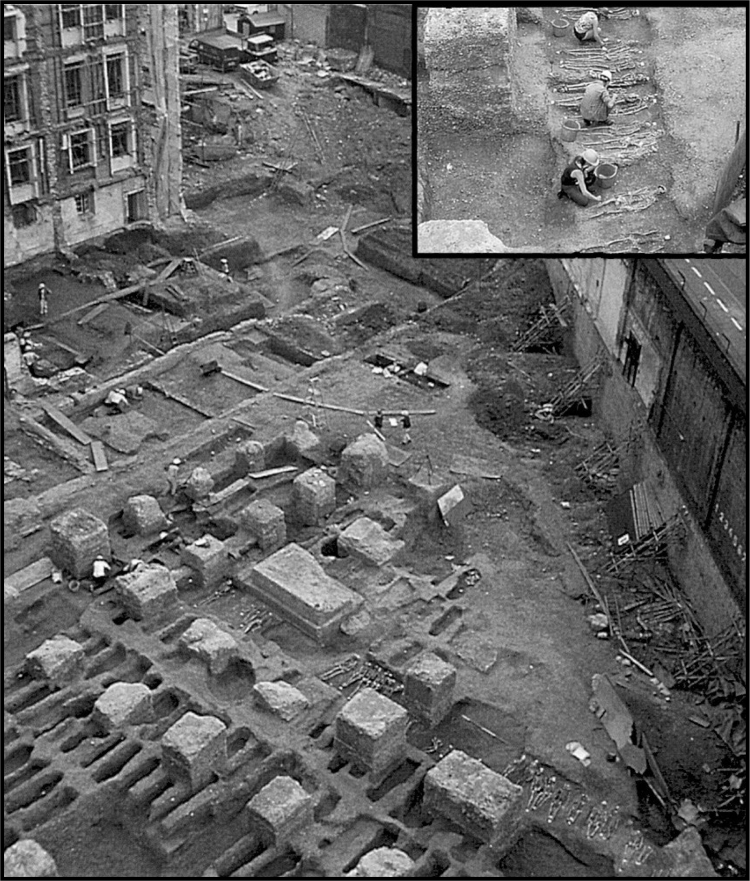
The Black Death is believed to have arrived in Europe from the Crimea during October 1347. It rapidly spread across Europe, arriving in Weymouth on the south coast of England in June/July 1348, and by November it had reached London.2 In the capital, the death rate rose rapidly from December 1348, reaching a peak in April 1349 and falling significantly by June 1349. The impact of the Black Death epidemic was catastrophic, and at its height, a contemporary observer stated that approximately 200 bodies a day were being buried.3 The disposal of so many dead ought to have left its mark in the archaeological record and, in 1986, a large cemetery was located on the site of the Royal Mint near the Tower of London, in East Smithfield. It was excavated by archaeologists from the Museum of London and, as shown in Figure 1, it contained two mass burial trenches and a mass burial pit, densely filled with several hundred articulated skeletons, as well as many individual graves.4 Written evidence confirms that, with West Smithfield, the East Smithfield Royal Mint cemetery was one of two emergency burial grounds created to cope with the Black Death epidemic.5 It is currently the largest and most comprehensively excavated Black Death cemetery in England, and the majority of an estimated 2400 people buried there are believed to have died from the Black Death, of which over 600 were recovered by the Museum of London.6 Opened in late 1348 or early 1349 by Ralph Stratford, the Bishop of London, it provides researchers and archaeologists with a unique assemblage of people who died at the peak of the Black Death epidemic in London.7 The cause of the epidemic has recently come under scrutiny and the established view that the Black Death was caused by the bacterium Yersinia pestis has been challenged.
Figure 1:
Mass-burial trench and graves from the Royal Mint cemetery of East Smithfield in London. The inset shows the mass-burial trench under excavation. (Courtesy of the Museum of London, © Museum of London.)
Plague and Yersinia pestis
From the Latin “plaga”, meaning “blow”, the word “plague” can be used in its broad sense to describe any large-scale calamity, such as an insect infestation or an epidemic disease with a high mortality rate. It is also often employed to describe a specific disease, the acute epidemic disease of rats and other wild rodents caused by the bacterium Yersinia pestis. In modern epidemics, the bacterium is usually transmitted to man by fleas—in particular by the rat flea Xenopsylla cheopis—resulting in the most common clinical form of the disease: bubonic plague. Although an uncommon occurrence in modern outbreaks, the bacterium Yersinia pestis can also enter the blood-stream (septicaemic plague) or the lungs (pneumonic plague), leading to highly fatal forms of the disease. Patients with bubonic plague are likely to suffer from high fever, delirium, aching limbs and painful swelling of the lymph nodes called buboes. In some patients, the buboes burst after a few days, releasing pus and then healing. In others, subcutaneous bleeding may occur, producing black patches that may lead to fatal ulcers. Until recently, it was widely believed that bubonic plague was behind the 1347–49 epidemic, and the presence of black subcutaneous lesions on some of the plague victims may have explained the origin of the term “Black Death”.8 However, some researchers have highlighted interesting differences between the epidemic of 1347–49 and more recent outbreaks of bubonic plague, raising the possibility that the bacterium Yersinia pestis was not behind the Black Death epidemic. A good review of the main arguments levelled against bubonic plague—as well as the more contagious pneumonic plague—can be found in Stephen Porter’s ‘An historical whodunit’.9 Indeed, works by Graham Twigg—The Black Death—and more recently by Susan Scott and Christopher Duncan—Biology of plagues and Return of the Black Death—as well as Samuel Cohn—The Black Death transformed10—have challenged the established view that Yersinia pestis and bubonic plague were the cause of the fourteenth-century epidemic.
