Abstract
There is an enormous amount of literature on psychological stress and cardiovascular disease. This report reviews conceptual issues in defining stress and then explores the ramifications of stress in terms of the effects of acute versus long-term stressors on cardiac functioning. Examples of acute stressor studies are discussed in terms of disasters (earthquakes) and in the context of experimental stress physiology studies, which offer a more detailed perspective on underlying physiology. Studies of chronic stressors are discussed in terms of job stress, marital unhappiness, and burden of caregiving. From all of these studies there are extensive data concerning stressors’ contributions to diverse pathophysiological changes including sudden death, myocardial infarction, myocardial ischemia, and wall motion abnormalities, as well as to alterations in cardiac regulation as indexed by changes in sympathetic nervous system activity and hemostasis. Although stressors trigger events, it is less clear that stress “causes” the events. There is nonetheless overwhelming evidence both for the deleterious effects of stress on the heart and for the fact that vulnerability and resilience factors play a role in amplifying or dampening those effects. Numerous approaches are available for stress management that can decrease patients’ suffering and enhance their quality of life.
Throughout medicine, “stress” is one of the most common patient complaints. In cardiology, complaints of stress take on special prominence because the links between brain and heart are so obvious. “Obvious” they may be, but are they clinically important? This report reviews the literature on this vast topic. Because the review is so broad in scope and touches on blood pressure (BP), hemodynamic functioning, arrhythmias, and angina, the review is qualitative, written from the vantage point of 30 years of work in the field.
Scope of the Review
One senses the vastness of this area because a day does not go by without patients or their families asking about stress and heart disease. Newspapers of greater or lesser repute commonly opine on the matter. A search on PubMed reveals approximately 40,000 citations. (Because of page limitations, it is impossible to cite this enormous literature. The author apologizes to colleagues whose valuable work, while uncited in this review, has nonetheless shaped his thinking and had an enormous effect on the field.) When one starts to page through these citations, however, one immediately sees that part of the problem is that the term “stress” is used in so many vastly different ways. “Stress” is like Proteus, the great shape-shifter. If one is to make any sense of this area, one needs to define the intellectual boundaries carefully.
This report does not discuss the extensive literature relating cardiovascular disease to depression, vital exhaustion, or type A behavior pattern. Similarly, the report does not discuss exercise stress, oxidative stress, or any of the multiple other physical stressors that impact on the heart. The report also excludes the rich literature derived from animal studies. Instead, the report discusses psychological stressors’ effects on the human heart.
The immense power and clinical utility of the concept of “stress” is that it refers to the organism's response to challenge. Nonetheless, the terminology is confusing. The term has its origins in engineering, where “stress” leads to “strain.” However, in physiology that distinction is blurred, and one thinks of “stress” as both the cause, the “stressor,” as well as the response to the stressor. To be pure, one is on surer ground if one refers to “stressors” and “responses to stressors”; however, that circumlocution is awkward.
What do patients mean when they complain of “stress”? They usually mean that they have become embroiled in unpleasant challenging new life circumstances, but sometimes they also refer to challenging new circumstances that are not exactly unpleasant but still demand attention (e.g., a promotion). Sometimes patients can pinpoint an exact event (“death in the family”); other times they refer to their overall life experience (“job stress,” “poverty”). Just as cardiologists qualitatively rate the extent of heart murmurs, psychologists and psychiatrists have a variety of ratings schemes for evaluating stress. Given that the complaint is entirely subjective, one either relies totally on the patient's self-report or else applies generally agreed upon rules for how stressful a given event is for most people. Alternatively, one can observe subjects during exposure to a stressor and then measure physiological and/or behavioral responses. Some researchers feel that the focus should not be on major life stressors but rather the daily hassles in life (rush hour traffic, preparing for Joint Commission on Accreditation of Healthcare Organizations visits, new rules on health care reimbursement, and so on). This report will discuss cardiovascular responses to acute major life stressors as well as chronic exposure to continuing stressors.
The report will differentiate acute from chronic stress because the psychological and physiological toll may be different in those settings. There is no crystal clear time point to separate acute from chronic, but this report considers stressors that last <1 week as “acute.” Studies of acute stress lend themselves to tighter experimental control and can also be better poised to address pathophysiological response mechanisms. The chronic stressor studies include both severe continuing adverse stressors (wartime) as well as chronic low level aggravations (hassles). In either event, with chronic stressors, experimental control is vastly more difficult and insight on underlying mechanisms is more tenuous. This distinction between acute and chronic is arbitrary; an acute sorrow can reverberate for years. The “stressor” may have lasted an instant (public criticism by a boss), but the patient may continue brooding about the humiliation for weeks or longer. To anticipate the last section of this review, patients’ coping strategies play a major role in determining the impact of a stressor.
Acute Stressors
There are 2 basic approaches to studying acute stressors: capitalizing on chance exposures in the environment versus modeling them in the laboratory. As an exemplar of chance disasters, this report will review what is known about earthquakes and the heart. This report will then review some of the laboratory findings flowing from experiments on reactivity to stressors.
Earthquakes
Earthquakes are unique disasters because they come with no warning. In addition, survivors are troubled by continuing aftershocks, which are ambiguous in their implications (“Is it another major quake?”). Widespread disasters cripple communications and transportation infrastructures. Although a 1-day interruption of electricity and water can be coped with, large-scale disasters typically result in multiple days or weeks of turmoil, inconvenience, worry, and loss. Of course, such disasters have an adverse effect on psychiatric morbidity, but what happens to the heart?
Extensive international data demonstrate an increased cardiovascular risk after earthquakes. The underlying mechanism for this risk is unclear. Given the emergency conditions surrounding a massive earthquake, it is difficult to conduct fine-grained experimental or epidemiologic studies. Thus, it is not known how much of the risk is conveyed by the emotional trauma acting alone versus factors like forgetting to take routine medications, living in cramped emergency quarters, facing disrupted sleep, and so on. Given the chaos surrounding massive disasters, it is unlikely that such data would ever be gathered.
