Abstract
Femoroacetabular impingement is a motion-based concept of conflict that occurs secondary to morphologic abnormalities of the proximal femur and/or acetabulum. Creating impingement-free motion through restoration of normal morphology serves as the goal of joint-preserving procedures. We retrospectively reviewed the short-term functional and radiographic outcomes of 46 patients (48 hips) with femoroacetabular impingement treated with a surgical dislocation and restoration of offset. The average Merle D’Aubigné-Postel score improved from a preoperative of 13 (range, 7–16 ± 1.7) to a postoperative score of 16.8 (range, 12–18 ± 1.3). Creating impingement-free motion via a surgical dislocation improves symptoms in patients with limited radiographic signs of arthritis who are experiencing impingement-related hip pain.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
The concept of idiopathic or primary osteoarthritis of the hip has been questioned for years [7, 9, 22]. As knowledge of the joint has progressed, the percentage of cases labeled primary has decreased [8]. Initially, attention was centered on altering the static coronal plane relationships between the proximal femur and acetabulum [13, 17]. Within the last 15 years, the dynamic concept of femoroacetabular impingement has gained acceptance as a causative factor related to the development of hip pain and osteoarthritis.
Impingement in a ball-and-socket joint takes two primary forms: acetabular overcoverage and an inappropriate proximal femoral contour [8, 16]. Most often a combination of factors leads to mismatch; however, proximal femoral contour abnormalities typically predominate. Recognizing and addressing all factors associated with impingement should both decrease symptoms and delay progression or potentially prevent the development of hip arthritis [1, 7, 8, 15]. Through a detailed understanding of the vascular anatomy of the proximal femur, a safe method of surgical dislocation was developed [6]. This approach has allowed for reshaping the proximal femur and acetabular walls, as well as treatment of the secondary labral pathology [11].
Previous published reports have documented an improvement in outcome scores after surgical dislocations to treat femoroacetabular impingement [2, 5, 15]. Surgical treatments have varied, both by the decision to resect or reattach the labrum and by the chosen surgical approach [5, 18, 19].
As recognition of this disease and its treatments are relatively recent, we evaluated our results to either confirm or refute previous findings. Specifically the purpose of this paper was to (1) report clinician-based short-term outcomes, as measured by the Merle D’Aubigné-Postel score, of patients with femoroacetabular impingement treated with a surgical dislocation via a trochanteric osteotomy, and (2) ensure the surgical approach is associated with osteotomy healing and the absence of femoral neck fractures.
Materials and Methods
We retrospectively reviewed the clinical records and radiographs of 51 selected patients with a diagnosis of femoroacetabular impingement who had failed nonoperative management and were treated with an open surgical dislocation of the hip [6] from May 2000 to September 2003. Five patients had inadequate preoperative or postoperative data for inclusion in the study group. This left 46 patients for evaluation. Two of these 46 patients had bilateral hip procedures, creating a study group of 48 hips. The indications for surgical intervention included skeletally mature patients with consistent clinical and radiographic findings of femoroacetabular impingement who had failed at least 1 month of conservative management including activity modification and NSAIDs. Exclusion criteria included skeletally immature patients and patients with advanced hip osteoarthritis evidenced by Tönnis grade 3 findings [22]. The average age of the patients was 33 years (range, 18–51 years). There were 21 women and 25 men. Twenty-one left hips and 27 right hips underwent surgery. The minimum followup time for a postoperative questionnaire (Appendix 1) was 6 months (mean, 38 months; range, 6–67 months); all patients in the study group completed the questionnaire. The minimum radiographic followup was 1 month (mean, 12 months; range, 1–60 months); this was compromised by 16 patients having followup visits in the patient’s state of residence. Prior to the review, the study received institutional ethics review board approval.
