Abstract
Objective
A major problem in the delivery of mental health services is the lack of availability of empirically supported treatment, particularly in rural areas. To date no studies have evaluated the administration of an empirically supported manual-based psychotherapy for a psychiatric condition via telemedicine. The aim of this study was to compare the relative efficacy and acceptability of a manual-based cognitive–behavioral therapy (CBT) for bulimia nervosa (BN) delivered in person to a comparable therapy delivered via telemedicine.
Method
One hundred twenty-eight adults meeting DSM-IV criteria for BN or eating disorder—not otherwise specified with binge eating or purging at least once per week were recruited through referrals from clinicians and media advertisements in the targeted geographical areas. Participants were randomly assigned to receive 20 sessions of manual-based, CBT for BN over 16 weeks delivered either face-to-face (FTF-CBT) or via telemedicine (TV-CBT) by trained therapists. The primary outcome measures were binge eating and purging frequency as assessed by interview at the end of treatment, and again at 3- and 12-month follow-ups. Secondary outcome measures included other bulimic symptoms and changes in mood.
Results
Retention in treatment was comparable for TV-CBT and FTF-CBT. Abstinence rates at end-of-treatment were generally slightly higher for FTF-CBT compared with TV-CBT, but differences were not statistically significant. FTF-CBT patients also experienced significantly greater reductions in eating disordered cognitions and interview-assessed depression. However, the differences overall were few in number and of marginal clinical significance.
Conclusions
CBT for BN delivered via telemedicine was both acceptable to participants and roughly equivalent in outcome to therapy delivered in person.
Keywords: Bulimia nervosa, Cognitive–behavioral therapy, Telemedicine
Introduction
There is general consensus among researchers in the field of eating disorders that at this time cognitive–behavioral therapy (CBT) is the treatment of choice for individuals with bulimia nervosa (BN) (Mitchell, Agras, & Wonderlich, 2007). Although undoubtedly not the final stage in the development of effective therapies for BN, CBT remains the most widely studied and the best-supported treatment for BN.
Despite this finding there is considerable evidence that most patients who are treated for BN do not receive an empirically supported psychotherapy for their condition (Arnow, 1999). In a survey of psychologists, Mussell, Crosby, Knopke, Peterson, and Mitchell (2000) found that the vast majority of clinicians who said that at least 5% of their practice included eating disorders reported not using CBT as the treatment of choice, and only 21.7% reported any significant training experience in CBT for any condition. In another study (Crow, Mussell, Peterson, Knopke, & Mitchell, 1999), a cohort of 353 potential subjects who called an eating disorders research program requesting treatment were asked about prior therapy. Of these, 65.4% had received treatment before and 96.7% of these had received psychotherapy but only 6.9% reported that the treatment they received included even minimal elements of CBT. Most recently, von Ransom and Robinson (2006) found that clinicians who work with eating disorders reported that they prefered to tailor their treatment to the patient rather than choose an approach based on the level of empirical support. Therefore, although CBT may be the treatment of choice for these patients, many therapists working with BN patients choose not to use it, and do not know how to deliver it. Furthermore, most patients who have been treated for BN have not received it.
A related problem is the lack of availability of empirically supported treatments for patients with BN and other forms of psychopathology in rural areas. This is particularly true in the region in which this study was conducted (e.g., North Dakota and Minnesota), where much of the population lives in smaller urban and rural settings. In attempting to identify ways to deliver therapies to this population, several possibilities exist. One would be to train therapists in these areas; however, this would be expensive and impractical and many therapists would not have the time or economic resources to undertake such training. Also, their skills would likely atrophy over time if they were not seeing a critical number of such patients. A second possibility would be to utilize a traveling therapist who would periodically go to various rural areas to provide treatment. However, this would typically be considered undesirable work and third party payors would not reimburse for travel time, resulting in a major financial disincentive. A third possibility, and the one we studied in this protocol, is to deliver therapy through new technologies such as telemedicine.
Two prior studies have examined the utility of telemedicine in treating psychiatric patients. A modest study by Nelson, Barnard, and Cain (2003) assigned a series of 28 depressed children to in-person therapy or telemedicine therapy and found no evidence of a difference in outcomes. A second, larger study by Ruskin et al. (2004) was reported in which a series of 119 depressed patients were randomized to in-person versus telemedicine-delivered therapy. The therapy delivered was supportive psychotherapy, psycho-education and medication management. Again, no significant differences were found in outcome and both approaches were helpful.
Although, several reports have detailed the use of psychotherapy via telemedicine (see for example, Frueh, Henderson, & Myrick, 2005; Cluver, Schuyler, Frueh, Brescia, & Arana, 2005; Griffiths, Blignault, & Yellowlees, 2006; Metropolitan Life Insurance Table, 1983; Passik et al., 2004; Shepherd et al., 2006; Ugarriza & Schmidt, 2006), to our knowledge there have been no studies testing telemedicine administration of an empirically supported manual-based psychotherapy for a psychiatric condition. In this research, we studied the relative efficacy and acceptability of a manual-based psychotherapy for BN, CBT, delivered in person by a therapist who traveled to the local community, compared with CBT delivered via telemedicine wherein the treated subject never actually met the therapist in person.
Method
Participants
This study was conducted at nine regions in eastern North Dakota and northwestern Minnesota (which adjoins North Dakota to the east). Participants were recruited in waves through mailings to local physicians and psychologists and through advertisements in the media.
Recruitment took place between October 1999 and September 2003. This study was approved by institutional review boards at the University of North Dakota (Grand Forks, North Dakota) and MeritCare Health System (Fargo, North Dakota). Written informed consent was obtained from all participants.