The Black Death had a devastating impact on Europe. In contrast with the epidemiology of recent outbreaks of plague, the disease appears to have killed a large proportion of the population and to have swept rapidly across the continent. Europeans are unlikely to have had any prior exposure to Yersinia pestis, which could explain the unusually high overall mortality of the Black Death epidemic.11 As discussed by Porter, the role that rats—and their fleas—may have played in the spread of plague has come under some scrutiny by what some people have described as “plague-revisionists”.12 For example, the cool climatic conditions of northern Europe would have made it difficult for the rat fleas to reproduce, particularly during the winter months.13 This ought to have hampered, if not stopped, the spread of the disease during the winter period but there appears to be no evidence of this occurring. Plague outbreaks also tend to be preceded by the presence of many dead rats, as they are themselves susceptible to the plague, but there seems to be a lack of contemporary accounts mentioning dead rats in the medieval literature.14 In Europe, unlike Asia, there are no known plague-resistant wild rodents that would have acted as a natural reservoir for Yersinia pestis. It is difficult to explain how the bacterium continued to affect Europe for another three centuries without the presence of a local reservoir. Interestingly, despite two well-documented fifteenth-century plague epidemics in Iceland, rats are not believed to have settled on the island until much later.15
Most of the discrepancies highlighted in the literature rely on an absence of evidence, which—as all archaeologists know—is not evidence of absence. Nonetheless, such inconsistencies certainly warrant further investigation and Yersinia pestis is no longer regarded as the only suspect. Scott and Duncan have suggested that a highly lethal and contagious virus, similar to the filoviruses responsible for haemorrhagic fevers such as Ebola, was behind the Black Death epidemic.16
The Role of Archaeology
The investigation of ancient “plagues” has always relied upon a multidisciplinary approach, involving fields as diverse as ancient history and zoology. Archaeology’s contribution to the investigation has the potential to be multifaceted, as it encompasses numerous sub-disciplines, many of which may be relevant to such studies.
Vertebrate and invertebrate zooarchaeology: to investigate possible disease hosts or vectors.
Archaeobotany, geoarchaeology and palaeoecology: to reconstruct the climatic conditions during plague epidemics, and the impact this may have had on potential disease hosts or vectors.
Urban archaeology: to establish the “environmental” conditions and their impact on disease biology and disease transmission such as housing, population density, town size, water supply, transport, food supply and general facilities.
Material culture, burial archaeology and archaeological dating: to ascertain the date of burial sites through scientific dating and/or by the presence of artefacts, as well as any cultural information found in the burial (such as the care with which the bodies were buried or the quality and quantity of any offerings).
Bioarchaeology and palaeopathology: to analyse the physical remains of the victims of the plague.
Archaeology, Climate and Vectors of Transmission
During the Black Death epidemic, Yersinia pestis is believed to have been carried primarily by rats and transmitted to humans by their fleas. As discussed above, some authors have argued against this vector of transmission, and archaeology could help researchers explore alternative hosts and vectors. Vertebrate zooarchaeology may allow us to identify the presence or availability of animal hosts, and (in the case of Yersinia pestis) the existence of any wild rodents that may act as a reservoir for the disease. The identification of rodent vectors may prove critical in the interpretation of such epidemics.17 The skeletal remains of many rodents can “easily” be identified through the study of their complex and characteristic dentitions.18 It has been argued that the rat played a key role in the appearance, spread and, in particular, the disappearance of plague in Europe. The black rat (Rattus rattus) is regarded by some as the dominant reservoir of Yersinia pestis and this species may have eventually been displaced and succeeded throughout Europe by the bigger brown rat (Rattus norvegicus). As the brown rat is believed to be less likely to transmit the fleas to humans, this might have resulted in the eventual disappearance of the disease. Changes in rodent ecology may thus explain the complex patterns of eruption, disappearance and re-emergence of plague that continued in Europe over many centuries.19 Archaeologically, it is possible to distinguish between Rattus rattus and Rattus norvegicus using differences in cranial morphology.20 Unfortunately, the patchy nature of the archaeological evidence and the contexts in which such remains may be preserved (i.e. plague pits, refuse pits and domestic habitations of the right period) make it unlikely that we will ever be able to determine any temporal and geographical changes in European rodent populations. With regards to ascertaining the origin of Rattus rattus, Anton Ervynck points out:
Generally, the dataset … is rather limited. This must be partly caused by unfavourable preservation conditions for small mammal bones at many archaeological sites, but is, without doubt, also linked to poor sampling and recovery methodology on previous excavations (i.e. lack of sieving).21
Similarly, the poor preservation of invertebrates, including fleas, limits the usefulness of invertebrate zooarchaeology in the study of ancient plague.22 Nonetheless, some invertebrates—and molluscs in particular—are well preserved, can be used to investigate past climates, and have been employed to reconstruct sea temperatures through the analysis of changes in the ratio of oxygen isotopes.23 As climatic and environmental conditions are likely to be key factors in determining the efficiency of disease vectors (such as the ability of fleas to reproduce and survive), it may be wise to invest greater efforts in determining the climatic conditions prevalent during the plague epidemics. Indeed, the year 1348 is believed to have been unusually warm and this may have had an impact on the virulence and spread of the Black Death.24 Palaeoclimatology employs a wide range of techniques to reconstruct past climates, including the analysis of ice cores (pollen and isotopic sampling), tree rings, lake and oceanic sediment layers (vegetation, insect, animal, pollen and isotopic sampling), molluscs (isotopic analysis) and historical documents. The climate between ad 1000 and the early 1900s appears to show periods—several decades in length—when the temperature seems to have been warmer or colder than the overall trend. Interestingly, mild episodes seem to have occurred in the early and late fourteenth century and cooler episodes in the fifteenth century and the late seventeenth century. Unfortunately, the record is poor in many areas before the seventeenth century and various uncertainties remain, including the precise nature of the climate in medieval times.25