Onset of pain was initially activity-related, but in 42 patients became constant. All patients localized pain to the groin area and had a positive impingement test [12]. The average duration of symptoms between onset and surgery was 42 months (range, 1–132 months). Thirty-five of 46 were taking NSAIDs for pain control. Eleven of the 46 were taking narcotics. Three of the 46 had previous arthroscopic hip surgery. Eleven of the remaining had other previous hip procedures (open relocation, irrigation and débridement, ORIF of femoral neck fracture, iliopsoas tenotomy, IT band tenotomy, trochanteric bursectomy, benign tumor resection, periacetabular osteotomy, intertrochanteric osteotomy, and removal of a dynamic hip screw from a previous femoral neck fracture).
Radiographic evaluation included an AP pelvis, AP hip, faux-profile view, and cross-table lateral view of the involved hip. AP pelvis radiographic adequacy was evaluated based on previous cadaveric radiographic positioning studies [21]. To clarify, the pelvic tilt was documented by the relative position of the sacrococcygeal joint and the pubic symphysis compared to average population values. To ensure we appropriately assessed retroversion, we documented and ensured proper pelvic rotation by comparing the position of the coccyx with respect to the symphysis, as well as the symmetry of the obturator foramina and iliac wings. One of us not associated with the surgery (MG) documented from the AP pelvis the following preoperative findings: acetabular retroversion, coxa profunda, protrusio, pistol grip deformity, aspherical femoral head, coxa vara, coxa valga, herniation pits, Tönnis OA classification [22], lateral center-edge angle, acetabular index, anterior center-edge angle, and the amount of cartilage space of the superior joint measured in millimeters above the center of the femoral head. The acetabulum was defined as retroverted if the anterior border crossed the posterior border medial to the lateral edge of the acetabulum [20]. Coxa profunda was defined as the floor of the fossa acetabuli contacting the ilioischial line, when associated with a center edge angle of greater than 35 degrees [2]. Protrusio was defined as the medial aspect of the femoral head contacting the ilioischial line with an associated center-edge angle of greater than 40°. A pistol grip deformity of the femoral head was defined as an extension of the lateral epiphysis down to the base of the femoral neck [9]. An aspherical head was defined as an extension of the lateral epiphysis onto the cephalad neck creating a nonspherical head. This was corroborated by evaluating the cross-table lateral view of the hip [4]. Coxa vara was defined by a neck-shaft angle less than 125° in association with the tip of the trochanter being greater than or equal to 5 mm above the center of the femoral head. Coxa valga was defined by a neck-shaft angle greater than 135° in association with the tip of the trochanter being greater than or equal to 5 mm below the center of the femoral head.
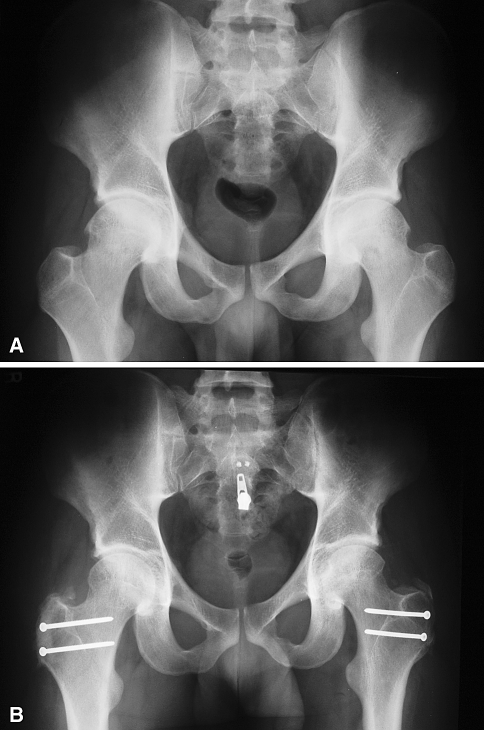
All hips on plain radiographs had insufficient femoral head-neck offset. The offset was considered inadequate if a the epiphysis extended outside of a circle drawn around the femoral head [4]. This was often notable on both the cross-table lateral and the anteroposterior hip view. Thirty-six of 48 hips had pure cam impingement, defined by primary proximal femoral pathology [10] (Fig. 1A–B). The remaining 12 had a mixed deformity with signs of primary proximal femoral and acetabular pathology [8]. There were no pure pincer impingement cases in this series (Table 1).