Participants were eligible for this study if they were at least 18 years of age, met DSM-IV criteria for BN (purging or non-purging subtype) or eating disorder-not otherwise specified (EDNOS) with one of the following: (1) DSM-IV criteria for BN except binge eating/purging at a minimum frequency of once per week; (2) DSM-IV criteria for BN with only subjective binge eating episodes.
Participants were ineligible for the study if their body weight was less than 85% of ideal weight (Metropolitan Life Insurance Table, 1983), if they received a change in prescribed psychotropic medication in the previous 6 weeks, had ever received eight or more sessions of CBT, abused alcohol or drugs as defined by DSM-IV in the previous 6 months or were dependent in the previous 1 month, were pregnant, had a significant active medical illness that would jeopardize safe study participation (e.g., type I diabetes mellitus), had a significant risk of suicide as determined by a trained assessor, were actively psychotic, or had a current or past DSM-IV diagnosis of schizophrenia or bipolar disorder.
Interventions
Cognitive–behavioral therapy
The therapy used in this study was the manual-based CBT developed by Fairburn and colleagues (Fairburn & Cooper, 1993; Fairburn, Kirl, O'Connor, & Cooper, 1986). This therapy has been used in a variety of trials including two large multi-center studies in the United States, one funded by the National Institute of Mental Health (Agras, Walsh, Fairburn, Wilson, & Kraemer, 2000) and one funded by the McKnight Foundation (Mitchell et al., 2002). The therapy consisted of 20 sessions delivered over a 16 weeks period. TV-CBT was delivered using a telemedicine system linking a regional healthcare system facility using T1 lines. Subjects interacted with the therapist only through telemedicine. Units were placed so as to mimic the interpersonal distance and height equality used in face-to-face (FTF) therapy. Rooms at distal sites were chosen for their privacy and lack of excessive noise.
Therapists and assessors
CBT was delivered by six doctoral-level psychologists with training and prior experience in delivering therapy with this manual. Training consisted of coursework, readings and supervised practice cases. All therapists treated both FTF-CBT and TV-CBT patients. Assessments were conduct by four masters or doctoral-level individuals all of whom had used the assessment instruments in previous studies. Weekly separate supervisory sessions were held with assessors and therapists and monitoring tapes were discussed.
Treatment fidelity
All therapy sessions were audiotaped. Sessions tapes were evaluated by the PI and feedback was provided to the therapists. In therapy supervision, each patient's progress was reviewed and therapists’ adherence to the treatment protocol was discussed. A random sample of patients’ tapes were audited and scored by alternative therapists. Detailed feedback on all tapes was provided to the PI and the therapists. The results of the therapy tape auditing and the process measures will be reported separately, and treatment fidelity was high.
Assessments
Individuals requesting information about the study called a toll-free number at the research center (the Neuropsychiatric Research Institute in Fargo) where they were given additional information about the study, screened via phone to see if they were likely to meet eligibility criteria, and scheduled for an informational meeting to be held in their geographic area within the next few weeks. Project staff, including one of the investigators and a research coordinator, would then travel to that site to hold an evening informational meeting. Participants were seen individually to obtain informed consent and were then scheduled to complete self-report measures and meet with an assessor, who would travel to that site to administer interviews.
Eligibility for the study in terms of eating disorder diagnosis was determined using the Eating Disorder Examination (EDE) (Fairburn & Cooper, 1993). The EDE is an investigator-administered interview used to determine DSM-IV eating disorder diagnosis and assess current eating disorder symptoms. The EDE provides frequency measures of binge eating and compensatory behaviors, which were used as the primary measures of treatment outcome. The EDE also contains four subscales (Dietary Restraint, Eating Concerns, Shape Concerns and Weight Concerns) associated with core psychopathology of eating disorders. The validity and reliability of EDE have been well documented and the instrument has been used extensively in treatment outcome studies of BN. The EDE was administered at baseline, end of treatment, and at 3- and 12-month follow-ups. Subjects also rated the suitability of the therapy and the likelihood that they would be successful in the assigned therapy after three sessions.
Comorbid DSM-IV Axis I disorders were determined using the Structured Clinical Interview for DSM-IV, Patient Edition (SCID-P) (First, Spitzer, Gibbon, & Williams, 1995). An addendum was added to the SCID-P to assess impulse control disorders. Standard questions were added to assess suicidality. The SCID-P was administered only at baseline.
A self-assessment battery was administered at baseline, end-of-treatment, and 3- and 12-month follow-ups. This battery included the Medical Outcomes Study Short-Form 36 (SF-36) (Ware, Gandek, & The IQOLA Project Group, 1994) to measure social functioning, the Rosenberg Self-Esteem (RSE) scale (Rosenberg, 1965) to measure self-esteem, and the Hamilton Rating Scale for Depression (HAM-D) (Hamilton, 1960). The Beck Depression Inventory (BDI) (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961) and a Binge-Purge Recall form were completed bi-weekly during treatment and at 3- and 12-month follow-ups. Subjects also rated the suitability of the therapy and the likelihood that they would be successful in the assigned therapy after three sessions.
Data were obtained on other psychiatric treatments received at the 3- and 12-month follow-up assessments using the McKnight Longitudinal Follow-up for Eating Disorders Interview (M-FED), an instrument used in several multi-center BN treatment and longitudinal studies (see for example, Crow, Agras, Halmi, Mitchell, & Kraemer, 2002; Mitchell et al., 2002).
The Working Alliance Inventory (WAI) (Horvath, 1982; Horvath & Greenberg, 1989) was used to study the therapeutic relationship. The WAI was completed by both participant (WAI-C) and therapist (WAI-T) at weeks 2, 8 and 16 (end-of-treatment).