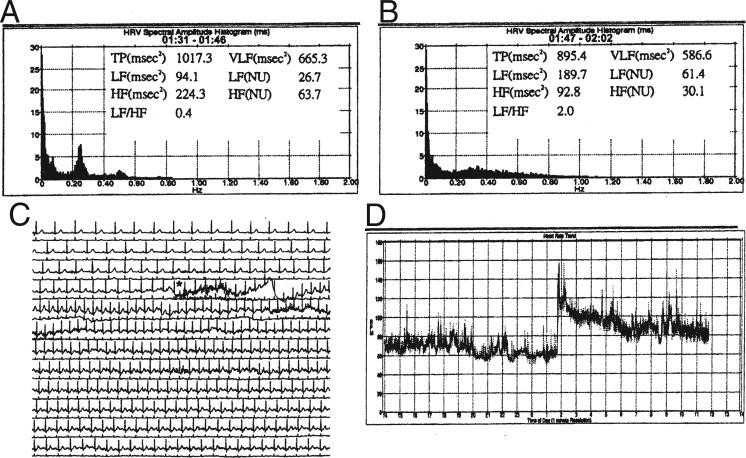
During the 1999 earthquake in Taiwan, 12 patients were being routinely studied with Holter monitoring. When the Holter was scored, contrasting the minutes before and minutes after the earthquake, pronounced increases in heart rate (HR) were observed at the time of the quake, up to 160 beats/min (Fig. 1). Perhaps more interesting was the observation that the HR variability itself changed, with a relative drop in high-frequency variability and an increase in the low-frequency/high-frequency ratio, denoting relative withdrawal of parasympathetic nervous system activity and an increase in sympathetic nervous system (SNS) activity (1). These changes were attenuated in patients who were receiving beta-blockers.
Figure 1. Holter Report During Earthquake.
(A and B) Heart rate variability 0 to 15 min before and 15 min after the earthquake, respectively. The histogram shows a decrease in the high-frequency (HF) zone and an increase in the low-frequency (LF)/HF ratio from 0.4 to 2.0. (C and D) A sudden increase in heart rate up to 160 beats/min and sinus tachycardia that persisted for 58 min. NU = normalized units; TP = total power; VLF = very low frequency. Reprinted, with permission, from Huang et al. (1).
Dating back to Cannon's work, investigators have observed stressors’ effects on various components of the hemostasis system (2). The Hanshin-Awaji earthquake in Japan in 1995 provided an opportunity to examine hemostatic changes in the face of massive stress. In addition to noting that BP increased and that some patients’ nocturnal BP no longer “dipped” after the earthquake, observers reported that blood viscosity increased as reflected by increases in hematocrit and markers of procoagulant activity (fibrinogen, von Willebrand factor, and D-dimer) also increased (3).
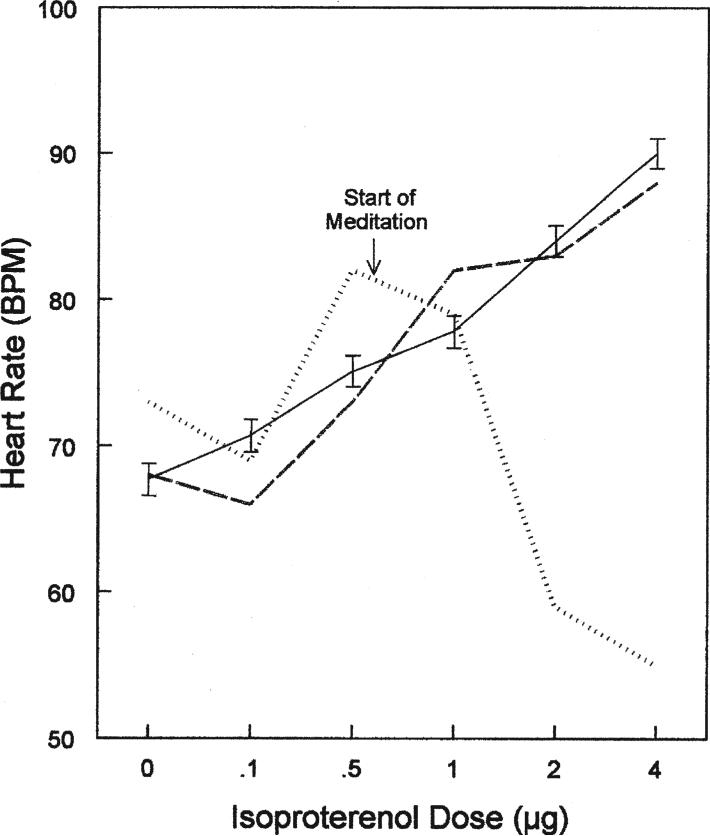
There is an increased risk for pulmonary embolism in the wake of earthquakes (4). In 2004, Central Nigata, Japan, was struck by 3 strong earthquakes and 90 aftershocks in the ensuing week. One hundred thousand residents were evacuated from their homes, and many of them spent nights sleeping in their cars. The combination of the psychological stress and the relative immobilization in cars resulted in a dramatic increase in pulmonary embolism (Fig. 2).
Figure 2. Incidence of Pulmonary Embolism Associated With Earthquake.
Patients with pulmonary embolism (A to C) and shock in the Niigata-Chuetsu earthquake (D). Pulmonary embolism increased after the earthquake compared with the prior 4 weeks and the corresponding 8 weeks in 2002 and 2003. The number of shocks was cited from the official records of the Niigata-Chuetsu earthquake by Japan Meteorological. p < 0.001 versus prior 4 weeks in *2004 or corresponding 8 weeks in †2002 or ‡2003. Reprinted, with permission, from Watanabe et al. (4).
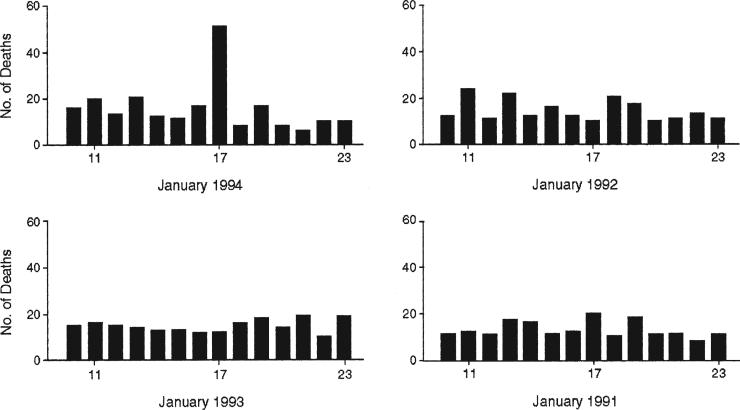
The Northridge, California earthquake in 1994 was well studied in terms of cardiovascular consequences. The daily numbers of deaths attributed to cardiovascular disease increased dramatically on the day of the earthquake, as contrasted with the same date in previous years (Fig. 3) (5).
Figure 3. Daily Cardiac Deaths in Los Angeles Associated With Earthquake.
On the day of the earthquake (January 17, 1994), there was a sharp rise in the number of deaths related to atherosclerotic cardiovascular disease (n = 51, relative risk 2.6, 95% confidence interval 1.8 to 3.7). The daily number of deaths related to atherosclerotic cardiovascular disease declined in the 6 days after the earthquake (z = 3.15, p = 0.002). Reprinted, with permission, from Leor et al. (5).
