Abstract
Objective
To determine the relations between hypertension and parental ratings of behavior and executive functions in children with primary hypertension and to examine the potential moderating influence of obesity.
Study Design
Hypertensive and normotensive control groups were matched for age, sex, race, intelligence quotient, maternal education, household income, and obesity. Parents completed the Child Behavior Checklist (CBCL) to assess Internalizing and Externalizing problems and the Behavior Rating Inventory of Executive Function (BRIEF) to assess behavioral correlates of executive function.
Results
Thirty-two hypertensive subjects and 32 normotensive controls (10 –18y) were enrolled. On the CBCL, hypertensives had higher Internalizing T-scores (53 vs. 44.5, p = 0.02) with 37% falling within the clinically significant range vs. 6% of controls (p = 0.005). Internalizing score increased with increasing BMI percentile in hypertensive, but not normotensive, subjects. Hypertensives had worse BRIEF Global Executive Composite (GEC) T-scores compared with controls (50 vs. 43, p = 0.009).
Conclusions
Children with both hypertension and obesity demonstrate higher rates of clinically significant internalizing problems, and hypertensives (irrespective of obesity) demonstrate lower parental ratings of executive function compared with normotensive controls.
Keywords: Neurocognitive function, anxiety, depression, blood pressure
Introduction
Investigators have long postulated that psychological factors may influence the development of sustained hypertension.1 The prevalence of hypertension is increased in adults with depression, anxiety, and panic disorder.2 Furthermore, recent studies indicate that baseline anxiety, depression, and hostility in normotensive adults are independent predictors of long-term incident hypertension.3–6
There is also evidence that hypertension may have a negative impact on neuropsychological processes.7 Studies demonstrate that young adults with mild to moderate hypertension have reduced performance on neuropsychological testing compared with normotensive controls, particularly within the domains of learning, memory, attention, abstract reasoning, and other executive functions.8–14 Furthermore, the deficits in cognitive function in young hypertensive adults have been shown to improve with effective antihypertensive therapy.15 Unlike studies in adults, data on the potential effects of hypertension on neuropsychological processes in children are limited.16
Children with primary hypertension are frequently overweight. Both adult and childhood obesity have been associated with an increased prevalence of internalizing problems, in particular depressive symptoms.17 In addition, recent studies suggest that obesity itself has potential negative effects on neurocognitive function in adults independent of the effect of blood pressure, although evidence for this association in children is less clear.18–20
To our knowledge, the relations between hypertension and both psychological and neurocognitive processes have not been evaluated in children with sustained primary hypertension. Accordingly, the objective of the current study was to examine these relations by comparing parental assessments of internalizing and externalizing behaviors and executive function in children with primary hypertension to that of normotensive controls. The potential moderating influence of obesity on these associations was also examined.
Methods
Participants
Newly diagnosed, untreated hypertensive children and adolescents, ages 10–18 years, were recruited from the Pediatric Hypertension Clinic at the University of Rochester Medical Center. All hypertensive subjects had a history of office systolic and/or diastolic blood pressure ≥ 95th percentile on at least 3 occasions.21 Sustained hypertension was confirmed by 24-hr ambulatory BP monitoring (ABPM), where hypertension was defined as mean daytime and/or nighttime BP ≥ 95th percentile for pediatric ambulatory norms.22 Children with both mean daytime and nighttime BP < 95th percentile were considered to have white coat hypertension and were excluded from the study. Because of the potential for confounding neuropsychological abnormalities, children with a known learning disorder (Section 504 plan or individual education plan), disorders of cognitive function, treatment with medications for attention deficit disorder, history of seizure disorder, history of severe head injury (loss of consciousness > 30 minutes), and those with a previous sleep study diagnosis of obstructive sleep apnea were excluded. Subjects with a history of chronic disease, previous treatment for elevated lead level, or evidence of secondary hypertension were also excluded.
