Abstract
The ideal method of stem fixation in revision knee arthroplasty is controversial with advantages and disadvantages for cemented and press-fit designs. Studies have suggested cemented revision knee stems may provide better long-term survival. The aim of this study was to report our experience with press-fit uncemented stems and metaphyseal cement fixation in a selected series of patients undergoing revision total knee arthroplasty. One hundred twenty-seven patients (135 knees) who underwent revision total knee arthroplasty using a press-fit technique (press-fit diaphyseal fixation and cemented metaphyseal fixation) were reviewed. Minimum followup was 2 years (mean, 5 years; range, 2–12 years). A Kaplan–Meier survivorship analysis using an end point of revision surgery or radiographic loosening was used to determine probability of survival at 5 and 10 years. Of the 127 patients (135 knees), 31 patients (36 knees) died and two patients (two knees) were lost to followup. Six patients (six knees) had revisions at a mean of 3.5 years (range, 1–8 years). Kaplan–Meier survivorship analysis revealed a probability of survival free of revision for aseptic loosening of 98% at 12 years. Survivorship of press-fit stems for revision knee arthroplasty is comparable to reported survivorship of cemented stem revision knee arthroplasty. Radiographic analysis has shown continued satisfactory appearances regardless of constraint, stem size, and augmentations.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Revision TKA is a challenging procedure that requires adequate exposure, implant extraction, and restoration and correction of bone and ligament deficiencies while minimizing complications to achieve satisfactory results. Although the results and longevity of primary TKAs have improved, increased numbers of primary procedures have led to a continued increase in the number and need for revision knee arthroplasties [9, 14, 19, 20]. Furthermore, the survival rate and clinical outcome of revision knee arthroplasties are inferior to those of primary knee arthroplasties [4–6, 10, 14].
Routine use of stem extensions has been shown to be beneficial in improving the survival and clinical outcomes of revision knee arthroplasty [1, 5, 7, 8, 19]. The purpose of stems during revision knee arthroplasties is to endosteal reference, bypass bone defects, and reduce interface stresses of damaged bone in the distal femur and proximal tibia. The ideal method of stem fixation remains controversial with advantages and disadvantages of cemented and press-fit designs. Numerous studies have suggested there may be a benefit to the use of cemented stems for long-term survival of revision knee arthroplasties [3, 12, 15, 17, 18, 21].
We have used press-fit diaphyseal stems and metaphyseal cement fixation for the majority of revision knee arthroplasties at our institution. We wanted to review our clinical experience with this technique to see if it has provided durable middle- to long-term results. With respect to our experience using press-fit titanium fluted stems, we wanted to address the following issues: (1) What has been the functional and clinical improvement in these patients after revision as measured using the Knee Society Clinical Rating System? (2) Have there been any radiographic changes, and, if so, are these associated with the use of differing stem lengths and diameters, the use of augments, or the use of more constrained implants? (3) What has been our rerevision experience in this group of patients? (4) What is the survivorship of this technique using Kaplan–Meier survival analysis?
Materials and Methods
A retrospective analysis was conducted of data collected prospectively in a selected series of consecutive patients who had revision TKAs with a titanium fluted design (Genesis II total knee replacement; Smith & Nephew, Memphis, TN) by the authors between 1996 and 2004. At our institution during the same period, another selected series of patients had revision TKAs using solid, press-fit diaphyseal cobalt-chrome stems (Coordinate; DePuy, Warsaw, IN) and metaphyseal cement fixation, the results of which were published [13]. The unique features of the Genesis II revision TKA are improved endosteal referencing instrumentation, sizing designed to fit female (sizes 3 to 5) and male (sizes 6 to 8) patients, a highly congruent design to avoid edge loading, replication of normal patellofemoral tracking, standard and revision (4 mm thicker) patellar components, an anatomic polished tibial component that helps prevent malrotation, an enhanced tibial locking mechanism, ethylene oxide polyethylene sterilization, lower contact stresses, and a rounded hourglass-shaped post and cam rather than flat-on-flat post/cam designs to enhance post-cam contact areas. The posterior stabilized insert provides no constraint in the implant, whereas the varus-valgus constrained (VVC) insert allows ± 3° rotation and ± 2° varus-valgus movement. A wide variety of metal augment options, individual stems designed for cemented and cementless use (100-, 150-, and 200-mm stems in 2-mm increments [10- to 24-mm width]), and slotted bullet-tipped cementless stems to minimize stem tip pain are available. Patients who underwent revision of both components for any reason with stemmed implants using press-fit stems and metaphyseal cement fixation were included in our study. Patients who had revision surgery with a hinged device, revision of a failed unicompartmental arthroplasty, revision of a patellar component, exchange of a polyethylene tibial insert, single component revision, or who had less than 2 years followup were excluded.
