Abstract
Helicobacter species have been found in human bile and biliary tract (BT) tissue and are suspected to cause BT diseases, including gallbladder and extrahepatic cancers, collectively referred to in this work as BT cancers. We conducted a literature review of the epidemiological evidence linking the presence of Helicobacter species in bile or BT biopsies to BT cancers and benign diseases. Reports showed great variability with respect to study methods. Nine studies of BT cancers were identified, all with 30 or fewer BT cancers; eight included cancer-free control subjects and used polymerase chain reaction (PCR) as a means of Helicobacter species detection. In four of these studies, Helicobacter species were detected in patients with BT cancer significantly more frequently than in controls, at least when controls without BT diseases were used. In two studies, no Helicobacter species were detected in either cases or controls. Helicobacter species were also often detected in benign BT diseases such as gallstone disease or chronic cholecystitis. As our current knowledge relies on a few small studies that showed substantial differences, larger studies and more standardised protocols for detecting DNA and antibodies against Helicobacter species are needed to investigate a potential association with BT cancer.
Keywords: Helicobacter , biliary tract neoplasms, gallbladder neoplasms, gallstones, cholecystitis
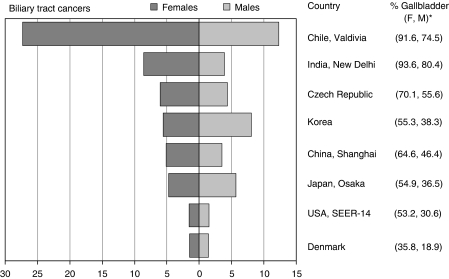
Gallbladder cancers (ICD-10 code C23) and extrahepatic biliary tract cancers (code C24, hereafter referred to collectively as biliary tract (BT) cancers) are relatively rare malignancies with wide variations in incidence rates worldwide (Figure 1). The highest BT cancer incidence rates are seen within Latin America (e.g., up to 9.3 per 100 000 for men and 25.3 per 100 000 for women in Chile), but the disease is also frequent in Northern India, Japan, Korea, and some Eastern European countries (Curado et al, 2007). Although gallbladder cancer is the most common BT cancer, its overall incidence, and its proportion of all BT cancer, varies substantially across regions and genders (e.g., 18.9% among men in Denmark and 93.6% among women in New Delhi, India, Figure 1) (Saika and Matsuda, 2007). It usually occurs in patients with a history of gallstone disease and chronic cholecystitis (Randi et al, 2006).
Figure 1.
Age standardised incidences rates per 100 000 (world standard population) for biliary tract cancer, including gallbladder and extrahepatic biliary tract cancers (ICD-10, C23-C24) in selected areas of the world (1998–2002). *Percentage of gallbladder cancers (code C23 only) on all biliary tract cancers in women (F) and men (M). Source: Curado et al, 2007.
Helicobacter pylori (H. pylori) infection is a well-established cause of stomach cancer (Amieva and El-Omar, 2008). Since the discovery of H. pylori in 1982, 30 other Helicobacter species have been isolated from the stomach, intestinal tract, and liver of mammals and birds. A few species found in human bile and BT tissue biopsies (Helicobacter bilis (H. bilis), Helicobacter pullorum (H. pullorum), Helicobacter hepaticus (H. hepaticus), and H. pylori) have been suspected to cause BT diseases. We aimed to review current information on Helicobacter species in BT cancer and benign BT diseases in humans and to help delineate future research needs on the topic.
Materials and methods
We carried out several detailed searches of the database MEDLINE through PUBMED, using the following entry terms in the first search round: (‘Gallbladder Neoplasms’[Mesh] OR ‘Gallbladder’[Mesh] OR ‘Gallbladder Diseases’[Mesh] OR Gallbladder [Text Word]) AND (‘Helicobacter’[Mesh] OR ‘Helicobacter Infections’[Mesh] OR ‘Helicobacter hepaticus’[Mesh] OR ‘Helicobacter pylori’[Mesh] OR ‘Helicobacter’[Text Word]). We then repeated the search using ‘Biliary tract neoplasms’, ‘Cholangiocarcinoma’, ‘Cholelithiasis’, ‘Cholecystis’, and ‘Gallstone’ as entry terms instead of ‘Gallbladder neoplasms’. Other MEDLINE searches were subsequently carried out using ‘Helicobacter bilis’ and ‘Helicobacter pullorum’ as single entry terms. Regional databases for India, Southeast Asia, and Latin America (the Index Medicus for South-East Asia Region (IMSEAR), Latin American and Caribbean Centre on Health Sciences Information (LILACS) and Indian Medlars Center National Informatics Centre (INDMED) databases, respectively) were also searched. Finally, we reviewed the reference lists of all identified relevant studies. No restrictions on date or publication language were applied. After exclusion of case-series with fewer than five patients or biological specimens, we retained all relevant human studies on BT cancer and their possible or proven precursor lesions published up to January 2008.