The Hill Process Rating System (Hill, 1978, 1986, 1989, 1992) was used to assess treatment integrity and process. The HPRS contains measures of overt and covert behavior variables. The WAI data and the HPRS data will be the subject of a separate report.
Randomization
Participants were randomized to receive CBT in person (FTF-CBT) or via telemedicine (TV-CBT). The randomization sequence was generated by an independent statistician. Randomization was stratified by eating disorder diagnosis (BN vs. eating disorder-not otherwise specified) and antidepressant medication history (never/previous vs. current) to achieve balance on these variables, resulting in four allocation strata. Within each stratum, randomization was performed in blocks of four to control for potential changes in participant characteristics or study conduct (e.g., personnel changes) over time. Treatment assignment codes were concealed from study personnel until time of randomization and assessors were blinded to therapy administration technique throughout, although this was at times difficult to achieve because of statements made about this therapy when being assessed.
Statistical analysis
Power calculations for this study were based upon the methods described by Hedeker and colleagues (Hedeker, Gibbons, & Waternaux, 1999) for two-group longitudinal designs with attrition. Based upon a two-tailed α of .05 and an attrition rate of 15% during therapy and 10% at follow-up, a randomized sample size of 65 per group (130 total) would provide a power of .80 to detect a difference of .50 standard deviations between FTF-CBT and TV-CBT in binge eating and purging frequencies (Hedeker et al., 1999).
The proportion of participants completing EDE assessments at end-of-treatment, 3- and 12-month follow-ups were compared between treatment conditions using Fisher's Exact test. Treatment groups were compared at baseline on demographic and clinical characteristics using Fisher's Exact test for dichotomous variables, independent samples t-tests for symmetrically distributed continuous measures, and Mann–Whitney non-parametric tests for binge eating and purging frequencies.
All primary analyses were based upon intention-to-treat and were conducted using SPSS for Windows Version 15.0 (SPSS Inc., Chicago, Illinois) or SAS Version 8.0 (SAS Institute, Cary, North Carolina). Primary outcome variables were abstinence rates from binge eating and purging and binge-purge episode frequencies as determined from the EDE at end-of-treatment and 3- and 12-month follow-ups. Treatment groups were compared on rates of abstinence from objective binge eating, purging, and combined binge eating/purging at end-of-treatment, 3- and 12-month follow-up using Fisher's Exact test. Mixed-effected linear regression models (Hedeker, Gibbons, & Waternaux, 2006) were used to compare FTF-CBT and TV-CBT participants on binge eating and purging episode frequencies at end-of-treatment, and 3- and 12-month follow-up controlling for baseline levels, with assessment points coded as class variables to allow post-hoc comparisons between groups at each assessment. Analyses were performed on log-transformed frequencies due to positive skew, with raw (i.e., untransformed) means and standard deviations reported in tables. Comparisons between groups were based upon the main effect for group with a two-tailed α of .05. Post-hoc comparisons between groups at specific time points were based upon a two-tailed Bonferroni-corrected α of .017 (.05/3).
Secondary measures of outcome included EDE scale scores, SF-36, RSE, and HAM-D were analyzed with mixed effects regression models comparable to those described above. Analyses for BDI and binge/purge frequencies from the Binge-Purge Recall were analyzed with a mixed effects curvilinear trend model (Hedeker et al., 2006) controlling for baseline assessment, which included a random intercept and linear and quadratic trend components. This model allowed for the comparison between FTF-CBT and TV-CBT both in overall level and trajectories over time.
Results
Study flow
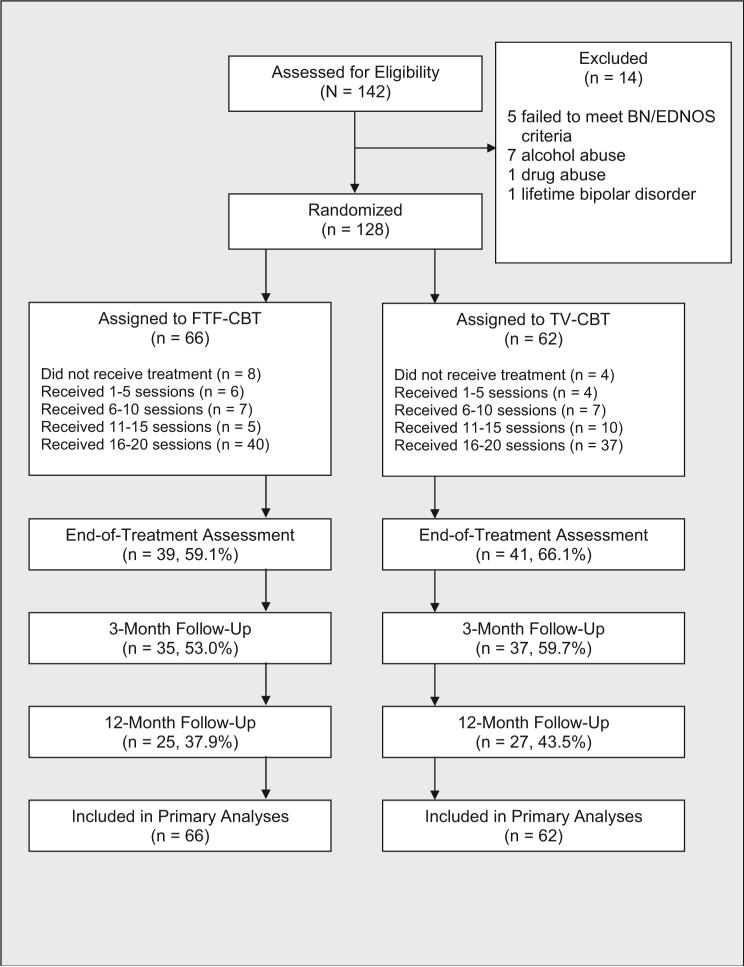
Fig. 1 presents the participant flow through the study. The proportion of participants completing EDE assessments did not differ between TV-CBT and FTF-CBT at end of treatment (Fisher's Exact p .467), 3-month follow-up (Fisher's Exact p = .480), or 12-month follow-up (Fisher's Exact p = .590).