The data are not unanimous about the impact of earthquakes on the heart. Brown (6), for instance, found that the 1989 Loma Prieta earthquake in California was not associated with an increase in myocardial infarctions (MIs). However, Brown (6) pointed out that earthquakes are not all the same. In addition to differences in their Richter magnitude and their duration, they cause varying amounts of destruction; furthermore, quakes with an onset in the middle of the night are particularly distressing. This “time of day” effect is interesting, because many studies have demonstrated that the waking hours represent the time of greatest cardiovascular risk.
One could study other types of disasters to examine the effects of short-term catastrophic stressors on cardiovascular functioning, but the earthquake literature is some of the most substantial, with replications throughout the world. There is no reason to suppose that earthquakes are unique short-term severe stressors. Parallel literatures could be cited in terms of sudden deaths in the context of acute bereavement or cardiac events in the courthouse. It is difficult to achieve much experimental control in these sorts of studies conducted in the free-ranging environment. For that level of control, one turns to the literature on experimental laboratory-based studies.
Short-term experimental stressors
The laboratory offers a controlled environment to study the extensive questions that naturalistic studies inevitably raise. Are the cardiac adverse effects of disasters attributable to change in diet, skipped medications, and exposure to toxic substances? Are patients with pre-existing known cardiac disease more vulnerable to stressors? How long or how aversive must a stressor be to detect adverse cardiac functioning? These are the sorts of questions that lend themselves to experimental approaches.
“Stress testing” in the sense of aerobic exercise testing is readily performed in the laboratory setting, but psychological stress testing is slightly more difficult to carry out. There are countless studies that examine physiological reactivity to low-level stressors like mental arithmetic calculations. These approaches lend themselves to tight experimental control, but their generalizability to “real world” stress is always questionable. Another way of saying this is that although such stressors are highly reliable, they are questionable in terms of their validity as markers of response to real world stressors like arguments with one's teen-age daughter.
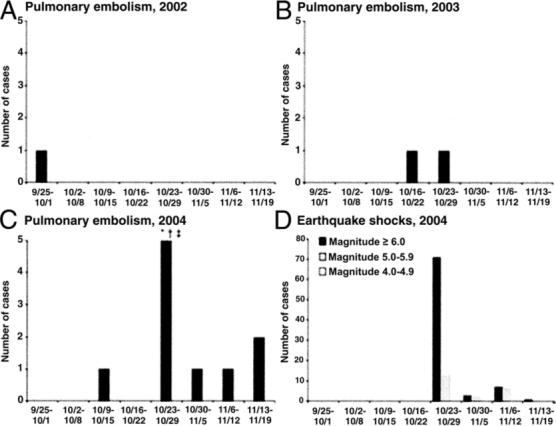
There have been some intermediate approaches to studying short-term stressors that will be highlighted in this article. These approaches use telemetry to study patients’ responses in their world. Public speaking provides an excellent model for the telemetry approach. For many individuals, public speaking is a trying experience, so trying that young doctors frequently dose themselves with beta-blockers in an effort to dampen their anxiety. Using indwelling intravenous catheters, Dimsdale and Moss (7) studied young house officers who were making formal presentations at various conferences. Figure 4 presents some of these data. The dashed line reveals that, on average, epinephrine increased 3-fold. However, the outliers are worth noting. The high responder was an individual who stood up, said “first slide, please,” and then had the misery of giving his totally slide-dependent talk by himself when the projector bulb blew. This sort of study reveals both the robust effect and the wide range of effects that behavioral stressors have on real-world SNS responses.
Figure 4. Effect of Public Speaking on Plasma Epinephrine.
Plasma epinephrine response to different activities. Each line represents a single subject; the dotted line indicates the mean. Reprinted, with permission, from Dimsdale and Moss (7).
Holter monitoring for rhythm or for documenting ischemia lends itself extremely well to studies of the impact of stress on the heart. These findings are so widely reported that they will not be reviewed here other than to emphasize the dissociation between anginal pain and ischemia. In patients with documented coronary artery disease (CAD) who were studied with Holter recording, Krantz et al. (8) found only sparse agreement between episodes of chest pain and episodes of ST-segment depression.
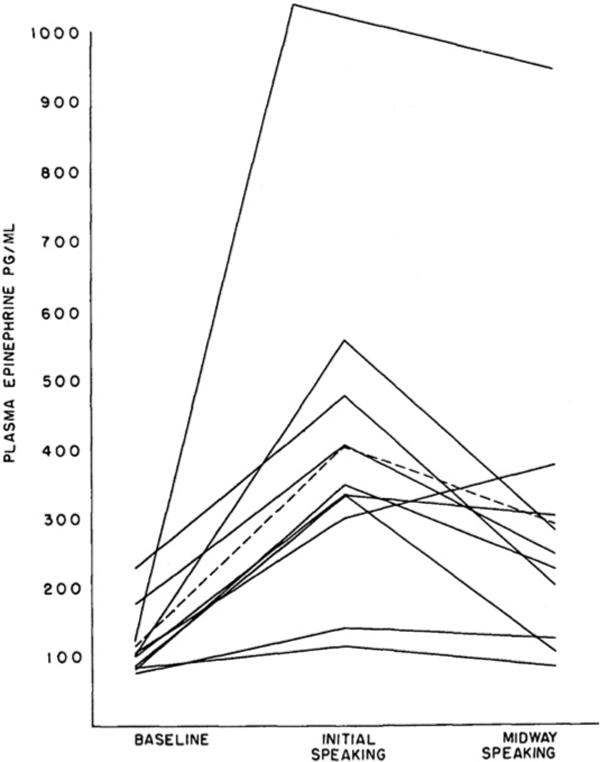
In an effort to better delineate the stress-ischemia relationship, Deanfield et al. (9) compared angina and myocar-dial ischemia after exposure to diverse stressors. The regional myocardial uptake of rubidium-32 was studied with positron emission tomography scanning before and after bicycle ergometry as well as before and after a 2-min period of serial-7 subtraction. In response to exercise, all patients showed abnormal regional perfusion and ST-segment wave changes, and almost all of the patients also reported anginal symptoms. An interesting contrast was observed with mental stress testing. While mental stress testing elicited extensive changes in regional perfusion (Fig. 5), the changes were not as straightforward as those with exercise. First, only 75% of the patients manifested the abnormal perfusion. More striking, however, was the dissociation between perfusion abnormalities, ST-segment wave changes, and chest pain. Of those who developed perfusion changes, only 33% also had both angina and ST-segment depression; 17% had ST-segment depression alone, and fully 50% had neither ST-segment depression nor angina. In other words, the psychological stressor was almost as consistently evocative of myocardial perfusion abnormalities as was exercise testing, but the perfusion abnormalities elicited by the psychological stressor were more likely to be silent by self-report and electrocardiogram. Similar findings were observed in another study that found that 60% of CAD patients developed wall motion abnormalities during mental stress testing (10).