For the sake of accuracy and comparability, only the following methods of direct Helicobacter species detection in bile, gallstones, or tissue biopsies were considered for the review: (1) amplification by polymerase chain reaction (PCR), (2) histology (histopathology, immunohistopathology), and (3) culture. For each of the studies selected in this review, the following was retrieved whenever available: location and year of data collection, histological diagnosis, age and gender of BT cancer cases, type of biological specimen, method of Helicobacter species detection, type of Helicobacter species identified, and selection criteria of control subjects, if present.
Results
Helicobacter species and BT cancers
Nine studies (Table 1) that investigated the presence of Helicobacter species in the bile or BT tissue biopsies of patients with BT cancers were identified (Roe et al, 1999; Fukuda et al, 2002; Matsukura et al, 2002; Bulajic et al, 2002a; Fallone et al, 2003; Murata et al, 2004; Pradhan and Dali, 2004; Kobayashi et al, 2005; Bohr et al, 2007). Eight studies used PCR as one of the means of Helicobacter species detection. The PCR primers varied across studies, but most used genus-specific primers (such as C97-C98) as a first-line test before undertaking PCR assays that targeted different Helicobacter species.
Table 1. Human studies on Helicobacter (H) species and gallbladder cancers (GC) or extra-hepatic biliary tract cancers (EBC) by testing method.
| Reference | Country | Cancer diagnosis | Biological specimen | Method | Organism | H-positive/ total cases |
|---|---|---|---|---|---|---|
| PCR | Primer | |||||
| Roe et al (1999) | Korea | EBC | Bile | 16S (H276f; H676r) | H genus | 6/15 |
| UreA (HPU1; HPU2) | UreA-positive H | 7/15 | ||||
| Bulajic et al (2002a) | Serbia | GC+EBC | Bile | 16S (various), UreA | H genus | 12/15 |
| Fukuda et al (2002) a | Japan | GC+EBC | Bile, tissue biopsies | 16S (C97–98) | H genus | 10/19 |
| 16S (species specific) | H bilis | 6/19 | ||||
| 16S (species specific) | H hepaticus | 4/19 | ||||
| UreA (HPU1; HPU2) | UreA-positive H | 1/19 | ||||
| Matsukura et al (2002) | Japan | EBC | Bile | 16S (species specific) | H bilis | 13/15 |
| Thailand | GC+EBC | Bile | 16S (species specific) | H bilis | 11/14 | |
| Fallone et al (2003) | Canada | EBC | Bile | 16S (C97–98) | H genus | 0/9 |
| Murata et al (2004) | Japan | GC+EBC | Tissue biopsies | 16S (species specific) | H bilis | 4/14 |
| Kobayashi et al (2005) | Japan | GC+EBC | Bile | 16S (C97–98 or C05) | H genus | 5/6 |
| 16S (species specific) | H bilis | 1/5 | ||||
| 16S (species specific) | H hepaticus | 0/5 | ||||
| UreA | UreA-positive H | 2/6 | ||||
| Bohr et al (2007) | Germany | GC | Tissue biopsies | 16S (C97–20; H3A-20) | H genus | 0/20 |
| Histology | Stain, antibodies, etc. | |||||
| Pradhan and Dali (2004) | Nepal | GC+ EBC | Tissue biopsies | Histopathology, Warthin-Starry | H genus | 6/7 |
| Bohr et al (2007) | Germany | GC | Tissue biopsies | Histopathology, Various staining | H genus | 0/20 |
| Histoimmunochemistry | H genus | 0/20 | ||||
| Culture | Conditions | |||||
| Roe et al (1999) | Korea | EBC | Bile | Fresh specimens, under microaerophilic and anaerobic conditions | H genus | 0/15 |
| Bohr et al (2007) | Germany | GC | Tissue biopsies | Fresh specimens, under microaerophilic conditions | H genus | 0/5 |
Five cases in this study were intra-hepatic bile duct cancers.
Variability among PCR study findings was substantial (between 0 and 82.8% of specimens tested positive for Helicobacter species) even when analysis was restricted to the same type of biological specimen (bile or tissue biopsies). Using species-specific primers, H. bilis was found in 35 out of 67 specimens (52.2%) from four different studies, whereas H. hepaticus was searched for in two studies, but only found in 4 out of 19 specimens (21.1%) in one study.
Two studies used histopathology staining to search for Helicobacter species in BT tissue biopsies. Although Helicobacter-like bacteria were detected in six out of seven BT cancers from a study in Nepal, no infections were detected in a German series of 20 BT cancers, using three different methods of staining and histoimmunochemistry. The German study also reported negative findings according to several PCR amplification methods, as well as culture, of fresh gallbladder tissue biopsies. Only one other study reported an attempt to cultivate these bacteria, but although tissue biopsies yielded positive PCR results, culture in microaerophilic conditions was unsuccessful (Table 1).
