Abstract
We and others previously demonstrated that nicotine, a major component of tobacco, stimulates non small cell lung carcinoma (NSCLC) proliferation through nicotinic acetylcholine receptor (nAChR)-mediated signals. Activation of peroxisome proliferator-activated receptor gamma (PPARγ) has been shown to inhibit NSCLC cell growth, but the exact mechanisms responsible for this effect remain incompletely defined. Herein, we show that nicotine induces NSCLC cell proliferation in part through α4 nAChR prompting us to explore the effects of rosiglitazone, a synthetic PPARγ ligand, on the expression of this receptor. Rosiglitazone inhibited the expression of α4 nAChR, but this effect was through a PPARγ-independent pathway since GW9662, an antagonist of PPARγ, and the transfection of cells with PPARγ siRNA failed to abolish the response. The inhibitory effect of rosiglitazone on α4 nAChR expression was accompanied by phosphorylation of p38 MAPK and ERK1/2, and downregulation of Akt phosphorylation. These signals mediated the inhibitory effects of rosiglitazone on α4 nAChR expression since chemical inhibitors prevented the effect. Rosiglitazone was also found to stimulate p53, a tumor suppressor known to mediate some of the effects of nicotine. Interestingly, p53 upregulation was needed for rosiglitazone-induced inhibition of α4 nAChR. Thus, rosiglitazone inhibits α4 nAChR expression in NSCLC cells through activation of ERK and p38 MAPK, which triggers induction of p53. Finally, like others, we found that nicotine stimulated the expression of α4 nAChR. This process was also inhibited by rosiglitazone through similar pathways.
Keywords: Rosiglitazone, α4 nicotinic acetylcholine receptor, ERK, p38 MAPK, p53, human lung carcinoma cells
INTRODUCTION
Lung carcinoma is the leading cause of carcinoma death in the United States with a dismal 5-year survival rate of less than 15% (1). It is well known that tobacco use is one of the most important risk factors for the development of lung carcinoma and is associated with at least 87% of cancer deaths (2). In particular, non-small cell lung cancer (NSCLC) demonstrates a strong etiologic association with smoking. Nicotine in tobacco smoke leads to both tobacco addiction and therefore represents an important target of investigation. Although nicotine does not appear to be carcinogenic by itself, its metabolism leads to the generation of potent carcinogens (2). Studies from our laboratory and that of others demonstrate that nicotine stimulates human lung cancer cell proliferation and angiogenesis, and suppresses drug-induced apoptosis of tumor cells (3, 4). Several lines of evidence suggest that these effects by nicotine and its derivatives are mediated by nicotinic acetylcholine receptors (nAChRs) expressed in tumor cells, thereby contributing to NSCLC progression (5, 6). In particular, nicotine acts through α-bungarotoxin sensitive nAChRs such as α7 nAChR (4, 7). Others have found that blockers of the α4 nAChR also inhibit the effects of nicotine (5, 8). These studies suggest that both α7 and α4 nAChRs, and perhaps others, mediate the effect of nicotine on NSCLC, and these represent targets for novel anti-cancer strategies.
Peroxisome proliferator-activated receptors (PPARs isotypes α, β/δ, γ) are ligand-inducible nuclear transcription factors that heterodimerize with retinoid X receptors and bind to PPAR response elements (PPRE) located in the promoter region of PPAR target genes (9). These lipid-sensitive receptors can be activated in a variable isotype-specific manner by natural fatty acids, leukotrienes, prostaglandins, and some synthetic agonists, including antidiabetic drugs such as rosiglitazone and ciglitazone, which are specific PPARγ ligands. PPARγ ligands are also effective in regulating cell activation, differentiation, proliferation, and/or apoptosis (10). The anticancer activity of PPARγ ligands has been documented in a variety of cancers including colon, breast, prostate, and lung (11). These and related studies support a role for PPARγ as a potential tumor suppressor, but the mechanisms responsible for these effects remain incompletely elucidated.
In this report, we show that rosiglitazone inhibits α4 nAChR expression in NSCLC cells through PPARγ-independent effects that include activation of ERK and p38 MAPK, which triggers induction of p53. To our knowledge, this is the first report linking rosiglitazone to nAChRs.
MATERIALS AND METHODS
Culture and Chemicals
The human NSCLC cell lines H1838, H2106 and A549 were obtained from the American Type Culture Collection (Manassas, VA) and grown in RPMI-1640 medium supplemented with 10% heat-inactivated FBS, HEPES buffer, 50 IU/ml penicillin/streptomycin, and 1 μg amphotericin (complete medium) as previously described (12). Polyclonal antibodies specific for extracellular signal regulated kinases½ (ERK1/2), phosphor-ERK1/2 (Thr202/Tyr204); the mitogen-activated protein kinase (MAPK) specific inhibitor, PD98059; and the PI3-K inhibitor, LY294002, were purchased from Cell Signaling (Beverly, MA). GW9662 was purchased from Cayman Chemical Co. (Ann Arbor, Michigan). The polyclonal antibodies against α4 nAChR and p53 were purchased from Santa Cruz Biotechnology, Inc (Santa Cruz, California). The α4 nAChR agonist, TC2559, the α4 nAChR antagonist, Dihydro-β-erythroidine, and the α7 nAChR antagonist, α-bungarotoxin, were purchased from TOCRIS Bioscience (Ellisville, Missouri). Rosiglitazone, nicotine, antibodies against PPARγ, the p38 MAPK inhibitor, SB239023, and other chemicals were purchased from Sigma Aldrich (St. Louis, MO) unless otherwise indicated.
Cell viability assay
NSCLC cells were plated at the indicated densities (2×103 cells/well) in 96-well multiwell culture plates (Costar). Cells were treated with agonists and antagonists for 2 h before exposure of the cells to rosiglitazone for 48 h or followed by nicotine for up to 5 days in the culture medium (containing 10% FBS). In separate experiments, cells were transfected with control, α4 nAChR, or p53 siRNAs for 40 h before exposure to rosiglitazone followed by nicotine for up to 5 days. Cell proliferation was evaluated using the CellTiter-Glo Luminescent Cell Viability Assay, a homogenous method of determining number of viable cells in culture based on quantitation of the ATP present which signals the presence of metabolically active cells.
Western blot analysis
The procedure was performed as previously described (13). Briefly, the cultured cells were washed and lysed in cell extraction buffer, then sonicated for 10 seconds. Protein concentrations were determined by the Bio-Rad protein assay. Equal amounts of protein from whole cell lysates were solubilized in 2 × SDS-sample buffers and separated on SDS-polyacrylamide gels. The separated proteins were transferred onto nitrocellulose and blocked with Blotto with 5% BSA or 5% nonfat dry milk and 0.1% Tween 20 for 1 hr at room temperature, and washed three times for 10 min with wash buffer (1×TBST). Blots were incubated with primary antibodies raised against α4 nAChR, PPARγ (1:2000), p-ERK1/2, ERK1/2, pAkt, Akt (1:1000) and p53 (1:2000) overnight at 4 C, washed with wash buffer, and incubated with a secondary antibody raised against rabbit IgG conjugated to horseradish peroxidase (1:2,000 dilution, Cell Signaling) for 1 hr at room temperature. The blots were washed, transferred to freshly made ECL solution (Amersham, Arlington, IL) and exposed to X-ray film. Protein bands were quantified by densitometer scanning using a BioRad GS-800 calibrated densitometer. In controls, the specific antibodies were omitted or replaced by serum IgG.
