Abstract
Femoroacetabular impingement (FAI) has been identified as a common cause of hip pain in young adults. However, treatment is not well standardized. We retrospectively reviewed 97 patients (100 hips) who underwent osteochondroplasty of the femoral head-neck for FAI using a mini-open anterior Hueter approach with arthroscopic assistance. The mean age of the patients was 33.4 years. The labrum was refixed in 40 hips, partially excised in 39 cases, completely excised in 14 cases, and left intact in seven. Six patients were lost to followup, leaving 91 (94 hips) with a minimum followup of 28.6 months (mean, 58.3 months; range, 28.6–104.4 months). We assessed patients clinically using the nonarthritic hip score (NAHS). One patient had a femoral neck fracture 3 weeks postoperatively. At the last followup, the mean NAHS score increased by 29.1 points (54.8 ± 12 preoperatively to 83.9 ± 16 points at last followup). Eleven hips developed osteoarthritis and subsequently had total hip arthroplasty. The best results were obtained in patients younger than 40 years old with a 0 Tönnis grade. Refixation of the labrum did not correlate with a higher NAHS score (87 ± 11 with refixation versus 82 ± 19 points without) at the last followup. The technique for FAI treatment allowed direct visualization of the anterior femoral head-neck junction while avoiding surgical dislocation, had a low complication rate, and improved functional scores.
Level of Evidence: Level II, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Femoroacetabular impingement (FAI) was defined in the late 1990s by Rheinhold Ganz and colleagues [2, 3, 13] as abnormal contact between the anterior acetabular rim and the femoral neck. It has been identified as a common cause of hip pain in young adults [7, 12, 20] and has been proposed as a cause of osteoarthritis [12]. In 2001, Ganz et al. described a safe technique [11] of dislocating the hip to modify the shape of the femoral head at the head-neck junction and correct the abnormalities on the acetabular side: lesions of the labrum, overcoverage of the anterior acetabular rim, and cartilage damage. This technique has received wide acceptance and many surgeons [1, 3, 10, 17–19, 24] have reported using it to treat FAI. Even if the preliminary results are encouraging, the surgical exposure carries some morbidity [1] in terms of pain and rehabilitation period. Furthermore, hardware removal is common: Beaulé et al. [1] removed the internal fixation in nine of 34 patients because of persistent bursitis.
Although the surgical dislocation technique as described by Ganz et al. [11] is reportedly safe and preserves femoral head vascularity, when Ganz and colleagues initially reported the surgical dislocation approach in the late 1990s, no followup data were available and the risk of femoral head necrosis was not assessed. Therefore in 1999 we developed a technique using the Hueter mini-invasive anterior approach with arthroscopic assistance to avoid hip dislocation and trochanteric osteotomy. Beaulé et al. [1] in reviewing their experience with the dislocation technique recently reported a 3% rate trochanteric nonunion, a 26% rate of bursitis leading to revision for screw removal from the greater trochanter, and an 18% rate of patients dissatisfied with the outcome. We presumed the minimally invasive technique we began using would be as effective as the surgical dislocation technique for FAI surgical treatment and avoid these complications.
We therefore asked whether (1) the lesions could be visualized and treated with this approach and ascertained the complications, (2) functional scores would improve and if so at what time after surgery, (3) the scores differed without and with fixation of a labral tear and with the arthrosis grade (Tönnis), and (4) the likelihood of THA related to age or arthrosis grade. Finally, we compared our outcomes to those in the literature.
Materials and Methods
We retrospectively reviewed 97 patients (100 hips) treated for persistent hip pain secondary to FAI using a new surgical technique from April 1999 to December 2004. The cohort was composed of 50 men and 47 women with an average age of 33.4 years (range, 16–56 years). All patients had a positive impingement test [13, 14] (pain reproduced in flexion, adduction, and internal rotation). Five patients had prior hip surgery: one had a previous femoral neck fracture; one had a posttraumatic femoral head deformity at age 14; one had a previous labral resection; one had already had surgery for FAI; and one had in situ pinning of a slipped capital femoral epiphysis. All patients had MRI arthrography or CT arthrography to analyze the labrum for tears. Thirty-two patients presented with osteoarthritis: Tönnis Grade 1 in 30 patients and Grade 2 in three patients. We lost six patients (six hips) to followup prior to the final review in late 2007; these patients had a minimum followup of 13 months (mean, 36 months; range, 13–70 months). This left 94 hips with a minimum followup of 28.6 months (mean, 58.3 months; range, 28.6–104.4 months).