Eight studies had one or more control groups allowing some comparison with cancer cases (Table 2). Controls were subjects who underwent the same procedure as cases, and were diagnosed with benign BT diseases. In three studies, a group of controls without BT diseases was also included. The presence of Helicobacter species in bile or BT tissue biopsies was detected significantly more often in cases than in controls in four studies, at least when controls without BT diseases were used, but none were detected in cases in two other studies (Table 2).
Table 2. Helicobacter (H) species detection in biliary tract (BT) cancer patients compared with controls.
| Reference | H-positive/total cases | Control diagnosis | H-positive/total controls |
|---|---|---|---|
| Roe et al (1999) | 6/15 | Benign BT diseases | 3/11 |
| Matsukura et al (2002) | |||
| Japan | 13/15 | Benign BT diseases | 8/16a |
| Thailand | 11/14 | Benign BT diseases | 10/26a |
| Bulajic et al (2002a) b | 12/15 | No BT diseases | 3/11a |
| Benign BT diseases | 37/63 | ||
| Fukuda et al (2002) c | 10/19 | Benign BT diseases | 3/19a |
| Fallone et al (2003) | 0/9 | Benign BT diseases | 0/75 |
| Murata et al (2004) | 4/14 | Benign BT diseases | 2/16 |
| Kobayashi et al (2005) | 5/6 | No BT diseases | 2/21a |
| Benign BT diseases | 16/30 | ||
| Bohr et al (2007) | 0/20 | No BT diseases | 0/22 |
| Benign BT diseases | 1/57d |
Fisher's exact test, P<0.05.
Bulajic et al (2002a) also reported age- and sex-adjusted odds ratio (9.9; 95% confidence interval: 1.4–70.5).
Five of the cases in this study were intrahepatic bile duct cancers.
In the only positive control specimen, the organism was identified as Helicobacter ganmani.
Helicobacter species and benign BT diseases
Our literature search identified 20 studies investigating the presence of Helicobacter species in the bile, gallstones, or BT tissue biopsies of patients with benign BT diseases (Arnaout et al, 1990; Figura et al, 1998; Fox et al, 1998; Monti et al, 1999; Rudi et al, 1999; Myung et al, 2000; Harada et al, 2001; Mendez-Sanchez et al, 2001; Monstein et al, 2002; Roosendaal et al, 2002; Bulajic et al, 2002b; Chen et al, 2003, 2007; Silva et al, 2003; Farshad et al, 2004; Abayli et al, 2005; Apostolov et al, 2005; Neri et al, 2005; Tiwari et al, 2006; Misra et al, 2007). Of these, 19 used PCR amplification methods (Table 3). The choice of primers varied across studies; some primers were based on genes coding for the 26kDa H. pylori protein, UreA or UreB enzymes, whereas others targeted 16S ribosomal RNA fragments, either common to all organisms of the Helicobacter genus, or specific to a particular species. Only in two studies, from Chile and Brazil, did the authors undertake sequencing to identify the detected species.
Table 3. Helicobacter (H) species in patients with benign biliary tract diseases.
| Reference | Country | Biological specimen | Method | Organism | H-positive/ total cases |
|---|---|---|---|---|---|
| PCR | Primer | ||||
| Figura et al (1998) | Italy | Bile | CagA (final product 298 bp) | CagA-positive H | 1/30 |
| Fox et al (1998) | Chile | Bile, tissue biopsies | 16S (C97–98 or C97–05) | H genus | 22/46 |
| Sequencing | H bilisa | 7/8 | |||
| Sequencing | H pullorum | 1/8 | |||
| Monti et al (1999) | Argentina | Bile | Not specified (final product 296 bp) | H genus | 2/26 |
| Rudi et al (1999) | Germany | Bile | 16S (various species specific) | H genus | 0/73 |
| Myung et al (2000) | Korea | Bile, tissue biopsies | UreA (final product 258 bp) | H genus | 5/53 |
| 26kDa | H genus | 4/53 | |||
| Stone | UreA or 26kDa | H genus | 7/53 | ||
| UreA or 26kDa | H genus | 0/7 | |||
| Harada et al (2001) | Japan | Bile, tissue biopsies | 16S (C97–98) | H genus | 2/53 |
| UreA (final product 258 bp) | UreA-positive H | 1/53 | |||
| Mendez-Sanchez et al (2001) | Mexico | Tissue biopsies | 16S (C97–98) | H genus | 1/95 |
| Bulajic et al (2002b) | Serbia | Bile | UreA (final product 258 bp) | H genus | 35/65 |
| Monstein et al (2002) | Sweden | Stone | 16S (species specific) | H pylori | 11/20 |
| Roosendaal et al (2002) | Netherlands | Bile | 16S (various specific primers) | H pylori | 1/21 |
| Chen et al (2003) | New Zealand | Tissue biopsies | 16S (C97–98) | H genus | 46/85 |
| 26kDa | H genus | 31/46 | |||
| 16S (species specific) | H pylori | 22/25 | |||
| 16S (C62-C12) | H bilis | 0/85 | |||
| Silva et al (2003) | Brazil | Bile, tissue biopsies | 16S (C97–98) | H genus | 18/46 |
| Sequencing | H pylori | 18/18 | |||
