Abstract
An 80 years old male patient was admitted in our hospital with massive haematomas in the left forearm, chest and abdominal wall accompanied by intense back pain symptoms. Laboratory evaluation showed anemia, mild thrombocytopenia and elevated lactate dehydrogenase and alkaline phosphatase levels and normal concentrations of all the other biochemical parameters. Study of the coagulation status demonstrated prolonged thrombin time (TT), low fibrinogen levels – 0.98 g/l while plasminogen, antihrombin III (AT III) and protein C levels were found to be within normal range. Computed tomography scans of the head, chest and abdomen showed an enlarged infiltrative prostate, osteolytic bone lesions in vertebras L5-S1 and a large haematoma of the abdominal wall as the only pathologic findings. Very high levels of the prostate specific antigen indicated the possible existence of a prostate carcinoma with metastases to the vertebral column that resulted in elevated alkaline phosphate and lactate dehydrogenase levels. There were no signs of liver involvement and impaired hepatic synthetic function. Based on the results of the laboratory tests we concluded that the cause of the bleeding disorder in our patient was an acquired hypofibrinogenemia, which is a very rare paraneoplastic phenomenon. The patient was treated with daily transfusions of cryoprecipitate with no long-term improvement. Then the specific anti-tumor therapy (ciproteron acetate) was initiated, and two weeks later, fibrinogen concentration and TT returned to normal values.
Keywords: bleeding disorder, cancer, fibrinogen
Fibrinogen is a 340-kd glycoprotein, synthesized in the liver. Fibrin is the end point of the coagulation cascade, which results in the conversion of fibrinogen to fibrin monomer and factor XIIIa mediated fibrin crosslinking of the fibrin polymer1. Fibrinogen levels of more than 1.00 g/l are considered adequate for hemostasis. Levels below 1.00 g/l are frequently associated with severe bleeding complications2. Plasma fibrinogen levels are genetically determined. The thrombin time (TT) is the primary screening test for both acquired and inherited hypo- / dysfibrinogenemia3. More frequently, hypofibrinogenemia occurs as an acquired condition associated with acute and chronic liver diseases4, but in rare cases can be congenital. Since the first case report in 1935, only 40 cases of congenital hypofibrinogenemia have been reported and they are clinically manifested in early childhood5,6. In cancer patients hypofibrinogenemia usually coexists with other coagulation abnormalities – thrombocytopaenia, elevated D-dimer and fibrinogen degradation products (FDP) that characterize disseminated intravascular coagulation (DIC)7. The present paper reports a rare case of isolated hypofibrinogenemia as acquired hypocoagulable state in a patient with prostate carcinoma (CaP).
Case report
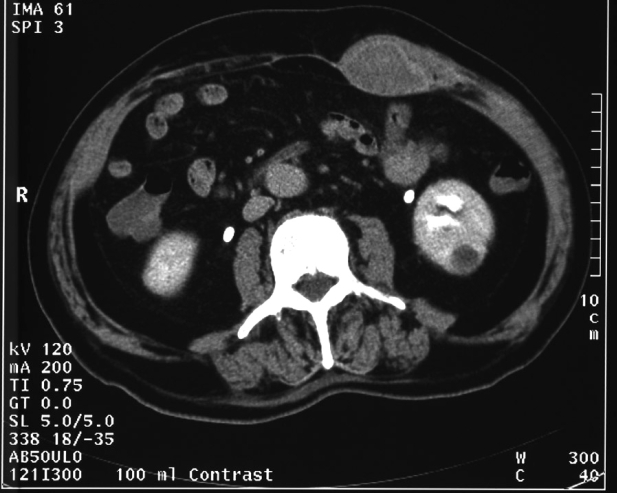
An 80 years old male patient was admitted to our hospital because of signs of massive haematomas in the left forearm, chest and abdominal wall and symptoms of intense back pain. His medical history revealed that a diagnosis of indolent gastric non-Hodgkin's lymphoma - MALT type (Helicobacter pylori negative) was established six years before his admission. After a chemotherapeutic regimen containing cyclophospamide, vincristine and prednisolone, a complete remission was achieved. This was confirmed by the treating hematologist after endoscopic examination, two months before this present admission. History of back pain lasting for one month was mentioned, and the patient denied consumption of any analgesic drugs or antibiotics. Two weeks before his admission to the hospital, the first ecchymoses appeared spontaneously on the left forearm. General assessment of his clinical condition of the patient was rather satisfactory, whit the exception of the existence of haematomas and pallor. Immediate laboratory evaluation was performed showing anemia and mild thrombocytopenia (Hb 77g/l, Hct 0, 28, MCV 89 fl, WBC 5x103/μl, Neutr 71%, Plt 103x103/μl) and elevated levels of lactate dehydrogenase (LDH) (1551 IU/l) and alkaline phosphatase (AP) (1016 IU/l) with normal concentrations of all the other biochemical parameters including total proteins (67 g/l), albumin (42 g/l), alanin and aspartate aminotransferases, gamma glutamil transpeptidase and total bilirubin. In the coagulation screening test, TT was prolonged (31.9 sec.), with normal prothrombin time PT (INR) and activated partial thromboplastin time (aPTT). D-dimer was slightly positive, fibrinogen was low (0.98 g/l), but FDP was negative as well as Lupus anticoagulant. The levels of all the other coagulation factors (i.e. Factors II, V, VII, VIII and IX), plasminogen, AT III and protein C were within normal range. Computed tomography (CT) scans of the head, chest and abdomen showed an enlarged infiltrative prostate, osteolytic bone lesions in vertebras L5-S1 and a large haematoma in the abdominal wall as the only pathologic findings (Figure 1).