Treatment with PPARγ, α4 nAChR and p53 small interfering RNA (siRNA)
The α4 nAChR siRNA (h) (Cat No. sc-42528), PPARγ siRNA (h) (Cat No. sc-29455), and p53 siRNA (h) (Cat No sc-29435), and control nonspecific siRNA oligonucleotides (Cat No. sc-37007) were purchased from Santa Cruz Biotechnology, Inc. (Santa Cruz, California). For the transfection procedure, cells were grown to 60% confluence, and experimental and control siRNAs were transfected using the oligofectamine reagent (Invitrogen) according to the manufacturer's instructions. Briefly, oligofectamine reagent was incubated with serum-free medium for 10 min. Subsequently, a mixture of respective siRNA was added. After incubation for 15 min at room temperature, the mixture was diluted with medium and added to each well. The final concentration of siRNAs in each well was 100 nM. After culturing for 40 h, cells were washed, resuspended in new culture media in the presence or absence of rosiglitazone for an additional 24 h for Western Blot, cell growth and luciferase reporter assays.
Transient transfection assay
The Cignal p53 Reporter kit (CCS-004L) was purchased from SuperArray Bioscience (Frederick, MD); it is designed to monitor the activity of the p53-regulated signal transduction pathway in cultured cells. Briefly, NSCLC cells were seeded at a density of 5 ×105 cells/well in 6-well plates and grown to 50 - 60% confluence. For each well, a mixture of inducible p53-responsive firefly luciferase construct and constitutively expressing Renilla luciferase construct (40:1, 0.1μg/μl) were cotransfected into the cells using the oligofectamine reagent (Invitrogen) according to the manufacturer's instructions. After 24 h of incubation, cells were treated with or without rosiglitazone in the presence or absence of nicotine, or with SB239023 and PD98059 for 2 h before exposure of the cells to rosiglitazone for an additional 24 h. The preparation of cell extracts and measurement of luciferase activities were carried out using the Dual-Luciferase Reporter Kit according to recommendations by the manufacturer (Promega). The assays for firefly luciferase activity and Renilla luciferase activity were performed sequentially in a Labsystems Luminoskan Ascent luminometer equipped with dual injectors. Changes in firefly luciferase activity were calculated and plotted after normalization with changes in Renilla luciferase activity within the same sample.
Statistical Analysis
All experiments were repeated a minimum of three times. All data from Western Blot analysis, luciferase reporter and cell growth assays were expressed in mean ± SD. The data presented in some figures are from a representative experiment, which was qualitatively similar in the replicate experiments. Statistical significance was determined with Student's t test (two-tailed) comparison between two groups of data set. Asterisks shown in the figures indicate significant differences of experimental groups in comparison with the corresponding control condition (P<0.05, see figure legends).
RESULTS
Nicotine stimulates NSCLC cell proliferation through α4 nAChR
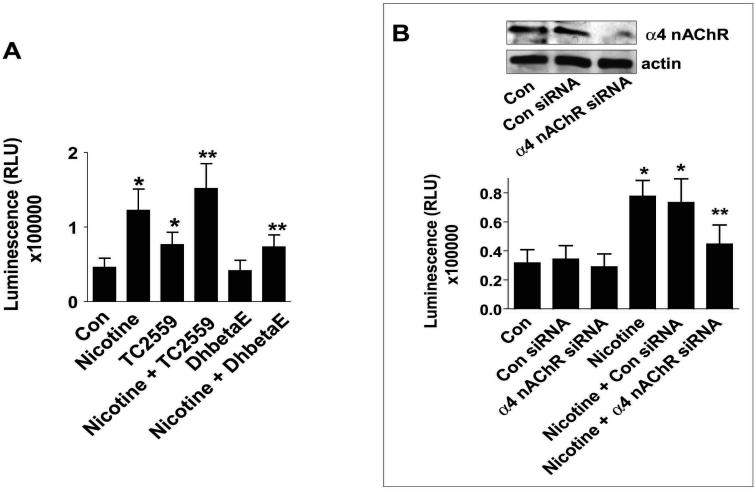
We and others demonstrated that nicotine stimulates NSCLC cell proliferation through nAChR-dependent signals (4, 14, 15). However, the exact contribution of distinct nAChRs to this process is unclear. Current evidence suggests a role for α4 and α7 nAChRs. α4 nAChR is a major nAChR that has not been studied extensively in NSCLC cells. We first tested its role and found that NSCLC cell proliferation is increased by both nicotine and TC2559, an α4 nAChR agonist; TC2559 was less efficient when compared to nicotine. When tested together, TC2559 enhanced the effect of nicotine (Fig. 1A). In contrast, Dihydro-β-erythroidine, an α4 nAChR antagonist, did not affect proliferation by itself, but reduced the stimulatory effect of nicotine as determined by Luminescent Cell Viability Assay (Fig. 1A). In further support of the role of α4 nAChR, we showed that silencing of α4 nAChR by siRNA significantly attenuated the stimulatory effect of nicotine on cell proliferation; note that the control siRNA had no effect (Fig. 1B). Similar results were obtained from an additional NSCLC cell line (H2106, not shown).
Figure 1. Nicotine stimulates NSCLC cell proliferation through α4 nAChR that is diminished by rosiglitazone.
A, H1838 cells were cultured with Dihydro-β-erythroidine (DhbetaE, 1 μM) or TC2559 (0.1 μM) in the presence or absence of nicotine for up to 5 days. Afterwards, the luminescence of viable cells was detected using Cell Titer-Glo Luminescent Cell Viability Assay Kit according to the protocol of the manufacturer (Promega). All data are depicted as mean ± SD. * indicates significant difference as compared to the untreated cells group. ** indicates significant difference of combination treatment as compared the DhbetaE or TC2559 alone (P<0.05). Con, indicates untreated control cells. B, H1838 cells were transfected with control or α4 nAChR siRNA (100 nM each) for 40 hr before exposure of cells to nicotine for up to 5 days. Afterwards, the luminescence of viable cells was detected using Cell Titer-Glo Luminescent Cell Viability Assay Kit according to the protocol of the manufacturer. All data are depicted as mean ± SD. * indicates significant difference as compared to the untreated cells group. ** indicates significant difference of combination treatment as compared the nicotine alone (P<0.05). The insert on the top showed the Western blot result for α4 nAChR protein production. Con, indicates untreated control cells. C, H1838 cells were transfected with control or α4 nAChR siRNA (100 nM each) for 40 h before exposure of cells to α-bungarotoxin (α-BT, 1 μM) and nicotine for up to 5 days. Afterwards, the luminescence of viable cells was detected using Cell Titer-Glo Luminescent Cell Viability Assay Kit according to the protocol of the manufacturer. All data are depicted as mean ± SD. * indicates significant difference as compared to the untreated cells group. ** indicates significant difference of combination treatment as compared the nicotine alone (P<0.05). *** indicates significant difference of combination α4 nAChR siRNA and α-bungarotoxin (α-BT) plus nicotine treatment as compared to the α4 nAChR siRNA plus nicotine (P<0.05). Con, indicates untreated control cells.