| Farshad et al (2004) | Iran | Stone | 16S (species specific) | H pylori | 6/33 |
| Bile | 16S (species specific) | H pylori | 4/33 | ||
| Abayli et al (2005) | Turkey | Stone | 16S (final product 349 bp) | H genus | 7/77 |
| Apostolov et al (2005) | Ukraine | Tissue biopsies | 16S (C97–98) | H genus | 16/22 |
| Neri et al (2005) | Italy | Bile, tissue biopsies | 16S (C95–98) | H genus | 17/33 |
| Tiwari et al (2006) | India | Bile | 16S | H genus | 29/30 |
| 16S (species specific) | H pylori | 10/29 | |||
| UreA (final product 411 bp) | UreA-positive H | 10/29 | |||
| CagA | CagA-positive H | 9/29 | |||
| Chen et al (2007) | China | Tissue biopsies | UreA (final product 411 bp) | UreA-positive H | 15/81 |
| UreB (final product 132 bp) | UreB-positive H | 18/81 | |||
| UreA or UreB | Ure-positive H | 22/81 | |||
| Misra et al (2007) | India | Stone | 16S (species specific) | H pylori | 8/11 |
| Histology | Stain, antibodies, etc. | ||||
| Arnaout et al (1990) | UK | Tissue biopsies | Histopathology, H&E (PAS), Warthin-Starry | H pylori | 0/16b |
| Fox et al (1998) | Chile | Tissue biopsies | Histopathology, Warthin-Starry | H genus | 2/18 |
| Mendez-Sanchez et al (2001) | Mexico | Tissue biopsies | Histopathology, H&E, Giemsa | H genus | 0/95 |
| Immuno-histopathology, polyclonal anti H pylori | H pylori | 1/95 | |||
| Abayli et al (2005) | Turkey | Tissue biopsies | Histopathology, H&E, gram, Warthin-Starry | H genus | 18/77 |
| Apostolov et al (2005) | Ukraine | Tissue biopsies | Immuno-histopathology, anti-CagA, anti-VacA, anti-H pylori | H pylori | 13/16c |
| Chen et al (2007) | China | Tissue biopsies | Histopathology, Warthin-Starry | H genus | 71/524 |
| Immuno-histopathology, polyclonal anti-H pylori | H pylori | 37/71d | |||
| Misra et al (2007) | India | Tissue biopsies | Histopathology, H&E (PAS), Loeffler, Warthin Starry | H genus | 50/111b |
| Immuno-histopathology, polyclonal anti-H pylori | H pylori | 50/111b | |||
| Culture | Conditions | ||||
| Fox et al (1998) | Chile | Bile, tissue biopsies | Frozen specimens, microaerophilic conditions | H genus | 0/46 |
| Harada et al (2001) | Japan | Bile | Frozen specimens, microaerophilic conditions | H genus | 0/39 |
| Silva et al (2003) | Brazil | Bile, tissue biopsies | Frozen specimens, microaerophilic conditions | H genus | 0/46 |
| Abayli et al (2005) | Turkey | Tissue biopsies | Fresh specimens, microaerophilic conditions | Oxydase- and ure-positive H genus | 6/77 |
H species identified in this study as H rappini was later reclassified as belonging to the H bilis species (Hanninen et al, 2005).
Only specimens with gastric metaplasia were investigated.
Only specimens H genus-positive by PCR were investigated.
Only specimens H genus-positive by histology were investigated.
Helicobacter species were assessed by PCR in gallstones in five studies. The frequency of detection varied from 0 to 72%, and the species identified was believed to be H. pylori in all cases. In one study from Sweden, H. pylori was searched for and detected in the nucleus rather than in the envelope of the stones, suggesting an early presence of the bacteria in the process of gallstone formation (Monstein et al, 2002). Of 16 PCR studies on Helicobacter species in bile or BT tissue biopsies in benign BT diseases, the percentage of positive specimens varied from near 0% in five studies to close to 50% in six others, with three studies showing intermediate percentages. Two other studies reported a high prevalence: 29 out of 30 bile specimens of patients with hepatobiliary diseases were Helicobacter genus-positive in one study, as were 16 out of 22 gallbladder tissue biopsies of chronic cholecystitis patients in another.
Histological and/or immunohistological examination of tissue biopsies was undertaken in seven studies (including two histological series of metaplastic gallbladder sections) using various staining methods and antibodies. Helicobacter-like bacteria were seen in all but one study, and the percentage of positive specimens varied from 1 to 45%. In three studies, immunohistological staining using anti-H. pylori antibodies confirmed the histological findings. Attempts to culture the bacteria were reported in four studies, with three failing to grow any Helicobacter species from frozen specimens, despite some success with PCR or histology. In another study, however, 6 out of 77 (8%) fresh gallbladder tissue biopsies from patients with gallstones grew Helicobacter-like bacteria (Table 3).
