Abstract
Purpose
To assess and predict changes in mental health service use as older youth leave the foster care system.
Methods
Participants were 325 19-year olds participating in a longitudinal study of older youth leaving the foster care system in Missouri. All were in the foster care system at age 17. Participants were interviewed nine times between their 17th and 19th birthdays using the Service Assessment for Children and Adolescents and a history calendar to improve recall of service history. Analyses included Cox proportional hazards regression to predict time to service stoppage and McNemar's test to assess difference in rates of service use between age 17 and 19.
Results
Mental health service use dropped dramatically across the study period for all services. Service rates dropped most steeply for youth who left the foster care system. Service use rates declined by roughly 60% from the month prior to leaving the foster care system to the month after leaving the system. Most young adults who stopped pharmacotherapy following discharge from foster care reported they did so of their own volition.
Conclusions
Practitioners should be aware of the possibility of patient-initiated mental health service discontinuation following exit from the foster care system and plan accordingly.
Keywords: adolescent-to-adult transition, mental health, medications
The transition from pediatric-to-adult service systems has been characterized as problematic in both general medical care1 2 and specialized mental health care3, yet few studies have tracked service use across this transition. This study uses a cohort of older youth from the foster care system to examine pediatric-to-adult mental health service use transitions. Older youth from the foster care system are of interest because of their high rates of mental disorder4 and mental health service use while in foster care5 and number of service and life changes expected as they leave the foster care system.
Few studies have examined changes in health service use over time as youth move into adulthood. A school-based study of youth depressed at onset of the study showed declining past year outpatient mental health treatment over time – 24% at age 13, 9% at age 18 and 3% at age 20.6 Two studies of youth from the foster care system showed declining use from 17 to 19. In one, psychotherapy rates halved if youth left foster care.7 In the other, in a state where all youth had to leave the foster care system by age 18, specialty mental health service use dropped from 47% to 21% from age 17 to age 19.8 None of these studies provided information on changes in specific types of mental health services beyond counseling and pharmacotherapy, nor did they examine reasons for service cessation. There are multiple reasons to anticipate that mental health service use declines as older youth leave the foster care system, including aging out of pediatric mental health services 2 3 and into an adult system with more stringent eligibility criteria,3 a lack of shared planning among pediatric and adult systems,3 loss of case managers, a shift in decision-making authority from an adult to the youth and loss of insurance coverage.2 By virtue of being in the foster care system, youth are eligible for Medicaid if they don't have other insurance coverage. While Congress has provided a mechanism to allow states to offer continued Medicaid coverage for older youth as they leave the foster care system, few states participate in the Medicaid option. No study has to date examined which of these reasons may account for potential service terminations during the transition to adulthood.
This study was designed to address several issues related to service change for a cohort of young people from the foster care system in Missouri, where young people can remain in the foster care system until age 21. They include changes in service use rates from 17 to 19, service continuity through transitions out of foster care, and questions of who paid for services once youth left the foster care system and who initiated service disruptions. We anticipated service declines for young people who left the foster care system, but not for those who stayed in it, and that foster care exit status, psychiatric history, attitudes toward service and knowledge of the service system would be associated with continued service use.
Patients and Methods
The study used a longitudinal cohort design, with older youth interviewed about their mental health service use every three months from age 17 to 19 (9 interviews).
Participants
Participants were 325 young adults interviewed at age 19 and who were enrolled in a longitudinal study of older youth from the foster care system. A prior paper discusses recruitment and eligibility criteria.5 Four hundred four young people, representing 90% of those eligible, were originally interviewed near their 17th birthdays, when all participants were in the legal custody of the Missouri Children's Division (MCD), the child welfare authority in Missouri. This paper uses results from the 325 youth who completed the age 19 interview, 80% of those originally enrolled in the study. Participants not retained were lost due to our inability to locate them (63 participants, 16%), dropout (7, 2%), incarceration (7, 2%), overseas military service (2, < 1%) and death prior to age 19 (1).