Healthy normotensive control subjects were recruited from the Pediatric Primary Care Practice at the University of Rochester Medical Center and several private pediatric practices in the Rochester, NY area. Control subjects were required to have two casual BP readings < 90th percentile in the preceding 6 months.21 The same exclusion criteria were applied for control subjects as for hypertensive subjects. The control group was proportion matched (not individually matched) to the hypertensive group for mean age, sex, race (Black, Hispanic, White), obesity, mean estimated full-scale intelligence quotient (IQ), maternal education (< high school, high school, college, > college), and annual household income. Annual household income was defined categorically as low, low-middle, high-middle, and high (< $25,000, $25,000 – $55,000, $55,000 – 95,000, and > $95,000). Obesity was defined as BMI ≥ 95th percentile and morbid obesity as BMI ≥ 99th percentile. Normotensive control subjects did not have ABPM. Study visit BP index was defined as the visit BP divided by the 95th percentile BP for sex, age, and height. The study protocol was approved by the Research Subjects Review Board (RSRB) at the University of Rochester Medical Center.
Ambulatory Blood Pressure Monitoring (ABPM) and Echocardiography
ABPM was performed using Spacelabs monitors 90217 (Spacelabs Medical, Issaquah, WA). Monitors were programmed to obtain BP readings every 20 minutes from 8AM –10 PM and every 30 minutes from 10 PM – 8 AM. Wake and sleep periods for ABPM analyses were determined by the patient’s self report. Blood pressures were analyzed using Spacelabs software (ABP Report Management System, version 1.03.16). All hypertensive subjects also underwent a complete 2-dimensional echocardiogram with M-mode and Doppler study (Acuson Sequoia or Aspen, Siemens, Mountain View, CA).23 Left ventricular mass was indexed to height2.7 to correct for the effect of body size.24
IQ, and Behavior Measures
Prorated IQ was determined from the Block Design and Vocabulary subscales of the Wechsler Intelligence Scale for Children, Fourth Edition (ages 10 – 15 years) or the Wechsler Adult Intelligence Scale, Third Edition (ages ≥ 16 years).25 Parents completed the Achenbach Child Behavior Checklist (CBCL) and the Behavior Rating Inventory of Executive Function (BRIEF).26,27
The CBCL is a 118 item measure of internalizing and externalizing behaviors designed for the evaluation of children aged 6 – 18 years. Internalizing behaviors reflect mood disturbance, including anxiety, depression, and social withdrawal. Externalizing behaviors reflect conflict with others and violation of social norms. The CBCL provides syndrome scales, DSM-IV oriented scales, and three composite scales (Internalizing, Externalizing, and Total Problems) reported as both raw scores and sex and age normed T-scores. T-scores are standardized scores, derived from raw scores, that have a normal distribution with a mean of 50 and a standard deviation of 10, whose purpose is to facilitate comparisons of results across groups. Higher scores indicate greater degrees of behavioral and emotional problems. The lower limit T-score of the syndrome scales and DSM-IV oriented scales are truncated at 50; however, the composite scales are not truncated.26 Therefore, the current study analyzed raw scores for the syndrome scales and DSM-IV oriented scales and T-scores for the composite scales. As a result, the syndrome and DSM-oriented scale data are not sex and age normed. T-scores ≥ 64 on the Internalizing, Externalizing, or Total Problem scales are considered in the clinical range, indicative of deviant behavior in the range of children referred for professional mental health evaluation for behavioral or emotional problems.26
The BRIEF is an 86 item parent-report measure designed to assess executive functioning in 5 – 18 year old children.27,28 It reports 8 subscales which reflect different aspects of executive function. There are two composite scales - the Behavior Regulation Index (BRI) and the Metacognition Index (MI), and a summary score, the Global Executive Composite (GEC). Results are reported as gender and age-normed T-scores and higher scores indicate greater degrees of dysfunction. Scores ≥ 65 are considered to be potentially clinically significant.27,28
Statistical Analysis
The normotensive and hypertensive groups were compared using 2-sample t-tests for continuous variables and the Fisher’s exact test for categorical variables. For variables with distributions violating assumptions of normality, Wilcoxon rank sum tests were used. Results are reported as mean ± SD or median and interquartile range, where appropriate. Correlations were determined using Spearman’s rank correlation coefficients. Multiple linear regression was performed to investigate the potential interaction between hypertension and obesity on Internalizing scores and BRIEF GEC scores, with either Internalizing score or GEC score as the dependent variable and hypertension (Y/N), BMI percentile, and an interaction term for hypertension and BMI percentile as independent variables. The significance level of the data analysis was set at 0.05. Analyses were performed with SAS (version 9.1, SAS Institute Inc, Cary, NC).