Because of the partial response of α4 nAChR in mediating the effect of nicotine on cell growth, we next tested the role of α7 nAChR, another major nAChR that has been shown to mediate some of the mitogenic effects of nicotine (4, 16). We showed that cells silenced for α4 nAChR by siRNA and concomitantly treated with the α7 nAChR antagonist, α-bungarotoxin, showed complete blockade of the stimulatory effect of nicotine on cell proliferation (Fig. 1C). Thus, both α4 and α7 nAChRs seem to be important.
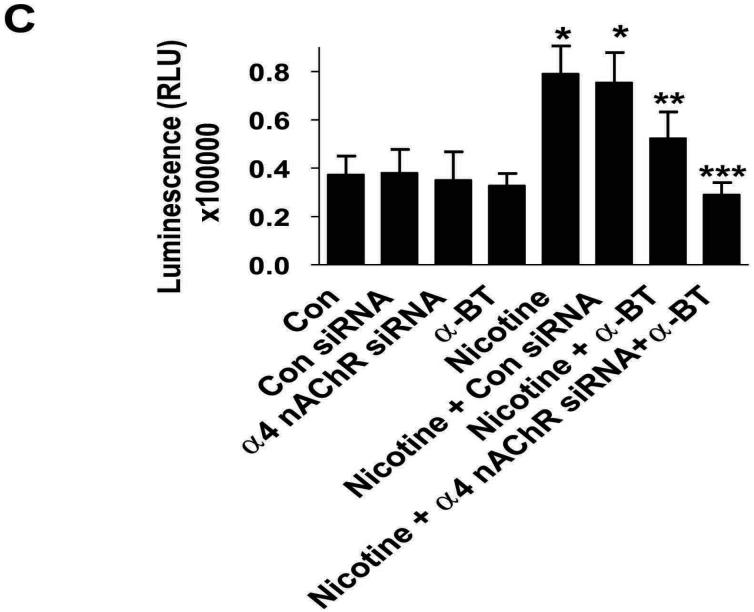
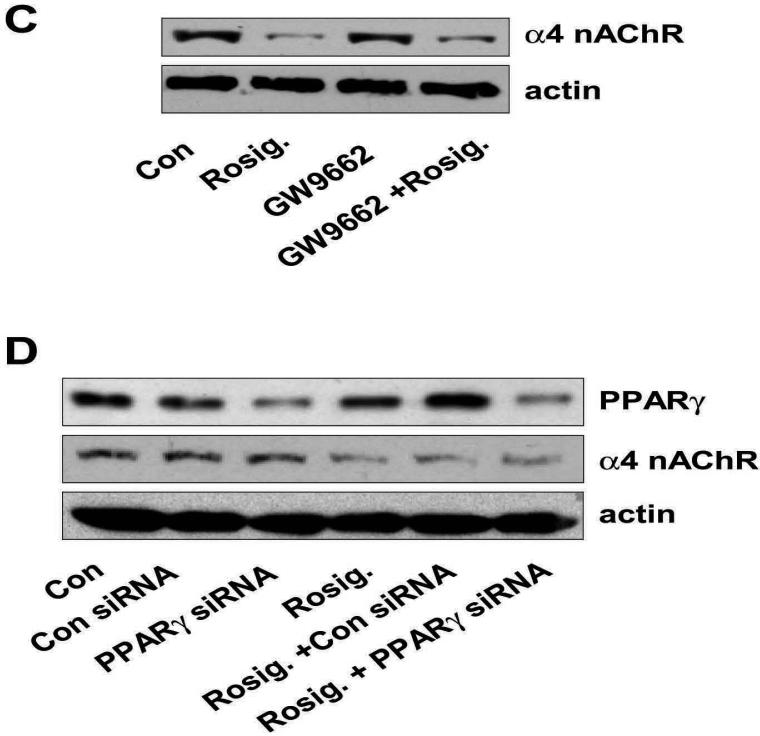
Rosiglitazone inhibits expression of α4 nAChR via a PPARγ-independent pathway
Having established the important role of α4 nAChR in nicotine-induced tumor cell proliferation, we evaluated the effect of rosiglitazone on α4 nAChR expression in the cell extracts of NSCLC cells. We showed a time- and dose-dependent inhibitory effect of rosiglitazone on α4 nAChR protein expression with a maximal effect after 24 hours of culture in the presence of 10 μM rosiglitazone (Fig. 2A and B). In order to test the role of PPARγ in mediating the effect of rosiglitazone, cells were treated with a PPARγ antagonist, GW9662, or transfected with a control or PPARγ siRNA. Interestingly, the effect of rosiglitazone on α4 nAChR protein was not affected either by GW9662 (Fig. 2C) or by the PPARγ siRNA (Fig. 2D). Similar results were obtained from other NSCLC cell lines (H2106 and A549, not shown).
Figure 2. Rosiglitazone inhibits expression of α4 nAChR in a PPARγ-independent pathway.
A, Cellular protein (20 μg) was isolated from H1838 cells treated with increasing concentrations of rosiglitazone for 24 h followed by Western blot analysis for α4 nAChR protein using an anti-α4 nAChR antibody. Blots were also incubated with an anti-actin antibody to control for gel loading. The bar graph to the right panel represents the mean ± SD of α4 nAChR/actin of at least three independent experiments. B, Cellular protein (20 μg) was isolated from H1838 cell lines cultured with rosiglitazone (10 μM) in the indicated time period. Afterward, western blot analysis was performed to α4 nAChR protein using anti-α4 nAChR antibody. The bar graph to the right panel represents the mean ± SD of α4 nAChR/actin of at least three independent experiments. The actin was used as internal control for normalization purpose. C. Cellular protein was isolated from H1838 cells cultured for 2 h in the presence or absence of GW9662 (20 μM) before exposure of cells to rosiglitazone (Rosig., 10 μM) for an additional 24 h, followed by Western blot analysis for α4 nAChR protein. Con, indicates untreated control cells. D, Cellular protein (20 μg) was isolated from H1838 cells, which were transfected with control or PPARγ siRNA (100 nM each) for 40 h before exposure of cells to rosiglitazone for an additional 24 h. afterward, Western Blot analysis were performed to determine the PPARγ and α4 nAChR protein. Blots were also incubated with an anti-actin antibody for normalization purposes. Con, indicates untreated control cells.