One hundred twenty-seven patients (135 knees) met the criteria for inclusion in the study. There were 71 women and 56 men with a mean age of 71 years (range, 41–94 years) at the time of surgery. Two patients (two knees) were lost to followup after 1 year and 2 years, respectively. At last followup, the implants were functioning well and these results are included in the survivorship analysis. Thirty-one patients (36 knees) died. One patient died within 3 months of surgery from a myocardial infarct at the age of 80 years; 30 patients (35 knees) died from unrelated causes at a mean of 3 years (range, 1–9 years) after surgery. The status of the implant and latest knee function score were known at death and are included in the survivorship analysis. None of the patients who died had revision surgery before death. Only one patient who died was known to have a chronically infected implant with progressive signs of loosening at the time of death. This patient died at age 77 years, 4.6 years after undergoing a two-stage revision for an infected primary implant. The remaining 94 patients (97 knees) were followed for a minimum of 2 years (mean, 5 years; range, 2–12 years).
The mechanism of failure and indication for revision were instability in 46 (34%) knees, septic loosening in 34 (25%), aseptic loosening in 28 (21%), osteolysis in 25 (19%), and periprosthetic fracture in two (1%). The Anderson Orthopaedic Research Institute (AORI) bone defect classification at surgery revealed femoral defects of 42 Type 1A, eight Type 2A lateral, three Type 2A medial, 36 Type 2B, and nine Type 3 with 37 incomplete [11]. The tibial defects were 40 Type 1, four Type 2A lateral, 15 Type 2A medial, 11 Type 3, and 38 incomplete. The revision procedure was performed at a teaching hospital under the supervision of one of three senior consultants (SJM, RWM, RBB).
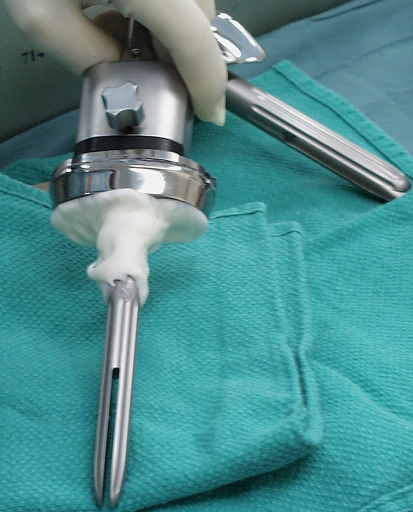
The operative technique we used was to hand ream the intramedullary canal of the femur and tibia until good cortical contact was made. In the revision system used in this study (Genesis II TKA; Smith & Nephew), the actual titanium fluted stems were 1 mm larger in diameter to allow a press-fit in the diaphysis. We cleaned and dried the cut bone surfaces before applying the cement in a doughy state to the cut surfaces without putting cement down the intramedullary canal. Cement also was applied to the undersurface and metaphyseal portion of the tibial and femoral implants to the level of the stem coupling before insertion (Figs. 1, 2). Antibiotic-impregnated cement was used routinely. The knee was held in extension until the cement had set. Care was taken to avoid cement in the medullary canal.