Results
Participants
Thirty-two subjects with sustained hypertension and 32 normotensive control subjects were enrolled in the study. As expected by the matching criteria, the hypertensive group and control groups were similar in age, sex, race, percent obese, IQ, maternal education, and household income, but differed by study visit BP index (Table1; online). Because of a trend toward differences by gender, subsequent multivariate analyses controlled for gender. Nightly snoring, a surrogate for potential obstructive sleep apnea, was reported in 12.5% of control subjects and 9.4% of hypertensives (p = 0.99).
Table 1.
Demographic characteristics of normotensive and hypertensive groups.
| Characteristic | Normotensive N = 32 | Hypertensive N = 32 | P-value |
|---|---|---|---|
| Age (y)* | 15 (13 – 16) | 16 (14 – 17) | 0.18 |
| Sex (M/F) % | 53/47 | 78/22 | 0.064 |
| Race (Black/Hispanic/White) % | 28/0/72 | 31/3/66 | |
| Obesity % | 53 | 53 | 0.99 |
| Morbid obesity % | 19 | 37 | 0.16 |
| IQ | 100 ± 18 | 99 ± 14 | 0.79 |
| Maternal education (<HS/HS/college/>college) % | 6/56/25/13 | 9/47/34/10 | 0.81 |
| Household Income (low/low-mid/high-mid/high) % | 14/38/34/14 | 14/54/21/11 | 0.66 |
| Study visit SBP index^ | 0.85 ± 0.06 | 1.04 ± 0.09 | < 0.001 |
| Study visit DBP index^ | 0.74 ± 0.06 | 0.84 ± 0.13 | < 0.001 |
median (interquartile range);
mean ± SD
CBCL Results: Internalizing and Externalizing Behaviors
Hypertensive subjects had higher median T-scores for the Internalizing scale and a higher proportion of subjects with Internalizing T-scores in the clinical range compared with controls (Table 2). On analysis of subscales, the hypertensive group had higher raw scores on the Anxious/Depressed, Withdrawn/Depressed, Social Problems, Attention Problems, and Aggressive Behavior syndrome scales and the Anxiety Problems, Attention Deficit/Hyperactivity Problems, and Oppositional Defiant Problems DSM-oriented scales.
Table 2.
CBCL results: Emotion, Behavior, and Internalizing/Externalizing Symptoms *
| CBCL Scale | Normotensive N = 32 | Hypertensive N = 32 | P- value |
|---|---|---|---|
| Syndrome Scales (raw scores) | |||
| Anxious/Depressed | 0 (0–2) | 2.5 (1–7) | 0.002 |
| Withdrawn/Depressed | 0 (0–1) | 1.5 (0–4) | 0.038 |
| Somatic Complaints | 1 (0–2.5) | 2 (0–5) | 0.11 |
| Social Problems | 0 (0–1) | 1 (0–3.5) | 0.01 |
| Thought Problems | 1 (0–2) | 1 (0–2.5) | 0.47 |
| Attention Problems | 1 (0–2.5) | 2 (1–5) | 0.005 |
| Rule Breaking Behavior | 0.5 (0–2) | 1 (1–2.5) | 0.12 |
| Aggressive Behavior | 1 (0–3.5) | 3 (1–6.5) | 0.041 |
|
| |||
| DSM-Oriented Scales (raw scores) | |||
| Affective Problems | 1 (0–2) | 2 (0–4.5) | 0.082 |
| Anxiety Problems | 0 (0–1) | 1.5 (0–3) | 0.0014 |
| Somatic Problems | 1 (0–2) | 1 (0–3.5) | 0.14 |
| ADHD Problems | 1 (0–2) | 3 (1–5.5) | 0.005 |
| Oppositional Defiant | 1 (0–1) | 1.5 (1–3) | 0.025 |
| Conduct Problems | 0 (0–1.5) | 0.5 (0–2.5) | 0.22 |
|
| |||
| Internalizing | |||
| T-score | 44.5 (36.5–50) | 53 (42.5–65.5) | 0.022 |
| % in clinical range | 6 | 37 | 0.005 |
|
| |||
| Externalizing | |||
| T-score | 44 (34–50) | 48.5 (41.5–55) | 0.087 |
| % in clinical range | 6 | 3 | 0.99 |
Median (interquartile range); Syndrome scale and DSM-oriented scale results reported as raw scores; Internalizing and Externalizing results reported as T-scores.