Figure 5. Effect of Mental Stress and Exercise on Regional Myocardial Uptake.
Changes in regional myocardial uptake or rubidium-82 and in electrocardiogram in relation to chest pain before and after mental arithmetic or exercise. Control scans show homogeneous regional cation uptake. In the patient above there are defects in uptake (arrows) by the anterior wall with mental arithmetic and exercise, and these changes are accompanied by ST-segment depression and angina. A = anterior wall; FW = left ventricular free wall; S = interventricular septum. Adapted and reprinted, with permission, from Deanfield et al. (9).
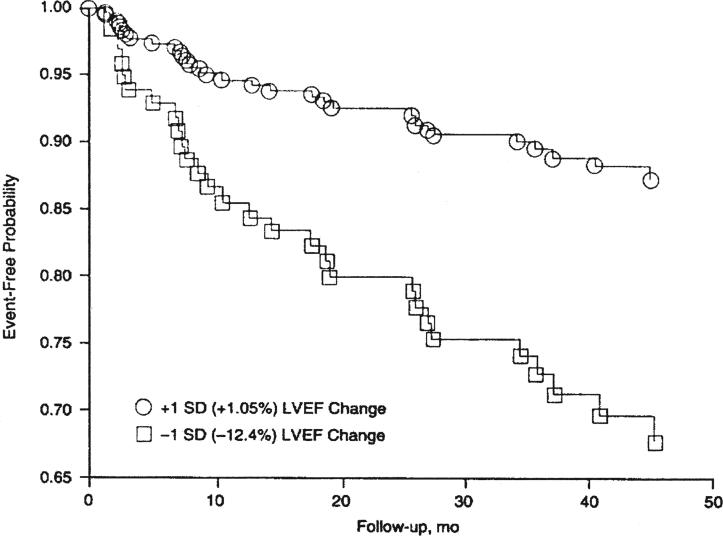
Do acute stress responses in the laboratory relate to clinical course? Certain sorts of patients such as patients with idiopathic long QT interval are remarkably sensitive to emotional stresses (11). However, these patients are assumed to be “zebras,” rare creatures in our waiting rooms. Jiang et al. (12) examined a series of patients with CAD, studying their stress responses in the laboratory and tracking their course over the ensuing years. Radionuclide ventriculography was used to quantify wall motion abnormalities and ejection fraction (EF) in response to laboratory stressors. First, it was striking to see that 67% of CAD patients developed either wall motion abnormalities or a >5% drop in left ventricular EF in response to mental arithmetic; that is, they were not rare “zebras” at all but were frequently encountered. Second, these changes were not merely “academic.” In a 4-year follow-up, the onset of new cardiac events was tracked. Patients who manifested a drop in left ventricular EF in response to stress were 2.4 times more likely to develop a cardiac event in the follow-up period. Figure 6 graphs the event-free survival as a function of stress-induced decrease in left ventricular EF. Similar findings were observed in the PIMI (Psychophysiological Investigations of Myocardial Ischemia) study, where the degree of wall motion abnormalities elicited by a public speaking stressor predicted all-cause mortality in CAD patients followed for 5 years (13).
Figure 6. Probability of Cardiac Event–Free Survival in Patients With and Without a Stress-Induced Drop in LVEF.
Probability of event–free survival as a function of mental stress-induced left ventricular ejection fraction (LVEF) change plotted at 2 prototypical values, 1 standard deviation (SD) below (LVEF change =−12.40%) and 1 SD above (LVEF change =+1.05%) the mean of the entire sample (LVEF change = −6.73%). Curves are adjusted for baseline LVEF, history of myocardial infarction, and age. The risk ratio associated with the lower curve compared with the higher curve is 2.40 (p = 0.02). Reprinted, with permission, from Jiang et al. (12).
Wittstein et al. (14) examined 19 patients with left ventricular dysfunction that appeared in the setting of intense emotional stress (death in the family, court appearance, and so on). Upon arriving at the hospital, these patients had severe left ventricular dysfunction that rapidly improved from an EF of 20% on admission to 45% 4 days later. The patients presented with transient left ventricular apical ballooning and massively elevated plasma catecholamines. Four of the 5 patients who had endomyocar-dial biopsy showed interstitial infiltrates and contraction band abnormalities, reminiscent of previously reported abnormalities found in coroners’ studies of emotional sudden cardiac deaths (15). Sharkey et al. (16) reported similar findings in terms of acute and reversible cardiomyopathy provoked by catastrophic stress in patients with no prior history of cardiovascular disease (Fig. 7).
Figure 7. Angiogram in Stress Cardiomyopathy.
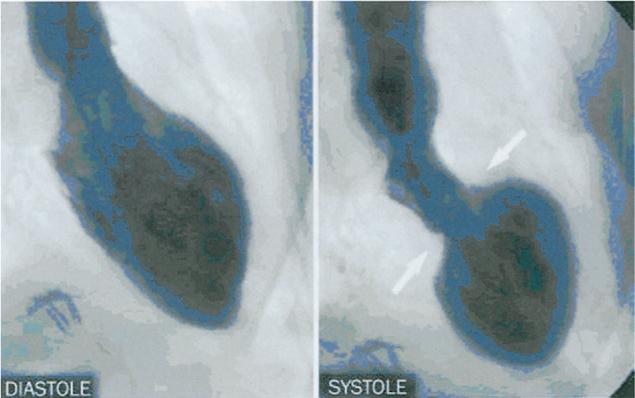
Left ventricular angiogram in diastole (left) and systole (right) in right anterior oblique projection demonstrating wall motion abnormality characteristic of stress cardiomyopathy. At end systole, left ventricular chamber adopts distinctive “short neck with round flask” configuration in which distal (apical) portion is akinetic/hypokinetic whereas, in contrast, the remaining proximal (basal) segment is hypercontractile (sharp area of transition is shown by arrows). Reprinted, with permission, from Sharkey et al. (16).
Implantable defibrillators offer unusual access to data on stress and arrhythmias. Some investigators have imposed stressors on patients while undergoing noninvasive programmed stimulation. When patients were performing arithmetic or were instructed to recall anger-eliciting events in their lives, the induced ventricular tachycardia was faster and more difficult to terminate through pacing, and 40% of the patients actually required a shock to terminate the stress-induced arrhythmia (17). Other investigators have observed that horrific disasters, such as the World Trade Center attack, doubled the rate of ventricular arrhythmias in patients fitted with implantable defibrillators (18).