Fig. 1.
Flowchart of study participants.
Participant characteristics at baseline
Participants in the treatment groups were similar in baseline sociodemographic and clinical characteristics (Table 1). Most participants were female and Caucasian, with an average age in the late 20's. The only significantly difference at baseline between treatment groups was in terms of current mood disorder, where 36% of TV-CBT participants met criteria compared with only 20% of FTF-CBT participants (Fisher's Exact p .05). A minority of participants reported laxative (n = 31, 24.2%) or diuretic use (n = 10, 7.8%) at baseline.
Table 1.
Baseline demographic and clinical characteristics for participants receiving FTF-CBT and TV-CBT
| Characteristic | Treatment group |
|||
|---|---|---|---|---|
| FTF-CBT (n = 66) |
TV-CBT (n = 62) |
|||
| n | % | n | % | |
| Current diagnosis | ||||
| Bulimia nervosa | 38 | 57.6 | 33 | 53.2 |
| Eating disorder not otherwise specified | 28 | 42.4 | 29 | 46.8 |
| Comorbid disorders | ||||
| Lifetime mood disorder | 45 | 68.2 | 45 | 72.6 |
| Current mood disordera | 13 | 19.7 | 22 | 35.5 |
| Lifetime anxiety disorder | 34 | 51.5 | 28 | 45.2 |
| Current anxiety disorder | 22 | 33.3 | 19 | 30.6 |
| Lifetime substance abuse/dependence | 12 | 18.2 | 17 | 27.4 |
| Current anti-depressant medication | 21 | 31.8 | 26 | 41.9 |
| Female | 64 | 97.0 | 62 | 100 |
| Caucasian | 62 | 93.9 | 61 | 98.4 |
| Post high school education | 55 | 83.3 | 56 | 90.3 |
| Mean |
SD |
Mean |
SD |
|
| Age | 29.6 | 10.9 | 28.4 | 10.4 |
| Body mass index (kg/m2) | 23.3 | 5.0 | 23.5 | 5.4 |
| Objective binge episodes previous 28 daysb | 21.9 | 27.3 | 19.1 | 24.7 |
| Vomiting episodes previous 28 daysc | 31.3 | 34.3 | 28.5 | 28.3 |
TV-CBT > FTF-CBT: Fisher's Exact p = .050.
Binge eating episode frequency reported as “too great to calculate” (n = 1) recoded to maximum reported value (132).
Vomiting episode frequency reported as “too great to calculate” (n = 3) recoded to maximum reported value (132).
Treatment exposure
A participant was considered to have completed a treatment session if they participated in therapy for at least 30 min. The average length of completed sessions was 50.5 min (SD = 7.4). The range of completed treatment sessions for FTF-CBT and TV-CBT participants is presented in Fig. 1. The mean number of completed sessions for FTF-CBT participants was 13.4 (SD = 7.1) compared with 14.2 (SD = 6.0) for TVCBT participants (t = .68; df = 126; p = .495).
Primary outcomes
Abstinence
Abstinence rates for objective binge eating, purging (vomiting, laxative abuse, and diuretic abuse), and combined objective binge eating and purging based upon the EDE interview are presented in Table 2. Abstinence was defined as none of these behaviors reported in the previous 28 days. Abstinence rates were determined in three different ways to allow comparisons to previous reports: (1) intention-to-treat based upon last observation carried forward (LOCF) replaces missing observations with the last valid observation for that participant; (2) intention-to-treat based upon baseline observation carried forward (BOCF) replaces missing observations with the baseline assessment for that participant (see for example, Agras et al., 2000); (3) completer analysis calculates rates of remission using only the valid observations for a given assessment (see for example, Bakke, Mitchell, Wonderlich, & Erickson, 2001).
Table 2.