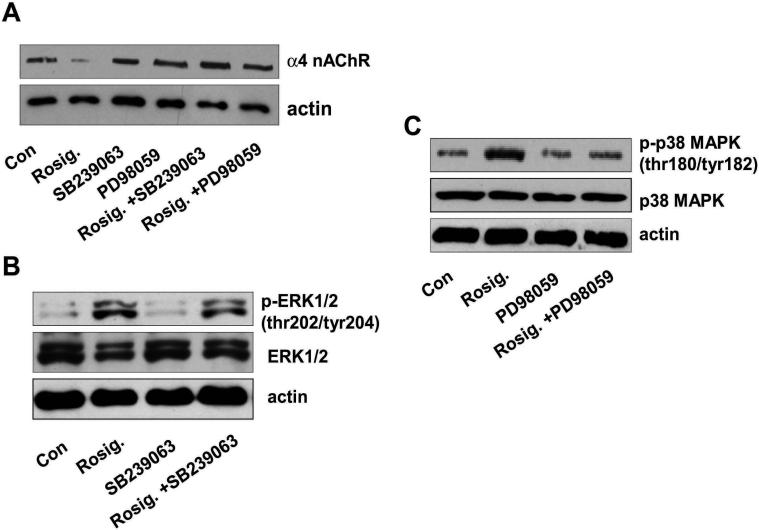
The inhibitors of p38 MAPK and ERK block the effect of rosiglitazone on expression of α4 nAChR
Because rosiglitazone appears to act via a PPARγ-independent pathway, we explored other potential signals responsible for its effects. We and others previously showed that PPARγ ligands activate kinase signaling related to p38 mitogen-activated protein kinase (p38 MAPK) and extracellular signal-regulated kinase ½ (ERK1/2) in several cell systems including lung cancer (17-19). Therefore, we tested whether regulation of α4 nAChR expression by rosiglitazone was related to p38 MAPK and ERK activation. We found that the inhibitors of p38 MAPK, SB239023, and of ERK1/2, PD98059, completely blocked the effect of rosiglitazone on α4 nAChR protein expression (Fig. 3A). Rosiglitazone stimulated the phosphorylation of both p38 MAPK and ERK. However, while SB239023 had no effect on rosiglitazone-induced phosphorylation of ERK1/2, PD98059 eliminated the stimulatory effect of rosiglitazone on phosphorylation of p38 MAPK (Fig. 3B and C) suggesting that ERK is upstream of p38 MAPK. Similar results were also found using another ERK inhibitor, U0126 (not shown). In addition, results were reproducible in other cell lines (H2106 and A549, not shown).
Figure 3. The inhibitors of p38 MAPK and ERK block the effect of rosiglitazone on expression of α4 nAChR.
A, Cellular protein (20 μg) was isolated from H1838 cells were treated with SB239023 (10 μM) or PD98059 (25 μM) for 2 h before exposure of the cells to rosiglitazone (Rosig.) for an additional 24 h. Afterwards, Western blot analysis was performed to detect the α4 nAChR protein. Actin was used for loading control for normalization purpose. Con, indicates untreated control cells. B, Cellular protein was isolated from H1838 cells treated with SB239023 (10 μM) for 1 h before exposure of the cells to rosiglitazone (Rosig.) for an additional 2 h. Afterwards, Western blot analysis was performed to detect the total ERK1/2 and phosphor-ERK1/2. Actin was used for loading control for normalization purpose. Con, indicates untreated control cells. C, Cellular protein was isolated from H1838 cells treated with PD98059 (25 μM) for 1 h before exposure of the cells to rosiglitazone (Rosig.) for an additional 2 h. Afterwards, Western blot analysis was performed to detect the total p38 MAPK and phosphor-p38 MAPK. Actin was used for loading control for normalization purpose. Con, indicates untreated control cells.
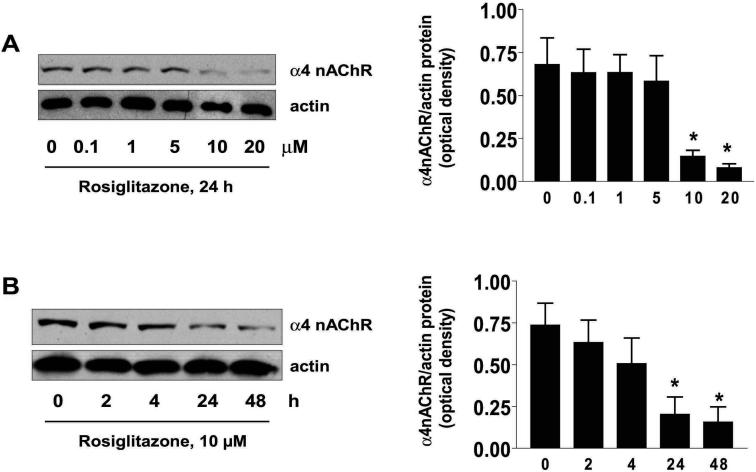
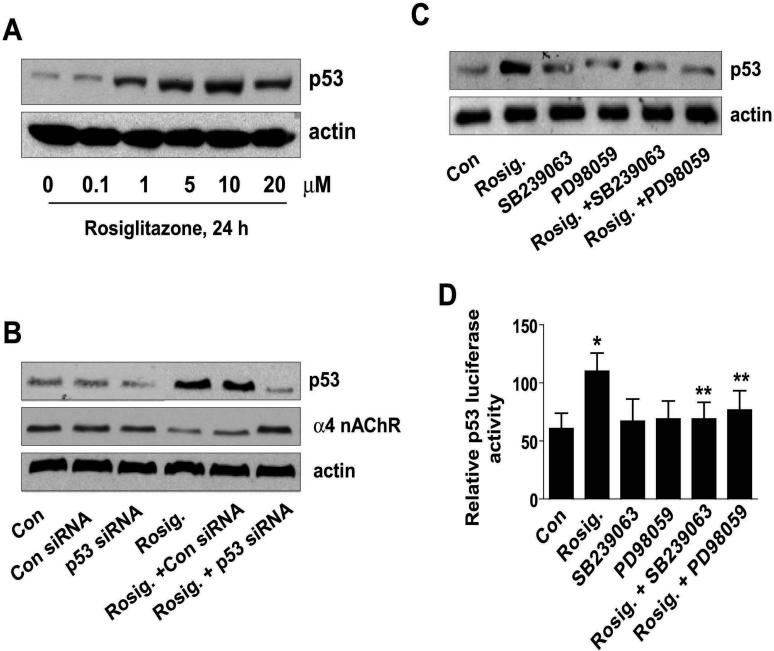
Rosiglitazone inhibits expression of α4 nAChR through p53
Rosiglitazone has been shown to increase p53 (20). Therefore, we tested if p53 played a role in mediating the effect of rosiglitazone on α4 nAChR expression. We showed that rosiglitazone indeed increased p53 protein expression in our system (Fig. 4A). Importantly, we found that silencing of p53 abolished the inhibitory effect of rosiglitazone on α4 nAChR protein expression (Fig. 4B). Consistent with a role for p53, we found that rosiglitazone did not inhibit α4 nAChR expression in H1792, a NSCLC cell line characterized by a p53 mutation (not shown). Note that the control siRNA had no effect. Similar results were obtained from another NSCLC cell line H2106 (not shown). We next assessed the role of p38 MAPK and ERK in mediating the effect of rosiglitazone on p53 protein expression and reporter activity. We showed that inhibitors of ERK and p38 MAPK blocked the stimulatory effect of rosiglitazone on p53 protein expression and p53 gene reporter activity (Fig 4C and D). This suggests that p38 MAPK and ERK are upstream of p53.
Figure 4. Rosiglitazone inhibits expression of α4 nAChR through p53.
A, Cellular protein was isolated from H1838 cells treated with increasing concentrations of rosiglitazone as indicated for 24 h followed by Western blot analysis for p53 protein using an anti-p53 antibody. Actin served as internal control for normalization purposes. B, Cellular protein (20 μg) was isolated from H1838 cells were with control or p53 siRNA (100 nM each) for 40 h before exposure of the cells to rosiglitazone (Rosig.) for an additional 24 h. Afterwards, Western blot analysis was performed to detect the p53 and α4 nAChR proteins. Actin was used for loading control for normalization purpose. Con, indicates untreated control cells. C, Cellular protein was isolated from H1838 cells cultured for up to 2 h in the presence or absence of SB239023 (10 μM), PD98059 (25 μM) before exposure of cells to rosiglitazone (Rosig., 10 μM) for an additional 24 h, then subjected to Western Blot analysis for p53 protein. Actin served as internal control for normalization purposes. Con, indicates untreated control cells. D, H1838 cells were transfected with a mixture of inducible p53-responsive firefly luciferase construct and constitutively expressing Renilla luciferase construct (40:1, 0.1μg/μl) for 24 h, then treated with SB239023 (10 μM), PD98059 (25 μM) for 1 h before exposure of the cells to rosiglitazone (Rosig., 10 μM) for an additional 24 h. The ratio of firefly luciferase to renilla luciferase activity was quantified as described in Material and Methods. The bars represent the mean ± SD of at least four independent experiments for each condition. * indicates significant increase of activity as compared to controls. ** indicates significance of combination treatment as compared with rosiglitazone (Rosig.) alone (P < 0.05). Con, indicates untreated control cells.
