Abstract
Background: The rate of operative vaginal delivery has remained stable the last decade, however the rate of vacuum has increased against forceps application. Different maternal and neonatal outcomes have been proposed by many reports. The aim of the present study is to compare the short term maternal and neonatal outcomes between vacuum and forceps delivery.
Material and methods: We conducted a medical record review of live born singleton, vacuum and forceps-deliveries. Maternal and delivery characteristics were recorded. Maternal and neonatal outcomes were also assessed. Out of 7098 deliveries, 374 were instrument assisted, 324 were conducted by vacuum (86.7%) and 50 by forceps (13.3%).
Results: The incidence of 3rd degree lacerations and periurethral hematomas was similar between vacuum and forceps (3.4% vs. 2% and 0.3% vs 0% respectively), while perineal hematomas were more common in forceps compared with vacuum application (2% vs 0.3% respectively), albeit not significantly. The rate of neonates with Apgar scores ≤ at 1 min was significantly higher after forceps compared with vacuum delivery (18% vs 5.2% respectively, p = 0.0003). The same observation was made concerning the neonatal intensive care unit (NICU) admissions (38% vs 11% respectively, p = 0.0001). The rate of neonatal trauma and respiratory distress syndrome did not differ significantly between the two groups.
Conclusion: Results of the present study indicate that both modes of instrumental vaginal delivery are safe with respect to maternal morbidity and neonatal trauma. However, forceps application increases the risk of neonatal compromise consequently necessitating their admission in the NICU.
Keywords: instrumental delivery, forceps, vacuum, perinatal outcomes
Approximately 10% of all deliveries in the western world are accomplished by one of the two methods of operative vaginal birth, vacuum extraction or forceps1. Forceps extractions are preferred in the United States, Canada, South America and Eastern Europe while vacuum is the instrument of choice in Western Europe, Asia and Middle East2–5. During the last decade, the rate of operative vaginal delivery has remained stable, whereas the rate of vacuum has increased against forceps application6–9. Vacuum extraction has recently gained popularity because of the new designs of vacuum cups with reduced risk of injury to the fetus and increased instrumental success rate10–12.
Forceps and vacuum have been compared in many studies. Review of the literature suggests differential maternal and neonatal outcomes and complication rates between the two methods. Both are associated with increased risk of maternal and neonatal injury when compared to normal spontaneous vaginal deliveries13. Poor maternal and newborn outcome has also been reported after the sequential use of vacuum and forceps delivery for assisted vaginal delivery14. Furthermore, it has been repeatedly shown that maternal injury is less frequent and less extensive with the use of vacuum15–17. However, recent studies show that maternal soft tissue injury rates are similar in vacuum and forceps assisted deliveries18. Differential neonatal morbidity and complication rates have been suggested by many authors as well. Although many studies suggest higher rates of cephalhematomas, retinal hemorrhages and intracranial hemorrhages8,15,19,20, others point the risks of vacuum but consider it as a safe alternative to forceps18,21.
The aim of the present study was to assess the rate of maternal and neonatal morbidity following vacuum and forceps-assisted deliveries in singleton term pregnancies.