Procedures
Participants were interviewed by trained professional interviewers. Interviews one and nine were in-person. Interviews 2-8 were conducted over the phone when possible. Participants were interviewed using a structured interview protocol in conjunction with a history calendar9 to improve recall accuracy. Youth were paid $40 for the initial interview, $40 for the final interview and $20 each for interviews 2-8. The Washington University Human Subjects Committee approved all procedures in advance.
Measurement
Mental health service use
Mental health service use was assessed with portions of the Service Assessment for Children and Adolescents (SACA) and its accompanying medication schedule.10 11 While previous studies employed restricted definitions of service use, the SACA asks about lifetime, past year and current mental health service use across a variety of service venues. At each subsequent interview, we inquired about the continuation of old services and the initiation of new services. For discontinued psychotropic medications, youth were asked about reasons for termination and whose decision it was to stop the medication.
Service changes can be operationalized in a variety of ways. In this study we looked at service use by month over time and compared service receipt at age 17 and 19. We also, however, wanted a measure that captured continued service use across the months when young people left the foster care system, reasoning that service may be most valuable during a stressful transition. Therefore, we used monthly service use data to create a dichotomous indicator of continued service use through the transition months out of state custody. Because the participants varied in the length of time that they had been out of the system before the final interview, our definition differed somewhat by duration of time since system exit until the final interview. For example, youth who had been out of care for 6 months or longer by the age 19 interview were classified as having had continued service if they used the service in each of the first two months out of the foster care system and four of the first six months. Youth out of care 4 months at the final interview were classified as having had continued service if they used the service in each of the first two months and 3 of the 4 months out of care.
Left State Custody
In Missouri, older youth can be discharged from the foster care system without custody being transferred to another adult at age 17. Young people are eligible to stay in the foster care system until age 21, but most leave before that. Youth self-reported the month at which they were discharged from the legal custody of the Missouri Children's Division. In this paper, the terms “leaving custody” and “leaving the foster care system” are synonymous. At the time of the study, Missouri did not participate in the Medicaid option extending coverage to youth who left the foster care system to age 21.
Predictor variables
Several types of variables, each measured at the initial interview at age 17, were used as predictors of later service use. These included indications of psychiatric history, placement history, maltreatment history, attitudes toward mental health services, and knowledge of local mental health services. Lifetime history of major depressive episode, posttraumatic stress disorder, mania, attention deficit disorder and disruptive behavioral disorder (conduct or oppositional disorder) were assessed through use of the Diagnostic Interview Schedule-Version IV.12 Physical abuse and physical neglect histories were assessed with the Childhood Trauma Questionnaire.13 We assessed penetrative sexual abuse histories with an item from Russell.14 Attitudes toward seeking mental health services were measured by a modified and updated version of the Confidence In Mental Health Practitioner subscale from the Attitudes Toward Seeking Professional Psychological Help Scale.15 The internal consistency coefficient for the modified 9-item scale was .73. A measure of service knowledge was constructed for this study. It consisted of responses to three vignettes written to describe a person with severe psychiatric need. Youth were then asked, “What could you do to help?” Responses were written down verbatim and subsequently coded from (0) insists no help is needed to (5) knew the name of a specific provider and had a justification for why they chose that provider. Interviewers coded the responses after extensive training where 90% coding agreement was achieved among interviewers. These three items were summed to create an index of mental health service knowledge. Living situation was assessed at each interview and initially coded into one of 20 categories. This was reduced to four for analyses (with family, non-kin foster family, congregate care and living more independently).
Statistical Analyses
McNemar's test was used for significance testing of differences in service rates from age 17 to 19. Chi square analyses were used to assess differences in service use rates among those in and out of the foster care system at age 19. We examined predictors of service stoppage and continuity two ways. For those using an outpatient special mental health or psychotropic medication services at age 17, we used Cox proportional hazard models to examine predictors of number of months until first month without the service. This was done only for those who were using the service at age 17. We also examined predictors of service continuity using logistic regression and the dichotomized constructed service continuity measure for youth who had left the foster care system. Models were built through manual backwards elimination, with variables remaining in the model if they were associated with service outcomes at a level of .10.