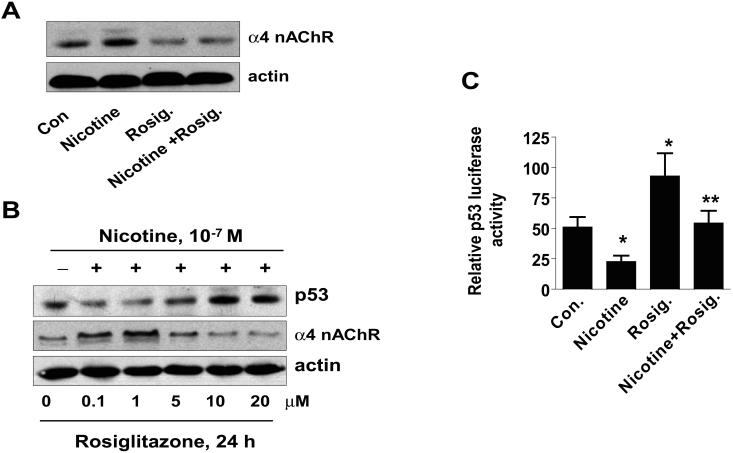
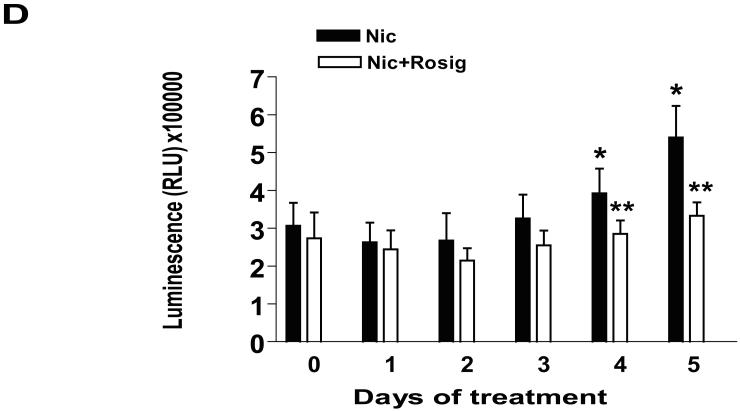
Rosiglitazone overcomes the effect of nicotine on expression of p53 and α4 nAChR, and on cell growth
Nicotine has been shown to stimulate α4 nAChR expression and this activity may serve to enhance the effects of nicotine on cell growth (3, 21). Therefore, we also explored if rosiglitazone affects this process. First, we showed that nicotine indeed stimulated α4 nAChR expression, and that rosiglitazone abolished this effect (Fig. 5A). The dose of nicotine used was based on other studies showing significant induction of α4 nAChR (22, 23). Nicotine has been shown to affect cell growth through downregulation of p53 (24). Thus, we asked whether rosiglitazone could overcome the effect of nicotine on p53, thereby explaining its ability to inhibit α4 nAChR expression even in the presence of nicotine. As shown in Fig. 5B, nicotine reduced p53 expression and induced α4 nAChR, but these were indeed overcome by rosiglitazone in a dose-dependent manner. We also found that rosiglitazone overcame the inhibitory effect of nicotine on p53 reporter activity (Fig. 5C). Rosiglitazone has been shown to inhibit NSCLC cell growth (25, 26). Therefore, we tested whether rosiglitazone antagonized the effect of nicotine on NSCLC cell proliferation. We showed that rosiglitazone reduced NSCLC cell proliferation in the setting of nicotine as determined by Luminescent Cell Viability Assay (Fig. 5D). Similar results were obtained from other NSCLC cell lines H2106 and A549 (not shown).
Figure 5. Rosiglitazone overcomes the effect of nicotine on expression of p53 and α4 nAChR.
A, Cellular protein (20 μg) was isolated from H1838 cells treated with Rosig. (10 μM) or nicotine (0.1 μM) for 24 h, or Rosig. for 2 h before exposure of the cells to nicotine for an additional 24 h, followed by Western blot analysis for α4 nAChR protein. Blots were also incubated with an anti-actin antibody for normalization purposes. Con, indicates untreated control cells. B, Cellular protein was isolated from H1838 cells treated with increasing concentrations of rosiglitazone (Rosig.) for 24 h in the presence or absence of nicotine (0.1 M) followed by Western blot analysis for p53 and α4 nAChR proteins using an anti-p53 or α4 nAChR antibodies. Actin served as internal control for normalization purposes. C, H1838 cells were transfected with a mixture of inducible p53-responsive firefly luciferase construct and constitutively expressing Renilla luciferase construct (40:1, 0.1 μg/μl) for 24 h, then treated rosiglitazone (Rosig., 10 μM) for 2 h before exposure of the cells to nicotine for an additional 24 h. The ratio of firefly luciferase to renilla luciferase activity was quantified as described in Material and Methods. The bars represent the mean ± SD of at least four independent experiments for each condition. * indicates significant increase of activity as compared to control untreated cells. ** indicates significance of combination treatment as compared with rosiglitazone (Rosig.) or nicotine alone (P < 0.05). Con, indicates untreated control cells. D, H1838 cells were cultured with rosiglitazone (Rosig., 10 μM) alone, nicotine (Nic., 100 μM) alone or Rosig. (10 μM) plus Nic. (100 μM) for 5 days. Afterward, the luminescence of viable cells was detected using Cell Titer-Glo Luminescent Cell Viability Assay Kit according to the protocol of the manufacturer. All data are depicted as mean ± SD. * indicates significant difference from day zero in Rosig. or nicotine alone. ** indicates significant difference from day zero in combination treatment (Rosig. plus nicotine) (P<0.05).
DISCUSSION
It is well known that tobacco exposure is the most important risk factor for the development of lung carcinoma in the United States (2). Nicotine, the major pharmacologically active substance in cigarette smoke, has been implicated in lung cancer development and progression (4). Nicotine acts mainly via nAChRs, which are a family of multimeric acetylcholine-triggered action channel proteins that form the predominant excitatory neurotransmitter receptors on muscles and nerves in the peripheral nervous system (27). Once considered to be restricted to neuronal cells, nAChRs are now known to be expressed in human lung epithelium and carcinoma cells (5, 28); however, their function in lung remains to be determined. While the α7 nAChR has been shown to mediate many of the effects of nicotine, the role of α4 nAChR in lung cancer progression has not been elucidated.