Fig. 1.
A clinical photograph of a revision TKA shows cement applied to the level of the tibial coupling.
Fig. 2.

A clinical photograph of a revision TKA shows cement applied to the level of the femoral coupling.
The implant had modular straight stem extensions of 100 mm, 150 mm, and 200 mm. The 100 mm was used in 15 (11%) femoral and 18 (13%) tibial components. The 150 mm was used in 111 (82%) femoral and 110 (82%) of the tibial components. The 200-mm stem was used in nine (7%) femoral and seven (5%) tibial components. Sixty-nine patients received a constrained insert (51%) and 66 patients received a posterior stabilized insert (49%). The mean diameter of the femoral stem was 16 mm (range, 10–24 mm). The mean diameter of the tibial stem was 14 mm (range, 10–24 mm).
Clinical evaluations were done using the Knee Society score and range of knee movement on all patients preoperatively and annually to latest followup. The mean scores of knee function and knee score were compared. Radiologic evaluations were done by two independent surgeons, blinded to the results (GCW, DDRN), analyzing implant position, the presence of radiolucent and radiosclerotic lines, and any progression of these lines. Radiographic analyses were done for all but 17 patients (18 knees). Nine patients (10 knees) had their films removed from the file after death; eight patients (eight knees) had missing films. Radiolucencies were recorded as definite (implant migration), probable (100% radiolucent line, greater than 2 mm), and possible (50% to 99% radiolucent line, greater than 2 mm) as adapted from Barrack et al. [2] and Harris et al. [16]. The presence of radiolucent lines was analyzed against the implant dimensions of stem length, stem diameter, augments, and level of constraint using a chi square test. The presence of radiosclerotic lines also was noted and analyzed against the use of posterior stabilized and VVC implants using a chi square test. Survivor analysis was assessed using a Kaplan–Meier curve with 95% confidence intervals using revision for any reason, revision and radiographically loose, and aseptic loosening as the end points. All data were analyzed using SPSS (Statistical Package for Social Sciences; SPSS Inc, Chicago, IL) software by an independent surgeon (GCW).
Results
Patients who underwent revision TKA using press-fit diaphyseal fixation with titanium fluted stems and cemented metaphyseal fixation showed functional and clinical improvements as measured using the Knee Society Clinical Rating System (Table 1). The mean Knee Society function and knee scores for the 88 patients (91 knees) who were living and had not had revision surgery improved from 32 (range, –20 to 80) and 38 (range, 27 to 78) points preoperatively, respectively, to 55 (range, −20 to 100) and 86 (range, 25–111) points at the final evaluation. The mean arc of flexion improved from 87° (range, 5°–140°) preoperatively to 108° (range, 15°–155°) at final evaluation. Of the 31 patients (36 implants) who died during the followup period, the mean Knee Society function and knee scores improved from 28 and 31 points, respectively, to 40 and 82 points, respectively, at latest followup before their death.
Table 1.