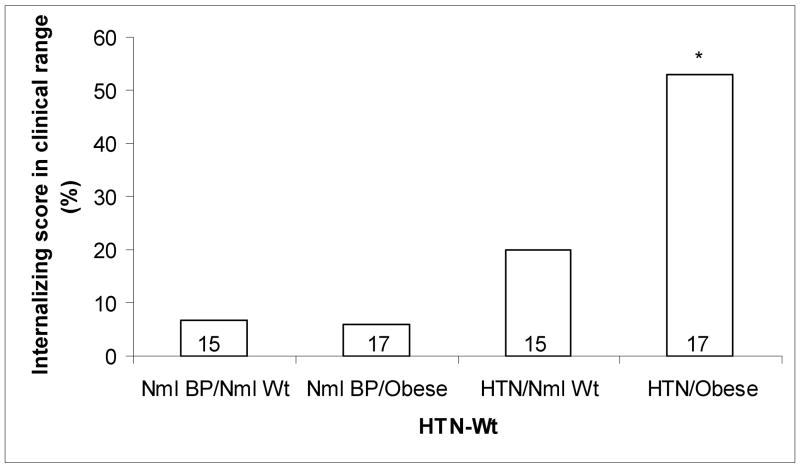
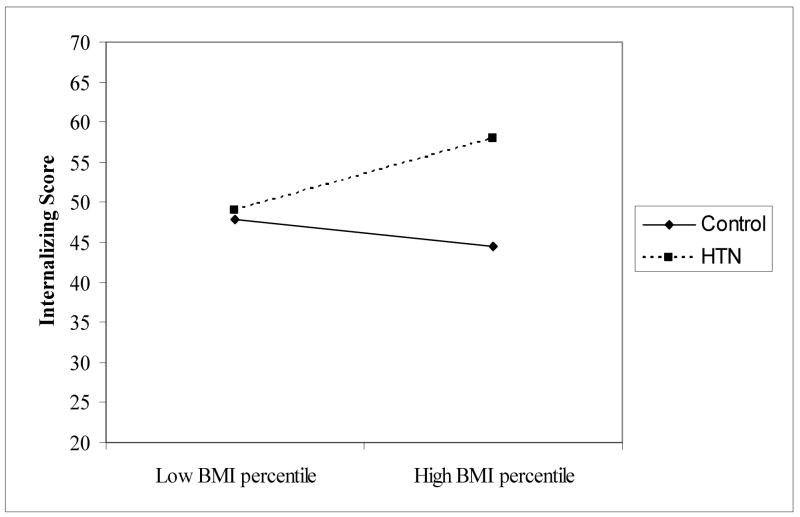
Figure 1 shows the proportion of subjects with Internalizing scores in the clinical range, with subjects stratified by both blood pressure (hypertensive vs. normotensive) and weight (obese vs. not obese). The increase in elevated Internalizing score was limited to the subjects who were both hypertensive and obese, with over 50% demonstrating scores in the clinical range (hypertensive/obese vs. normotensive/normal weight, 52.9 vs. 6.7%; p = 0.007). Subjects with obesity alone, without hypertension, did not differ from normal weight normotensive subjects in the proportion with Internalizing score in the clinical range (5.9 vs. 6.7 %, p = 0.99). Furthermore, none of the 6 subjects with morbid obesity in the normotensive control group had an Internalizing score in the clinical range, whereas 7 of 12 (58%) of subjects with morbid obesity in the hypertensive group had Internalizing scores in the clinical range (p = 0.038). Multiple linear regression was fit to further investigate the potential interaction between hypertension and obesity on Internalizing problems, including an interaction term for hypertension and BMI percentile in the model. The results of the regression analysis confirmed a significant interaction between hypertension and BMI percentile on Internalizing behaviors (interaction term, p = 0.04, Figure 2). For the hypertension group, with each one unit increase in BMI percentile, Internalizing scores increased by 0.26 units on average (95% CI = 0 – 0.52, p = 0.05). There was no significant association detected between Internalizing problems with BMI percentile in the normotensive control group. The results did not differ when gender was included as an independent variable in the regression model (data not shown).