Primary outcomes: abstinence rates and binge eating and purging rates by group from EDE interview
| Outcome variable | Treatment group |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FTF-CBT |
TV-CBT |
|||||||||||||||
| Baseline (n = 66) |
End of Tx (n = 39) |
3-month FU (n = 35) |
12-month FU (n = 25) |
Baseline (n = 62) |
End of Tx (n = 41) |
3-month FU (n = 37) |
12-month FU (n = 27) |
|||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | n | % | n | % | |
| Abstinence: LOCF | ||||||||||||||||
| OBE | 10 | 15.2 | 33 | 50.0 | 33 | 50.0 | 35 | 53.0 | 17 | 27.4 | 31 | 50.0 | 30 | 48.4 | 29 | 46.8 |
| Purginga | 6 | 9.1 | 24 | 36.4 | 22 | 33.3 | 23 | 34.8 | 4 | 6.5 | 19 | 30.6 | 14 | 22.6 | 16 | 25.8 |
| OBE and Purginga | 1 | 1.5 | 19 | 28.8 | 17 | 25.8 | 19 | 28.8 | 2 | 3.2 | 17 | 27.4 | 13 | 21.0 | 14 | 22.6 |
| Abstinence: BOCF | ||||||||||||||||
| OBE | 10 | 15.2 | 33 | 50.0 | 29 | 43.9 | 26 | 39.4 | 17 | 27.4 | 31 | 50.0 | 28 | 45.2 | 26 | 41.9 |
| Purginga | 6 | 9.1 | 24 | 36.4 | 19 | 28.8 | 17 | 25.8 | 4 | 6.5 | 19 | 30.6 | 14 | 22.6 | 16 | 25.8 |
| OBE & Purginga | 1 | 1.5 | 19 | 28.8 | 14 | 21.2 | 13 | 19.7 | 2 | 3.2 | 17 | 27.4 | 13 | 21.0 | 13 | 21.0 |
| Abstinence: completer | ||||||||||||||||
| OBE | 10 | 15.2 | 27 | 69.2 | 23 | 65.7 | 18 | 72.0 | 17 | 27.4 | 23 | 56.1 | 19 | 51.4 | 13 | 48.1 |
| Purginga | 6 | 9.1 | 21 | 53.8 | 17 | 48.6 | 14 | 56.0 | 4 | 6.5 | 17 | 41.5 | 12 | 32.4 | 14 | 50.0 |
| OBE and Purginga | 1 | 1.5 | 18 | 46.2 | 13 | 37.1 | 12 | 48.0 | 2 | 3.2 | 15 | 36.5 | 11 | 29.7 | 11 | 40.7 |
| Mean |
SD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
Mean |
SD |
|
| OBE episodes | 21.9 | 27.3 | 3.7 | 11.2 | 5.1 | 11.5 | 6.6 | 14.9 | 19.1 | 24.7 | 6.2 | 12.3 | 6.5 | 12.3 | 11.8 | 21.8 |
| Purging episodes | 35.6 | 34.1 | 5.6 | 12.5 | 8.7 | 16.5 | 8.2 | 17.8 | 36.8 | 34.7 | 11.1 | 19.0 | 10.7 | 17.9 | 19.4 | 34.0 |
Abstinence: no behaviors reported in previous 28 days based upon EDE interview. OBE: objective binge-eating episode; LOCF: last observation carried forward; BOCF: baseline observation carried forward.
Purging is defined as vomiting, laxative abuse, and diuretic abuse.
Abstinence rates from objective binge eating, purging, and combined binge eating/purging were generally slightly higher for FTF-CBT (with the exception of OBE based upon BOCF at 3- and 12-month follow-ups and OBE+Purging based upon BOCF at 12-month follow-up) compared with TV-CBT. However, none of these differences in abstinence rates approached statistical significance, regardless of how abstinence was calculated.
Binge eating and purging frequencies
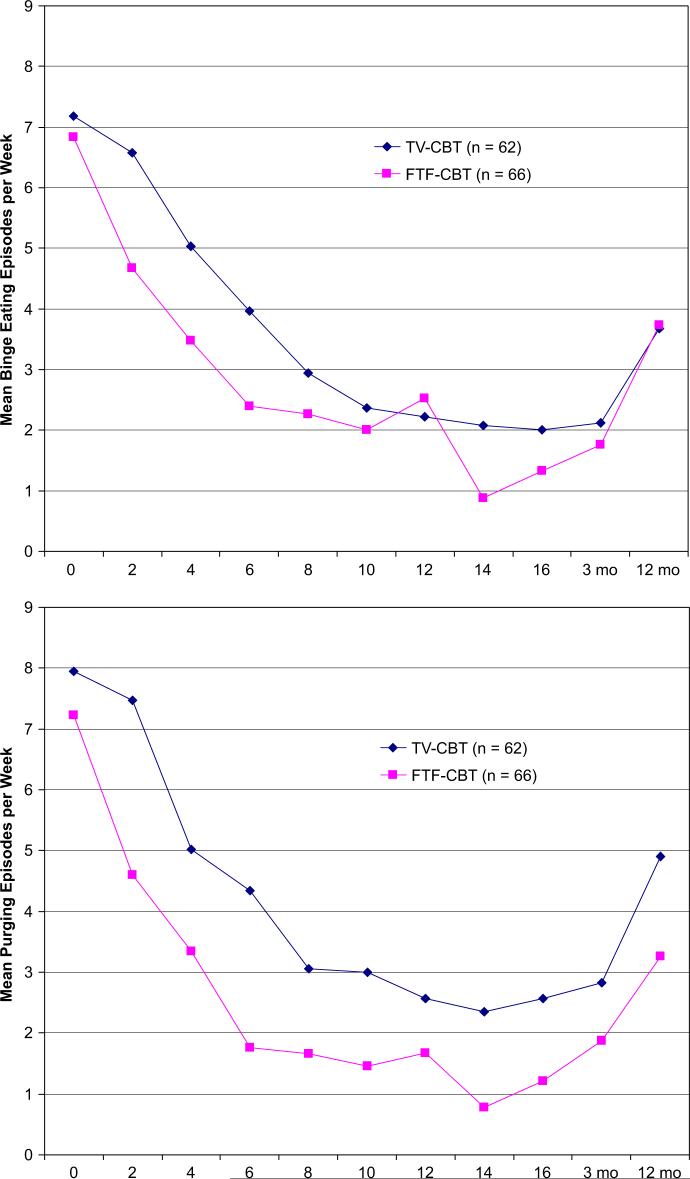
Significant differences were found between FTF-CBT and TV-CBT on the frequency of binge eating episodes (F = 6.76; df = 1, 79; p = .011) (see Table 2). Fig. 2 shows changes in binge eating and purging frequencies over time. Of note, response in the FTF-CBT group appear to occur rapidly, while response in the TV-CBT group appear delayed. Post-hoc comparisons revealed that purging frequency at the 12-month follow-up was significantly lower for the FTF-CBT group (t = 2.59; df = 118; p = .011). No differences were found between groups in the frequency of binge eating episodes (F = 2.66; df = 1, 79; p = .107). There was evidence of some relapse/deterioration between 3 and 12 months follow-up. However, FTF-CBT participants report significantly lower levels (but comparable trajectories) for both binge eating (F = 9.10; df = 1, 113; p = .003) and purging (F = 7.79; df = 1, 113; p = .006). While binge eating rates between FTF-CBT and TV-CBT participants were comparable at 3- and 12-month follow-up, differences in purging frequencies between groups at follow-up assessment were maintained.