Material and Methods
Operative vaginal deliveries of singleton live infants at term were retrospectively studied from January 2000 to December 2006. Three hundred and seventy four out of 7098 (5.3%) deliveries performed during the study period met the inclusion criteria. Maternal and neonatal records of the 4th Department of Obstetrics and Gynecology and the 1st Department of Neonatology and Neonatal Intensive Care Unit (NICU), both of Aristotle University of Thessaloniki, Greece, were reviewed. All deliveries were performed by experienced obstetricians and by residents under the supervision of an attending consultant in obstetrics. Multiple pregnancies, stillbirths, infants with birth-weight less than 2500 g or more than 4000 g, fetal anomalies and noncephalic presentation were excluded from the study
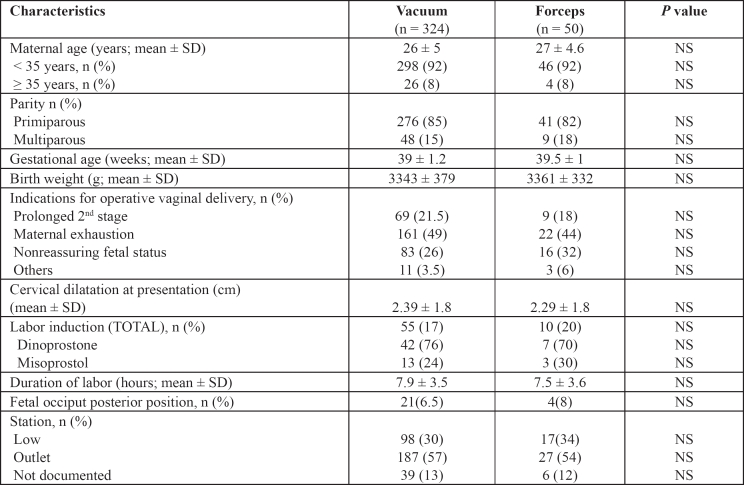
Maternal demographic data such as mean maternal age, parity, gestational age at delivery and delivery characteristics such as birth-weight, indications of operative vaginal delivery, cervical dilation at presentation, rate of labor induction, duration of labor, rate of fetal posterior occiput position and station at placement were recorded (Table 1). Prolonged second stage of labor (inadequate progress for three hours in nulliparous and two hours in multiparous women with documented uterine activity) and maternal exhaustion (maternal inability to deliver due to physical exhaustion) were considered as indications for operative vaginal delivery. Furthermore, non-reassuring fetal status such as tachycardia, bradycardia and late decelerations of fetal heart rate and other reasons such as previous cesarean section and maternal co-morbidity (cardiac or vascular diseases, myasthenia, myopia) were included in the indications for operative vaginal delivery.
Table 1. Maternal and delivery characteristics between vacuum and forceps deliveries.
SD: standard deviation, NS : non significant
Soft tissue damage, such as perineal hematomas, 2nd, 3rd degree perineal lacerations and periurethral injury were maternal outcomes of interest. Neonatal morbidity data recorded were low Apgar scores (≤ 4 and < 7, at 1 and 5 minute, respectively), neonatal trauma as well as NICU admissions and duration of NICU stay. Neonatal trauma included cephalhematomas, clavicle fractures, brachial plexus injury and development of respiratory distress. A qualified neonatologist attended all the above deliveries. Admission criteria to NICU were Apgar score ≤at 1 minute and the need for intubation in the delivery room as well as the presence of respiratory distress for more than 4 hours, while in the nursery.
Statistical analysis
The Statistical Package for Social Science version 14.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. Continuous outcomes were compared with the use of independent Student's t-test or Mann-Whitney non parametric test as required. Categorical variables were compared with the use of chi square test or Fisher's exact test, as appropriate. In addition, Odds ratio (OR) based on 95% confidence interval (CI) was also estimated. Differences between groups were considered statistically significant at p < 0.05. All p values were two-sided.
Results
The rate of operative vaginal delivery remained stable in the study period, while the ratio between forceps and vacuum delivery was 1/6. Out of 374 operative vaginal deliveries, 324 (86.7%) were vacuum and 50 (13.3%) forceps-assisted. There was no significant difference between vacuum-assisted and forceps-assisted deliveries as regards to maternal age (26 ± 5 years and 27 ± 4.6 years, respectively), gestational age at labour (39 ± 1.2 and 39 ± 1, respectively) and the rate of primiparous and multiparous women (Table 1). The indications for operative vaginal delivery was similar between the two study groups and maternal exhaustion was the most common indication for both ways of operative vaginal delivery.
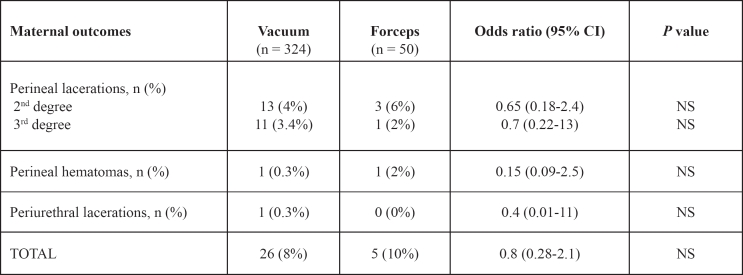
There was no significant difference in maternal morbidity between the two study groups (Table 2). Second and third degree perineal lacerations did not differ significantly between vacuum and forceps delivery. Perineal hematomas were more common in the forceps compared with vacuum group (2% vs. 0.3%, respectively) but did not reach significant difference (p: 0.20).
Table 2. Maternal outcomes between vacuum and forceps assisted vaginal delivery.