Chronic Stressors
Studies reporting effects of chronic stressors on cardiovascular disease are more likely epidemiological than patho-physiological in nature. They usually focus on topics such as job stress, marital discord, or perceptions of being treated unfairly. However, there is a beginning interest in chronic every day hassles that vitiate one's morale and may have health consequences. These everyday niggling aggravations are certainly not benign in terms of morale. In addition, chronic hassles are associated with worsening health behaviors in terms of smoking and exercise (19) and in terms of levels of inflammatory and procoagulant markers (20). Although most of the chronic stressor research focuses on more virulent stressors, this study of day-to-day micro-stressors is likely to be a focus of increasing future research.
The paradigmatic studies of chronic stressors examine BP during wartime. For instance, during the siege of Leningrad, BP increased dramatically. What is more striking is that the effect of that siege combined with its starvation conditions cast a long shadow into the future. Even 50 years later, survivors of the Leningrad siege had increased BP and increased mortality from cardiovascular disease compared with Russians who had not been in the besieged city (21).
The INTERHEART study (22) investigated the relation of chronic stressors to incidence of MI in a sample of ∼25,000 people from 52 countries. Stress was defined as “feeling irritable, filled with anxiety, or as having sleeping difficulties as a result of conditions at work or at home.” After adjusting for age, gender, geographic region, and smoking, those who reported “permanent stress” at work or at home had >2.1 times the risk for developing an MI.
Of course these reports of stress are subjective, but stress is, after all, subjective. The problem is that after sustaining a cardiac event, the patient strives harder to remember stressors, a kind of retrospective distortion of history that can introduce bias. The only way around that is to prospectively assess stress and wait for the onset of cardiac events. That kind of study requires large sample sizes in the general population or somewhat smaller sample sizes in high-risk patients. There are some such studies concerning chronic job stress.
One model for job stress views jobs that are highly demanding and that allow the employee relatively little control as “high stress.” An alternate model for job stress considers effort–reward imbalance, a mismatch between high efforts at work and low reward. There are many epidemiologic studies suggesting that individuals with such high-stress jobs are at increased cardiovascular risk. Studies from Stockholm (23) found that initial MI patients were significantly more likely to have high work demands and low control. The Whitehall II study (24) found a 2.15-fold increased risk for new coronary heart disease in men who experienced a mismatch between effort and reward at work. The high-risk subjects were those who were competitive, hostile, and overcommitted at work, in the face of poor promotion prospects and blocked careers.
Increasingly, studies are examining possible pathophysiological pathways of job stress. How does job stress increase risk? While the answer to that question is enormously complicated, tantalizing data are accumulating. Subjects who are in low control jobs have blunted baroreflex sensitivity; that is, when their BP increases, they fail to make the appropriate adjustments of HR (25). Other studies have demonstrated that workers with low job control respond to stressors in the laboratory environment with increased fibrinogen (26). Such studies seem to suggest that the job-stressed patient is primed to hyper-respond to stressors even outside of the work environment.
Freud said that happiness comes when one has pleasure in love and work. Orth-Gomer et al. (27) studied the impact of work stress and marital stress on the subsequent incidence of CAD in a cohort of Stockholm women followed for ∼5 years. Marital stress was associated with a 2.9-fold increased risk of recurrent events, whereas work stress did not predict subsequent coronary events in these women. Similar data are available for men in the MRFIT (Multiple Risk Factor Intervention Trial). That trial found that chronic work stress and marital dissolution increased the risk of cardiovascular mortality in men who were followed for 9 years (28). As the late Dutch internist Johannes Groen (one of the original observers of the link between dietary cholesterol and heart disease) used to say, “What's a man to do, where can he go if he is unhappy at work and at home?” The implied, if somewhat flamboyant, answer was always “to an early grave.”
There have been some interesting recent reports examining how chronic stress may relate to some of the physiological underpinnings of cardiac risk. Two unhappily prevalent chronic stressors (discrimination and caregiving) have provided informative data about how these risks operate.
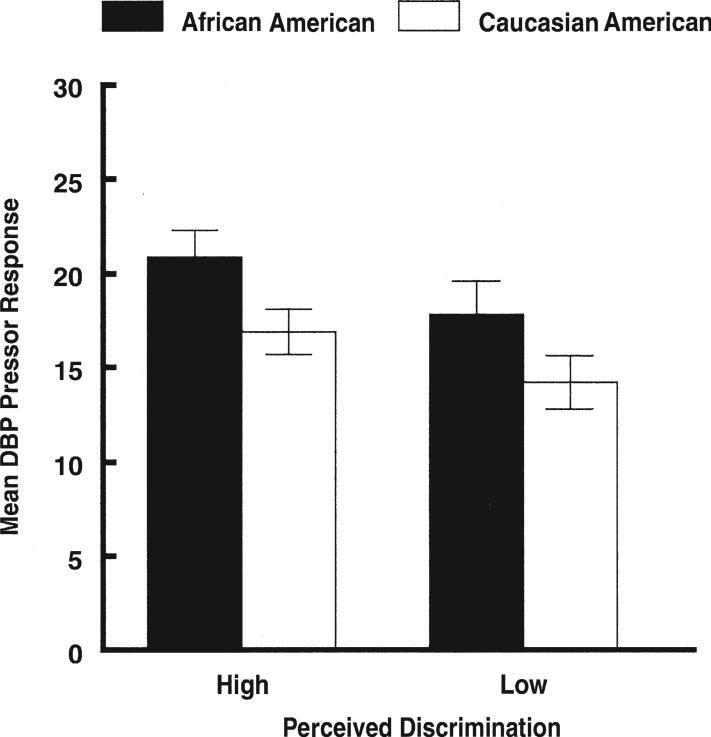
Experience of ethnic discrimination is a lancinating event that echoes over a lifetime. While florid discrimination is less present in the U.S., subtle micro-aggressions based on race, religion, and so on are common. Other than being upsetting, does discrimination have a cardiac toll? In a recent study, Thomas et al. (29) examined how perceived discrimination was related to pressor sensitivity in healthy subjects. Phenylephrine was infused intravenously, and the investigators examined the resulting increase in diastolic BP. Regardless of race, those subjects who reported experiencing more discrimination in their lives had a significantly increased pressor sensitivity in the face of equivalent amounts of SNS agonist infusion (Fig. 8).
Figure 8. Effect of Perceived Discrimination on Pressor Sensitivity.