Fig. 1A–B.
(A) This preoperative AP pelvis of a patient in the series reveals radiographic signs of bilateral cam impingement. (B) This postoperative AP pelvis was taken 14 months after surgery on the right side. Bilateral surgical hardware is noted, reflecting the patient satisfaction with the initial unilateral treatment.
Table 1.
Radiographic pathology
| Pathology | Number |
|---|---|
| Acetabular retroversion | 12 |
| Coxa profunda | 7 |
| Protrusio acetabuli | 1 |
| Pistol grip deformity | 1 |
| Aspherical femoral head | 45 |
| Coxa vara | 6 |
| Coxa valga | 7 |
| Herniation pits | 7 |
| Tönnis OA classification | |
| Class 0 | 37 |
| Class 1 | 10 |
| Class 2 | 1 |
We performed a preoperative gadolinium-enhanced arthrographic MRI on all but one hip (47 of 48). Almost all were completed and read by the same musculoskeletal radiologist (TL) with specialized training in arthrographic MRI. Documented pathology included loss of head/neck offset, the type and location of labral damage (all labral damage located between 10 o’clock and 2 o’clock except ossification that often extended posteroinferiorly), the type of acetabular and femoral head cartilage damage, and the presence of herniation pits (Table 2).
Table 2.
MRI pathology
| Pathology | Number |
|---|---|
| Loss of head/neck offset | 38 |
| Labral damage | |
| Undersurface tear | 14 |
| Base tear | 20 |
| Ossification | 11 |
| Thickening | 4 |
| Acetabular cartilage damage | |
| Thinning | 25 |
| Delamination | 8 |
| Femoral head cartilage damage | |
| Thinning | 8 |
| Herniation pits | 13 |
The common goal of all procedures was restoring impingement-free motion. All patients underwent a surgical dislocation through a modification of the Gibson approach and osteochondroplasty of the head-neck junction [8]. The other procedures were varied based on preoperative evaluation and intraoperative findings. Acetabuloplasty (trimming of the acetabular rim) was performed to decrease overcoverage. The labrum was never excised in this series. The portion of the labrum that was damaged was débrided, with the remainder undergoing repair to the acetabular rim. Rim fractures were excised or repaired based on the degree of coverage, with the goal to prevent undercoverage. Abrasion chondroplasty was performed after cartilage flap débridement when necessary in an attempt to initiate fibrocartilage formation. Additional procedures in the series included relative femoral neck lengthening, intertrochanteric osteotomy for coxa vara, lateralization of the greater trochanter, osteochondral grafting of femoral head cartilage defects, curtain osteophyte resection, sciatic neurolysis, and loose body removal (Table 3).
Table 3.
Intraoperative procedures
| Procedure | Number |
|---|---|
| Osteochondroplasty | 48 |
| Acetabuloplasty - rim trimming | 12 |
| Labral débridement and repair | 34 |
| Rim fracture treatment | |
| Excision | 1 |
| Fixation | 1 |
| Abrasion chondroplasty | 21 |
| Relative femoral neck lengthening | 2 |
| Valgus intertrochanteric osteotomy | 1 |
| Greater trochanteric lateralization | 4 |
| Osteochondral grafting of femoral head | 2 |
| Curtain osteophyte resection | 3 |
| Sciatic neurolysis | 1 |
| Loose body removal | 1 |
Labral and cartilage damage were localized by translating left and right hips into a right hip clock face system with 12 o’clock located superiorly, 6 o’clock located inferiorly, 3 o’clock located anteriorly, and 9 o’clock located posteriorly. Intraoperative data correlated with preoperative MRI findings.
A first-generation cephalosporin was given preoperatively and continued until the drain was removed. Drains were removed once less than 30 mL was noted over a 24-hour period. Thromboembolic prophylaxis consisted of a low-molecular-weight heparin while in the hospital. Upon discharge, a buffered aspirin was given daily for 6 weeks.