CI: confidence interval, NS: non significant
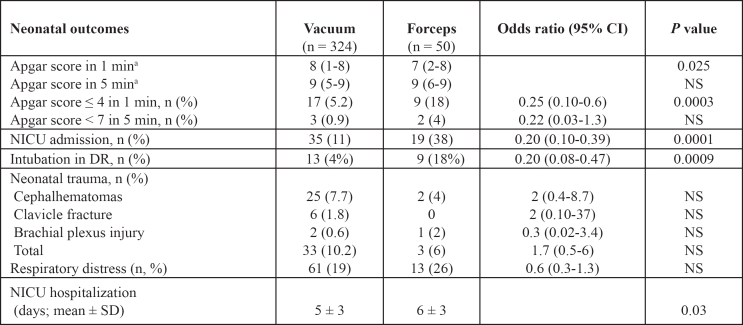
Mean birth weight was similar in vacuum and forceps group (3343g ± 379g vs. 3361g ± 332g, respectively, (p: 0.70). Median Apgar score at 1 minute was significantly lower after forceps delivery. Furthermore, significantly more neonates in this group had an Apgar score ≤ 4 at 1 min (p: 0.0003) (Table 3). The number of neonates needing resuscitation in labour ward and admission to the NICU was significantly higher among those delivered by forceps (p: 0.0001). However, the rate of respiratory distress between vacuum and forceps delivery (19% vs. 26% respectively) and the total incidence of neonatal trauma (10.2% vs. 6% respectively), as well as the incidence of cephalhematomas, clavicle fracture and brachial plexus injury did not differ significantly between the two methods. The duration of maternal or neonatal hospitalization was significantly higher after forceps application.
Discussion
This study was performed to estimate the short term maternal and neonatal morbidity in association with forceps or vacuum-assisted vaginal delivery. According to our results, there were no significant differences related to maternal morbidity and neonatal trauma. However, certain aspects of adverse neonatal outcomes, mainly low Apgar score and NICU admissions, were significantly more frequent in those born after forceps.
The goal of operative vaginal delivery is to assist the spontaneous vaginal birth providing minimum maternal and neonatal morbidity. High level of clinical and technical skills and therefore, adequate training is necessary for the use of both instruments3,19,21. Nevertheless, clinical fellows are exposed more commonly to the vacuum procedure, which seems that it is the instrumental delivery of choice in low and outlet station, while mid-pelvic and deep transverse arrest are mainly completed by cesarean section3,10,25,26. Low rate of forceps application results in less skillful trainees and less qualified instructors. Forceps training during residency is of critical significance for the obstetricians' further practice.
The rate of the instrumental delivery in our study was 5.3%, which was comparable to that found in previously published studies15,18,21. Several reports from Europe showed that the proportion of instrumental delivery is approximately 10%1,22, while in North America and Australia accounts for 7-16% of deliveries1,9,23. An explanation of the low rate of operative vaginal delivery in the present study, is the policy to complete the mid cavity delivery by cesarean section and our low experience with forceps application. The latter was also the reason for the low proportion of forceps against vacuum delivery, which is considered the instrumental application of first choice in our institution. The ratio of 1/6 between forceps and vacuum application in our study was also published previously18. In addition, other reports demonstrated increased rate of vacuum against forceps delivery, although the rate of operative vaginal birth has remained stable the last two decades6,9,23,24. Another possible explanation of the increased worldwide rate of vacuum against forceps is the less maternal injury and newborn's morbidity after the introduction of less traumatic soft vacuum extractor when compared to the rigid cups27. The former results are in accordance with findings derived from Cochrane data base review28. Maternal and neonatal outcomes related with the application of the different cups types was beyond the scopes of the present study.
Operative vaginal delivery is used to shorten the second stage of labor. It may be indicated for maternal exhaustion or fetal conditions including non reassuring fetal status to prevent hypoxic brain damage or fetal death29,30. Inadequate progress of labor (arrest of labor progress with documented uterine activity) represents another indication. Maternal exhaustion was the most common indication in our study and accounted for 49% in the vacuum and for 44% in the forceps group, that was similarly described by others10,15. Maternal conditions where down bearing effort is not encouraged, such as cardiac failure and cerebral aneurysms are also indications for instrumental delivery29. However, the decision to perform forceps or vacuum is not always straight forward. Absolute and relative contraindications for its use do exist. Malpresentation, incompletely dilated cervix, unengaged fetal head, cephalopelvic disproportion and fetal clotting disorder are some of the absolute contraindications29,31.