Effects of ethnicity and perceived discrimination on diastolic pressor response. For visual purposes, perceived discrimination was dichotomized into high and low groups using median split. Individuals who perceive more ethnic discrimination have greater blood pressure responses to phenylephrine (p < 0.05). DBP = diastolic blood pressure. Reprinted, with permission, from Thomas et al. (29).
Millions of Americans provide caregiving for an ill family member. One of the most frequent and harrowing scenarios for caregiving involves taking care of a spouse with dementia. The unremitting downhill course of the patient is profoundly dispiriting for the caregiver. The Caregiver Health Effects study (30) followed ∼400 caregivers and ∼400 matched control subjects. In a 4-year period, caregivers had a 63% higher mortality rate than noncaregiving control subjects. The increased mortality was particularly evident in caregivers who already had known cardiovascular disease. In a series of mechanistically oriented studies, the San Diego Caregiver study examined possible pathways between caregiving and cardiovascular disease. The investigators found that distressed caregivers had an increased risk for developing hypertension when followed over a 6-year period (31). Other reports from this group have found that caregivers have increased levels of D-dimer, a circulating procoagulant factor (32), more sleep disruption, and higher level of circulating plasma inflammatory cytokines (33).
Vulnerability, Resilience, and Treatment Considerations
At this point certain tough questions about stress and heart disease need to be answered.
Are the data unanimous about the effects of stress on cardiovascular disease? Obviously not. There are contradictory studies about all risks; not all studies, for instance, find that increased cholesterol is associated with angiographically-proven CAD. From the earliest days of cardiology, there has been a suspicion that stress has powerful adverse effects on the heart. In the first volume of Circulation, for instance, one finds the topic reviewed by Harold Wolff (34). Over the years, the empirical reports and reviews have proliferated, and this review tries to give a contemporary overview of the sorts of approaches being examined at the start of the 21st century. One would have to conclude that the overall data suggest that stress contributes to adverse clinical cardiac events and provides a milieu of increased vulnerability to the heart. That is not to say that “stress causes heart disease.” That simplistic notion is nonviable (as is a similar statement that “high cholesterol causes heart disease”) because heart disease is so heterogeneous and multiply-determined in terms of vulnerability and resilience.
How important is stress in comparison with more traditional risk factors like elevated cholesterol? There are different ways of quantifying cholesterol's risks in populations with varying degrees of vulnerability. However, if one examines the risk of increased cholesterol in studies such as the Framingham study, relative risks of total cholesterol 200 to 239 mg/dl are 1.31; for total cholesterol levels >240 mg/dl, the risks are approximately 1.9 (35). Many of the stressor studies reviewed above show risk gradients comparable to or steeper than the risk gradient of elevated cholesterol.
Is not all of the effect of stress on the heart due to other adverse behaviors such as smoking? Sure, smoking is poison. No argument. The problem is that once people are addicted, it becomes enormously difficult to get them off tobacco when their life stress and depression levels are elevated (36). In addition, many of the larger epidemiologic studies referenced in the preceding text controlled for risk-enhancing behaviors such as smoking and obesity. Thus, one way or another, stress has to be dealt with in modifying other health behaviors.
Will considerations of stress lead to a flood of forensic cases? Yes. Extensive case law is accumulating concerning the role of stress and heart disease, and most physicians who do forensic work in psychiatry or cardiology can expect to be asked to testify in such cases. Short-term unusual severe stressors as well as job stress allegations are already heavily present on the court dockets, particularly in workmen's compensation cases. Courts are interested in whether stress “caused” or “contributed to” the development of a condition. Given the multiply-determined nature of cardiovascular disease, it is clear that psychological stressors contribute to cardiovascular disease, but “how much?” It is hard to assert that “stress caused this patient's disease,” just as one would be hard pressed to state that a “high fat diet caused this patient's disease.” Courts are also troubled about how to handle populations of extra vulnerability. Could a stressful stimulus be reasonably expected to elicit a fatal arrhythmia in the “average” patient with arrhythmias? Can one assign blame/causation/contribution when the stressor was relatively mild but the patient was singularly vulnerable (e.g., patients with long QT syndrome)? Thus, the answer to the question about forensic implications of stress is that our society has already been wrestling with this issue for a long time.
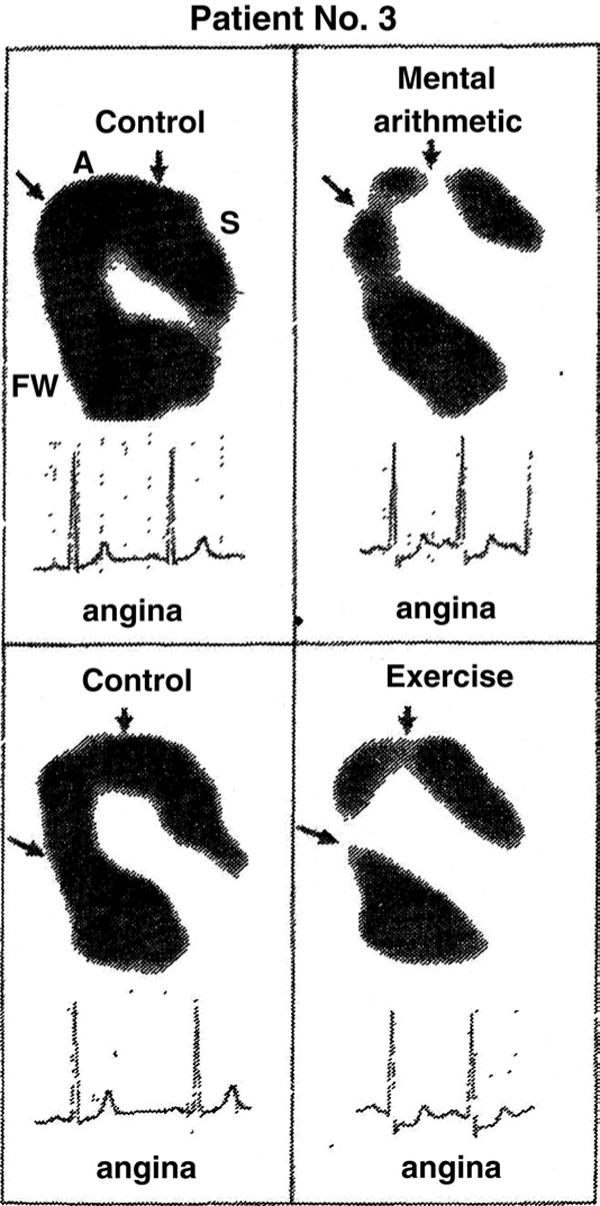
Because stress is everywhere, what good does it do to identify a risk factor that cannot be modified? There are 2 replies to this question. Stress is no different from other background cardiac risk factors such as genetics or age. There is no reason to ignore such factors, just because they are not modifiable. However, stress can be modified through numerous approaches. It remains to be proven if such stress modifications consistently decrease the risk for MI and cardiac death (37). However, in terms of more modest goals, the interventions are certainly effective in addressing other end points such as patient well-being. Diverse and effective stress intervention programs have been tested in heart patients, programs that provide formal psychotherapy, psychotropic medications, time management training, progressive relaxation training, meditation, or regular exercise. The therapeutic nihilists are wrong. The majority of these intervention programs improve patients’ morale and functioning and decrease suffering. Increasingly, such programs are tracking markers of cardiovascular risk (such as endothelial function) as opposed to cardiac events and find that the psychosocial intervention programs have positive effects (38). The powerful effects of behavioral interventions sometimes become evident by serendipity. Years ago, we were infusing isoproterenol as a way of measuring in vivo beta-adrenergic receptor sensitivity. The average HR response to increasing doses of isoproterenol was admirably consistent until we happened to study a subject who got bored with the testing and started quietly meditating (39). No increased HR was detected! Figure 9 provides graphic detail of the potential powers of behavioral intervention to block even pharmacologic stress effects.