Results
Multivariate logistic regression analyses to predict retention revealed that the following characteristics were associated with decreased odds of being retained in the study: being male (O.R.= .34, p<.001), having past year PTSD at initial interview (O.R.=.36, p=.025), having a history of juvenile detention by first interview (O.R.=.26, p=.016), and being released from the state's custody prior to age 19 (O.R.=.26, p<.0001). The resulting sample included 197 females (61%) and 192 youth of color (59%), most of whom were African American. The region contained few Latino or Asian youth in the foster care system.
Rates of Service Use
Table 1 shows the rates of reported current mental health service at age 17 and 19 for the 325 young adults interviewed at age 19. Service use decreased substantially for outpatient specialized mental health, residential treatment, and school based mental health services. In addition, at age 17, 50 older youth (15%) reported past year in-patient psychiatric hospitalizations. At age 19, this had decreased to 11 young adults (3%, McNemar statistic=28.70, df=1, p<.0001). At age 17, 6 older youth (2%) reported past year use of an emergency room for emotional or behavioral problems. At age 19, 3 young adults (1%) reported the same (significance testing not conducted due to low expected cell frequencies).
Table 1. Current use of mental health services at age 17 and 19.
| Age 17 | Age 19 | |||||
|---|---|---|---|---|---|---|
| n | % | n | % | McNemar Statistica | p | |
| Outpatient specialized service | 113 | 35% | 31 | 10% | 70.04 | <.0001 |
| Psychotropic medication | 115 | 35% | 43 | 13% | 60.27 | <.0001 |
| Residential treatment | 123 | 37% | 30 | 9% | 83.97 | <.0001 |
| School special help | 44 | 14% | 7 | 2% | 31.84 | <.0001 |
| Clergy for behavioral healthb | 9 | 3% | 3 | 1% | -- | -- |
| Family doctor for behavioral healthb | 9 | 3% | 3 | 1% | -- | -- |
degrees of freedom=1 for all analyses
significance testing not conducted due to low expected cell counts
Table 2 compares current mental health service use among 19-year olds who remained within, and who had been discharged from the foster care system. Rates of service use were substantially lower for those young adults who had left care for most service types.
Table 2. Rates of current mental health service use at age 19 by whether youth had left custody by age 19.
| In Custody age 19
(n=160) |
Left Custody by age 19
(n=165) |
|||||
|---|---|---|---|---|---|---|
| n | % | n | % | χ2a | p | |
| Outpatient specialized | 26 | 16% | 5 | 3% | 16.45 | <.0001 |