Figure 1.
Comparison of percent with Internalizing score in the clinical range with subjects stratified by both hypertension and obesity. Value inside bars shows the number of subjects in each stratum. * P < 0.05 compared with Nml BP/Nml Wt group.
Figure 2.
The effect of hypertension on the relationship between BMI percentile and Internalizing score. Internalizing score and BMI percentile are both plotted as continuous variables.
BRIEF Results: Executive Function
The hypertensive group had higher median T-scores (poorer executive function) on the BRI, MI, and GEC composite scales compared with normotensive controls. On analysis of subscales, the hypertensive group had higher median T-scores on the Shift, Emotional Control, Initiate, Working Memory, Plan, and Monitor scales. The proportion of subjects with T-scores in the clinically significant range was not different for any BRIEF composite scale for hypertensive subjects compared with controls, with only 2 – 5 subjects in the clinical range for each scale (Table 3). There was no correlation between any of the BRIEF scales or the Internalizing CBCL scale and daytime SBP, sleep SBP, daytime DBP, sleep DBP, 24-hr SBP load, 24-hr DBP load on ABPM or LVMI on echocardiography (data not shown). Interaction analysis between hypertension and obesity was repeated on executive function (GEC scores). The regression analysis results did not show a significant interaction between hypertension and BMI percentile on GEC scores (interaction term, p = 0.29). The result did not differ after including gender as a covariate in the model.
Table 3.
BRIEF results: Executive Function *
| BRIEF Scale | Normotensives N= 32 | Hypertensives N = 32 | P- value |
|---|---|---|---|
| Inhibit | 42 (42–47.5) | 45 (42–54) | 0.17 |
| Shift | 41.5 (38–45) | 47 (40.5–59) | 0.01 |
| Emotional control | 41 (39.5–46.5) | 53 (41–60) | 0.001 |
| Initiate | 43 (38.5–50) | 51 (44.5–57.5) | 0.019 |
| Working memory | 42 (40–51.5) | 48.5 (43.5–59) | 0.029 |
| Plan/Organize | 44 (40.5–50) | 50 (47–57) | 0.021 |
| Organization of Materials | 46 (40–58.5) | 49 (43–57) | 0.63 |
| Monitor | 40 (38.5–50) | 51 (42.5–58) | 0.003 |
| BRI | 42.5 (39.5–44.5) | 51 (41.5–57.5 | 0.014 |
| % in clinical range | 3 | 8 | 0.43 |
| MI | 44 (39–51) | 51 (44–56.5) | 0.031 |
| % in clinical range | 5 | 6 | 0.99 |
| GEC | 43 (38.5–48) | 50 (42.5–57) | 0.009 |
| % in clinical range | 3 | 6 | 0.67 |
Median (interquartile range)
Due to the statistical trend of more males in the hypertensive group, regression analyses were done to evaluate differences between the hypertensive and control groups in behavior and executive function after controlling for sex, with Internalizing and GEC T-score as the dependent variables separately. Hypertension remained a significant predictor of both the Internalizing (p = 0.024) and GEC scores (p = 0.028), whereas sex was not a significant predictor of either Internalizing (p = 0.68) or GEC score (p = 0.37).