Discussion
We aimed to evaluate available evidence linking Helicobacter infection with BT cancer. It became clear that our current knowledge relies mainly on a few small studies that show substantial differences in methods and results. In four studies, mainly from Japan, the detection of Helicobacter species was significantly more frequent in bile or BT tissue biopsies of cancer patients compared with controls, at least when controls without BT diseases were used. Using species-specific primers, the Helicobacter species most consistently searched for and identified from bile or BT tissue biopsies of cancer patients was H. bilis. In two studies from Canada and Germany, however, no Helicobacter species were detected in BT cancers, despite the use in the German study of numerous detection techniques.
The presence of Helicobacter species, including H. pylori, was also often detected in benign BT diseases such as gallstone disease or chronic cholecystitis, which are recognised risk factors for the development of BT cancer. However, as with BT cancer, studies of benign BT diseases showed extreme variability in methods and findings.
Lower Helicobacter species prevalence was typically observed in western countries with low BT cancer incidence, and higher prevalence in countries with high BT cancer incidence, the best example being Japan. Whether regional variations in the prevalence of Helicobacter species in BT cancers are real or are a result of differences in the type and quality of detection methods used is unknown.
Most findings presented here derive from PCR-based studies, the comparability of which depends on the quality of the biological specimens (bile, stone, or tissue biopsies; fresh, fixed, or frozen), the strategy chosen for Helicobacter detection, and potential problems such as contamination and the presence of Taq polymerase inhibitors. The sensitivity and specificity of PCR are also directly dependent on the choice of primers. In early studies, primers targeting the genes encoding the 26kDa protein or the UreA or UreB proteins were often used. Although authors believed that H. pylori was identified, these findings may also be consistent with other Helicobacter species. For example, it has been shown that a gene coding for the 26kDa protein is present in at least eight other Helicobacter species (including H. bilis and H. pullorum) with high similarity to the gene in H. pylori (Lundstrom et al, 2001). Similarly, urease structural genes from H. hepaticus are highly homologous to UreA and UreB from H. pylori (Shen et al, 1998). Even PCR based on the conserved 16S rRNA genes may yield different results depending on the set of primers used (Moyaert et al, 2008).
It should be noted that the available sequence information from non-H. pylori species is still limited. Moreover, for H. pylori, it has been shown that the intraspecies sequence variability is substantial, which may hamper uniform detection by a single set of PCR primers (Kraft et al, 2006). Therefore, it is difficult to determine whether PCR primers can distinguish Helicobacter species, especially in patients from different geographic regions. The sensitivity of PCR is also inversely proportional to the length of the amplicon. This is particularly important in clinical materials with a high risk of DNA damage, such as formalin-fixed, paraffin-embedded tissue biopsies.
Taken together, for reliable Helicobacter species detection and distinction, it would be advisable, although seldom done so far, to use multiple PCR primer sets at somewhat reduced annealing temperatures to permit amplification of imperfectly matching sequences. Ultimately, amplicons obtained by such PCR should be sequenced to confirm the true identity of the Helicobacter species.
Means of detection other than PCR also have substantial drawbacks. Helicobacter species culture has been unsuccessful in the majority of studies of BT cancer or benign BT diseases. The use of frozen specimens, which are notoriously difficult to culture, may explain some of the negative findings (Solnick and Schauer, 2001). Histology has been considered the gold standard for the detection of H. pylori in the stomach for many years; however, few studies have assessed histological changes associated with Helicobacter infection in the gallbladder or BT tissue. In two studies from India and China, colonisation by Helicobacter was shown in the gallbladder epithelium, especially in the areas of gastric metaplasia (Chen et al, 2007; Misra et al, 2007), but it is not known whether this was merely a consequence of tissue damage. Serological studies have not been reviewed here, but cross-reactivity between the immune response to antigens from H. pylori and H. bilis has been reported (Ananieva et al, 2002; Pisani et al, 2008). Furthermore, it has been shown that the prevalence of serological and histological markers of H. pylori decreases in gastric cancer (Camorlinga-Ponce et al, 2008) and it is not known whether the same happens in BT cancer.
An implication of Helicobacter infection in BT cancer pathogenesis is nevertheless plausible. Helicobacter species that can survive in, or colonise, the bile ducts may induce the formation of gallstones both directly, through the urease activity of some of the species, or indirectly through a T-cell-dependent immune response (Belzer et al, 2006; Maurer et al, 2007). The colonisation of the mucosa by bacteria may also aggravate the chronic inflammatory state already caused by gallstones (Wistuba and Gazdar, 2004; Jergens et al, 2007). In animal studies, the sequence of events going from chronic inflammation to cancer has been directly linked to some Helicobacter species. For instance, H. hepaticus can cause chronic active infection of bile canaliculi that progresses to liver carcinoma in A/JCr laboratory strains of mice (Ward et al, 1994). Similarly, colon cancer in SMAD-3-deficient mice is enhanced by dual infection with H. hepaticus and H. bilis (Maggio-Price et al, 2006).