In view of the above, we first tested the role of a4 nAChRs in nicotine-induced NSCLC proliferation. We found that TC2559, a α4 nAChR agonist, stimulated NSCLC proliferation although not as efficiently as nicotine. In contrast, DhbetaE, an antagonist of α4 nAChRs, inhibited nicotine-induced cell proliferation. This, together with data showing that α4 nAChR siRNA inhibited the nicotine-induced response, strongly suggests a role for α4 nAChRs in mediating, at least in part, the mitogenic effects of nicotine in tumor cells. It is likely that more than one nAChR mediates the effects of nicotine and this explains the partial inhibitory effects of the antagonist. Our data suggest that α7 nAChR also contributes to the response. We and others have reported that α-bungarotoxin, an inhibitor or α7 nAChRs, also inhibits nicotine-induced cell proliferation. Here, we show that α-bungarotoxin only partially inhibited the effect of nicotine, whereas complete inhibition required both α-bungarotoxin and knockdown of the α4 nAChR suggesting that both α4 and α7 nAChRs mediate the mitogenic effects of nicotine in NSCLC.
Our studies point to α4 and α7 nAChRs as targets for anti-lung cancer therapies, and suggest that new agents with unexplained anti-cancer activity might work by affecting these receptors. Such agents are those like rosiglitazone, a synthetic PPARγ ligand with anti-inflammatory and anti-tumor properties that has been shown to inhibit human lung cancer growth through several mechanisms (19, 25, 26). We, therefore, explored the effects of rosiglitazone on the expression of α4 nAChRs in tumor cells. We found that rosiglitazone inhibited α4 nAChR protein expression in a dose and time-dependent manner. Interestingly, the inhibitory effect of rosiglitazone was independent of PPARγ since a specific chemical inhibitor of PPARγ (GW9662) and knockdown of PPARγ expression failed to abolish the effect. This is not surprising since we and others demonstrated that the actions of rosiglitazone are through PPARγ-dependent and -independent pathways (26, 29). The concentrations used here were consistent with those reported by others (30, 31). For example, Valentiner et al found that rosiglitazone inhibited in vitro growth and viability of human neuroblastoma cell lines in a dose-dependent manner showing considerable effects only at high concentrations (10 μM and 100 μM) (30). In another study, rosiglitazone inhibited both the proliferation and invasiveness of the human adrenocortical cancer cell line H295R in a dose-dependent manner with the maximal effect (about 50% inhibition) obtained at 20 μM (31).
Data from our group and others demonstrate that thiazolidinediones may activate kinase signaling pathways including p38 MAPK and ERK in normal and cancer cells (19, 32, 33). Activation of these kinases links PPARγ ligand-mediated signaling to the transcriptional regulation of genes that are crucial for cell growth inhibition. Thus, we turned our attention to testing whether these signals mediate the inhibitory effect of rosiglitazone. We showed that rosiglitazone induced the phosphorylation of both p38 MAPK and ERK½. More importantly, we showed that specific inhibitors of these signals blocked the effects of rosiglitazone. The inhibitor of ERK, PD98059, inhibited the phosphorylation of p38 MAPK suggesting that ERK lays upstream of that pathway. Crosstalk between these kinases has been reported (34, 35). In other work, p38 MAPK inhibitors were found not to affect ERK activation induced by fibroblast growth factor-2 in embryonic joint articular surface cells, and ERK inhibitors did not influence p38 MAPK phosphorylation in the same system confirming the specificity and unidirectional properties of these pathways depending on the cell types tested (35). However, opposite results have also been noted (36, 37).
We then tested the pathways downstream of ERK and p38 kinases responsible for the inhibitory effect of rosiglitazone. Thiazolidinediones including rosiglitazone have been shown to increase the expression of p53 in several tumor cells (38, 39). As a tumor suppressor gene, p53 is lost or functionally inactivated in the majority of human tumors including lung (40). p53 mutations are also frequent in tobacco-related cancers, and overexpression of p53 inhibits NSCLC growth and induces apoptosis both in vitro and in vivo (20, 41). These observations, and the fact that there are at least two p53 binding sites in the promoter region of the α4 nAChR gene (Han et al., unpublished), prompted us to investigate the role of p53 in our system. We found that rosiglitazone indeed increased p53 expression which mediated the inhibition of α4 nAChR. Furthermore, we found that this effect was blocked by inhibitors of ERKs and p38 MAPK suggesting that p53 is downstream of these signals and was not observed in a cell line with a p53 mutation. In line with this, one study demonstrated that activation of ERKs and p38 MAPK was involved in the induction of phosphorylation of p53 at multiple sites in nasopharyngeal carcinoma cells (42). Another report found that p38 MAPK formed a complex with p53 after the treatment of caffeic acid phenethyl ester and that a specific p38 MAPK inhibitor, SB203580, blocked expression and phosphorylation of p53 in glioma cells (43). Thus, rosiglitazone appears to inhibit α4 nAChR expression by activating ERK and p38 MAPK followed by induction of p53.
Finally, we examined the effects of rosiglitazone on α4 nAChR expression in the setting of nicotine exposure. Nicotine is known to stimulate the expression of its receptors (3, 21), and this is considered a feedback mechanism capable of amplifying its effects. As expected, nicotine stimulated α4 nAChR expression and this effect was associated with downregulation of p53. However, rosiglitazone overcame this effect by antagonizing the activation of PI3-K/Akt and reducing p53 and, ultimately, inhibiting α4 nAChR expression even in the presence of nicotine. Our results suggested that targeting α4 nAChR by rosiglitazone may be responsible for its ability to inhibit lung cancer cell growth.
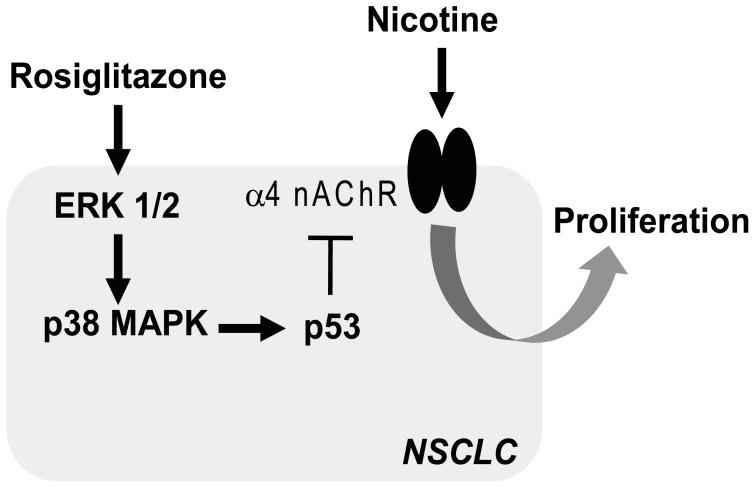
Taken together, our observations demonstrate that rosiglitazone inhibits α4 nAChR expression in NSCLC through PPARγ-independent pathways that include activation of ERK and p38 MAPK signaling. In turn, this results in induction of p53 (Fig. 6). To our knowledge, this is the first demonstration of a link between α4 nAChRs and rosiglitazone. It reveals a novel mechanism by which targeting α4 nAChRs by rosiglitazone may inhibit NSCLC proliferation and unveils a potential new target for intervention.
Figure 6. Schematic representations of signal pathways in response to rosiglitazone-inhibited NSCLC cell growth.
The PPARγ ligand, rosiglitazone, inhibits α4 nAChR expression through activation of ERK and p38 MAPK signaling followed by induction of p53 expression in a PPARγ-independent signaling. This, in turn, partially blocks α4 nAChR-mediated nicotine-induced NSCLC cell proliferation.