Discussion
In the current study, parental assessments of internalizing and externalizing behaviors and behaviors associated with executive functions of children with sustained primary hypertension were compared to assessments of normotensive controls proportionally matched to the hypertensive group for age, sex, race, IQ, maternal education, and household income. The groups were also matched for obesity, a factor that has been associated with anxiety and depression, and implicated in decreased performance on neurocognitive testing.17–20 Compared to normotensive controls, hypertensive subjects demonstrated more anxiety, depression, and social problems, as well as more problems with parent-rated attention on the CBCL. On further analysis, increased risk of elevated internalizing behavior was largely limited to subjects who were both obese and hypertensive, with half of obese hypertensive children demonstrating Internalizing scores in the clinical range, a score associated with referral for professional mental health services for behavioral or emotional problems. Multivariate regression analysis confirmed a significant interaction between obesity, hypertension, and internalizing behaviors, showing that higher BMI percentile was associated with higher Internalizing scores in subjects who were hypertensive, but not in normotensive subjects. Taken together, these findings suggest an interrelationship among obesity, hypertension, and anxiety/depression and demonstrate that potentially clinically significant anxiety and depression are not uncommon in children with obesity-associated hypertension. The mechanism linking negative affect (anxiety and depression) and hypertension is unclear. However, adults with anxiety have an increased prevalence of autonomic dysregulation (reduced heart rate variability) and increased sympathetic nervous system activity, factors that have been implicated in the pathogenesis of primary hypertension.29–31
Studies in adults with untreated, mild-to-moderate hypertension show that hypertensives have diminished performance on neurocognitive testing compared with normotensives, particularly in the domains of working memory, attention, abstract reasoning, and executive function.7–14 The disparity in performance on neurocognitive testing between hypertensives and normotensives is more pronounced in young adults compared with middle-aged adults,11,13 a finding with potential implications for hypertensive children and adolescents. The mechanism of hypertension associated reduced performance on neuropsychological testing remains unknown. Investigators have postulated that hypertension leads to small vessel remodeling which, in turn, results in decreased ability to enhance regional cerebral blood flow in response to increased neuronal activity.7 Similar to the findings in young adults, the current study also found that ratings of executive function impairment were elevated in hypertensives compared with controls. The greatest differences were noted in the Emotional Control and Monitor scales, where there was more than one standard deviation difference between groups. The Emotional Control scale evaluates the subject’s ability to modulate emotional responses and the Monitor scale evaluates the subjects self-monitoring during and soon after a task to assure goal attainment.27,28 The finding of more problems with parent-rated attention on the CBCL in the hypertension subjects is consistent with the higher scores on the BRIEF Working Memory scale, an expected correlation which has been attributed to the fact that working memory theoretically underlies attentional functioning.27 In contrast to results from the CBCL, hypertensives did not differ from normotensive controls in the proportion of subjects with scores in the clinically significant range for any BRIEF scale. Instead, the differences between groups occurred largely within the normal range. These results parallel findings in adults, where some neuropsychological measures differ by a full standard deviation between hypertensives and normotensive controls, but few hypertensives are classified as cognitively impaired. In a review of hypertension and cognition, Waldstein and colleagues conclude that, while young hypertensive adults are not clinically impaired, their deficits on neuropsychological testing may still be clinically significant, equivalent to the difference between an average and above average test score.11 The current study findings suggest that children and adolescents with primary hypertension may have a similar level and magnitude of deficits in some neuropsychological processes. The practical significance of these deficits is not known but one might speculate that the presence of such deficits would be problematic in the cognitively challenging environment of school, and especially as executive demands increase over successive school years. Future research using direct testing of executive function in hypertensive children, as well as longitudinal assessments, would help to confirm the presence of executive function deficits in hypertensive children and to clarify the significance of such deficits.
The current study has several limitations. Most importantly, the cross-sectional study design limits inference on the causal relationship between internalizing problems, hypertension, and deficits in executive function. A second limitation is that the measures of internalizing and externalizing problems and executive function were limited to parental assessments of behavior. While both the CBCL and the BRIEF evaluate problems by asking about child behaviors, factor analysis supports that the factors assessed by the Internalizing and Externalizing scales of the CBCL are distinct from factors assessed by the summary scales of the BRIEF.27,28 In addition, while standard direct tests of executive function are available for children, some investigators suggest that the BRIEF is a more sensitive assessment of executive deficits in daily life.28 Third, despite the matching criteria, there was a trend toward more males in the control group. This limitation should have been ameliorated by the use of sex-normed T-scores (with the exception of the syndrome and DSM-oriented CBCL scales, where raw scores were reported). In addition, regression analyses results showed that sex did not have a moderating effect on study group differences. Lastly, the normotensive subjects did not have ABPM to confirm normotension. Therefore, there may have been subjects in the normotensive control group who had masked hypertension or who were otherwise not truly normotensive. However, this limitation would have biased the results toward no difference in behavior scores between the hypertensive and normotensive subjects.
In summary, children with both obesity and hypertension appear at high risk for potentially clinically significant internalizing problems, and hypertensive children, regardless of obesity, have evidence of deficits in executive function. Behavioral screening should be conducted in this at-risk population to identify those children who may need professional mental health services.