Archaeology and the Epidemiological Environment
Archaeology may also play a part in establishing the “epidemiological environment” by providing researchers with an understanding of the urban environment and the social conditions prevalent at the time of a plague epidemic. This could help us determine whether past living conditions—including housing, population density, town size, water supply, transport infrastructure, food supply and general facilities—may have had an impact on the emergence and spread of a disease. Urban centres such as London have experienced periods of enormous change and growth over the past 1000 years. During the thirteenth century, the period immediately preceding the Black Death, multi-storey timber-framed buildings appeared in the streets of London in order to cope with the need for space.26 This must have led to overcrowding and increased demand on London’s infrastructures, such as water supply and the disposal of sewage, all of which are likely to have facilitated the spread of infectious disease. The London Bills of Mortality (seventeenth to nineteenth centuries) offer particular insights into diseases that cannot be detected in archaeological skeletons, such as cholera, smallpox, measles and plague.27 The nineteenth-century population increase, for example, was accompanied by several outbreaks of typhus and cholera.28 The creation of the London Granary in 1440 and changes in travel, trade and transport with the colonization of the New World (fifteenth-century onwards), the expansion of the British empire (mid-eighteenth century) and the development of the railways in the nineteenth century, may have improved food availability, but must have also introduced new pathogens and vectors of disease.29 One of the greatest improvements in health was the construction of London’s modern sewage system during the 1860s, which had a fundamental impact on diseases such as cholera. With regard to the Black Death, the urban environment and social conditions prevalent at the time of the epidemic may have played an important role in the biology of the disease. Has the epidemiological environment been established with sufficient detail? How would the living conditions in major urban centres, such as the use of multi-storey timber-framed buildings in London, have affected the ecology of humans, rodents and other potential vectors of the plague? Indeed, would the houses and storage rooms have been “suitable” to Rattus rattus and Rattus norvegicus, or sufficiently warm for Xenopsylla cheopis to reproduce or live during the winter months? Experimental archaeology, by reconstructing a fourteenth-century house, or ethnoarchaeological research, may help establish whether medieval houses and towns provided the “appropriate” epidemiological environment for Yersinia pestis.
Archaeology and the Burial Environment
Burial sites, such as plague pits, offer archaeologists the unique opportunity of studying the remains of people who died from the plague. As discussed above, one such plague pit was excavated by the Museum of London in 1986. The site contained two mass burial trenches, a mass burial pit and numerous individual graves. The interpretation of such archaeological sites, including the distribution of the skeletal remains, can be fraught with dangers. Indeed, when dealing with any archaeological site, it is important to appreciate the nature of the evidence, as non-randomness and systematic bias in an assemblage can lead to interpretation errors.30 An assemblage is the result of culture, preservation or a mixture of both. Many factors can have an impact on the number and/or distribution of skeletal remains. The study of the processes that cause sampling bias or differential preservation is known as taphonomy, and can be highly variable on a local scale.31 The acidity of the soil, for example, may differ across a site due to variations in underground water movements, damaging and destroying skeletons in specific areas, but not others. Out of the “total dead population”, only a proportion is likely to have been buried at one site. There is also a progressive loss of information during and after burial, with only a percentage of the original cemetery population ending up in front of the archaeologist. This is mostly due to decay and decomposition but is also affected by the amount of post-burial disturbance, and the extent of the excavation.32 Indeed, only a percentage of the remains will be preserved, of which only some will be discovered and recovered. Sites are often only partially excavated and material can be lost during the excavation process, resulting in an incomplete and therefore biased assemblage. At the Royal Mint for example, out of an estimated 2400 buried at the site, approximately 600 skeletons were recovered. This makes it difficult to interpret the significance of any organization within the Black Death site, such as any biological or burial-goods differences between the people buried in the individual graves, the mass burial trenches and the pit. This is especially relevant when comparing assemblages from different sites, particularly when the proportions of total buried population discovered or excavated are not the same.33 Differences in the number of dead individuals and in mortality profiles (age and sex distribution) may be used to assess the impact of plague on different populations, but any biases not associated with the presence of plague need to be taken into account.34
In order fully to interpret any archaeological site and, in the case of plague, determine whether it was used during an epidemic, it is important to establish the period during which the burial site was in use. As plague outbreaks tend to be catastrophic in nature, burial sites such as plague pits are used over a short period of time, as in the Royal Mint site, and determining when the site was in use may be beyond most archaeological scientific dating methods (such as radiocarbon dating). Changes in grave goods (material culture) can be used to provide a “relative” date. This approach was recently employed by researchers examining a pit containing approximately 150 skeletons believed to have died during the plague of Athens.35 The remains of approximately thirty small vases scattered among the bodies of the lower layers of the pit were recovered. Most of the vases were dated at around 430 bc, some within the decade of 420 bc, and a few from the last quarter of the fifth century bc. The authors suggest that the poor quality and quantity of the offerings, the hurried manner of burial, and the chronology of the burial offerings, link this site with the outbreak of the plague of Athens during the early part of the Peloponnesian War, between 430 and 426 bc.36 In this case, the knowledge of Greek pottery chronology is fairly well established and this method offers a good alternative to conventional dating. However, this relative level of accuracy is rare and may not be adequate. As in the case of the Royal Mint site, as discussed above, historical records are usually required to identify or confirm the site as a plague burial.