Several reports documented differential maternal and neonatal outcomes and complication rates between the two methods of instrumental delivery. Perineal damage, such as second and third degree lacerations has been shown to occur more often with the use of forceps in some studies8,10,15,16, whereas others, including the present study showed no difference between the two methods18,32. The rate of periurethral injuries and perineal hematomas that was shown from our data was also similar in both ways of operative vaginal delivery, although a trend of perineal hematomas was observed after forceps application. Johnson et al, showed insignificant difference of perineal hematoma between the two methods, while the periurethral injuries were more common after forceps delivery15. A possible explanation of the former discrepancy is the variety of the criteria, which have been used from the different studies for the instrumental application, especially in relation to the station at placement (mid, low and outlet).
Sequential use of vacuum and forceps vaginal delivery accounts for almost 0.5% of vaginal deliveries33. The percentage of failure after forceps application was reported approximately 7%, while it is almost double (12%) after vacuum-assisted vaginal delivery16. Failure of vacuum and the sequential use of forceps to complete deliveries, increase the risk of fetal and maternal morbidity4,14,16,33. Therefore, considering the increased rate of neonatal and maternal trauma, unsuccessful application of vacuum should not be encouraged by forceps procedure, except for the outlet pelvis and fetal head position.
Complication rates and neonatal morbidity differ substantially among published reports1,8,10,15,19. Nevertheless, despite the fact that some authors highlight the risk of vacuum, the latter procedure is generally considered as a safe alternative to forceps or with comparable outcomes concerning the neonatal morbidity18,21. In the present study, NICU admissions were significantly higher after forceps application. In a recent retrospective cohort study similar results were found8, whereas others documented no difference with respect to NICU admission between the two methods15. An important finding of the present study was the significantly higher median Apgar score at 1 min after vacuum extraction. Interestingly, Apgar score ≤ 4 at 1 min was more common after forceps delivery, while there was no difference of Apgar score ≤ 7 at 5 min. Additionally the duration of NICU hospitalization was significantly longer after forceps application, a finding not supported by others10,18. The influence of instrumental deliveries on Apgar score at 1 and 5 min is not clear. Bofill et al, showed no differences in the Apgar scores values at 1 and 5 min, independently of the instrument used10. Similar results have been shown by others15. However, other report after vacuum delivery showed Apgar score < 7 more common at 5 min8.
According to the results of this study, and in in accordance with other investigators18, the mode of instrumental delivery does not seem to have an important impact on the rate of cephalhematomas, clavicle fracture and brachial plexus injury. This is because of mainly outlet uses of instrumental delivery in cases of maternal fatigue or exhaustion and the recourse to cesarean section in case of mid cavity arrest. Significantly higher rates of cephalhematomas have been reported after vacuum application8,10,15, whereas Johnson et al15 found that the overall neonatal trauma as well as clavicle fracture and nerve injury did not differ between the two modes of assisted vaginal delivery.
The present data was not without deficiencies, such as the retrospective design and the small sample of patients especially in the forceps group. In addition, the long term maternal and neonatal outcomes were not in the objective of the present study.
In conclusion our data show that the application of both forceps and vacuum are safe alternatives to complete vaginal delivery in selected population of singleton live births at term, with a range of birth weight from 2500 to 4000 g and with cephalic presentation. Maternal short-term outcomes are comparable between both modes of delivery. This is also true concerning the neonatal trauma. However, from the present study it seems that neonates delivered by forceps are more likely to have a low Apgar score at 1 min subsequently needing admission to the NICU.
Table 3. Neonatal outcomes between vacuum and forceps assisted vaginal delivery.