Previous investigators have suggested that the neurocognitive deficits seen in hypertensives are an early manifestation of hypertensive target organ damage of the brain.7 If this were the case, then one might expect these deficits to be reversible with antihypertensive treatment. Studies to determine if the neuropsychological deficits in hypertensive children improve with antihypertensive therapy are warranted.
Acknowledgments
Marc B. Lande, MD was supported, in part, by NIH grant 5K23HL080068-04 from the National Heart, Lung, and Blood Institute. Heather Adams, PhD was supported, in part, by NIH grant 1K32 NS058756-01A1 from the National Institute of Neurological Disorders and Stroke.
We thank Laura Gebhardt for excellent study coordination.
References
- 1.Alexander F. Emotional factors in essential hypertension: presentation of a tentative hypothesis. Pyschosom Med. 1939;1:175–9. [Google Scholar]
- 2.Pickering TG. Mental stress as a causal factor in the development of hypertension and cardiovascular disease. Curr Hypertens Rep. 2001;3:249–54. doi: 10.1007/s11906-001-0047-1. [DOI] [PubMed] [Google Scholar]
- 3.Markovitz JH, Jonas BS, Davidson K. Psychologic factors as precursors to hypertension. Curr Hypertens Rep. 2001;3:25–32. doi: 10.1007/s11906-001-0074-y. [DOI] [PubMed] [Google Scholar]
- 4.Raikkonen K, Matthews KA, Kuller LH. Trajectory of psychological risk and incident hypertension in middle-aged women. Hypertension. 2001;38:798–802. [PubMed] [Google Scholar]
- 5.Yan LL, Liu K, Matthews KA, Daviglus ML, Ferguson TF, Kiefe CI. Psychosocial factors and risk of hypertension: the coronary artery risk development in young adults (CARDIA) study. JAMA. 2003;290:2138–48. doi: 10.1001/jama.290.16.2138. [DOI] [PubMed] [Google Scholar]
- 6.Jonas BS, Lando JF. Negative affect as a prospective risk for hypertension. Psychosom Med. 2000;62:188–96. doi: 10.1097/00006842-200003000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Jennings JR. Autoregulation of blood pressure and thought: preliminary results of an application of brain imaging to psychosomatic medicine. Psychosom Med. 2003;65:384–95. doi: 10.1097/01.psy.0000062531.75102.25. [DOI] [PubMed] [Google Scholar]
- 8.Shapiro AP, Miller RE, King E, Ginchereau EH. Fitzgibbon Behavioral consequences of mild hypertension. Hypertension. 1982;4:355–60. doi: 10.1161/01.hyp.4.3.355. [DOI] [PubMed] [Google Scholar]
- 9.Elias MF, Robbins MA, Schultz NR, Streeten DH, Elias PK. Clinical significance of cognitive performance by hypertensive patients. Hypertension. 1987;9:192–7. doi: 10.1161/01.hyp.9.2.192. [DOI] [PubMed] [Google Scholar]
- 10.Waldstein SR, Ryan CM, Manuck SB, Parkinson DK, Bromet EJ. Learning and memory function in men with untreated blood pressure elevation. Journal of Consulting & Clinical Psychology. 1991;59:513–7. doi: 10.1037//0022-006x.59.4.513. [DOI] [PubMed] [Google Scholar]
- 11.Waldstein SR, Snow J, Muldoon MF, Katzel LI. Neuropsychological consequences of cardiovascular disease. In: Tarter RE, Butters M, Beers SR, editors. Medical neuropsychology. 2. New York: Kluwer Academic/Plenum Publishers; 2001. pp. 51–83. [Google Scholar]
- 12.Waldstein SR, Manuck SB, Ryan CM, Muldoon MF. Neuropsychological correlates of hypertension: review and methodologic considerations. Psychol Bull. 1991;110:451–68. doi: 10.1037/0033-2909.110.3.451. [DOI] [PubMed] [Google Scholar]
- 13.Waldstein SR, Jennings JR, Ryan CM, Muldoon MF, Shapiro AP, Polefrone JM, Fazzari TV, Manuck SB. Hypertension and neuropsychological performances in men: interactive effects of age. Health Psychol. 1996;15:102–9. doi: 10.1037//0278-6133.15.2.102. [DOI] [PubMed] [Google Scholar]