All 100 hips underwent surgery with the same procedure by the senior author (FL). The patients were in supine position on a regular table with an extension to allow traction along the axis of the operated lower limb (Fig. 1). In order to minimize the risk of traction complication, the other leg was kept free so as to allow pelvic tilt if too much traction was applied. The size of the perineal post was 12 cm. We did not use fluoroscopy. The knee was slightly flexed to relax the anterior structure of the hip (capsule, rectus femoris, and psoas). The incision was anterolateral, about 2 to 4 cm in length. The skin incision was parallel to the classic incision described by Hueter in Sariali et al. [23] but located inferiorly by approximately 1.5 cm to minimize risk of injury to the lateral femoral cutaneous nerve. The incision was centered on the top of the great trochanter. The superficial fascia of the thigh was opened along the tensor fascia lata muscle which is partially detached from its aponeurosis and then retracted laterally. The proximate part of the innominate aponeurosis was cut and the rectus femoris muscle was retracted medially. We did not detach the gluteus minimus laterally or the iliopsoas medially from the capsule. The anterosuperior capsule was dissected free with a finger; this is an avascular space and usually does not bleed (Fig. 2). This approach also has the advantage of passing between two innervation territories: the muscles innervated by the femoral nerve (rectus femoris, iliopsoas), and the muscles innervated by the gluteal nerve (gluteus minimus, gluteus medius, and tensor fascia lata). The capsule was then incised along the acetabular rim from 10 to 2 o’clock then along the medial edge of the iliofemoral ligament (Fig. 3). This incision was stopped superior to the lateral femoral circumflex artery. We used small self-retaining retractors for soft tissue retraction. The arthroscope (30° scope) was then inserted inside the joint through another portal situated 2 cm laterally and distally relatively to the distal part of the approach.
Fig. 1.
The patient is positioned supine with the traction device. The traction is only applied on the operated lower limb during the acetabular time. The approach is made with slight flexion. No fluoroscopy is needed. The incision is anterolateral and approximately 2 to 4 cm. The skin incision is parallel to the classic incision described by Hueter but moved downward approximately 1.5 cm to prevent injury of the lateral nerve of the thigh. The incision is centered on the summit of the great trochanter. Another more lateral and lower portal is used for the scope.
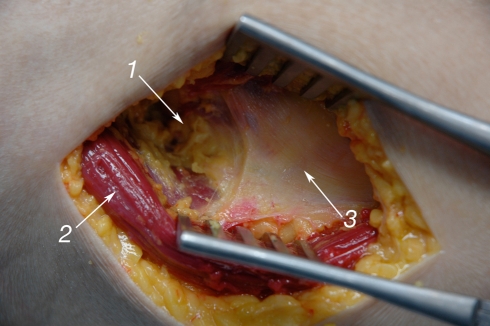
Fig. 2.
Large anatomic dissection view of the approach to show the “gap” (1) in the innominate aponeurosis (2) where the deep fibers of the rectus are running straight down. The approach passes between the rectus femoris and the tensor fascia lata muscles (3). The approach is usually 2 to 4 cm long and the section of the ascending branch of the lateral circumflex artery is not necessary.
Fig. 3.
T-shaped opening of the capsule. It may be sometimes necessary to cut the reflected head of the rectus femoris to improve access to the acetabulum.
Traction (approximately 15 kg) was applied to the lower limb to open and distract the joint. The joint distraction was usually less than 1 cm, allowing exploration of the acetabular cartilage and the examination of the deep part of the labrum with the arthroscope. The duration of traction ranged between 5 and 45 minutes and was used only during the acetabular surgical procedure. The mean traction duration was about 32 minutes if the labrum was refixed and about 11 minutes otherwise.