Figure 9. Effect of Meditation on HR Response to Infused Isoproterenol.
Effects of meditation on chronotropic responses to isoproterenol. (Solid line) Mean ± standard error response to isoproterenol in 93 women; (dotted line) patient's response while meditating; (dashed line) patient's response while instructed not to meditate. BPM = beats/min; HR = heart rate. Reprinted, with permission, from Dimsdale and Mills (39).
Conclusions
Cardiovascular responses to stress are exquisitely coordinated and functional up to a point. When the stressor continues or when the patient continues imposing the stressor through brooding, there are adverse effects on the heart. These stress effects, like other settings of cardiac risk, are potentially modifiable, if not by cardiologists themselves, then by their colleagues who help patients change their behaviors and cognitions.
Acknowledgments
The author thanks Beatrice Golomb, Paul Mills, Jan Stiglitz, and Michael Ziegler, as well as the Journal's anonymous reviewer for helpful comments and criticism.
This work has been supported by grants HL36005, HL44915, M01-RR0827, and CA23100 from the National Institutes of Health.
Abbreviations and Acronyms
- BP
blood pressure
- CAD
coronary artery disease
- EF
ejection fraction
- HR
heart rate
- MI
myocardial infarction
- SNS
sympathetic nervous system
REFERENCES
- 1.Huang J, Chiou C, Ting C, Chen Y, Chen S. Sudden changes in heart rate variability during the 1999 Taiwan earthquake. Am J Cardiol. 2001;87:245–8. doi: 10.1016/s0002-9149(00)01331-x. [DOI] [PubMed] [Google Scholar]
- 2.von Kanel R, Mills P, Fainman C, Dimsdale J. Effects of psychological stress and psychiatric disorders on blood coagulation and fibrinolysis: a biobehavioral pathway to coronary artery disease? Psychosomatic Med. 2001;63:531–44. doi: 10.1097/00006842-200107000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Matsuo T, Suzuki S, Kodama K, Kario K. Hemostatic activation and cardiac events after the 1995 Hanshin-Awaji Earthquake. Int J Hematol. 1998;67:123–9. doi: 10.1016/s0925-5710(97)00118-7. [DOI] [PubMed] [Google Scholar]
- 4.Watanabe H, Kodama M, Tanabe N, et al. Impact of earthquakes on risk for pulmonary embolism. Int J Cardiol. 2008 doi: 10.1016/j.ijcard.2007.06.039. In press. [DOI] [PubMed] [Google Scholar]
- 5.Leor J, Poole W, Kloner R. Sudden cardiac death triggered by an earthquake. N Engl J Med. 1996;334:413–9. doi: 10.1056/NEJM199602153340701. [DOI] [PubMed] [Google Scholar]
- 6.Brown D. Disparate effects of the 1989 Loma Prieta and 1994 Northridge earthquakes on hospital admissions for acute myocardial infarction: importance of superimposition of triggers. Am Heart J. 1999;137:830–6. doi: 10.1016/s0002-8703(99)70406-0. [DOI] [PubMed] [Google Scholar]
- 7.Dimsdale JE, Moss J. Short term catecholamine response to psychological stress. Psychosom Med. 1980;42:493–7. doi: 10.1097/00006842-198009000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Krantz D, Hedges S, Gabbay F, et al. Triggers of angina and ST-segment depression in ambulatory patients with coronary artery disease: evidence for an uncoupling of angina and ischemia. Am Heart J. 1994;128:703–12. doi: 10.1016/0002-8703(94)90268-2. [DOI] [PubMed] [Google Scholar]
- 9.Deanfield J, Shea M, Kensett M, et al. Silent myocardial ischaemia due to mental stress. Lancet. 1984;2:1001–5. doi: 10.1016/s0140-6736(84)91106-1. [DOI] [PubMed] [Google Scholar]
- 10.Rozanski A, Bairey C, Krantz D, et al. Mental stress and the induction of silent myocardial ischemia in patients with coronary artery disease. N Engl J Med. 1988;318:1005–12. doi: 10.1056/NEJM198804213181601. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz PJ, Zaza A, Locati E, Moss AJ. Stress and sudden death: the case of the long QT syndrome. Circulation. 1991;83(Suppl II):II71–80. [PubMed] [Google Scholar]
- 12.Jiang W, Babyak M, Krantz D, et al. Mental stress-induced myocar-dial ischemia and cardiac events. JAMA. 1996;275:1651–6. doi: 10.1001/jama.275.21.1651. [DOI] [PubMed] [Google Scholar]
- 13.Sheps D, McMahon R, Becker L, et al. Mental stress-induced ischemia and all-cause mortality in patients with coronary artery disease: results from the psychophysiological investigations of myocardial ischemia study. Circulation. 2002;105:1780–4. doi: 10.1161/01.cir.0000014491.90666.06. [DOI] [PubMed] [Google Scholar]
- 14.Wittstein I, Thiemann D, Lima J, et al. Neurohumoral features of myocardial stunning due to sudden emotional stress. N Engl J Med. 2005;352:539–48. doi: 10.1056/NEJMoa043046. [DOI] [PubMed] [Google Scholar]
- 15.Cebelin M, Hirsch C. Human stress cardiomyopathy. Myocardial lesions in victims of homicidal assaults without internal injuries. Hum Pathol. 1980;11:123–32. doi: 10.1016/s0046-8177(80)80129-8. [DOI] [PubMed] [Google Scholar]
- 16.Sharkey S, Lesser J, Zenovich A, et al. Acute and reversible cardiomyopathy provoked by stress in women from the United States. Circulation. 2005;111:472–9. doi: 10.1161/01.CIR.0000153801.51470.EB. [DOI] [PubMed] [Google Scholar]
- 17.Lampert R, Jain D, Burg M, Batsford W, McPherson C. Destabilizing effects of mental stress on ventricular arrhythmias in patients with implantable cardioverter-defibrillators. Circulation. 2000;101:158–64. doi: 10.1161/01.cir.101.2.158. [DOI] [PubMed] [Google Scholar]