ACKNOWLEDGEMENT
This work was supported by American Thoracic Society (ATS)/LUNGevity Foundation Partnership Grant LC-06-004, Emory University Research Grant 2-55016, the NIH CA123104 (S. W. H), and by a Merit Review Grant from the Department of Veterans Affairs and NIH R01 CA116812 (J. R).
REFERENCES
- 1.Gilligan D, Nicolson M, Smith I, et al. Preoperative chemotherapy in patients with resectable non-small cell lung cancer: results of the MRC LU22/NVALT 2/EORTC 08012 multicentre randomised trial and update of systematic review. Lancet. 2007;369:1929–37. doi: 10.1016/S0140-6736(07)60714-4. [DOI] [PubMed] [Google Scholar]
- 2.Li MD. The genetics of nicotine dependence. Curr Psychiatry Rep. 2006;8:158–64. doi: 10.1007/s11920-006-0016-0. [DOI] [PubMed] [Google Scholar]
- 3.Tsurutani J, Castillo SS, Brognard J, et al. Tobacco components stimulate Akt-dependent proliferation and NFkappaB-dependent survival in lung cancer cells. Carcinogenesis. 2005;26:1182–95. doi: 10.1093/carcin/bgi072. [DOI] [PubMed] [Google Scholar]
- 4.Zheng Y, Ritzenthaler JD, Roman J, Han S. Nicotine Stimulates Human Lung Cancer Cell Growth by Inducing Fibronectin Expression. Am J Respir Cell Mol Biol. 2007;37:681–90. doi: 10.1165/rcmb.2007-0051OC. [DOI] [PubMed] [Google Scholar]
- 5.Lam DC, Girard L, Ramirez R, et al. Expression of Nicotinic Acetylcholine Receptor Subunit Genes in Non-Small-Cell Lung Cancer Reveals Differences between Smokers and Nonsmokers. Cancer Res. 2007;67:4638–47. doi: 10.1158/0008-5472.CAN-06-4628. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Q, Tang X, Zhang ZF, Velikina R, Shi S, Le AD. Nicotine induces hypoxiainducible factor-1alpha expression in human lung cancer cells via nicotinic acetylcholine receptor-mediated signaling pathways. Clin Cancer Res. 2007;13:4686–94. doi: 10.1158/1078-0432.CCR-06-2898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hruska M, Nishi R. Cell-autonomous inhibition of alpha 7-containing nicotinic acetylcholine receptors prevents death of parasympathetic neurons during development. J Neurosci. 2007;27:11501–9. doi: 10.1523/JNEUROSCI.3057-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson SA, Smith O, Linn DM, Linn CL. Acetylcholine neuroprotection against glutamate-induced excitotoxicity in adult pig retinal ganglion cells is partially mediated through alpha4 nAChRs. Exp Eye Res. 2006;83:1135–45. doi: 10.1016/j.exer.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 9.Tan NS, Michalik L, Desvergne B, Wahli W. Multiple expression control mechanisms of peroxisome proliferator-activated receptors and their target genes. J Steroid Biochem Mol Biol. 2005;93:99–105. doi: 10.1016/j.jsbmb.2004.12.025. [DOI] [PubMed] [Google Scholar]
- 10.Zingarelli B, Cook JA. Peroxisome proliferator-activated receptor-gamma is a new therapeutic target in sepsis and inflammation. Shock. 2005;23:393–9. doi: 10.1097/01.shk.0000160521.91363.88. [DOI] [PubMed] [Google Scholar]
- 11.Han S, Roman J. Peroxisome proliferator-activated receptor gamma: a novel target for cancer therapeutics? Anticancer Drugs. 2007;18:237–44. doi: 10.1097/CAD.0b013e328011e67d. [DOI] [PubMed] [Google Scholar]
- 12.Han S, Ritzenthaler JD, Wingerd B, Roman J. Activation of peroxisome proliferator-activated receptor beta/delta (PPARbeta/delta) increases the expression of prostaglandin E2 receptor subtype EP4 The roles of phosphatidylinositol 3-kinase and CCAAT/enhancer-binding protein beta. J Biol Chem. 2005;280:33240–9. doi: 10.1074/jbc.M507617200. [DOI] [PubMed] [Google Scholar]
- 13.Han SW, Lei ZM, Rao CV. Up-regulation of cyclooxygenase-2 gene expression by chorionic gonadotropin during the differentiation of human endometrial stromal cells into decidua. Endocrinology. 1996;137:1791–7. doi: 10.1210/endo.137.5.8612516. [DOI] [PubMed] [Google Scholar]
- 14.Dasgupta P, Rastogi S, Pillai S, et al. Nicotine induces cell proliferation by beta-arrestin-mediated activation of Src and Rb-Raf-1 pathways. J Clin Invest. 2006;116:2208–17. doi: 10.1172/JCI28164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grozio A, Catassi A, Cavalieri Z, Paleari L, Cesario A, Russo P. Nicotine, lung and cancer. Anticancer Agents Med Chem. 2007;7:461–6. doi: 10.2174/187152007781058587. [DOI] [PubMed] [Google Scholar]
- 16.Dasgupta P, Chellappan SP. Nicotine-mediated cell proliferation and angiogenesis: new twists to an old story. Cell Cycle. 2006;5:2324–8. doi: 10.4161/cc.5.20.3366. [DOI] [PubMed] [Google Scholar]
- 17.Yano M, Matsumura T, Senokuchi T, et al. Statins activate peroxisome proliferator-activated receptor gamma through extracellular signal-regulated kinase 1/2 and p38 mitogen-activated protein kinase-dependent cyclooxygenase-2 expression in macrophages. Circ Res. 2007;100:1442–51. doi: 10.1161/01.RES.0000268411.49545.9c. [DOI] [PubMed] [Google Scholar]
- 18.Li M, Lee TW, Mok TS, Warner TD, Yim AP, Chen GG. Activation of peroxisome proliferator-activated receptor-gamma by troglitazone (TGZ) inhibits human lung cell growth. J Cell Biochem. 2005;96:760–74. doi: 10.1002/jcb.20474. [DOI] [PubMed] [Google Scholar]
- 19.Han S, Zheng Y, Roman J. Rosiglitazone, an Agonist of PPARgamma, Inhibits Non-Small Cell Carcinoma Cell Proliferation In Part through Activation of Tumor Sclerosis Complex-2. PPAR Res. 2007;2007:29632. doi: 10.1155/2007/29632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fulzele SV, Chatterjee A, Shaik MS, Jackson T, Ichite N, Singh M. 15-Deoxy-Delta12,14-prostaglandin J2 enhances docetaxel anti-tumor activity against A549 and H460 non-small-cell lung cancer cell lines and xenograft tumors. Anticancer Drugs. 2007;18:65–78. doi: 10.1097/CAD.0b013e3280101006. [DOI] [PubMed] [Google Scholar]
- 21.Skok MV, Kalashnik EN, Koval LN, et al. Functional nicotinic acetylcholine receptors are expressed in B lymphocyte-derived cell lines. Mol Pharmacol. 2003;64:885–9. doi: 10.1124/mol.64.4.885. [DOI] [PubMed] [Google Scholar]