| Psychotropic medication | 34 | 21% | 9 | 5% | 17.65 | <.0001 |
| Residential treatment | 28 | 18% | 2 | 1% | 25.72 | <.0001 |
degrees of freedom=1 for all analyses
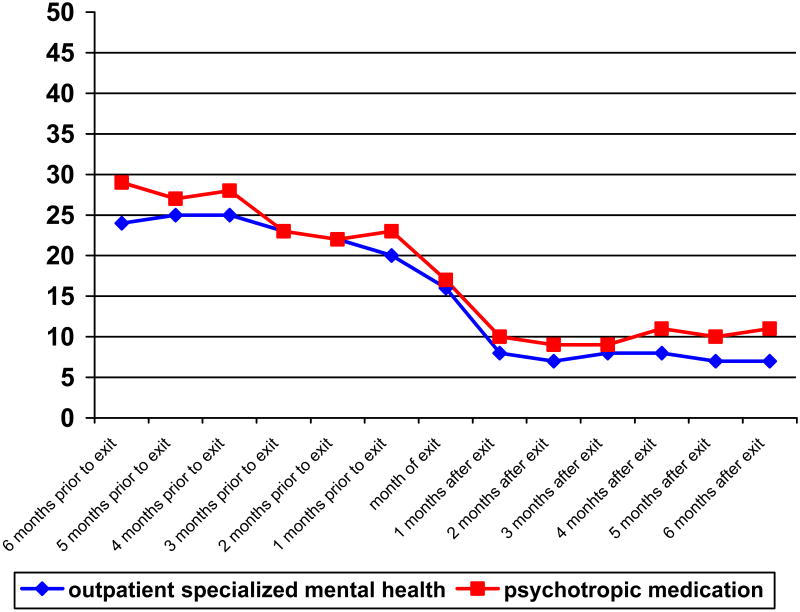
To demonstrate the decline in service use during the transition out of the foster care system, we graphed in Figure 1 the percentage of respondents in receipt of psychotropic medication and outpatient therapy from six months prior to system discharge to six months following discharge from the foster care system, for those who had been discharged from the foster care system prior to the final interview. This drop was most marked from the month prior to leaving the foster care system to the month after leaving the foster care system, when service use dropped by approximately 60%.
Figure 1.
Among youth who were discharged from the foster care system, the percentage receiving psychotropic medication and outpatient specialized service from six months prior to six months after discharge from foster care.
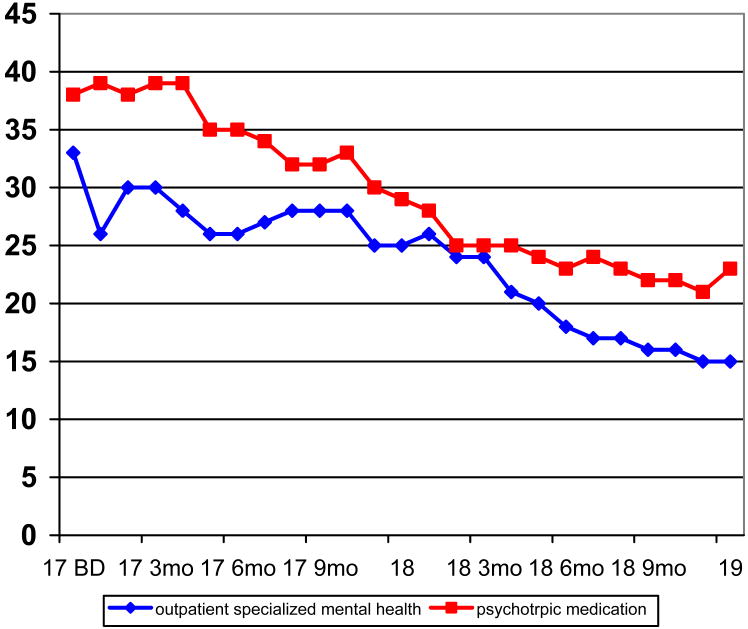
Although the decline was steepest at the time youth left the foster care system, service use declined throughout the study period for youth. This is demonstrated in Figure 2, which shows the receipt of psychotropic medication and outpatient therapy across the study period for young people who remained in the foster care system.
Figure 2.
Among youth who remained in the foster care system from age 17 to 19, the percentage who received outpatient specialized mental health services and psychotropic medication during this period.
Continued Service through the Transition Period
Only 10 of 94 (11%) young people who used an outpatient mental health specialty service at some point during the study and who left the foster care system before age 19 met the study's definition of continued service use across the transition period out of the foster care system. Only 13 of 70 (19%) young people who used psychotropic medications during the study period and had left the foster care system at least three months prior to the final interview met the study's definition of continued medication use across the transition period.
Who Paid for Services for Those Who Left the Foster Care System?
Twenty non-medication mental health services were recorded as having been received since youth were discharged from the foster care system and in the year prior to the age 19 interview. Of these 20 services, participants reported that 13 (65%) were paid by Medicaid, 1 (5%) was paid by private insurance, 1 (5%) was paid out-of-pocket and 5 (25%) services were not reimbursed.