- 14.Muldoon MF, Waldstein SR, Ryan CM, Jennings JR, Polefrone JM, Shapiro AP, Manuck SB. Effects of six anti-hypertensive medications on cognitive performance. J Hypertens. 2002;20:1643–52. doi: 10.1097/00004872-200208000-00028. [DOI] [PubMed] [Google Scholar]
- 15.Miller RE, Shapiro AP, King E, Ginchereau EH, Hosutt JA. Effect of antihypertensive treatment on the behavioral consequences of elevated blood pressure. Hypertension. 1984;6:202–8. [PubMed] [Google Scholar]
- 16.Lande MB, Kaczorowski JM, Auinger P, Schwartz GJ, Weitzman M. Elevated blood pressure and decreased cognitive function among school-aged children and adolescents in the United States. J Pediatr. 2003;143:720–4. doi: 10.1067/S0022-3476(03)00412-8. [DOI] [PubMed] [Google Scholar]
- 17.Daniels SR. The consequences of childhood overweight and obesity. Future Child. 2006;16:47–67. doi: 10.1353/foc.2006.0004. [DOI] [PubMed] [Google Scholar]
- 18.Waldstein SR, Katzel LI. Interactive relations of central versus total obesity and blood pressure to cognitive function. Int J Obes. 2006;30:201–7. doi: 10.1038/sj.ijo.0803114. [DOI] [PubMed] [Google Scholar]
- 19.Gunstad J, Paul RH, Cohen RA, Tate DF, Spitznagel MB, Gordon E. Elevated body mass index is associated with executive dysfunction in otherwise healthy adults. Compr Psychiatry. 2007;48:57–61. doi: 10.1016/j.comppsych.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 20.Holtkamp K, Konrad K, Muller B, Heussen N, Herpertz S, Herpertz-Dahlmann B, Hebebrand J. Overweight and obesity in children with attention-deficit/hyperactivity disorder. Int J Obes Metab Disord. 2004;28:685–9. doi: 10.1038/sj.ijo.0802623. [DOI] [PubMed] [Google Scholar]
- 21.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114:1–22. [PubMed] [Google Scholar]
- 22.Soergel M, Kirschstein M, Busch C, Danne T, Gellermann J, Holl R, Krull F, Reichert H, Reusz GS, Rascher W. Oscillometric twenty-four hour ambulatory blood pressure values in healthy children and adolescents: a multicenter trial including 1141 subjects. J Pediatr. 1997;130:178–184. doi: 10.1016/s0022-3476(97)70340-8. [DOI] [PubMed] [Google Scholar]
- 23.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography’s guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 24.de Simone G, Daniels SR, Devereux RB, Meyer RA, Roman MJ, de Divitiis O, et al. Left ventricular mass and body size in normotensive children and adults: assessment of allometric relations and impact of overweight. J Am Coll Cardiol. 1992;20:1251–1260. doi: 10.1016/0735-1097(92)90385-z. [DOI] [PubMed] [Google Scholar]
- 25.Wechsler D. WISC-IV administration manual. San Antonio, TX: The Psychological Corporation; 2003. [Google Scholar]
- 26.Achenbach TM, Rescorla LA. Manual of the ASEBA school-aged forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- 27.Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior Rating Inventory of Executive Function. Lutz, FL: Psychological Assessment Resources; 2000. [DOI] [PubMed] [Google Scholar]
- 28.Strauss E, Sherman EMS, Spreen O. A compendium of neuropsychological tests: administration, norms, and commentary. 3. New York: Oxford University Press; 2006. [Google Scholar]
- 29.Friedman BH. An autonomic flexibility-neurovisceral integration model of anxiety and cardiac vagal tone. Biol Psychol. 2007;74:185–99. doi: 10.1016/j.biopsycho.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 30.Singh JP, Larso MG, Tsuji H, Evans JC, O’Donnell CJ, Levy D. Reduced heart rate variability and new-onset hypertension: insights into pathogenesis of hypertension: the Framingham Heart Study. Hypertension. 1998;32:293–7. doi: 10.1161/01.hyp.32.2.293. [DOI] [PubMed] [Google Scholar]
- 31.Julius S. The association of tachycardia with obesity and elevated blood pressure. J Pediatr. 2002;140:643–5. doi: 10.1067/mpd.2002.125519. [DOI] [PubMed] [Google Scholar]