Archaeology and Skeletal Remains
Burial environment and embalming practices affect the overall preservation of human remains and the information that can be derived from these remains. In most archaeological sites, the skeleton is all that survives. Soft tissues are rarely preserved, especially in Europe.
Skeletal Analysis
In order to determine the mortality profile of an assemblage, archaeologists need to establish the age and sex of each skeleton. Sex determination based on skeletal features can be problematic in some adults, and is not possible in non-adult skeletons.37 The ageing of a non-adult skeleton is fairly accurate and is based on the development of bones and teeth. The ageing of an adult skeleton is usually based on the degenerative age-related changes that occur on parts of the skeleton where bones come into contact (i.e. joint surfaces). The most reliable areas are on the hip bone, and the changes are assigned scores. Scores are combined to provide an approximate age-at-death within a five or ten year range.38 However, the methods employed tend to overestimate young adults and underestimate older adults, thus providing flawed mortality profiles.39 Adults tend to be grouped into broad age categories (in years): 15–24, 25–34, 35–44, 45+, adults or unknown. The problems inherent in these methods have created different interpretations of the mortality profile of the Royal Mint assemblage:40 in particular, whether or not such a “catastrophic assemblage” reflects the once living population—this assumes that the disease responsible for the epidemic killed indiscriminately, irrespective of age or sex—and how the Royal Mint assemblage ought to differ from an “attritional assemblage” that accumulates over a long period (i.e. a cemetery that is used over several years, decades or centuries).
Regrettably, only a limited number of diseases affect the skeleton, and bone can only react in a limited number of ways. It can be removed, added, or a combination of both. To make matters more complex, a skeleton can be affected by more than one disease. All these factors make diagnosis difficult and, when possible, it is based on the location, distribution and nature of the changes. Unfortunately, plague (or any of the alternative candidates) does not appear to affect bone, and cannot be identified skeletally.41 Remains with preserved soft tissue (such as natural mummification) may help diagnosis but no such specimens appear to have been found.42 Instead, researchers have focused on trying to extract Yersinia pestis DNA from skeletal remains.
Biomolecular Analysis
Recent developments in biomolecular methods, such as polymerase chain reaction (PCR), have allowed researchers to amplify and analyse very small fragments of ancient DNA preserved within the bones and teeth of our ancestors. The publication of several “unrepeatable” high-profile studies and the technical difficulties of ancient DNA research (i.e. detecting small amounts of degraded DNA and the high risk of contamination) lead Alan Cooper and Hendrik Poinar to propose the following “criteria of authenticity”:43
Physically isolated work area: a laboratory in which the target DNA is not routinely amplified should be used to avoid contamination problems.
Control amplifications: several extraction and PCR controls should be carried out to detect sporadic or low-copy number contamination.
Appropriate molecular behaviour: the strength of PCR amplifications should be inversely related to product size and, when single-copy nuclear or pathogen DNA is detected, reproducible mitochondrial DNA results ought to be included.
Reproducibility: researchers ought to be able to repeat their results and include the use of different overlapping primer pairs to help detect numts (nuclear mitochondrial-like sequences or pseudogenes) or contamination by a PCR product.
Cloning: researchers should check the direct PCR sequences by cloning the amplified products.
Independent replication: separate samples (of the same specimen) should be extracted and sequenced by independent laboratories.
Biochemical preservation: researchers should assess the overall preservation of amino acids and other residues to provide indirect evidence of DNA survival.
Quantitation: in order to eliminate the risk of sporadic contamination, the copy number of the DNA target needs to be determined using competitive PCR.
Associated remains: when targeting human DNA, researchers should demonstrate that similar DNA targets have survived in any associated faunal remains.