Postoperative physical therapy consisted of a continuous passive motion machine while in the hospital. This was initially set at 30° and advanced 5° per day until discharge. Active assisted range of motion began immediately and advanced to resistance exercises once the greater trochanter showed radiographic signs of union. Postoperative weight-bearing protocol included weight-of-leg weight bearing for 6 weeks using crutches or a walker. If radiographs revealed greater trochanteric healing at 6 weeks, single crutch progressive weight bearing began and continued for 2 weeks. Patients were allowed full weight bearing without an assistive device after this time.
Patient clinical outcome was assessed using the Merle D’Aubigné-Postel score [14]. As noted previously, 16 patients had followup out of state. In addition to receiving the followup clinic notes from the local orthopaedic surgeons, we (MG) contacted these patients and/or their doctors by phone or mailed them questionnaires (Appendix 1). This combination allowed us to get Merle D’Aubigné-Postel scores on the out-of-state patients. The standard followup protocol was 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and yearly thereafter.
Radiographs were taken at 6 weeks, 12 weeks, and yearly thereafter. An attempt was made to obtain radiographs from all out-of-state patients who were followed by other orthopaedic surgeons. We were able to locate followup radiographs on 38 of the 46 patients. The same observer evaluated the followup radiographs for the same preoperative variables as well as the Brooker classification of heterotopic ossification [3]. We assessed offset by noting whether or not there was a clear difference in the head-neck junction (ie, an extended lateral epiphysis).
Outcome scores were first evaluated for the normality of distribution of the data. We did not find a normal distribution with the Merle d’Aubigné-Postel scores, and therefore used the Wilcoxon signed rank test (SPSS Incorporated, Chicago, IL).
Results
Forty-six of 48 hips (96%) showed a postoperative improvement in outcome score. The mean Merle d’Aubigné-Postel score improved (p < 0.001) from a preoperative score of 13 (range, 7–16 ± 1.7) to a postoperative score of 16.8 (range, 12–18 ± 1.3).
We noted radiographic restoration of normal hip offset in all patients immediately postoperatively. Nine of 48 (19%) had Class 1 ossification; the remainder had no signs of heterotopic bone formation. All trochanteric osteotomies healed. Two patients had symptoms related to screw placement in the greater trochanter. Both had screw removal with improvement in symptoms. There were no wound healing complications or infections. There were no cases of thromboembolic disease, nerve palsy, or postoperative femoral neck fracture. No hips have had radiographic signs of avascular necrosis to this point. Definitive statements regarding avascular necrosis and progression of osteoarthritis cannot be made as our radiographic followup is limited secondary to multiple patients being followed out of state.
Discussion
Previous published reports have documented an improvement in outcome scores after surgical dislocations to treat femoroacetabular impingement [2, 5, 15]. Surgical treatments have varied, both by the decision to resect or reattach the labrum and by the chosen surgical approach [5, 18, 19]. We evaluated our results to either confirm or refute previous findings. Specifically, the purpose of this paper was to report clinician-based short-term outcomes, as measured by the Merle D’Aubigné-Postel score of patients with femoroacetabular impingement treated with a surgical dislocation via a trochanteric osteotomy. In addition, we evaluated short-term radiographic followup to ensure the safety of the surgical approach through documentation of osteotomy healing and the absence of femoral neck fractures.