Fig. 2.
Binge eating and purging recall by group.
Secondary outcomes
Table 3 presents means and standard deviations of secondary outcomes across assessment times by group. No differences between groups were found for EDE Restraint and Weight Concern scales, Rosenberg Self-Esteem, or SF-36 scores. However, FTF-CBT participants reported significantly greater reductions from baseline in EDE Eating Concerns (F = 6.5; df = 1, 79; p = .012), with significant post-hoc differences at 3-month follow-up (t = 3.09, df = 118, p = .003). There was also a significant group difference in EDE Shape Concerns (F = 4.66, df = 1, 79; p = .030), with significant post-hoc differences at 12-month follow-up. The FTF-CBT also resulted in greater reductions in Ham-D scores (F = 4.53, df = 1, 72, p = .037, with significant post-hoc differences between groups at end-of-treatment (t = 4.35, df = 105, p = .008).
Table 3.
Secondary outcomes measures by group
| Outcome variable | Treatment group |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FTF-CBT |
TV-CBT |
|||||||||||||||
| Baseline (n = 66) |
End of Tx (n = 39) |
3-month FU (n = 35) |
12-month FU (n = 25) |
Baseline (n = 62) |
End of Tx (n = 41) |
3-month FU (n = 37) |
12-month FU (n = 27) |
|||||||||
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | |
| EDE | ||||||||||||||||
| Restraint | 3.5 | 1.2 | 1.5 | 1.5 | 1.5 | 1.4 | 1.6 | 1.5 | 3.4 | 1.4 | 1.7 | 1.5 | 1.7 | 1.6 | 1.8 | 1.5 |
| Eating concerns | 2.1 | 1.4 | .7 | 1.0 | .4 | .5 | .6 | 1.0 | 1.7 | 1.3 | .8 | 1.0 | .9 | 1.2 | .9 | 1.3 |
| Shape concerns | 3.8 | 1.3 | 2.3 | 1.5 | 2.1 | 1.3 | 1.8 | 1.2 | 3.5 | 1.4 | 2.3 | 1.5 | 2.2 | 1.5 | 2.1 | 1.6 |
| Weight concerns | 3.5 | 1.3 | 2.1 | 1.6 | 2.1 | 1.3 | 1.8 | 1.2 | 3.4 | 1.3 | 1.9 | 1.3 | 2.2 | 1.4 | 2.1 | 1.5 |
| Hamilton depression | 15.7 | 9.2 | 7.0 | 7.4 | 8.6 | 8.1 | 9.1 | 9.3 | 14.5 | 9.0 | 10.6 | 8.7 | 9.4 | 8.4 | 8.7 | 7.9 |
| Rosenberg self-esteem | 3.6 | 2.0 | 2.0 | 1.9 | 2.1 | 2.0 | 2.0 | 2.0 | 3.6 | 1.9 | 2.2 | 2.0 | 1.7 | 2.0 | 1.8 | 2.0 |
| SF-36 | ||||||||||||||||
| Physical component | 54.6 | 8.0 | 56.2 | 5.7 | 57.1 | 4.9 | 55.4 | 5.3 | 53.4 | 9.1 | 54.1 | 7.9 | 52.7 | 9.0 | 53.6 | 9.3 |
| Mental component | 34.2 | 12.7 | 45.5 | 11.9 | 43.9 | 13.6 | 42.7 | 12.8 | 35.4 | 14.2 | 42.9 | 12.6 | 44.0 | 13.6 | 43.5 | 14.4 |
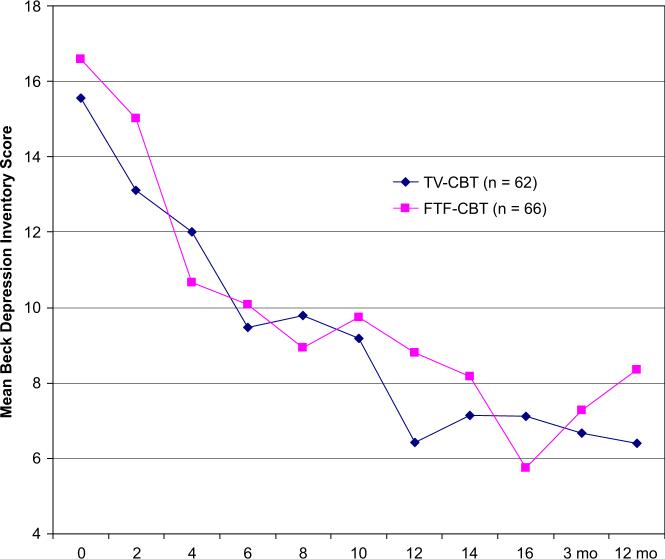
No differences were found between groups on level or patter of change in BDI scores (Fig. 3). The self-rated suitability of treatment and likelihood of response were not different between groups.
Fig. 3.
Beck Depression Inventory scores by group.
Discussion
This randomized trial, comparing CBT for BN delivered via telemedicine versus in person, demonstrated that telemedicine-delivered CBT was both acceptable to patients and roughly equivalent in outcome to therapy delivered in person. The strengths of this study include a relatively large sample size, careful training and supervision of assessors and therapists, the use of a manual-based approach for psychotherapy and the broadening of inclusion criteria to include subthreshhold cases that are frequently seen in clinical practice.