Knee Society scores of patients at latest followup
| Score | Mean score preoperatively | Mean latest score | Mean change |
|---|---|---|---|
| Knee | 38 | 86 | 48 |
| Function | 32 | 55 | 22 |
| Total | 69 | 135 | 69 |
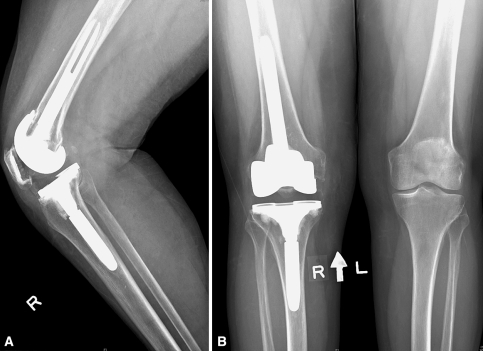
Radiographic evaluation found three knees had definite radiolucencies, and no knees had probable or possible radiolucencies. Nineteen knees (13%) with 1-mm radiolucent lines less than 50% were seen; 15 (11%) were tibial radiolucencies only, three (2%) were femoral radiolucencies only, and one knee had radiolucencies around both components (Table 2). These radiolucencies were evident on early radiographs, were not progressive, and were less than 2 mm. The eight patients (eight knees) with missing films were still alive and radiographic reports found in the notes indicated no change from previous radiographs and no evidence of radiolucent lines. No major differences were seen when comparing stem length, stem diameter, or tibial augments with incidence of radiolucent lines (chi square p > 0.1). The incidence of radiolucencies also was not significantly different between VVC and posterior stabilized inserts (p = 0.9). Progressive radiolucent lines in three knees resulted from deep infections. One patient died before revision surgery; the second patient has refused revision surgery and continues receiving chronic antibiotic suppression. This patient has a total Knee Society score of 106 at latest followup with 80° active flexion. The third patient is awaiting a staged procedure. There was no radiographic evidence of osteolysis around any of the implants. A partial or complete radiosclerotic line was observed around the cementless stems in 90% of knees (Figs. 3, 4). These radiosclerotic lines were observed on films taken at 1 year and were not observed to be progressive with time. There was no significant difference in the presence of the radiosclerotic line and the use of a posterior stabilized or VVC insert (chi square p = 0.9).
Table 2.
Radiographic analysis of radiolucent lines
| Radiolucent lines | Number | Percentage |
|---|---|---|
| None | 79 | 79% |
| Tibia | 15 | 15% |
| Femur | 3 | 3% |
| Both | 1 | 1% |
| Radiographically loose implant | 2 | 2% |
| Total | 100 | 100% |
Fig. 3A–B.
(A) Lateral and (B) anteroposterior radiographs of a revision knee arthroplasty using press-fit titanium fluted stems and metaphyseal cement fixation show the radiosclerotic line around the stems.
Fig. 4.
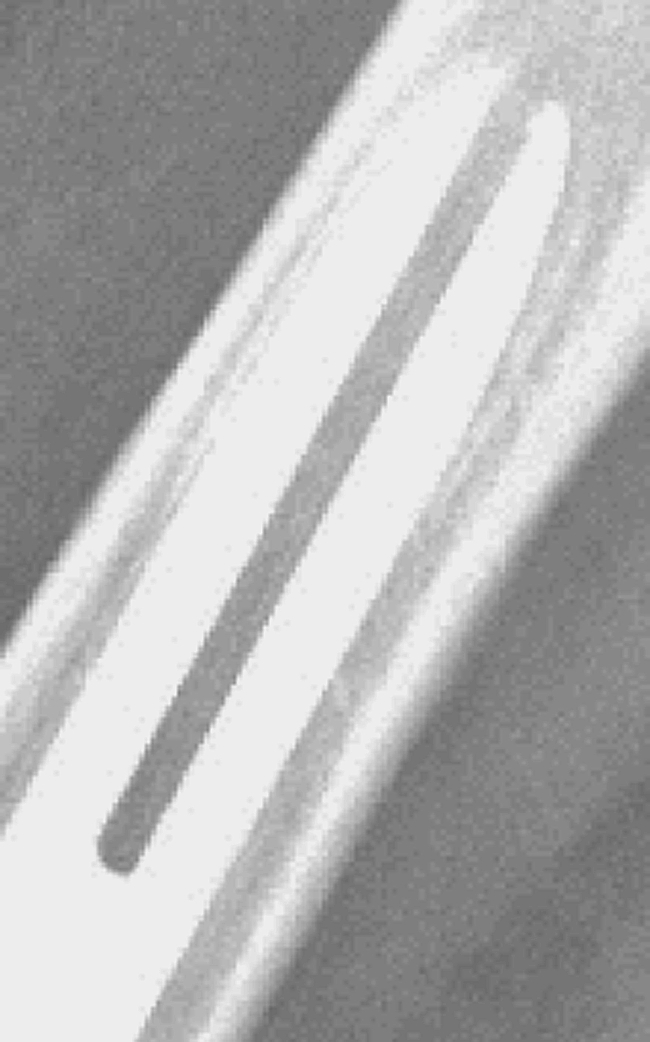
A magnified image of Fig. 3 shows the radiosclerotic line around the press-fit titanium fluted femoral stem.