Unfortunately, these guidelines add both time and expense to any ancient DNA project and are not always fully adhered to by researchers. The uncertainties surrounding some of the published studies, the high risk of contamination and the possibility of false positive results certainly warrant the use of independent replication. If the analysis of ancient DNA is going to help us identify the disease responsible for ancient “plagues”, researchers also need to agree on:
What constitutes a sufficient number of specimens/individuals/sites to ascertain whether a pathogen (identified by ancient DNA analysis) was responsible for a particular epidemic.
What constitutes adequate control samples to test for DNA contamination.
Whether soil bacteria are a source of false positive results.
If we should be collecting soil samples from the burial sites to include as control samples to test for false positive reactions.
Whether two independent laboratories should always be used to confirm the results.
Whether we should be using the same approach for all “plague” epidemics so that results may be comparable.
With regards to detecting “plague” DNA, these methods have provided mixed results. Molecular identification by “suicide PCR” of Yersinia pestis in the pulp tissue of teeth (one child, two adults) from a large fourteenth-century plague cemetery (approximately 800 skeletons) in Montpellier, southern France, tested positive.44 These results have generated a lot of controversy as DNA samples were not recovered and the results have never been duplicated by another laboratory.45 Thomas Gilbert and his co-researchers tried to confirm the French research and tested 108 teeth belonging to sixty-one individuals from different European plague burial sites (thirteenth to seventeenth century).46 They failed to amplify any Yersinia pestis DNA from the samples extracted and believe that the results proposed by Didier Raoult, Gérard Aboudharam and colleagues should be independently corroborated before confirming Yersinia pestis as the aetiological agent of the Black Death. This led to a response by Michel Drancourt and Raoult, and further comments by Gilbert and his co-researchers,47 but many now regard the research by Raoult, Aboudharam, et al. as unsatisfactory and the jury is still out. Using the same “suicide PCR” approach as Raoult, Aboudharam, et al., Ingrid Wiechmann and Gisela Grupe also claim to have identified Yersinia pestis-specific DNA sequences in two sixth-century skeletons from Upper Bavaria.48 Drancourt and Raoult have also published their own authentication criteria49 and have alleged that the Yersinia pestis Orientalis genotype was involved in all three pandemics.50 Recently, Drancourt, Linda Houhamdi and Raoult have proposed a new model to explain the persistence and periodic re-emergence of plague in Europe.51 In this yet unproven model, they suggest soil as the reservoir of Yersinia pestis, burrowing rodents as a first link, and human ectoparasites as the driving force behind the pandemics. No one has attempted to extract ancient Yersinia pestis DNA from the remains of possible hosts, such as rodents, but there is no reason why the DNA should not be present in the pulp chambers of plague-infected rat teeth. Testing the method on the teeth of modern rats infected with Yersinia pestis ought to be straightforward but finding archaeological specimens of the right period, or context, may be more difficult.
Recent work investigating the plague of Athens (430–426 BC) tested three human teeth from a mass burial pit containing at least 150 individuals.52 Interestingly, the results appear to incriminate typhoid fever as the probable cause of the epidemic. Six DNA amplifications targeted at genomic parts of the agents of plague (Yersinia pestis), typhus (Rickettsia prowazekii), anthrax (Bacillus anthracis), tuberculosis (Mycobacterium tuberculosis), cowpox (cowpox virus) and “cat-scratch” disease (Bartonella henselae) failed to yield any product in “suicide” reactions from DNA samples isolated from the three teeth. On the seventh such attempt, DNA sequences of Salmonella enterica serovar Typhi were identified. They argue that this provides clear evidence for the presence of that micro-organism in the dental pulp of the teeth recovered from the Kerameikos mass grave. These results are very interesting, but, as previously suggested, it would be useful if another laboratory repeated this work on a larger sample from a Greek site of the same period before typhoid fever is attributed as the sole “cause” of the plague of Athens, and thus eliminated the possibility of an isolated outbreak of typhoid fever.53 Manolis Papagrigorakis and his co-researchers admit they did not follow all of Cooper and Poinar’s recommendations (see criteria 7 and 8 above)54 and, using phylogenetic analysis, Beth Shapiro and her colleagues have also questioned whether the DNA sequence amplified was that of typhoid. They suggest the sequence may be that of a free-living soil bacterium and, as discussed above, recommend sampling the surrounding soil as a negative control.55 In their response, Papagrigorakis, et al. refute any environmental contamination, as they tested the soil washed off the ancient teeth, and argue that the phylogenetic analysis of a single gene may be insufficient and misleading. Nonetheless, they agree that there is, as yet, no definite proof that the plague of Athens was caused by typhoid fever.56
Conclusion: The Black Death and the Epidemiological Context
Over three decades before the Black Death epidemic, the Great Famine of 1315–17 had devastated northern Europe, causing great suffering and high mortality. This prolonged period of famine is regarded as one of the greatest calamities of the medieval period, but little is known about its impact on the people who survived it and how it altered the lives of Europe’s inhabitants. Can we look at the Black Death epidemic without considering the effect of the Great Famine on previous generations? Did years of famine and high mortality alter the genetic makeup of northern Europeans and affect their susceptibility to an epidemic disease? Could this explain why the Black Death appears to have had a different impact on northern Europe?