One finding in this study was the substantial drop-out rate, which is unfortunately common in BN treatment trials but was particularly important here. This higher than anticipated drop-out rate likely reduced the statistical power of this study, thereby reducing our ability to detect differences in outcome between TV-CBT and FTF-CBT. In this trial, the drop-out rate may be attributable in part to the nature of the therapy delivery. First therapists in FTF-CBT were traveling to distal sites at preset times and telemedicine visits were at times difficult to arrange; consequently there was very little flexibility in scheduling. If scheduling conflicts arose sessions could not always be rescheduled. The fallback was usually to do a brief therapy session by phone. Second, there were technical problems at times, which also impacted adversely on therapy involving the telemedicine equipment. Third, weather conditions during winter in the upper Midwest were problematic and at times sessions would have to be canceled because it was deemed unsafe for the research personnel to travel across long distances. None-the-less the abstinence rates at end-of-treatment were very similar to the rates in two recent large multi-center trials using CBT (17, 18: ITT abstinence rate McKnight trial = 31%, NIMH trial = 29%, this trial = 28%; completer abstinence rates: McKnight trial = 41%; NIMH trial = 40%; this trial = 41%).
Anecdotally, the therapists in the study were more concerned about doing therapy via telemedicine versus in person than the subjects early on in the study. However, in general they noted that after a few sessions with each patient this did not seem to be a particularly important issue.
The study also demonstrated a number of logistical issues and practical considerations that need to be addressed when using telemedicine to deliver psychotherapy. We have discussed some of these in detail in prior publications (Bakke et al., 2001; Mitchell, Swan-Kremeier, & Myers, 2003). First, in terms of the use of the equipment, lighting must be addressed, as well as monitor and chair placement so as not to have the intervention seem dominated by one party, or overly distant. Also, the rooms where telemedicine equipment is used at distal sites are often not optimal for psychotherapy, and not uncommonly are conference rooms. For this reason some of the rooms used were less than optimal. Another issue to consider is that some insurance companies will now reimburse for telemedicine-delivered psychotherapy and other psychiatric therapies in some states, but not in others. This remains in transition. The problem of therapy homework can usually be solved by simply faxing materials from the site to the center. Of particular concern are issues related to suicidality, in that the therapist may discover that the patient at the distal site is in need of some emergency intervention. In this particular study, we dealt with this by always having a research coordinator on site trained to assist the therapist in handling these emergencies; however, if the system were used in routine clinical care, some sort of emergency backup would need to be in place.
The results of the study suggest that a manual-based form of psychotherapy for a specific psychiatric disorder can be effectively delivered via telemedicine. We believe this has implications for delivery of other manual-based, empirically supported psychotherapies for other psychiatric conditions, and that this may help to address the lack of dissemination of such therapies, particularly to rural areas.
Footnotes
Funding for this study was provided by a grant funded jointly by the National Institute of Mental Health and the National Institute of Diabetes and Digestive and Kidney Diseases (R01-MHDK-58820), the National Institute of Mental Health (KO2 MH65919) and the Neuropsychiatric Research Institute.
References
- Agras WS, Walsh T, Fairburn CB, Wilson GT, Kraemer HC. A multicenter comparison of cognitive–behavioral therapy and interpersonal psychotherapy for bulimia nervosa. Archives of General Psychiatry. 2000;57:459–466. doi: 10.1001/archpsyc.57.5.459. [DOI] [PubMed] [Google Scholar]
- Arnow BA. Why are empirically supported treatments for bulimia nervosa underutilized and what can we do about it? Journal of Clinical Psychology. 1999;55:769–779. doi: 10.1002/(sici)1097-4679(199906)55:6<769::aid-jclp9>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- Bakke B, Mitchell JE, Wonderlich S, Erickson R. Administering cognitive–behavioral therapy for bulimia nervosa via telemedicine in rural settings. International Journal of Eating Disorders. 2001;30:454–457. doi: 10.1002/eat.1107. [DOI] [PubMed] [Google Scholar]
- Beck AT, Ward CM, Mendelson M, Mock JE, Erbaugh JK. An inventory for measuring depression. Archives of General Psychiatry. 1961;44:1210–1218. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Cluver JS, Schuyler D, Frueh BC, Brescia F, Arana GW. Remote pspychotherapy for terminally ill cancer patients. Journal of Telemedicine and Telecare. 2005;11:157–159. doi: 10.1258/1357633053688741. [DOI] [PubMed] [Google Scholar]
- Crow S, Agras S, Halmi K, Mitchell JE, Kraemer H. Full syndromal versus subthreshold anorexia nervosa, bulimia nervosa, and binge eating disorder: A multicenter study. International Journal of Eating Disorders. 2002;232:309–318. doi: 10.1002/eat.10088. [DOI] [PubMed] [Google Scholar]
- Crow S, Mussell MP, Peterson C, Knopke A, Mitchell J. Prior treatment received by patients with bulimia nervosa. International Journal of Eating Disorders. 1999;25:39–44. doi: 10.1002/(sici)1098-108x(199901)25:1<39::aid-eat5>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The eating disorders examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment and treatment. 12th ed Guilford Press; New York: 1993. pp. 317–360. [Google Scholar]