Figure 1: Abdominal computed tomography demonstrating massive haematoma in the abdominal wall.
Prostate specific antigen level (PSA) was very high (218 ng/ml) with low Free/total PSA index (0.11) indicating that the patient had a prostate carcinoma with bone metastases that resulted in elevated AP and LDH. There were no signs of liver involvement and impaired hepatic synthetic function. The patient was treated with daily transfusions of cryoprecipitate with no long-term improvement. The high risk of life-threatening bleeding complication prevented prostate biopsy, and specific anti-tumor therapy was empirically initiated (ciproteron acetate). Two weeks after the initiation of anti-tumor treatment, fibrinogen concentration (2.93 G/L) and TT returned to normal levels and infusion of cryoprecipitate was discontinued. It could be stated that the rapid treatment response seen in our patient confirmed our preliminary clinical diagnosis of a prostate cancer. Then, transrectal ultrasonography with prostate biopsy was performed and histological findings further confirmed the diagnosis (Adenocarcinoma prostate – G III, Gleason score 4+3). Subsequently a more aggressive urological treatment approach was possible. CT scans of the abdomen done after three and six months of anti-tumor treatment showed complete resolution of the haematoma of the abdominal wall (Figure 2).
Figure 2: CT scan of the abdomen performed six months later showed complete resolution of haematoma.
Discussion
Various types of thrombotic or hemorrhagic events may be seen in patients with hematological and solid tumors. The most frequent are disseminated intravascular coagulation, antiphospholipid syndrome, impaired fibrinolysis, presence of acquired inhibitors of clotting factors and decreased biosynthesis of the vitamin K dependent blood clotting proteins. These bleeding and thrombotic disorders were described several decades ago8,9.
Hypofibrinogenemia is caused either by impaired synthesis due to liver involvement or coexisting chronic hepatic disease2 or increased fibrinogen consumption - mostly as one of the signs of chronic or acute DIC7,10,11. Recently, hypofibrinogenemia was described in hemophagohistiocytosis (HLH), a rare disorder with familiar and acquired forms which can be associated with infection, malignancy and autoimmunity12. Isolated hypofibrinogenemia can be induced with antineoplastic treatment and is described with regimens containing L- asparginase13, etoposide14 or prednisolone15. Cytotoxic agent-induced hypofibrinogenemia always occurs during the treatment and resolves after discontinuing the drugs. The exact mechanism remains unclear and a possible explanation is reduced synthesis of proteins including clotting factors and inhibitors – fibrinogen among them. That is why cytotoxic agent-induced hypofibrinogenemia next to increased bleeding can be associated with thrombosis as the result of reduction of AT III and protein C levels13. Our patient was treated with cytotoxic agents six years before admission which excludes the possible role of cytotoxic drugs as the cause of hypofibrinogenemia. In patients with solid tumors, increased consumption of fibrinogen is seen in DIC and during the activation of fibrinolysis, secondary to increase release of plasminogen activator16. However, there were no clinical or laboratory findings of DIC or impaired fibrinolysis in our patient. Also, there were no signs of involvement of liver or impaired liver synthetic function. A treatment of choice in hypofibrinogenemia is cryoprecipitate which contains factor VIII, von Willebrand factor (vWF), fibrinogen, factor XIII and (a few cryoprecipitable proteins, including) fibronectin2. This cryoprecipitate treatment improves bleeding symptoms. In our patient, the infusions of cryoprecipitate alone were ineffective until the initiation of specific antitumor therapy. After discontinuing cryoprecipitate, the levels of fibrinogen remained stable with subsequent complete regression of the signs of bleeding. We see this as a clinical proof to our statement that, in our patient, isolated hypofibrinogenemia was a paraneoplastic phenomenon and could not be explained either by impaired fibrinogen synthesis or increased consumption.