Between 1315 and 1317, a series of unusually cold winters and wet summers appears to have caused a succession of failed harvests across northern Europe.57 Records of wheat prices have been used to monitor the impact of the famine.58 In London, for example, the price of wheat achieved unparalleled heights in July 1315, rose to its highest level between April and July 1316 and peaked once more during May 1317.59 The moderately wealthy could not afford sufficient food and many people are believed to have died in the streets.60 This period is also likely to have had a profound effect on the health of people who survived the famine, particularly the children growing up at the time. Recent research is investigating the impact of the Great Famine on the skeletal and dental development of individuals who grew up during the famine years, using skeletons aged between thirty and forty years at death, from the Royal Mint site.61 The Black Death epidemic took place some thirty years after the Great Famine and any plague victim from the Royal Mint site that died in their thirties would have lived through the famine as a child. The results of this research should allow us to determine the impact of the Great Famine on the development of individuals who were children during the famine years and give us an insight into the overall health of Londoners in the fourteenth century.62
Many archaeological sub-disciplines have a role to play in the study of ancient plagues, particularly in the investigation of the transmission and epidemiological environment of diseases, and the burial and physical remains of the victims. Understanding how ancient calamities, such as plague and famine, may have affected continents like Europe, and how pathogens may have adapted to northern conditions and changed over the past 600 years, could become more relevant than ever, particularly with the emergence of antibiotic resistant strains of bubonic plague.63
Acknowledgments
I would like to thank the organizers for inviting me to speak at the conference and Prof. Charlotte Roberts for her useful comments. I wish to thank the Museum of London, and in particular Bill White of the Museum's Centre for Human Bioarchaeology, for arranging access to the Royal Mint skeletal assemblage. I would also like to thank the other participants in the Royal Mint research: Prof. Simon Hillson (Institute of Archaeology, UCL), Prof. Tony Waldron (Institute of Archaeology, UCL), Prof. Derek Keene (Institute of Historical Research, University of London), Gustav Milne (Institute of Archaeology, UCL) and Prof. Chris Dean (Department of Anatomy and Developmental Biology, UCL). Our research was supported by the Wellcome Trust (2002–2005) and is currently funded by the Leverhulme Trust (2006–2009).
Footnotes
1 Daniel Antoine and Simon Hillson, ‘Famine, Black Death and health in fourteenth-century London’, Archaeol. Int., 2004/2005, 8: 26–8.
2 Philip Ziegler, The Black Death, Harmondsworth, Penguin, 1970, pp. 123–4, 161; Duncan Hawkins, ‘The Black Death and the new London cemeteries of 1348’, Antiquity, 1990, 64 (244): 637–42.
3 Rosemary Horrox (trans. and ed.), The Black Death, Manchester University Press, 1994, pp. 64–5; see also Antoine and Hillson, op. cit., note 1 above, p. 26.
4 Antoine and Hillson, op. cit., note 1 above, pp. 26–8.
5 Ziegler, op. cit., note 2 above, p. 162; Hawkins, op. cit., note 2 above, pp. 637–8.
6 Antoine and Hillson, op. cit., note 1 above, p. 26.
7 Ziegler, op. cit., note 2 above, p. 162; Hawkins, op. cit., note 2 above, pp. 637–8; Antoine and Hillson, op. cit., note 1 above, pp. 26–8.
8 Antoine and Hillson, op. cit., note 1 above, p. 26.
9 Stephen Porter, ‘An historical whodunit’, Biologist, 2004, 51 (2): 109–13.
10 Graham Twigg, The Black Death: a biological reappraisal, London, Batsford, 1984; Susan Scott and Christopher Duncan, Biology of plagues: evidence from historical populations, Cambridge University Press, 2001; Susan Scott and Christopher Duncan, Return of the Black Death: the world’s greatest serial killer, Chichester, Wiley, 2004; Samuel K Cohn Jr, The Black Death transformed: disease and culture in early Renaissance Europe, London, Arnold, 2002.
11 Cohn, op. cit., note 10 above, pp. 26–8, 100–1, 111–13.
12 Porter, op. cit., note 9 above, pp. 109–13; see also Antoine and Hillson, op. cit., note 1 above, p. 26.
13 Gunnar Karlsson, ‘Plague without rats: the case of fifteenth-century Iceland’, J. Mediev. Hist., 1996, 22 (3): 263–84.
14 David Herlihy, The Black Death and the transformation of the west, ed. Samuel K Cohn, London, Harvard University Press, 1997, p. 26; Antoine and Hillson, op. cit., note 1 above, pp. 26–7.
15 Karlsson, op. cit., note 13 above, p. 265.
16 Scott and Duncan, Return of the Black Death, op. cit., note 10 above, p. 225.
17 Michael McCormick, ‘Rats, communications, and plague: toward an ecological history’, J. Interdiscip. Hist., 2003, 34: 1–25.
18 Simon Hillson, Teeth, Cambridge University Press, 2005.
19 Andrew B Appleby, ‘The disappearance of plague: a continuing puzzle’, Econ. Hist. Rev., 1980, 33 (2): 161–73; Paul Slack, ‘The disappearance of the plague: an alternative view’, Econ. Hist. Rev., 1981, 34 (3): 469–76.