- 22.Fenster CP, Whitworth TL, Sheffield EB, Quick MW, Lester RA. Upregulation of surface alpha4beta2 nicotinic receptors is initiated by receptor desensitization after chronic exposure to nicotine. J Neurosci. 1999;19:4804–14. doi: 10.1523/JNEUROSCI.19-12-04804.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lopez-Hernandez GY, Sanchez-Padilla J, Ortiz-Acevedo A, et al. Nicotine-induced upregulation and desensitization of alpha4beta2 neuronal nicotinic receptors depend on subunit ratio. J Biol Chem. 2004;279:38007–15. doi: 10.1074/jbc.M403537200. [DOI] [PubMed] [Google Scholar]
- 24.Guo J, Chu M, Abbeyquaye T, Chen CY. Persistent nicotine treatment potentiates amplification of the dihydrofolate reductase gene in rat lung epithelial cells as a consequence of Ras activation. J Biol Chem. 2005;280:30422–31. doi: 10.1074/jbc.M504688200. [DOI] [PubMed] [Google Scholar]
- 25.Hazra S, Batra RK, Tai HH, Sharma S, Cui X, Dubinett SM. Pioglitazone and rosiglitazone decrease prostaglandin E2 in non-small-cell lung cancer cells by up-regulating 15-hydroxyprostaglandin dehydrogenase. Mol Pharmacol. 2007;71:1715–20. doi: 10.1124/mol.106.033357. [DOI] [PubMed] [Google Scholar]
- 26.Han S, Roman J. Rosiglitazone suppresses human lung carcinoma cell growth through PPARgamma-dependent and PPARgamma-independent signal pathways. Mol Cancer Ther. 2006;5:430–7. doi: 10.1158/1535-7163.MCT-05-0347. [DOI] [PubMed] [Google Scholar]
- 27.Lindstrom J. Nicotinic acetylcholine receptors in health and disease. Mol Neurobiol. 1997;15:193–222. doi: 10.1007/BF02740634. [DOI] [PubMed] [Google Scholar]
- 28.Su X, Lee JW, Matthay ZA, et al. Activation of the alpha7 nAChR reduces acid-induced acute lung injury in mice and rats. Am J Respir Cell Mol Biol. 2007;37:186–92. doi: 10.1165/rcmb.2006-0240OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Seargent JM, Yates EA, Gill JH. GW9662, a potent antagonist of PPARgamma, inhibits growth of breast tumour cells and promotes the anticancer effects of the PPARgamma agonist rosiglitazone, independently of PPARgamma activation. Br J Pharmacol. 2004;143:933–7. doi: 10.1038/sj.bjp.0705973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Valentiner U, Carlsson M, Erttmann R, Hildebrandt H, Schumacher U. Ligands for the peroxisome proliferator-activated receptor-gamma have inhibitory effects on growth of human neuroblastoma cells in vitro. Toxicology. 2005;213:157–68. doi: 10.1016/j.tox.2005.05.024. [DOI] [PubMed] [Google Scholar]
- 31.Ferruzzi P, Ceni E, Tarocchi M, et al. Thiazolidinediones inhibit growth and invasiveness of the human adrenocortical cancer cell line H295R. J Clin Endocrinol Metab. 2005;90:1332–9. doi: 10.1210/jc.2004-0978. [DOI] [PubMed] [Google Scholar]
- 32.Talbert DR, Allred CD, Zaytseva YY, Kilgore MW. Transactivation of ERalpha by Rosiglitazone induces proliferation in breast cancer cells. Breast Cancer Res Treat. 2008;108:23–33. doi: 10.1007/s10549-007-9575-y. [DOI] [PubMed] [Google Scholar]
- 33.Lennon AM, Ramauge M, Dessouroux A, Pierre M. MAP kinase cascades are activated in astrocytes and preadipocytes by 15-deoxy-Delta(12-14)-prostaglandin J(2) and the thiazolidinedione ciglitazone through peroxisome proliferator activator receptor gamma-independent mechanisms involving reactive oxygenated species. J Biol Chem. 2002;277:29681–5. doi: 10.1074/jbc.M201517200. [DOI] [PubMed] [Google Scholar]
- 34.Lewthwaite JC, Bastow ER, Lamb KJ, Blenis J, Wheeler-Jones CP, Pitsillides AA. A specific mechanomodulatory role for p38 MAPK in embryonic joint articular surface cell MEK-ERK pathway regulation. J Biol Chem. 2006;281:11011–8. doi: 10.1074/jbc.M510680200. [DOI] [PubMed] [Google Scholar]
- 35.Shimo T, Matsumura S, Ibaragi S, et al. Specific inhibitor of MEK-mediated cross-talk between ERK and p38 MAPK during differentiation of human osteosarcoma cells. J Cell Commun Signal. 2007;1:103–11. doi: 10.1007/s12079-007-0010-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goetze S, Kintscher U, Kim S, et al. Peroxisome proliferator-activated receptor-gamma ligands inhibit nuclear but not cytosolic extracellular signal-regulated kinase/mitogen-activated protein kinase-regulated steps in vascular smooth muscle cell migration. J Cardiovasc Pharmacol. 2001;38:909–21. doi: 10.1097/00005344-200112000-00013. [DOI] [PubMed] [Google Scholar]
- 37.Chang PC, Chen TH, Chang CJ, Hou CC, Chan P, Lee HM. Advanced glycosylation end products induce inducible nitric oxide synthase (iNOS) expression via a p38 MAPK-dependent pathway. Kidney Int. 2004;65:1664–75. doi: 10.1111/j.1523-1755.2004.00602.x. [DOI] [PubMed] [Google Scholar]
- 38.Yang YC, Tsao YP, Ho TC, Choung IP. Peroxisome proliferator-activated receptor-gamma agonists cause growth arrest and apoptosis in human ovarian carcinoma cell lines. Int J Gynecol Cancer. 2007;17:418–25. doi: 10.1111/j.1525-1438.2006.00866.x. [DOI] [PubMed] [Google Scholar]
- 39.Bonofiglio D, Aquila S, Catalano S, et al. Peroxisome proliferator-activated receptor-gamma activates p53 gene promoter binding to the nuclear factor-kappaB sequence in human MCF7 breast cancer cells. Mol Endocrinol. 2006;20:3083–92. doi: 10.1210/me.2006-0192. [DOI] [PubMed] [Google Scholar]
- 40.Huang CL, Yokomise H, Miyatake A. Clinical significance of the p53 pathway and associated gene therapy in non-small cell lung cancers. Future Oncol. 2007;3:83–93. doi: 10.2217/14796694.3.1.83. [DOI] [PubMed] [Google Scholar]
- 41.Li Y, Lin B, Agadir A, et al. Molecular determinants of AHPN (CD437)-induced growth arrest and apoptosis in human lung cancer cell lines. Mol Cell Biol. 1998;18:4719–31. doi: 10.1128/mcb.18.8.4719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Li L, Guo L, Tao Y, et al. Latent membrane protein 1 of Epstein-Barr virus regulates p53 phosphorylation through MAP kinases. Cancer Lett. 2007;255:219–31. doi: 10.1016/j.canlet.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 43.Lee YJ, Kuo HC, Chu CY, Wang CJ, Lin WC, Tseng TH. Involvement of tumor suppressor protein p53 and p38 MAPK in caffeic acid phenethyl ester-induced apoptosis of C6 glioma cells. Biochem Pharmacol. 2003;66:2281–9. doi: 10.1016/j.bcp.2003.07.014. [DOI] [PubMed] [Google Scholar]