In conclusion, further development of PCR testing protocols is required, as well as a better characterisation of antigens suitable for histoimmunochemistry. As the BT is only accessible through invasive procedure or surgery, the choice of controls who can provide adequate specimens for case–control studies is limited. Larger epidemiological studies will only be possible by developing serological methods validated against direct detection of Helicobacter species in the gallbladder.
Acknowledgments
We thank T. Perdrix-Thoma for editorial assistance and S. Grant for help with literature searches.
Footnotes
Conflict of interest
The authors declared no conflict of interest.
References
- Abayli B, Colakoglu S, Serin M, Erdogan S, Isiksal YF, Tuncer I, Koksal F, Demiryurek H (2005) Helicobacter pylori in the etiology of cholesterol gallstones. J Clin Gastroenterol 39: 134–137 [PubMed] [Google Scholar]
- Amieva MR, El-Omar EM (2008) Host–bacterial interactions in Helicobacter pylori infection. Gastroenterology 134: 306–323 [DOI] [PubMed] [Google Scholar]
- Ananieva O, Nilsson I, Vorobjova T, Uibo R, Wadstrom T (2002) Immune responses to bile-tolerant Helicobacter species in patients with chronic liver diseases, a randomized population group, and healthy blood donors. Clin Diagn Lab Immunol 9: 1160–1164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apostolov E, Al-Soud WA, Nilsson I, Kornilovska I, Usenko V, Lyzogubov V, Gaydar Y, Wadstrom T, Ljungh A (2005) Helicobacter pylori and other Helicobacter species in gallbladder and liver of patients with chronic cholecystitis detected by immunological and molecular methods. Scand J Gastroenterol 40: 96–102 [DOI] [PubMed] [Google Scholar]
- Arnaout AH, Abbas SH, Shousha S (1990) Helicobacter pylori is not identified in areas of gastric metaplasia of gall bladder. J Pathol 160: 333–334 [DOI] [PubMed] [Google Scholar]
- Belzer C, Kusters JG, Kuipers EJ, van Vliet AH (2006) Urease induced calcium precipitation by Helicobacter species may initiate gallstone formation. Gut 55: 1678–1679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohr UR, Kuester D, Meyer F, Wex T, Stillert M, Csepregi A, Lippert H, Roessner A, Malfertheiner P (2007) Low prevalence of Helicobacteraceae in gall-stone disease and gall-bladder carcinoma in the German population. Clin Microbiol Infect 13: 525–531 [DOI] [PubMed] [Google Scholar]
- Bulajic M, Maisonneuve P, Schneider-Brachert W, Muller P, Reischl U, Stimec B, Lehn N, Lowenfels AB, Lohr M (2002a) Helicobacter pylori and the risk of benign and malignant biliary tract disease. Cancer 95: 1946–1953 [DOI] [PubMed] [Google Scholar]
- Bulajic M, Stimec B, Milicevic M, Loehr M, Mueller P, Boricic I, Kovacevic N, Bulajic M (2002b) Modalities of testing Helicobacter pylori in patients with nonmalignant bile duct diseases. World J Gastroenterol 8: 301–304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen DF, Hu L, Yi P, Liu WW, Fang DC, Cao H (2007) H. pylori exist in the gallbladder mucosa of patients with chronic cholecystitis. World J Gastroenterol 13: 1608–1611 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen W, Li D, Cannan RJ, Stubbs RS (2003) Common presence of Helicobacter DNA in the gallbladder of patients with gallstone diseases and controls. Dig Liver Dis 35: 237–243 [DOI] [PubMed] [Google Scholar]
- Camorlinga-Ponce M, Flores-Luna L, Lazcano-Ponce E, Herrero R, Bernal-Sahagún F, Abdo-Francis JM, Aguirre-García J, Muñoz N, Torres J (2008) Age and severity of mucosal lesions influence the performance of serologic markers in Helicobacter pylori-associated gastroduodenal pathologies. Cancer Epidemiol Biomarkers Prev 17: 2498–2504 [DOI] [PubMed] [Google Scholar]
- Curado MP, Edwards B, Shin HR, Storm H, Ferlay J, Heanue M, Boyle P (eds) (2007) Cancer Incidence in Five Continents, Vol. IX. IARC Scientific Publications No 160. IARC: Lyon [Google Scholar]
- Fallone CA, Tran S, Semret M, Discepola F, Behr M, Barkun AN (2003) Helicobacter DNA in bile: correlation with hepato-biliary diseases. Aliment Pharmacol Ther 17: 453–458 [DOI] [PubMed] [Google Scholar]