- 18.Steinberg J, Arshad A, Kowalski M, et al. Increased incidence of life-threatening ventricular arrhythmias in implantable defibrillator patients after the World Trade Center attack. J Am Coll Cardiol. 2004;44:1261–4. doi: 10.1016/j.jacc.2004.06.032. [DOI] [PubMed] [Google Scholar]
- 19.Twisk J, Snel J, Kemper H, van Mechelen W. Changes in daily hassles and life events and the relationship with coronary heart disease risk factors: a 2-year longitudinal study in 27−29 year old males and females. J Psychosom Res. 1999;46:229–40. doi: 10.1016/s0022-3999(98)00088-9. [DOI] [PubMed] [Google Scholar]
- 20.Jain S, Mills P, von Kanel R, Hong S, Dimsdale J. Effects of perceived stress and uplifts on inflammation and coagulability. Psychophysiology. 2007;44:154–60. doi: 10.1111/j.1469-8986.2006.00480.x. [DOI] [PubMed] [Google Scholar]
- 21.Sparen P, Vagero D, Shestov D, et al. Long term mortality after severe starvation during the siege of Leningrad: a prospective cohort study. BMJ. 2004;328:11–5. doi: 10.1136/bmj.37942.603970.9A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rosengren A, Hawken S, Ounpuu S, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11,119 cases and 13,646 controls from 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:953–62. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- 23.Theorell T, Tsutsumi A, Hallquist J, et al. Decision latitude, job strain, and myocardial infarction: a study of working men in Stockholm. Am J Public Health. 1998;88:382–8. doi: 10.2105/ajph.88.3.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bosma H, Peter R, Siegrist J, Marmot M. Two alternative job stress models and the risk of coronary artery disease. Am J Public Health. 1998;88:68–74. doi: 10.2105/ajph.88.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thomas K, Nelesen R, Ziegler M, Bardwell W, Dimsdale J. Job strain, ethnicity, and sympathetic nervous system activity. Hypertension. 2004;44:891–6. doi: 10.1161/01.HYP.0000148499.54730.0d. [DOI] [PubMed] [Google Scholar]
- 26.Steptoe A, Kunz-Ebrecht S, Owen N, et al. Influence of socioeconomic status and job control on plasma fibrinogen responses to acute mental stress. Psychosom Med. 2003;65:137–44. doi: 10.1097/01.psy.0000039755.23250.a7. [DOI] [PubMed] [Google Scholar]
- 27.Orth-Gomer K, Wamala S, Horsten M, Schenck-Gustafsson K, Schneiderman N, Mittleman M. Marital stress worsens prognosis in women with coronary heart disease: the Stockholm female coronary risk study. JAMA. 2000;284:3008–14. doi: 10.1001/jama.284.23.3008. [DOI] [PubMed] [Google Scholar]
- 28.Matthews K, Gump B. Chronic work stress and marital dissolution increase risk of posttrial mortality in men from the Multiple Risk Factor Intervention trial. Arch Intern Med. 2002;162:309–15. doi: 10.1001/archinte.162.3.309. [DOI] [PubMed] [Google Scholar]
- 29.Thomas K, Nelesen R, Malcarne V, Ziegler M, Dimsdale J. Ethnicity, perceived discrimination, and vascular reactivity to phenylephrine. Psychosom Med. 2006;68:692–7. doi: 10.1097/01.psy.0000238214.80871.e6. [DOI] [PubMed] [Google Scholar]
- 30.Schulz R, Beach S. Caregiving as a risk factor for mortality: the caregiver health effects study. JAMA. 1999;282:2215–9. doi: 10.1001/jama.282.23.2215. [DOI] [PubMed] [Google Scholar]
- 31.Shaw W, Patterson T, Ziegler M, Dimsdale J, Grant I. Accelerated risk of hypertensive blood pressure recordings among Alzheimer caregivers. J Psychosom Res. 1999;46:215–27. doi: 10.1016/s0022-3999(98)00084-1. [DOI] [PubMed] [Google Scholar]
- 32.Von Kanel R, Dimsdale J, Adler K, Patterson T, Mills P, Grant I. Exaggerated plasma fibrin formation (D-dimer) in elderly Alzheimer caregivers as compared to non-caregiving controls. Gerontology. 2005;51:7–13. doi: 10.1159/000081428. [DOI] [PubMed] [Google Scholar]
- 33.von Kanel R, Dimsdale J, Ancoli-Israel S, et al. Poor sleep is association with higher plasma proinflammatory cytokine interleukin-6 and procoagulant marker fibrin D-dimer in older Alzheimer caregivers. J Am Geriatrics Soc. 2006;54:431–7. doi: 10.1111/j.1532-5415.2005.00642.x. [DOI] [PubMed] [Google Scholar]
- 34.Wolff H. Life stress and cardiovascular disease. Circulation. 1950;1:187–203. doi: 10.1161/01.cir.1.2.187. [DOI] [PubMed] [Google Scholar]
- 35.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–47. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 36.Siahpush M, Carlin JB. Financial stress, smoking cessation and relapse: results from a prospective study of an Australian national sample. Addiction. 2006;101:121–7. doi: 10.1111/j.1360-0443.2005.01292.x. [DOI] [PubMed] [Google Scholar]
- 37.Rees K, Bennett P, West R, Davey Smith G, Ebrahim S. Psychological interventions for coronary heart disease. Cochrane Database Syst Rev. 2004;2:CD002902. doi: 10.1002/14651858.CD002902.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Blumenthal J, Sherwood A, Babyak M, et al. Effects of exercise and stress management training on markers of cardiovascular risk in patients with ischemic heart disease: a randomized controlled trial. JAMA. 2005;293:1626–34. doi: 10.1001/jama.293.13.1626. [DOI] [PubMed] [Google Scholar]
- 39.Dimsdale J, Mills P. An unanticipated effect of meditation on cardiovascular pharmacology and physiology. Am J Cardiol. 2002;90:908–9. doi: 10.1016/s0002-9149(02)02726-1. [DOI] [PubMed] [Google Scholar]