References
- 1.Brennan S, Felowes A, Faed J, George P. Hypofibrinogenemia in an individual with 2 coding (γ82A→G and Bβ235P→ L) and 2 noncoding mutations. Blood. 2000;95:1709–1713. [PubMed] [Google Scholar]
- 2.Pantanowitz L, Kruskall M, Uhl L. Cryoprecipitate. Am J Clin Pathol. 2003;119:874–881. doi: 10.1309/56MQ-VQAQ-G8YU-90X9. [DOI] [PubMed] [Google Scholar]
- 3.Hirota-Kawadobora M, Ishikawa S, Fujihara N, et al. Analysis of hypofibrinogenemias found on routine coagulation tests and identification of heterozygous dysfibrinogenemia or fibrinogen deficiency. Rinsho Byori. 2007;55:989–995. [PubMed] [Google Scholar]
- 4.Blonsky W, Siropaides T, Reddy KR. Coagulopathy in liver disease. Curr Treat Options Gastroenterol. 2007;10:464–473. doi: 10.1007/s11938-007-0046-7. [DOI] [PubMed] [Google Scholar]
- 5.Datta S, Bagchi S. Acute osteomyelitis in congenital hypofibrinogenemia. Clinical Brief. 2006;73:529–530. doi: 10.1007/BF02759901. [DOI] [PubMed] [Google Scholar]
- 6.Vu D, Neerman-Arbez M. Molecular mechanisms accounting for fibrinogen deficiency. J Thromb Haemost. 2007;5(Suppl 1):125–131. doi: 10.1111/j.1538-7836.2007.02465.x. [DOI] [PubMed] [Google Scholar]
- 7.Sallah S, Wan HY, Hguyen NP, Hanrahan LR, Sigounas G. Disseminated intravascular coagulation in solid tumors: Clinical and pathologic study. Thromob haemost. 2001;86:828–833. [PubMed] [Google Scholar]
- 8.Rosenthal M, Niemetz J, Wisch N. Hemorrhage and thromboses associated with neoplastic disorders. H Chron Dis. 1963;16:667–675. doi: 10.1016/0021-9681(63)90004-3. [DOI] [PubMed] [Google Scholar]
- 9.Sack GH, Levin J, Bell WR. Trousseau's syndrome and other manifestations of chronic disseminated coagulopathy in patients with neoplasm: clinical, pathophysiologic and therapeutic features. Medicine. 1977;56:1–37. [PubMed] [Google Scholar]
- 10.Pasquini E, Gianni L, Aitini E, et al. Acute disseminated intravascular coagulation syndrome in cancer patients. Oncology. 1995;52:505–508. doi: 10.1159/000227520. [DOI] [PubMed] [Google Scholar]
- 11.Weltermnann A, Pabinger I, Geissler K, et al. Hypofibrinogenemia in non-M3 acute myeloid leukemia. Incidence, clinical and laboratory characteristic and prognosis. Leukemia. 1998;12:1182–1186. doi: 10.1038/sj.leu.2401101. [DOI] [PubMed] [Google Scholar]
- 12.Jordan M, Hildeman D, Kappler J, Marrack P. An animal model of hemophagoytic lymphohistiocytosis (HLH) CD8+T cells and interferon gamma are essential for this disorder. Blood. 2004;104:735–743. doi: 10.1182/blood-2003-10-3413. [DOI] [PubMed] [Google Scholar]
- 13.Beinart G, Damon L. Thrombosis associated with l-asparginase therapy and low fibrinogen levels in adult acute lymphoblastic leukemia. Am J Hematol. 2004;77:331–335. doi: 10.1002/ajh.20230. [DOI] [PubMed] [Google Scholar]
- 14.Miura T, Nakamura M, Tsunematsu Y, Fujimoto J, Maguro T, Yamada K. Hypofibrinogenemia in a girl with Langerhans cell histiocytosis treated with etoposide and prednisolone therapy. Acta Pediatr Jpn. 1993;35:148–150. doi: 10.1111/j.1442-200x.1993.tb03027.x. [DOI] [PubMed] [Google Scholar]
- 15.Yokose N, Ogata K, Nakamura K, et al. Hypofibrinogenemia induced by prednisolone therapy in a patient with chronic lymphocytic leukemia complicated with autoimmune hemolytic anemia. Am J Hematol. 1997;55:166–167. doi: 10.1002/(sici)1096-8652(199707)55:3<166::aid-ajh11>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 16.Al-Mondhiry H, Drago J, Bartholomew MJ. The fibrinolytic system in experimental prostate tumor. Thromb haemost. 1986;56:133–136. [PubMed] [Google Scholar]