The surgeon described all the lesions for the operative notes, videos were obtained, and photos were taken for all patients. The operator (FL) measured the depth of the acetabular cartilage and classified the acetabular lesions according to Beck et al. [2] criteria. As the Beck classification was not published until 2005, the cases performed in the late 1990s and early 2000s were staged retrospectively using the videos and the photos made during the surgical procedure.
We found labral tears in 93 of the 100 hips. The labrum was refixed in 40 hips, partially excised in 39 cases, completely excised in 14 cases, and left intact in the remaining seven. Labrum débridement, consisting in a minimal excision of the damaged labrum, was performed in 39 patients. In 40 patients, a labral refixation to the acetabular rim was performed using two or three 2.9-mm suture anchors (Fig. 4A–D).
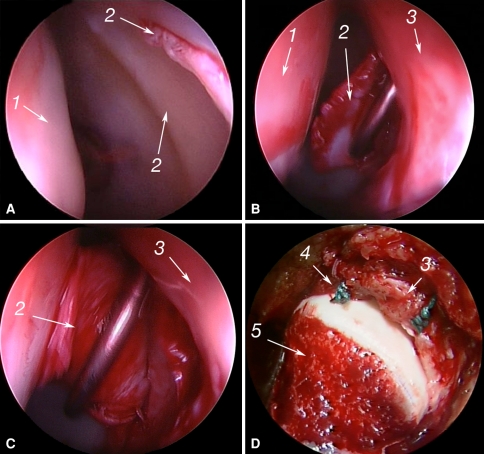
Fig. 4A–D.
Scope view inside the acetabulum of a 19-year-old man (martial arts performer) with a huge flap is shown: (A) View just after beginning of traction. (B) Huge mobile flap of cartilage. This large flap is not removed. (C) The labrum is first fixed with two suture anchors and the flap is fixed to the labrum with nonabsorbable monofilament (Prolene 5–0; Ethicon). The osteochondroplasty of the femoral head neck junction can then be performed with a chisel or burr. (D) This young patient had a very good result (NAHS improvement: 35 to > 95) at 55 months. 1 = femoral head, 2 = cartilage flap, 3 = labrum, 4 = anchor to refix he labrum, 5 = osteochondroplasty at the head neck junction.
The femoral side was probably the most critical part of the procedure. We found it easy to locate the bump on the femoral head. In fact, the impinged cartilage was more red and inflamed than the normal cartilage, so it was easy to know where to perform the osteochondroplasty of the femoral head-neck junction. We used a burr and a small chisel to perform the osteochondroplasty. A regular arthroscopic burr was used, however this instrument does not work efficiently when used in the air, therefore it was easier to complete trimming of the femoral head with the burr submerged in water. This was easily accomplished by removing the retractor, filling the joint with water and finishing the procedure under arthroscopic control. At the end of the procedure, the hip was flexed to ensure the impingement had been corrected (Fig. 5).
Fig. 5.
At the end of the procedure, the impingement is tested with flexion, internal rotation, and adduction.
Postoperatively, patients used crutches for approximately 5 days. Afterwards, we allowed full weight bearing without walking assists. We encouraged patients to start biking as soon as possible but recommended avoiding impact sports for 6 months.
All patients had clinical evaluations preoperatively, at 45 days, 3 and 12 months postoperatively, and at the last followup. The clinical functional outcomes were assessed with the Christensen nonarthritic hip score (NAHS) [6] using a self-administered questionnaire filled out by the patients. This score is designed for younger patients with higher demands and expectations than older patients with degenerative joint disease. It is divided into four domains: pain (five questions), mechanical symptoms (four questions), physical function (five questions), and level of activities (six questions). We arbitrarily divided patients into four groups according to the NAHS score: 91 and above (very good results), 81–90 (good results), 71–80 (fair), and under 70 (poor).