Six patients (six knees) had revision surgery: two for a ruptured medial collateral ligament, two for infection, and two for aseptic loosening. The patients with rupture of the medial collateral ligament both had VVC implants previously and had conversion to a hinged prosthesis and all components were solidly fixed at the time of revision surgery. The infected implants at revision were solidly fixed and were reimplantations of previously infected knee arthroplasties. The patients who had revision surgery for aseptic loosening had a loose tibial component and the femoral component was well fixed. Each had an isolated revision of the stemmed tibial component. The operative notes of both patients who had revision surgery for aseptic loosening revealed that in one patient, the initial procedure identified a sizeable bone defect on the medial tibia (AORI Type T2-A defect) that was treated with a stepped hemiwedge and VVC insert. In the second patient, the initial procedure consisted of a revision with a minimal tibial bone defect requiring no augmentation and a posterior stabilized insert.
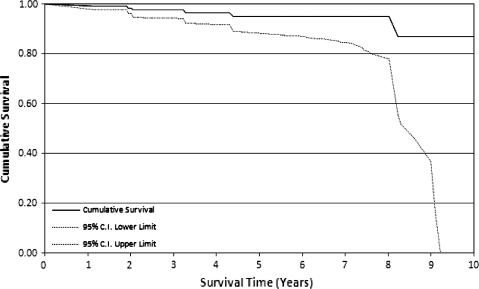
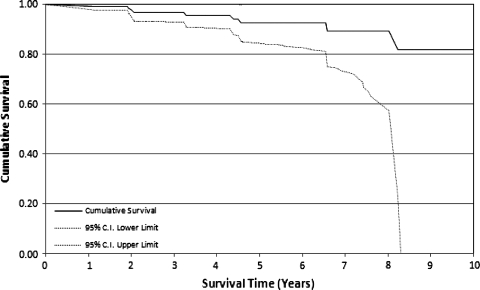
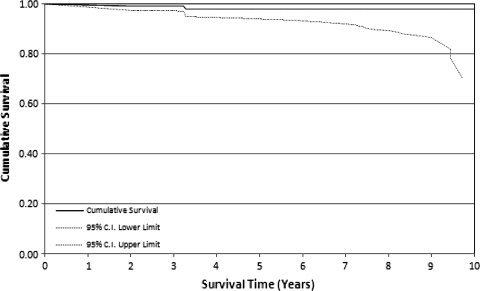
The Kaplan–Meier survivorship free of rerevision was 87% at 12 years (95% at 5 years) (Fig. 5). The Kaplan–Meier survivorship free of rerevision or radiographic loosening was 82% at 12 years (92% at 5 years) (Fig. 6). The Kaplan–Meier survivorship with aseptic loosening as an indication for rerevision was 98% at 12 years (98% at 5 years) (Fig. 7).
Fig. 5.
A Kaplan–Meier survivorship curve is shown using an end point of revision for any reason.
Fig. 6.
A Kaplan–Meier survivorship curve is shown using an end point of revision or radiographic loosening.
Fig. 7.
A Kaplan–Meier survivorship curve is shown using an end point of aseptic loosening.