Young adults who were using psychotropic medication were also asked who paid for the last prescription filled. Ten young adults who had left the foster care system were taking a total of 17 prescription psychotropic medications at the final interview. Of these 17 prescriptions, respondents said 8 (47%) were paid by Medicaid, 5 (29%) were paid out-of-pocket, 3 (18%) were paid by private insurance and 1 (6%) was paid by a family member.
Reasons for Service Termination
Table 3 shows the primary reasons the participants gave for each termination of psychopharmacology. Youth gave many reasons for stopping the use of medications. Many youth did not like being on medications or thought that they did not need psychotropic medications. Table 3 also shows the participants' answers to the question about who decided the medication should be stopped. For older youth in custody, the healthcare professional was reported to have made the decision to end psychotropic medication 60% of the time; for those not in custody, the health care professional was reported to have made the decision to halt the medication 31% of the time (χ2=23.42, df=1, p<.0001).
Table 3. Reasons for stopping psychotropic medications by custody status.
| In Custody at Time Medication Stopped | Out of Custody at Time Medication Stopped | |||
|---|---|---|---|---|
| n | % | n | % | |
| Who decided medication should end? | 274 medications stopped | 93 medications stopped | ||
| Health care professional | 165 | 60 | 29 | 31 |
| Young adult | 94 | 34 | 59 | 63 |
| Foster parent | 5 | 2 | 0 | 0 |
| Other | 8 | 3 | 5 | 5 |
| Don't Know | 3 | 1 | 0 | 0 |
| Missing | 1 | 0 | 0 | 0 |
| Reasons for Stopping Medication | 252 medications stopped | 97 medications stopped | ||
| Not working | 62 | 25 | 14 | 14 |
| Didn't like being on meds | 32 | 13 | 19 | 20 |
| Didn't need it | 45 | 18 | 11 | 11 |
| Side effects | 43 | 17 | 15 | 15 |
| Pregnant or nursing | 10 | 4 | 11 | 11 |
| Cost | 10 | 4 | 11 | 11 |
| Ran out | 15 | 6 | 5 | 5 |
| Didn't know where to get prescription filled | 6 | 2 | 0 | 0 |
| Other | 27 | 11 | 11 | 11 |
Predictors of Service Stoppage and Continuity
Table 4 shows the results of the multivariate Cox proportional hazard modeling of time to discontinuation of psychotropic medications for the 115 young people who were receiving psychotropic medications at age 17, with variables eliminated using manual backward elimination. The time at when youth left the foster care system was the strongest predictor of early medication stoppage. In addition, youth with a history of a disruptive behavioral disorder and youth of color were more likely to stop taking medications early and youth from congregate care and youth with a history of penetrative sexual abuse were more likely to continue using psychotropic medications for a longer time.
Table 4. Predictors of months until psychotropic medications stopped (n=115).
| Hazard Ratio | Lower CI | Upper CI | p | |||||
|---|---|---|---|---|---|---|---|---|
| Age 17 Predictor Variables | ||||||||
| History of Disruptive Behavioral Disorder | 1.57 | 1.01 | 2.45 | .046 | ||||
| In congregate care | 0.62 | 0.39 | 0.97 | .037 | ||||
| Youth of color | 1.76 | 1.11 | 2.78 | .016 | ||||
| History of penetrative sexual abuse | .56 | .34 | .91 | .020 | ||||
| Discharge Status | ||||||||
| Left care age 17 to 17 6 mos.a | 3.29 | 1.54 | 7.04 | .002 | ||||
| Left care age 17 6 mo to 18 a | 2.18 | 1.21 | 3.94 | .009 | ||||
| Left care age 18 to 18 6 mos. a | 4.94 | 2.61 | 9.37 | <.0001 | ||||
| Left care 18 6 mos. To 19 a | 7.33 | 3.36 | 15.97 | <.0001 | ||||
compared to those who did not leave custody before age 19
Using logistic regression to predict continued medication use across the transition period out of foster care, only two variables remained in the model after manual backwards elimination. Young people who reported histories of physical neglect (OR=.073, CI .01 - .62, p<.016) and who were male (OR=.23, CI .04 – 1.23, p=.086) were less likely to continue psychotropic medication use across the transition period.