Our study has clear limitations. First, approximately 10% of the original study group (five of 51 patients) did not have the necessary preoperative and postoperative outcome data to be included in the final evaluation. Of these five patients, one did ultimately undergo THA. That patient had preoperative radiographic evidence of advanced osteoarthritis (Tönnis grade 2) prior to his surgical dislocation. Inclusion of this patient would have altered the results. The remaining four excluded patients reported improvement in symptoms based on the last followup clinic note but could not be contacted for postoperative outcome scores. Second, the time between surgery and radiographic followup was limited secondary to the wide geographic range of the patient population. Approximately one-third (16 of 46) of the patients continue to followup with local orthopaedic surgeons, creating logistical problems in obtaining the radiographs. Because of this, no firm conclusions can be reached regarding the risk of avascular necrosis or the progression of osteoarthritis. Third, this is a retrospective review with no case control. Information bias may be present as the operating surgeon (JM) performed the majority of the postoperative evaluations. The common but nonvalidated outcome instrument used in the study was taken from these postoperative evaluations. Of note, no comparison of preoperative and postoperative range of motion profile is provided. This is secondary to the difficulty of obtaining all the detailed data required from the patients following up with local orthopaedic surgeons. Selection bias may also be present as nearly one-third of the patients had the ability to travel across the country to have this procedure performed. Finally, this data is from the early stages of treatment of femoroacetabular impingement. The indications for rim fracture fixation versus excision, acetabular rim trimming versus periacetabular osteotomy, and the need for proximal femoral osteotomies were and are still evolving.
The clinician-based Merle D’Aubigné-Postel outcome scores improved in 46 of the 48 (96%) hips that underwent surgery. These findings are consistent with previous studies reporting short- or intermediate-term results using the same outcome measure (Table 4) [2, 5, 15]. In addition, patient-based disease-specific, and health-related outcome questionnaires have been used to reflect a substantial improvement in the overall quality of life of most patients undergoing this surgery [1]. These series provide some limited evidence of the generalizability of the technique, although all studies took place in very specialized centers with experienced hip surgeons. More importantly, the series provide evidence that the short-term results of joint-preserving impingement surgery are good when evaluated by many different types of outcome measures. This finding is even more notable considering the complexity of this group of patients. The complexity is evidenced in two specific ways. Multiple patients in this group had previous surgical attempts at pain relief. In addition, various proximal femoral abnormalities were noted and treated in addition to impingement lesions, including osteochondral disease or trochanteric offset.
Table 4.
Published series of open dislocations using Merle d’Aubigne score
| Number of hips | Average preoperative score | Postoperative score | Level of significance | Average followup time | |
|---|---|---|---|---|---|
| Beck M, et al. Clin Orthop 2004 [2] | 19 | 14.1 | 16.5 | p = .015 | 4.7 years |
| Murphy S, et al. Clin Orthop 2004 [15] | 23 (scores for surviving 15 hips) | 13.2 | 16.9 | p < .0001 | 5.2 years |
| Espinosa N, et al. J Bone Joint Surg 2006 [5] | Group 1 (labral resection)—25 | 12 | 15 | p = .0009 | 2 years |
| Group 2 (labral reattachment)—35 | 12 | 17 | p < .0001 | 2 years | |
| Graves M, Mast J. Clin Orthop 2008 | 48 | 13 | 16.8 | p < .001 | 3.2 years |
Short-term radiographic followup was positive, but limited conclusions can be drawn from the data at the present time. Correction of the offending preoperative lesion was noted in all cases. The limited number of trochanteric osteotomy complications was noticeable (no cases of trochanteric nonunion and two cases of trochanteric bursitis, both relieved with hardware removal). This is consistent with the Berne data [2, 5], but differs slightly from the data reported from California [1]. Trochanteric fixation constructs were similar in all studies, typically consisting of two small fragment cortical screws placed from the lateral aspect of the greater trochanter into the medial calcar area of the proximal femur. Initial trochanteric fixation in the California study consisted of large fragment cortical screws, which could account for the higher percentage of symptomatic hardware in that group. Heterotopic bone formation was noted; however, it was never greater than Brooker Grade 1 [3]. More extensive heterotopic ossification has been noted previously, but appears to be a rare occurrence based on the published literature [1]. We have observed no signs of avascular necrosis to date, but the length of radiographic followup is inadequate to make definitive statements about this potential postoperative complication. Secondary to the limited radiographic data available, no statement can be made regarding the progression of osteoarthritis.