aaNumerical data are expressed as median with range
CI: confidence interval, DR: delivery room, NICU: Neonatal Intensive Care Unit, NS: non significant
References
- 1.Wen SW, Liu S, Kramer MS, et al. Comparison of maternal and infant outcomes between vacuum extraction and forceps deliveries. Am J Epidemiol. 2001;153:103–107. doi: 10.1093/aje/153.2.103. [DOI] [PubMed] [Google Scholar]
- 2.Meniru GI. An analysis of recent trends in vacuum extraction and forceps delivery in the United Kingdom. Br J Obstet Gynaecol. 1996;103:168–170. doi: 10.1111/j.1471-0528.1996.tb09670.x. [DOI] [PubMed] [Google Scholar]
- 3.O'Grady JP, Pope CS, Hofffman DE. Forceps delivery. Best Pract Res Clin Obstet Gynaecol. 2002;16:1–16. doi: 10.1053/beog.2002.0251. [DOI] [PubMed] [Google Scholar]
- 4.Learman LA. Regional differences in operative obstetrics: a look to the South. Obstet Gynecol. 1998;92:514–159. doi: 10.1016/s0029-7844(98)00260-9. [DOI] [PubMed] [Google Scholar]
- 5.Hillier CE, Johanson RB. Worldwide survey of assisted vaginal delivery. Int J Gynaecol Obstet. 1994;47:109–114. doi: 10.1016/0020-7292(94)90349-2. [DOI] [PubMed] [Google Scholar]
- 6.Kozak LJ, Weeks JD. U.S. trends in obstetric procedures, 1990-2000. Birth. 2002;29:157–161. doi: 10.1046/j.1523-536x.2002.00182.x. [DOI] [PubMed] [Google Scholar]
- 7.Roberts CL, Algert CS, Carnegie M, Peat B. Operative delivery during labor: trends and predictive factors. Paediatr Perinat Epidemiol. 2002;16:115–123. doi: 10.1046/j.1365-3016.2002.00409.x. [DOI] [PubMed] [Google Scholar]
- 8.Caughey AB, Sandberg PL, Zlatnik MG, Thiet MP, Parer JT, Laros RK., Jr Forceps compared with vacuum: rates of neonatal and maternal morbidity. Obstet Gynecol. 2005;106:908–912. doi: 10.1097/01.AOG.0000182616.39503.b2. [DOI] [PubMed] [Google Scholar]
- 9.Clark SL, Belfort MA, Hankins GD, Meyers JA, Houser FM. Variation in the rates of operative delivery in the United States. Am J Obstet Gynecol. 2007;196:526.e1–e5. doi: 10.1016/j.ajog.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 10.Bofill JA, Rust OA, Schorr SJ, et al. A randomized prospective trial of obstetric forceps versus the M-cup extractor. Am J Obstet Gynecol. 1996;175:1325–1330. doi: 10.1016/s0002-9378(96)70049-2. [DOI] [PubMed] [Google Scholar]
- 11.Kuit JA, Eppinga HG, Wallenburg HC, Huikeshoven FJ. A randomized comparison of vacuum extraction delivery with a rigid and a pliable cup. Obstet Gynecol. 1993;82:280–284. [PubMed] [Google Scholar]
- 12.Chenoy R, Johanson R. A randomized prospective study comparing delivery with metal and silicone rubber vacuum extractor cups. Br J Obstet Gynaecol. 1992;99:360–363. doi: 10.1111/j.1471-0528.1992.tb13748.x. [DOI] [PubMed] [Google Scholar]
- 13.Yancey MK, Herpolsheimer A, Jordan GD, Benson WL, Brady K. Maternal and neonatal effects of outlet forceps delivery compared with spontaneous vaginal delivery in term pregnancies. Obstet Gynecol. 1991;78:646–650. [PubMed] [Google Scholar]
- 14.Gardella C, Taylor M, Benedetti T, Hitti J, Critchlow C. The effect of sequential use of vacuum and forceps for assisted vaginal delivery on neonatal and maternal outcomes. Am J Obstet Gynecol. 2001;185:896–902. doi: 10.1067/mob.2001.117309. [DOI] [PubMed] [Google Scholar]
- 15.Johnson JH, Figueroe R, Garry D, Elimian A, Maulic D. Immediate maternal and neonatal effects of forceps and vacuum-assisted deliveries. Obstet Gynecol. 2004;103:513–518. doi: 10.1097/01.AOG.0000114985.22844.6d. [DOI] [PubMed] [Google Scholar]
- 16.Vacca A. Vacuum-assisted delivery. Best Pract Res Clin Obstet Gynaecol. 2002;16:17–30. doi: 10.1053/beog.2001.0252. [DOI] [PubMed] [Google Scholar]