Only foster care system discharge status was predictive of months until outpatient specialty mental health service was terminated. Earlier discharge was associated with earlier stoppage of services. Each six month period of earlier discharge was associated with an increase in the hazards ratio of stopping service early of 1.25 (CI 1.06 - 1.47, p=.009). Only a history of physical neglect was associated with lower odds of continued outpatient specialty mental health services across the transition out of the foster care system (OR=.11, CI .01, .92, p=.042).
Discussion
This is the first study known to systematically examine mental health service use as older youth leave the foster care system. Four findings deserve discussion: the severe drop-off in service use, the terminations often initiated by the patient, the role of Medicaid in service use, and the lack of predictors of continued service use.
Service discontinuity in mental health services was the norm for youth leaving the foster care system. Rates of mental health service utilization for youth from the foster care system dropped substantially from ages 17 to 19. The decline was most marked for those who had exited the foster care system. Services typically stopped soon after system exit and discharge status was the most robust predictor of continued service use, with earlier discharge from the foster care system associated with earlier service stoppage and service discontinuities. However, young people who stayed in care to age 19 also showed a steady decrease in outpatient specialized mental health service use and use of psychotropic medications over time. These decreases in service use were somewhat greater than was expected, given results from other studies of youth from foster care.7 8
The drop off in service use may have been exceptionally steep because young people wanted to leave their mental health services. Most young adults who stopped taking psychotropic medications after leaving the foster care system said it was their decision to do so. Many young adults stopped taking psychotropic medications because they didn't like being on medications or didn't think they needed to take the medications. Once it became their option, and not a case manager's or substitute parent's, they stopped the medications. This is consistent with recent research showing some young people in the foster care system are unhappy with the way psychotropic medications are prescribed.16
A minority of young adults who had left the foster care system who stopped psychotropic medications (11%) or stopped seeing an outpatient mental health professional (25%) reported that they did so because of cost. Yet, using mental health services after leaving the foster care system was uncommon in the absence of Medicaid payments. Very few young adults who were not receiving Medicaid continued to receive mental health services. Only three youth not on Medicaid reported current pharmacotherapy. Continued Medicaid coverage appears vital if young adults leaving the foster care system are going to continue to receive needed mental health services. State administrators fearful about the cost of participating in the federal option of continuing Medicaid to age 21 for youth who have left foster care should note that youth in this age group were eager to terminate many of their services. Cost estimates based on service usage prior to leaving care will overestimate the cost of participating in this federal Medicaid option. Inappropriate underutilization of services is more likely than inappropriate overutilization of services.
It is unclear how generalizable these results may be to non-psychiatric disorders treated in the pediatric setting. Clinicians need to be aware however, that their older youth patients may experience a strong desire to attempt to experience life, at least temporarily, free from the burden of chronic disease management.
This research, although an improvement over existing studies, was limited in several ways. Since child welfare and mental health systems can be structured differently, the study's results may be geographically limited. The data were obtained solely from participants. Providers, for example, may have given different reasons for why services were terminated. The study examined several indicators of service use, but we were unable to determine whether the services used were clinically indicated or evidence-based or otherwise of high quality. Finally, young adults who remained in the study differed from those who did not. It is unknown how these differences may have affected the study results.