20 H R Hunt, S Rosen, and C A Hoppert, ‘Morphology of molar teeth and occlusion in young rats’, J. Dent. Res., 1970, 49: 508–14; M J Lawrence and R W Brown, Mammals of Britain: their tracks, trails and signs, London, Blandford Press, 1973, pp. 194–9.
21 Anton Ervynck, ‘Sedentism or urbanism? On the origin of the commensal black rat (Rattus rattus)’, in Keith Dobney and Terry O’Connor (eds), Bones and the man: studies in honour of Don Brothwell, Oxford, Oxbow Books, 2002, pp. 95–109, on p. 95.
22 Several examples of fleas from the archaeological record are discussed in Paul C Buckland and Jon P Sadler, ‘A biogeography of the human flea, Pulex irritans L. (Siphonaptera: Pulicidae)’, Journal of Biogeography, 1989, 16 (2): 115–120.
23 Marcello A Mannino, Baruch F Spiro, and Kenneth D Thomas, ‘Sampling shells for seasonality: oxygen isotope analysis on shell carbonates of the inter-tidal gastropod Monodonta lineata (da Costa) from populations across its modern range and from a Mesolithic site in southern Britain’, J. Archaeol. Sci., 2003, 30(6): 667–79.
24 Charlotte Roberts and Margaret Cox, Health and disease in Britain: from prehistory to the present day, Stroud, Sutton Publishing, 2003, p. 227.
25 R S Bradley, K R Briffa, J E Cole, M K Hughes, and T J Osborn, ‘The climate of the last millennium’, in Keith D Alverson, Raymond S Bradley, and Thomas F Pedersen (eds), Paleoclimate, global change and the future, Berlin and New York, Springer, 2003, pp. 105–41.
26 John Schofield, Medieval London houses, New Haven and London, Yale University Press, 1995.
27 Roberts and Cox, op. cit., note 24 above, pp. 287, 290–3.
28 Ibid., pp. 337–8; Hugh Clout (ed.), The Times history of London, London, Times Books, HarperCollins, 2004, pp. 10–11, 88–89, 96–97.
29 M Samuel and Gustav Milne, ‘The “Ledene Hall” and medieval market’, in Gustav Milne (ed.), From Roman basilica to medieval market: archaeology in action in the City of London’, London, HMSO, 1992, pp. 39–50; Clout (ed.), op. cit., note 28 above, pp. 82, 88–91; Roberts and Cox, op. cit., note 24 above, pp. 368–9.
30 T Waldron, Counting the dead: the epidemiology of skeletal populations, Chichester, Wiley, 1994, pp. 10–27; see also T Waldron, Shadows in the soil: human bones and archaeology, Stroud, Tempus, 2001, pp. 44–48.
31 S P Nawrocki, ‘Taphonomic processes in historic cemeteries’, in Anne L Grauer (ed.), Bodies of evidence: reconstructing history through skeletal analysis, New York, Wiley-Liss, 1995, pp. 49–66.
32 Waldron, Shadows in the soil, op. cit., note 30 above, pp. 41–53.
33 Ibid.
34 Charlotte Roberts and Anne Grauer, ‘Commentary: Bones, bodies and representivity in the archaeological record’, Int. J. Epidemiol., 2001, 30 (1): 109–10.
35 Manolis J Papagrigorakis, Christos Yapijakis, Philippos N Synodinos, and Effie Baziotopoulou-Valavani, ‘DNA examination of ancient dental pulp incriminates typhoid fever as a probable cause of the plague of Athens’, Int. J. Infect. Dis., 2006, 10 (3): 206–14.
36 Ibid.
37 Roberts and Grauer, op. cit., note 34 above.
38 Jane E Buikstra and Douglas H Ubelaker, Standards for data collection from human skeletal remains, Arkansas Archeological Survey Research Series No. 44, Fayetteville, AR, Arkansas Archaeological Survey, 1994.
39 Theya Molleson and Margaret Cox, The Spitalfields project. Volume 2: the anthropology: the middling sort, Research Report 86, York, Council for British Archaeology, 1993, pp. 145–155, 167–179; Roberts and Grauer, op. cit., note 34 above.
40 H A Waldron, ‘Are plague pits of particular use to palaeoepidemiologists?’, Int. J. Epidemiol., 2001, 30 (1): 104–8; Beverley J Margerison and Christopher J Knüsel, ‘Paleodemographic comparison of a catastrophic and an attritional death assemblage’, Am. J. Physical Anthropol., 2002, 119 (2): 134–43.
41 Arthur C Aufderheide and Conrado Rodríguez-Martín, The Cambridge encyclopedia of human paleopathology, Cambridge University Press, 1998, pp. 195–198; Roberts and Grauer, op. cit., note 34 above.
42 Aufderheide and Rodríguez-Martín, op. cit., note 41 above, p. 198.
43 See publication for full guidelines: A Cooper and H N Poinar, ‘Ancient DNA: do it right or not at all’, Science, 2000, 289: 1139.