Discussion
The use of cemented or press-fit stems in revision TKAs is controversial with varied results among different series with short and long-term followups (Table 3). We used press-fit diaphyseal stems and metaphyseal cement fixation for the majority of revision knee arthroplasties. Because several studies have reported excellent survivorship with fully cemented stems [12, 15, 17, 21], we wanted to review our clinical experience to see if our technique provided comparable functional, clinical, and radiographic results. Although the technique using solid press-fit diaphyseal cobalt-chrome stems with metaphyseal cement fixation has been described [13], we wanted to evaluate a selected series of consecutive patients who had revision TKAs using press-fit titanium fluted stems.
Table 3.
Summary of published studies
| Study, year | Stem fixation | Case number | Survivorship | Septic revision rate | Aseptic revision rate | Knee Society pain score preoperatively to postoperatively | Knee Society function score preoperatively to postoperatively | Average range of motion (preoperatively to latest) |
|---|---|---|---|---|---|---|---|---|
| Haas et al. 1995 [14] | Uncemented | 76 | 83% at 8 years | 4% | 2.6% at 3 years | 49–76 | 80–95 | |
| Gofton et al. 2002 [13] | Press-fit, cobalt-chrome stems | 89 | 93.5% at 8.6 years | 4.5% at 5.9 years | 15–38 | 40–52 | 88–98 | |
| Shannon et al. 2003 [19] | Uncemented | 63 | 84% at 6 years | 6% | 10% at 5.75 years | 56–81 | 49–62 | 83–101 |
| Fehring et al. 2003 [12] | Uncemented | 95 | 71% “stable” | |||||
| Cemented | 107 | 93% “stable” | ||||||
| Whaley et al. 2003 [21] | Cemented | 38 | 94% at 10 years | 2.6% | 5.3% at 10 years | 17–51 | 48–57 | 90–100 |
| Bottner et al. 2006 [6] | Uncemented | 33 | 3% | 6% at 3 years | 42–83 | 48–76 | 94–105 | |
| Mabry et al. 2007 [17] | Cemented | 73 | 92% at 10 years | 28–45 | 58–85 | 91–96 |
The current study is a retrospective review of prospectively collected data and therefore subject to the inherent limitations of this study design. Nonetheless, it represents a large consecutive series of 127 patients (135 knees) with only two patients (two knees) lost to followup. Another limitation of this study is it includes three surgeons, each with their own indications for the length and diameter of stem needed, and the amount of constraint required. Moreover, the current study is subject to surgeon bias toward the use of press-fit stems in revision TKA by the senior authors. Cemented stems were used sparingly during the study period by the senior authors in selected low-demand patients with large canals and poor bone stock. The current study also reflects some surgeon bias to the use of longer diaphyseal engaging stems, of which 89% and 87% were greater than 100 mm in length on the femoral and tibial sides, respectively.
In answering our first question, we found that in this series of patients, the Knee Society function and knee scores improved compared with preoperatively. Earlier studies of press-fit stems have had similar improvements in function and knee scores [6, 13, 14, 19]. One study of press-fit stems did not document Knee Society scores [12]. Studies of cemented stems in revision TKAs show similar improvements in function and Knee Society scores and range of motion [17, 21]. Therefore, we found no advantage in the use of press-fit stems over cemented stems for functional or clinical outcomes.
In answering our second question, we identified three knees with definite radiolucencies, all of which were the result of deep infections. This is in contrast to the finding of one study that cautioned against the use of press-fit stems because 19% of 95 stems were found to be possibly loose and 10% of stems were obviously loose radiographically at a mean of 61 months [12]. However, in that study, Fehring et al. described the use of metaphyseal engaging stems with none of the stemmed implants extending into the diaphysis. We identified 13% of knees with nonprogressive radiolucencies less than 2 mm. This is similar to percentages reported in other studies using press-fit diaphyseal engaging stems [13, 19]. We found no statistically significant correlations with the presence of these lines and the use of shorter stems, narrower stems, tibial augments, or increasing constraint. We also identified partial or complete radiosclerotic lines around 90% of knee stems but did not find a statistical correlation between the presence of these lines and increasing constraint. The presence of these lines was noted in a previous study using solid diaphyseal press-fit cobalt-chrome stems in revision TKAs [13]; however, no correlation was found between the presence of these lines and clinical outcomes in that study. Unlike in the current study, radiosclerotic lines were more common in patients having more articular constraint [13]. The presence of incomplete parallel sclerotic lines has been reported around 90% of uncemented diaphyseal engaging femoral stems and 97% of tibia stems from another center [19]. The importance of these lines remains unknown.