Acknowledgments
This work was supported by grants from the National Institute of Mental Health (R01 MH61404 and P30 MH068579).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
J. Curtis McMillen, George Warren Brown School of Social Work, Washington University in St. Louis
Ramesh Raghavan, George Warren Brown School of Social Work and Department of Psychiatry, Washington University in St. Louis
References
- 1.Reiss J, Gibson R. Health care transition: Destination unknown. Pediatrics. 2002;110(6 pt 2):1307–14. [PubMed] [Google Scholar]
- 2.Reiss JG, Gibson RW, Walker LR. Health care transition: Youth family and provider perspectives. Pediatrics. 2005;115:112–120. doi: 10.1542/peds.2004-1321. [DOI] [PubMed] [Google Scholar]
- 3.Davis M, Sondheimer DL. State child mental health efforts to support youth in transition to adulthood. J Behav Health Serv Res. 2005;32:27–42. doi: 10.1007/BF02287326. [DOI] [PubMed] [Google Scholar]
- 4.McMillen JC, Zima BT, Scott LD, et al. The prevalence of psychiatric disorders among older youths in the foster care system. J Am Acad Child Adolesc Psychiatry. 2005;44:88–95. doi: 10.1097/01.chi.0000145806.24274.d2. [DOI] [PubMed] [Google Scholar]
- 5.McMillen JC, Scott LS, Zima BT, et al. The mental health service use of older youth in foster care. Psychiatr Serv. 2004;55:811–817. doi: 10.1176/appi.ps.55.7.811. [DOI] [PubMed] [Google Scholar]
- 6.Cuffe SP, Waller JL, Addy CL, et al. A longitudinal study of adolescent mental health service use. J Behav Health Serv Res. 2001;28:1–11. doi: 10.1007/BF02287230. [DOI] [PubMed] [Google Scholar]
- 7.Courtney ME, Dworsky A, Ruth, et al. Midwest evaluation of the adult functioning of former foster youth: Outcomes at age 19. Chicago: Chapin Hall Center for Children; 2005. [Google Scholar]
- 8.Courtney E, Piliavin I, Grogan-Kaylor A, et al. Foster youth transitions to adulthood: A longitudinal view of youth leaving care. Child Welfare. 2001;80:685–717. [PubMed] [Google Scholar]
- 9.Caspi A, Moffitt TE, Thornton, et al. The life history calendar: A research and clinical assessment method for collecting retrospective event-history data. International Journal of Methods in Psychiatric Research. 1996;6:101–114. [Google Scholar]
- 10.Horwitz SM, Hoagwood K, Stiffman AR, et al. Reliability of the Services Assessment for Children and Adolescents. Psychiatr Serv. 2001;52:1088–1094. doi: 10.1176/appi.ps.52.8.1088. [DOI] [PubMed] [Google Scholar]
- 11.Stiffman AR, Horwitz SM, Hoagwood K, et al. The Service Assessment for Children and Adolescents (SACA): Adult and child reports. J Am Acad Child Adolesc Psychiatry. 2000;39:1032–1039. doi: 10.1097/00004583-200008000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Robins L, Cottler L, Bucholz K, et al. Diagnostic Interview Schedule for DSM-IV. St. Louis, MO: Washington University in St. Louis; 1995. [Google Scholar]
- 13.Bernstein DP, Fink L. The Childhood Trauma Questionnaire Manual. San Antonio: The Psychological Corporation; 1998. [Google Scholar]
- 14.Russell DEH. The secret trauma: Incest in the lives of girls and women. New York: Basic Books; 1986. [Google Scholar]
- 15.Fischer EH, Turner JL. Orientations to seeking professional help: Development and research utility of an attitude scale. J Consult Clin Psychol. 1970;35:79–90. doi: 10.1037/h0029636. [DOI] [PubMed] [Google Scholar]
- 16.Lee B, Munson MR, Ware NC, et al. Voices of foster care youths: Consumer views of mental health services. Psychiatr Serv. 2006;57:487–492. doi: 10.1176/ps.2006.57.4.487. [DOI] [PubMed] [Google Scholar]