- Farshad S, Alborzi A, Malek Hosseini SA, Oboodi B, Rasouli M, Japoni A, Nasiri J (2004) Identification of Helicobacter pylori DNA in Iranian patients with gallstones. Epidemiol Infect 132: 1185–1189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Figura N, Cetta F, Angelico M, Montalto G, Cetta D, Pacenti L, Vindigni C, Vaira D, Festuccia F, De Santis A, Rattan G, Giannace R, Campagna S, Gennari C (1998) Most Helicobacter pylori-infected patients have specific antibodies, and some also have H. pylori antigens and genomic material in bile: is it a risk factor for gallstone formation? Dig Dis Sci 43: 854–862 [DOI] [PubMed] [Google Scholar]
- Fox JG, Dewhirst FE, Shen Z, Feng Y, Taylor NS, Paster BJ, Ericson RL, Lau CN, Correa P, Araya JC, Roa I (1998) Hepatic Helicobacter species identified in bile and gallbladder tissue from Chileans with chronic cholecystitis. Gastroenterology 114: 755–763 [DOI] [PubMed] [Google Scholar]
- Fukuda K, Kuroki T, Tajima Y, Tsuneoka N, Kitajima T, Matsuzaki S, Furui J, Kanematsu T (2002) Comparative analysis of Helicobacter DNAs and biliary pathology in patients with and without hepatobiliary cancer. Carcinogenesis 23: 1927–1931 [DOI] [PubMed] [Google Scholar]
- Hanninen ML, Karenlampi RI, Koort JM, Mikkonen T, Bjorkroth KJ (2005) Extension of the species Helicobacter bilis to include the reference strains of Helicobacter sp. flexispira taxa 2, 3 and 8 and Finnish canine and feline flexispira strains. Int J Syst Evol Microbiol 55: 891–898 [DOI] [PubMed] [Google Scholar]
- Harada K, Ozaki S, Kono N, Tsuneyama K, Katayanagi K, Hiramatsu K, Nakanuma Y (2001) Frequent molecular identification of Campylobacter but not Helicobacter genus in bile and biliary epithelium in hepatolithiasis. J Pathol 193: 218–223 [DOI] [PubMed] [Google Scholar]
- Jergens AE, Wilson-Welder JH, Dorn A, Henderson A, Liu Z, Evans RB, Hostetter J, Wannemuehler MJ (2007) Helicobacter bilis triggers persistent immune reactivity to antigens derived from the commensal bacteria in gnotobiotic C3H/HeN mice. Gut 56: 934–940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi T, Harada K, Miwa K, Nakanuma Y (2005) Helicobacter genus DNA fragments are commonly detectable in bile from patients with extrahepatic biliary diseases and associated with their pathogenesis. Dig Dis Sci 50: 862–867 [DOI] [PubMed] [Google Scholar]
- Kraft C, Stack A, Josenhans C, Niehus E, Dietrich G, Correa P, Fox JG, Falush D, Suerbaum S (2006) Genomic changes during chronic Helicobacter pylori infection. J Bacteriol 188: 249–254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundstrom AM, Sundaeus V, Bolin I (2001) The 26-kilodalton, AhpC homologue, of Helicobacter pylori is also produced by other Helicobacter species. Helicobacter 6: 44–54 [DOI] [PubMed] [Google Scholar]
- Maggio-Price L, Treuting P, Zeng W, Tsang M, Bielefeldt-Ohmann H, Iritani BM (2006) Helicobacter infection is required for inflammation and colon cancer in SMAD3-deficient mice. Cancer Res 66: 828–838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsukura N, Yokomuro S, Yamada S, Tajiri T, Sundo T, Hadama T, Kamiya S, Naito Z, Fox JG (2002) Association between Helicobacter bilis in bile and biliary tract malignancies: H. bilis in bile from Japanese and Thai patients with benign and malignant diseases in the biliary tract. Jpn J Cancer Res 93: 842–847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maurer KJ, Rao VP, Ge Z, Rogers AB, Oura TJ, Carey MC, Fox JG (2007) T-cell function is critical for murine cholesterol gallstone formation. Gastroenterology 133: 1304–1315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendez-Sanchez N, Pichardo R, Gonzalez J, Sanchez H, Moreno M, Barquera F, Estevez HO, Uribe M (2001) Lack of association between Helicobacter sp colonization and gallstone disease. J Clin Gastroenterol 32: 138–141 [DOI] [PubMed] [Google Scholar]
- Misra V, Misra SP, Dwivedi M, Shouche Y, Dharne M, Singh PA (2007) Helicobacter pylori in areas of gastric metaplasia in the gallbladder and isolation of H. pylori DNA from gallstones. Pathology 39: 419–424 [DOI] [PubMed] [Google Scholar]
- Monstein HJ, Jonsson Y, Zdolsek J, Svanvik J (2002) Identification of Helicobacter pylori DNA in human cholesterol gallstones. Scand J Gastroenterol 37: 112–119 [DOI] [PubMed] [Google Scholar]
- Monti J, Fay M, Banchio C, Amendola R, Farias R, Musi A, Sanchez A, Kesner L, Katz J, Ferro F, Kogan Z, Corti R (1999) [Detection of Helicobacter pylori by polymerase reaction in bile samples from gallbladder and bile stones]. Acta Gastroenterol Latinoam 29: 251–253 [PubMed] [Google Scholar]