- Fairburn CG, Kirl H, O'Connor M, Cooper PJ. A comparison of two psychological treatments for bulimia nervosa. Behaviour Research and Therapy. 1986;24:629–643. doi: 10.1016/0005-7967(86)90058-6. [DOI] [PubMed] [Google Scholar]
- First MG, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders—Patient edition (SCID ¼ I/P, version 2) Biometrics Research Department; New York: 1995. [Google Scholar]
- Frueh BC, Henderson S, Myrick H. Telehealth service delivery for persons with alcoholism. Journal of Telemedicine and Telecare. 2005;11:372–375. doi: 10.1258/135763305774472060. [DOI] [PubMed] [Google Scholar]
- Griffiths L, Blignault I, Yellowlees P. Telemedicine as a means of delivering cognitive–behavioral therapy to rural and remote mental health clients. Journal of Telemedicine and Telecare. 2006;12:136–140. doi: 10.1258/135763306776738567. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology Neurosurgery and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedeker D, Gibbons RD, Waternaux C. Sample size estimation for longitudinal designs with attrition: Comparing time-related contrasts between two groups. Journal of Educational and Behavioral Statistics. 1999;24:70–93. [Google Scholar]
- Hedeker D, Gibbons RD, Waternaux C. Sample size estimation for longitudinal designs with attrition: Comparing time-related contrasts between two groups. Journal of Educational and Behavioral Statistics. 2006;24:70–93. [Google Scholar]
- Hill CE. Development of a counselor verbal response category system. Journal of Counseling Psychology. 1978;25:461–468. [Google Scholar]
- Hill CE. An overview of the Hill counselor and client verbal response modes category systems. In: Greenberg LS, Pinsof WM, editors. The psychotherapeutic process: A research handbook. Guilford Press; New York: 1986. pp. 131–160. [Google Scholar]
- Hill CE. In: Psychologist techniques and client outcomes: Eight cases of brief psychotherapy. Hill CE, editor. Sage; Newbury Park, CA: 1989. [Google Scholar]
- Hill CE. An overview of four measures developed to test the Hill process model: Psychologist intentions, psychologist response modes, client reactions, and client behaviors. Journal of Counseling and Development. 1992;70:728–739. [Google Scholar]
- Horvath AO. Working Alliance Inventory (revised). Instructional Psychology Research Group. 1. Vol. 82. Simon Fraser University; Burnaby, British Columbia: 1982. [Google Scholar]
- Horvath AO, Greenberg LS. Development and validation of the working alliance inventory. Journal of Counseling Psychology. 1989;36:223–233. [Google Scholar]
- Metropolitan Life Insurance Table Height and weight tables. Statistical Bulletin. 1983;64:3–9. [PubMed] [Google Scholar]
- Mitchell JE, Agras S, Wonderlich S. Treatment of bulimia nervosa. Where are we and where are we going? International Journal of Eating Disorders. 2007;40:95–101. doi: 10.1002/eat.20343. [DOI] [PubMed] [Google Scholar]
- Mitchell JE, Halmi K, Wilson G, Agras S, Kraemer H, Crow S. A randomized secondary treatment study of women with bulimia nervosa who fail to respond to CBT. International Journal of Eating Disorders. 2002;32:271. doi: 10.1002/eat.10092. [DOI] [PubMed] [Google Scholar]
- Mitchell JE, Swan-Kremeier L, Myers T. Delivering psychotherapy to patients with bulimia nervosa via telemedicine. Eating Disorders Review. 2003;11:13–22. [Google Scholar]
- Mussell MP, Crosby RD, Knopke AJ, Peterson CB, Mitchell JE. Utilization of empirically supported psychotherapy treatments for individuals with eating disorders: A survey of psychologists. International Journal of Eating Disorders. 2000;22:230–237. doi: 10.1002/(sici)1098-108x(200003)27:2<230::aid-eat11>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- Nelson El., Barnard M, Cain S. Treating childhood depression over videoconferencing. Telemedicine Journal and E-Health. 2003;9:49–55. doi: 10.1089/153056203763317648. [DOI] [PubMed] [Google Scholar]
- Passik SD, Kirsh KL, Leibee S, Kaplan LS, Love C, Napier E, et al. A feasibility study of dignity psychotherapy delivered via telemedicine. Palliat Support Care. 2004;2:149–155. doi: 10.1017/s1478951504040209. [DOI] [PubMed] [Google Scholar]
- Rosenberg J. Society and the adolescent self-image. Princeton University Press; Princeton, NJ: 1965. [Google Scholar]
- Ruskin PE, Silver-Aylaian M, Kling MA, Reed SA, Bradham DD, Hebel JR, et al. Treatment outcomes in depression: Comparison of remote treatment through telepsychiatry to in-person treatment. American Journal of Psychiatry. 2004;161:1471–1476. doi: 10.1176/appi.ajp.161.8.1471. [DOI] [PubMed] [Google Scholar]
- Shepherd L, Goldstein D, Whitford H, Thewes B, Brummell V, Hicks M. The utility of videoconferencing to provide innovative delivery of psychological treatment for rural cancer patients: Results of a pilot study. Journal of Pain and Symptom Management. 2006;32:453–461. doi: 10.1016/j.jpainsymman.2006.05.018. [DOI] [PubMed] [Google Scholar]
- Ugarriza DN, Schmidt L. Telecare for women with postpartum depression. Journal of Psychosocial Nursing and Mental Health Services. 2006;44:37–45. doi: 10.3928/02793695-20060101-08. [DOI] [PubMed] [Google Scholar]
- von Ransom KM, Robinson KE. Who is providing what type of psychotherapy to eating disorder clients? A survey. International Journal of Eating Disorders. 2006;39:27–34. doi: 10.1002/eat.20201. [DOI] [PubMed] [Google Scholar]
- Ware JE, Gandek B, The IQOLA Project Group The SF-36 Health Survey: Development and use in mental health research and the IQOLA Project. International Journal of Mental Health. 1994;23:49–73. [Google Scholar]