In answering our fourth question, we had to perform rerevisions in six patients (six knees) in the current study. Four patients (four knees) required extraction of femoral and tibial components, which were found to be solidly fixed at the time of rerevision. Two patients (two knees) required extraction of the tibial component only. It has been our experience that extracting press-fit stems, although difficult, is bone-conserving in contrast to removal of fully cemented stems. Press-fit diaphyseal engaging stems in revision TKA are not designed to achieve ingrowth and do not appear to allow ongrowth as occurs in cementless primary or revision THA stems. Avoiding cement in the intramedullary canal and facilitating rerevision is the main rationale behind our use of press-fit diaphyseal stems, which we believe is particularly important in patients who require removal of well-fixed implants secondary to infection and in patients who are expected to have another revision during their lifetime.
In answering our final question, we report a survival rate of 98% at 12 years for aseptic loosening and 87% at 12 years for revision for any reason. In the current series, we had two revisions for aseptic loosening (1.5%) and both occurred early with no other components radiographically loose. This is less than the 4.5% aseptic loosening rate in our previous series using cobalt-chrome stems [13]. This rate also is less than the rates reported in other studies [6, 19]. Long-term survivorship using cemented stems was reported in one study to be 96.7% using revision for any reason as an end point and 95.7% using component survival free of aseptic loosening as an end point at 11 years [21]. In another study, the survival rate of 73 cemented stems in revision TKAs was 92% at 10 years for aseptic loosening and 89% for revision for any reason [17]. The slightly lower septic loosening rates in series using cemented revision stems could be explained by the additional antibiotic delivery in the intramedullary canals in these series; however, antibiotics routinely were added to metaphyseal cementation in our current series.
The results of this study suggest press-fit stems can provide similar functional and clinical outcomes as cemented stems in revision knee arthroplasties. Radiographic analysis has shown continued satisfactory appearances regardless of stem length and diameter, the use of augments, or increasing constraint. Survivorship of press-fit stems is comparable to reported long-term survivorship of cemented stems with the rate of recurrent septic loosening comparable to those reported for fully cemented revision stems. Others continue to advocate for the routine use of cemented stems in revision TKAs [12, 17, 21], however we do not believe there is a clear advantage for routine use of fully cemented stems in revision TKAs.
Footnotes
One or more of the authors (DDRN, SJM, RWM, RBB) have received funding from Smith & Nephew, DePuy, and Stryker.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that Institutional Review Board approval for this study was obtained.