- Moyaert H, Pasmans F, Ducatelle R, Haesebrouck F, Baele M (2008) Evaluation of 16S rRNA gene-based PCR assays for genus-level identification of Helicobacter species. J Clin Microbiol 46: 1867–1869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murata H, Tsuji S, Tsujii M, Fu HY, Tanimura H, Tsujimoto M, Matsuura N, Kawano S, Hori M (2004) Helicobacter bilis infection in biliary tract cancer. Aliment Pharmacol Ther 20(Suppl 1): 90–94 [DOI] [PubMed] [Google Scholar]
- Myung SJ, Kim MH, Shim KN, Kim YS, Kim EO, Kim HJ, Park ET, Yoo KS, Lim BC, Seo DW, Lee SK, Min YI, Kim JY (2000) Detection of Helicobacter pylori DNA in human biliary tree and its association with hepatolithiasis. Dig Dis Sci 45: 1405–1412 [DOI] [PubMed] [Google Scholar]
- Neri V, Margiotta M, de Francesco V, Ambrosi A, Valle ND, Fersini A, Tartaglia N, Minenna MF, Ricciardelli C, Giorgio F, Panella C, Ierardi E (2005) DNA sequences and proteic antigens of H. pylori in cholecystic bile and tissue of patients with gallstones. Aliment Pharmacol Ther 22: 715–720 [DOI] [PubMed] [Google Scholar]
- Pisani P, Whary MT, Nilsson I, Sriamporn S, Wadstrom T, Fox JG, Ljungh A, Forman D (2008) Cross-reactivity between immune responses to Helicobacter bilis and Helicobacter pylori in a population in Thailand at high risk of developing cholangiocarcinoma. Clin Vaccine Immunol 15: 1363–1368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pradhan SB, Dali S (2004) Relation between gallbladder neoplasm and Helicobacter hepaticus infection. Kathmandu Univ Med J (KUMJ) 2: 331–335 [PubMed] [Google Scholar]
- Randi G, Franceschi S, La Vecchia C (2006) Gallbladder cancer worldwide: geographical distribution and risk factors. Int J Cancer 118: 1591–1602 [DOI] [PubMed] [Google Scholar]
- Roe IH, Kim JT, Lee HS, Lee JH (1999) Detection of Helicobacter DNA in bile from bile duct diseases. J Korean Med Sci 14: 182–186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roosendaal R, Kuipers EJ, Vandenbroucke-Grauls CM, Kusters JG (2002) Helicobacter species are not detectable by 16S rDNA PCR in bile from Dutch patients with common bile duct stones. Digestion 66: 89–91 [DOI] [PubMed] [Google Scholar]
- Rudi J, Rudy A, Maiwald M, Stremmel W (1999) Helicobacter sp. are not detectable in bile from German patients with biliary disease. Gastroenterology 116: 1016–1017 [DOI] [PubMed] [Google Scholar]
- Saika K, Matsuda T (2007) Comparison of time trends in gallbladder cancer incidence (1973–1997) in East Asia, Europe and the USA, from Cancer Incidence in Five Continents Vols IV–VIII. Jpn J Clin Oncol 37: 974–976 [DOI] [PubMed] [Google Scholar]
- Shen Z, Schauer DB, Mobley HL, Fox JG (1998) Development of a PCR-restriction fragment length polymorphism assay using the nucleotide sequence of the Helicobacter hepaticus urease structural genes ureAB. J Clin Microbiol 36: 2447–2453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva CP, Pereira-Lima JC, Oliveira AG, Guerra JB, Marques DL, Sarmanho L, Cabral MM, Queiroz DM (2003) Association of the presence of Helicobacter in gallbladder tissue with cholelithiasis and cholecystitis. J Clin Microbiol 41: 5615–5618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solnick JV, Schauer DB (2001) Emergence of diverse Helicobacter species in the pathogenesis of gastric and enterohepatic diseases. Clin Microbiol Rev 14: 59–97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiwari SK, Khan AA, Ibrahim M, Habeeb MA, Habibullah CM (2006) Helicobacter pylori and other Helicobacter species DNA in human bile samples from patients with various hepato-biliary diseases. World J Gastroenterol 12: 2181–2186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward JM, Fox JG, Anver MR, Haines DC, George CV, Collins Jr MJ, Gorelick PL, Nagashima K, Gonda MA, Gilden RV, Tully JG, Russel RJ, Benveniste RE, Paster BJ, Dewhirst FE, Donovan JC, Anderson LM, Rice JM (1994) Chronic active hepatitis and associated liver tumors in mice caused by a persistent bacterial infection with a novel Helicobacter species. J Natl Cancer Inst 86: 1222–1227 [DOI] [PubMed] [Google Scholar]
- Wistuba II, Gazdar AF (2004) Gallbladder cancer: lessons from a rare tumour. Nat Rev Cancer 4: 695–706 [DOI] [PubMed] [Google Scholar]