Short-term followup suggests that an open surgical dislocation relieves pain and improves function without many short-term complications. Our data are consistent with other reports using patient-reported general and disease-specific outcomes, as well as clinician-reported outcomes [1, 2, 5, 15]. We believe caution should be used in patient selection. Based on previously published studies, hips with more advanced signs of arthritis have not fared as well with this procedure [1, 2, 15]. Longer-term data collection is necessary to document the long-term benefits of creating impingement-free motion.
Acknowledgments
We thank Dr. Thaddeus Laird for his expertise and time commitment in reading and performing the arthro-MRIs.
Appendix 1. Patient Questionnaire
- Are you experiencing pain? If so, how would you rate it?
- None
- Mild, occasional
- Moderate to severe
- Marked severity limiting function
- Totally disabled
- Are you taking medications?
- None
- Antiinflammatories
- Narcotics
- What is your best ambulatory function?
- Running
- Walking
- Do you participate in exercise?
- Impact sports
- Non-impact sports
- No exercise or inactive
- Describe your stamina for walking?
- Unlimited
- > 1 mile
- 0.5–1 mile
- < 0.5 miles
- Can you climb stairs?
- Without a banister
- With a banister
- Can’t climb stairs
- Can you don shoes and socks?
- Without difficulty
- With difficulty
- Not at all. Need assistance.
- Do you require any walking aids?
- None
- Cane
- Crutches
- Wheelchair
- Describe your sitting abilities.
- A chair of any height
- Only in high chairs
- Can’t sit in a chair
- Are you currently limping?
- Not at all
- Occasionally when tired
- Always
- Always and require an external support of some type
- Describe your feelings regarding the operation.
- Happy
- Satisfied
- Unhappy
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
An erratum to this article can be found at http://dx.doi.org/10.1007/s11999-009-0778-x
References
- 1.Beaule PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773–779. [DOI] [PubMed]
- 2.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clinical Orthop Relat Res. 2004;418:67–73. [DOI] [PubMed]
- 3.Brooker AF, Bowerman JW, Robinson RA, Riley LH Jr. Ectopic ossification following total hip replacement. Incidence and a method of classification. J Bone Joint Surg Am. 1973;55:1629–1632. [PubMed]
- 4.Eijer H, Myers SR, Ganz R. Anterior femoroacetabular impingement after femoral neck fractures. J Orthop Trauma. 2001;15:475–481. [DOI] [PubMed]
- 5.Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925–935. [DOI] [PubMed]
- 6.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. [DOI] [PubMed]
- 7.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. [DOI] [PMC free article] [PubMed]
- 8.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed]
- 9.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33. [PubMed]
- 10.Ito K, Minka MA, 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. [DOI] [PubMed]
- 11.Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66. [DOI] [PubMed]
- 12.MacDonald SJ, Garbuz D, Ganz R. Clinical evaluation of the symptomatic young adult hip. Semin Arthroplasty. 1997;8:3–9.
- 13.Maquet GJ. Biomechanics of the Hip. New York, NY: Springer-Verlag; 1984.
- 14.Merle D’Aubigne R, Postel M. Functional results of hip arthroplasty with acrylic prosthesis. J Bone Joint Surg Am. 1954;36:451–475. [PubMed]
- 15.Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;429:178–181. [DOI] [PubMed]
- 16.Parvizi J, Leunig M, Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg. 2007;15:561–570. [DOI] [PubMed]
- 17.Pauwels F. Biomechanics of the Normal and Diseased Hip. Berlin, Germany: Springer-Verlag; 1976.
- 18.Philippon MJ, Stubbs AJ, Schenker ML, Maxwell RB, Ganz R, Leunig M. Arthroscopic management of femoroacetabular impingement: osteoplasty technique and literature review. Am J Sports Med. 2007;35:1571–1580. [DOI] [PubMed]
- 19.Pierannunzii L, d’Imporzano M. Treatment of femoroacetabular impingement: a modified resection osteoplasty technique through an anterior approach. Orthopedics. 2007;30:96–102. [DOI] [PubMed]
- 20.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. [DOI] [PubMed]
- 21.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003;407:241–248. [DOI] [PubMed]
- 22.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. [DOI] [PubMed]