References
- 1.Albrektsson BE, Ryd L, Carlsson LV, Freeman MA, Herberts P, Regnér L, Selvik G. The effect of a stem on the tibial component of knee arthroplasty: a roentgen stereophotogrammetric study of uncemented tibial components in the Freeman-Samuelson knee arthroplasty. J Bone Joint Surg Br. 1990;72:252–258. [DOI] [PubMed]
- 2.Barrack RL, Mulroy RD Jr, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty: a 12-year radiographic review. J Bone Joint Surg Br. 1992;74:385–389. [DOI] [PubMed]
- 3.Barrack RL, Stanley T, Burt M, Hopkins S. The effect of stem design on end-of-stem pain in revision total knee arthroplasty. J Arthroplasty. 2004;19(suppl 2):119–124. [DOI] [PubMed]
- 4.Bartel DL, Burstein AH, Santavicca EA, Insall JN. Performance of the tibial component in total knee replacement. J Bone Joint Surg Am. 1982;64:1026–1033. [PubMed]
- 5.Bertin KC, Freeman MA, Samuelson KM, Ratcliffe SS, Todd RC. Stemmed revision arthroplasty for aseptic loosening of total knee replacement. J Bone Joint Surg Br. 1985;67:242–248. [DOI] [PubMed]
- 6.Bottner F, Laskin R, Windsor RE, Haas SB. Hybrid component fixation in revision total knee arthroplasty. Clin Orthop Relat Res. 2006;446:127–131. [DOI] [PubMed]
- 7.Bourne RB, Finlay JB. The influence of tibial component intramedullary stems and implant-cortex on the strain distribution of the proximal tibia following total knee arthroplasty. Clin Orthop Relat Res. 1986;208:95–99. [PubMed]
- 8.Brooks PJ, Walker PS, Scott RD. Tibial component fixation in deficient tibial bone stock. Clin Orthop Relat Res. 1984;184:302–308. [PubMed]
- 9.Dixon T, Shaw M, Ebrahhim S, Dieppe P. Trends in hip and knee joint replacement: socioeconomic inequalities and projections of need. Ann Rheum Dis. 2004;63:825–830. [DOI] [PMC free article] [PubMed]
- 10.Donaldson WF 3rd, Sculco TP, Insall JN, Ranawat CS. Total condylar III knee prosthesis: long-term follow-up study. Clin Orthop Relat Res. 1988;226:21–28. [PubMed]
- 11.Engh GA, Ammeen DJ. Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect. 1999;48:167–175. [PubMed]
- 12.Fehring TK, Odum S, Olekson C, Griffin WL, Mason JB, McCoy TH. Stem fixation in revision total knee arthroplasty: a comparative analysis. Clin Orthop Relat Res. 2003;416:217–224. [DOI] [PubMed]
- 13.Gofton WT, Tsigaras H, Butler RA, Patterson JJ, Barrack RL, Rorabeck CH. Revision total knee arthroplasty: fixation with modular stems. Clin Orthop Relat Res. 2002;404:158–168. [DOI] [PubMed]
- 14.Haas SB, Insall JN, Montgomery W 3rd, Windsor RE. Revision total knee arthroplasty with use of modular components with stems inserted without cement. J Bone Joint Surg Am. 1995;77:1700–1707. [DOI] [PubMed]
- 15.Hanssen AD. Cemented stems are requisite in revision knee replacement. Orthopedics. 2004;27:990, 1003. [DOI] [PubMed]
- 16.Harris WH, McCarthy JC Jr, O’Neill DA. Femoral component loosening using contemporary techniques of femoral cement fixation. J Bone Joint Surg Am. 1982;64:1063–1067. [PubMed]
- 17.Mabry TM, Vessely MB, Schleck CD, Harmsen WS, Berry DJ. Revision total knee arthroplasty with modular cemented stems: long-term follow-up. J Arthroplasty. 2007;22(suppl 2):100–105. [DOI] [PubMed]
- 18.Murray PB, Rand JA, Hanssen AD. Cemented long-stem revision total knee arthroplasty. Clin Orthop Relat Res. 1994;309:116–123. [PubMed]
- 19.Shannon BD, Klassen JF, Rand JA, Berry DJ, Trousdale RT. Revision total knee arthroplasty with cemented components and uncemented intramedullary stems. J Arthroplasty. 2003;18(suppl 1):27–32. [DOI] [PubMed]
- 20.Sheng PY, Konttinen L, Lehto M, Ogino D, Jämsen E, Nevalainen J, Pajamäki J, Halonen P, Konttinen YT. Revision total knee arthroplasty: 1990 through 2002. A review of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2006;88:1425–1430. [DOI] [PubMed]
- 21.Whaley AL, Trousdale RT, Rand JA, Hanssen AD. Cemented long-stem revision total knee arthroplasty. J Arthroplasty. 2003;18:592–599. [DOI] [PubMed]