44 Didier Raoult, Gérard Aboudharam, Eric Crubézy, Georges Larrouy, Bertrand Ludes, and Michel Drancourt, ‘Molecular identification by “suicide PCR” of Yersinia pestis as the agent of medieval Black Death’, Proc. Natl. Acad. Sci. USA, 2000, 97: 12800–803.
45 James Wood and Sharon DeWitte-Aviña, ‘Was the Black Death yersinial plague?’, Lancet Infectious Diseases, 2003, 3 (6): 327–8; Michael B Prentice, Tom Gilbert and Alan Cooper, ‘Was the Black Death caused by Yersinia pestis?’, Lancet Infectious Diseases, 2004, 4 (2): 72.
46 M Thomas P Gilbert, Jon Cuccui, William White, Niels Lynnerup, Richard W Titball, Alan Cooper, and Michael B Prentice, ‘Absence of Yersinia pestis-specific DNA in human teeth from five European excavations of putative plague victims’, Microbiology, 2004, 150; 341–54.
47 Michel Drancourt and Didier Raoult, ‘Molecular detection of Yersinia pestis in dental pulp’, Microbiology, 2004, 150: 263–4; M Thomas P Gilbert, Jon Cuccui, William White, Niels Lynnerup, Richard W Titball, Alan Cooper and Michael B Prentice, ‘Response to Drancourt and Raoult’, Microbiology, 2004, 150: 264–5.
48 Ingrid Wiechmann and Gisela Grupe, ‘Detection of Yersinia pestis DNA in two early medieval skeletal finds from Aschheim (Upper Bavaria, 6th century A.D.)’, Am. J. Physical Anthropol., 2005, 126: 48–55.
49 Michel Drancourt and Didier Raoult, ‘Paleomicrobiology: current issues and perspectives’, Nat. Rev. Microbiol., 2005, 3: 23–35.
50 Michel Drancourt, Véronique Roux, La Vu Dang, Lam Tran-Hung, Dominique Castex, Viviane Chenal-Francisque, Hiroyaki Ogata, Pierre-Edouard Fournier, Eric Crubézy, Didier Raoult, ‘Genotyping, Orientalis-like Yersinia pestis, and plague pandemics’, Emerg. Infect. Dis., 2004, 10 (9): 1585–92; Michel Drancourt, Michel Signoli, La Vu Dang, Bruno Bizot, Véronique Roux, Stéfan Tzortzis, Didier Raoult, ‘Yersinia pestis Orientalis in remains of ancient plague patients’, Emerg. Infect. Dis., 2007, 13: Available from http://www.cdc.gov/EID/content/13/2/332.htm; see criticism by Gilles Vergnaud, ‘Yersinia pestis genotyping’ [letter], Emerg. Infect. Dis., Aug. 2005, 11 (8); available from http://www.cdc.gov/ncidod/EID/vol11no08/04-0942_05-0568.htm.
51 Michel Drancourt, Linda Houhamdi, and Didier Raoult, ‘Yersinia pestis as a telluric, human ectoparasite-borne organism’, Lancet Infectious Diseases, 2006, 6 (4): 234–41.
52 Papagrigorakis, et al., op. cit., note 35 above.
53 Daniel Antoine, comment on ‘Typhoid caused fall of Athens’, BBC News, 2006, http://news.bbc.co.uk/1/hi/health/4639840.stm.
54 Papagrigorakis, et al., op. cit., note 35 above, p. 212; Cooper and Poinar, op. cit., note 43 above.
55 Beth Shapiro, Andrew Rambaut and M Thomas P Gilbert, ‘No proof that typhoid caused the plague of Athens (a reply to Papagrigorakis et al.)’, Int. J. Infect. Dis., 2006, 10 (4): 334–5.
56 Manolis J Papagrigorakis, Christos Yapijakis, Philippos N Synodinos, and Effie Baziotopoulou-Valavani, ‘Insufficient phylogenetic analysis may not exclude candidacy of typhoid fever as a probable cause of the plague of Athens’, Int. J. Infect. Dis., 2006, 10 (4): 335–6; see also Michael P Cummings and Axel Meyer, ‘Magic bullets and golden rules: data sampling in molecular phylogenetics’, Zoology, 2005, 108 (4): 329–36.
57 Antoine and Hillson, op. cit., note 1 above, p. 27.
58 Derek Keene, personal communication; Bruce M S Campbell, James A Galloway, Derek Keene, and M Murphy, A medieval capital and its grain supply: agrarian production and distribution in the London region c. 1300, Historical Geography Research Series No. 30, London, Institute of British Geographers, 1993.
59 Antoine and Hillson, op. cit., note 1 above, p. 27.
60 William C Jordan, The great famine: northern Europe in the early fourteenth century, Princeton University Press, 1996.
61 Antoine and Hillson, op. cit note 1 above, p. 27.
62 Ibid., pp. 26–28; Daniel Antoine, Simon Hillson, Derek Keene, M Christopher Dean and Gustav Milne, forthcoming.
63 Timothy J Welch, W Florian Fricke, Patrick F McDermott, David G White, Marie-Laure Rosso, et al., ‘Multiple antimicrobial resistance in plague: an emerging public health risk’, PLoS ONE, 2007, 2 (3): e309.