- 17.Chalmers JA, Chalmers I. The obstetric vacuum extractor is the instrument of first choice for operative vaginal delivery. Br J Obstet Gynaecol. 1989;96:505–506. doi: 10.1111/j.1471-0528.1989.tb03246.x. [DOI] [PubMed] [Google Scholar]
- 18.Lurie S, Glezerman M, Sadan O. Maternal and neonatal effects of forceps versus vacuum operative vaginal delivery. Int J Gynecol Obstet. 2005;89:293–294. doi: 10.1016/j.ijgo.2005.02.007. [DOI] [PubMed] [Google Scholar]
- 19.Murphy DJ, Liebling RE, Verity L, Swingler R, Patel R. Cohort study of the early maternal and neonatal morbidity associated with operative delivery in the second stage of labour. Lancet. 2001;358:1203–1207. doi: 10.1016/S0140-6736(01)06341-3. [DOI] [PubMed] [Google Scholar]
- 20.Robertson PA, Laros RKJr, Zhao RL. Neonatal and maternal outcome in low-mid-pelvic operative deliveries. Am J Obstet Gynecol. 1990;162:1436–1442. doi: 10.1016/0002-9378(90)90903-k. [DOI] [PubMed] [Google Scholar]
- 21.Demissie K, Rhoads GG, Smulian JC, et al. Operative vaginal delivery and neonatal and infant adverse outcomes: population based retrospective analysis. BMJ. 2004;329:24–29. doi: 10.1136/bmj.329.7456.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dupuis O, Silveira R, Redarce T, Dittmar A, Rudigoz RC. Instrumental extraction in 2002 in the "AURORE" hospital network: incidence and serious complications. Gynecol Obstet Fertil. 2003;31:920–926. doi: 10.1016/j.gyobfe.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 23.Hankins GD, Rowe TF. Operative vaginal delivery-year. Am J Obstet Gynecol. 1996;175:275–282. doi: 10.1016/s0002-9378(96)70135-7. [DOI] [PubMed] [Google Scholar]
- 24.Chang ALS, Noah MS, Laros RJr. Obstetric attending physician characteristics and their impact on vacuum and forceps delivery rates: University of California at San Francisco experience from 1977 to 1999. Am J Obstet Gynecol. 2002;186:1299–1303. doi: 10.1067/mob.2002.123735. [DOI] [PubMed] [Google Scholar]
- 25.Bofill JA, Rust OA, Perry KG, Roberts WE, Martin RW, Morrison JC. Operative vaginal delivery: a survey of fellows of ACOG. Obstet Gynecol. 1996;88:1007–1010. doi: 10.1016/s0029-7844(96)00328-6. [DOI] [PubMed] [Google Scholar]
- 26.Bonar KD, Kaunitz AM, Sanchez-Ramos L. The effect of obstetrics resident gender on forceps delivery rate. Am J Obstet Gynecol. 2000;182:1050–1051. doi: 10.1067/mob.2000.105392. [DOI] [PubMed] [Google Scholar]
- 27.Kuit JA, Eppinga HG, Wallenberg HCS, Huikeshoven FJM. A randomized comparison of vacuum extraction delivery with a rigid and a pliable cup. Obstet Gynecol. 1993;82:280–284. [PubMed] [Google Scholar]
- 28.Johanson R, Menon V. Soft versus rigid vacuum extractor cups for assisted vaginal delivery (Cochrane Review) In the Cochrane Library. 2001. Oxford: Update Software. [DOI] [PubMed]
- 29.Edozien LC. Towards safe practice in instrumental vaginal delivery. Best Pract Res Clin Obstet Gynaecol. 2007;21:639–655. doi: 10.1016/j.bpobgyn.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 30.Cunningham FG, Gant NF, Leveno KJ, Gilstrap LC, Hauth JC, Wenstrom KD. Forceps delivery and vacuum extraction. 21st ed. MacGraw-Hill USA: Williams Obstetrics; 2001. pp. 485–508. [Google Scholar]
- 31.SOGC Clinical Practice Guidelines. Guidelines for operative vaginal birth. Int J Gynecol Obstet. 2005;88:229–236. doi: 10.1016/j.ijgo.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 32.Fitzpatrick M, Behan M, O'Connell PR, O'Herlihy C. Randomized clinical trial to assess anal sphincter function following forceps or vacuum assisted vaginal delivery. BJOG. 2003;110:424–429. [PubMed] [Google Scholar]
- 33.Towner D, Castro MA, Wilkens EE, Gilbert WM. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med. 1999;341:1709–1714. doi: 10.1056/NEJM199912023412301. [DOI] [PubMed] [Google Scholar]