All patients had preoperative AP pelvic xrays, as well as lateral hip views. In case of poor clinical outcomes (NAHS score < 70) at the last followup, we obtained AP pelvic and lateral hip radiographs.
We compared age and acetabular cartilage lesions (depth and Beck grade) at the time of the initial procedure in the group of patients who had undergone THR at the last followup with those in patients who had not undergone THA. Distribution of all variables (NAHS score, age, lesion depth) was tested for normality using the Ryan-Joiner and Shapiro-Wilk tests. For normally distributed variables, when two groups (preoperative patients group and postoperative patients group) had the same variances, differences between them were analyzed using Student’s t-test. For abnormally distributed variables or normally distributed variables with different variances, we used the Mann-Whitney U test. For nominal variables (patients group), the chi square test was used.
Results
The surgical procedure was achievable in all the patients and allowed visualization and treatment of the lesions on both the acetabular and the femoral sides. However, 13 patients had a revision for persistent pain at a mean follow up of 30 ± 24 months and in all cases we performed arthroscopic débridement. In eight of the 13 cases, we observed a failure of the labrum refixation and the damaged part of the labrum was removed. In six cases, osteochondroplasty of the head was performed to improve the groove at the head-neck junction.
At 3 weeks postoperatively, one patient, aged 56 years, had a fracture of the femoral neck. Radiographs showed an undisplaced fracture of the femoral neck. We instituted nonoperative treatment and the patient healed after 3 months but with slight varus malunion. Two patients had a deep infection treated successfully with surgical débridement and organism-specific antibiotics for 3 months. One patient underwent revision at 33 months postoperatively for heterotopic ossification (Brooker Type 2). No patient developed avascular osteonecrosis of the femoral head.
At the last followup, the mean NAHS score increased (p < 0.000001) by 29.1 points (54.8 ± 12 versus 83.9 ± 16 points). The mean functional score observed at last followup was reached after a mean period of 6.2 ± 3 months with values ranging from 1 to 18 months. Sixty-seven percent of patients reached their final score before 6 months but 14% needed more than 1 year to do so. There was no difference (p < 0.13) in NAHS score at the last followup between patients with refixation (86 ± 11) and without refixation (82 ± 19) of the labrum. In the group of patients younger than 40 years old and with a Tönnis grade of 0 (43), 93% had a score above 80 at a mean followup of 57 months.
Eleven hips developed osteoarthritis and underwent THA at a mean followup of 40 ± 8.9 months (range, 5–75 months). Nine patients had THA and two had resurfacing hip arthroplasty. Patients who underwent THA were older (p = 0.04; 40.3 versus 32) than those who did not. In the replaced group, the acetabular lesions were deeper (p < 0.000001; 10.9 mm versus 6 mm) and a higher percentage of Beck Grade 5 (p < 0.000001; 54% versus 7%) was found.
Discussion
Although the dislocation hip technique that was developed by Ganz et al. [11] was reportedly effective and safe, it seemed risky to us at the beginning of our experience because no available data were reported in the literature at that time (1999). In addition, as a result of our considerable experience with the Hueter approach in performing THA [23], we believed the impingement lesion could be well-visualized and correctly treated with minimal soft tissue dissection. We presumed our minimally invasive approach would be as effective as the open surgical dislocation technique for treating FAI and might avoid complications related to trochanterotomy. We specifically asked whether (1) the lesions could be visualized and treated with this approach and ascertained the complications, (2) functional scores would improve and if so at what time after surgery, (3) the scores differed without and with fixation of a labral tear and with the arthrosis grade (Tönnis), and (4) the likelihood of THA related to age or arthrosis grade.
Our study has some limitations. We had some loss to followup, our patients were selected, and we did not study alternative approaches. The ideal study would be prospective and randomized, comparing the dislocation technique and the mini-invasive surgery on one hand, and labral fixation to labral removal on the other.
The lesions were correctly visualized in all the cases, which is similar to the reported studies using dislocation surgery [1, 3, 10, 18, 19]. The combination of several factors may explain this efficiency: the mainly anterior localization of the FAI lesions, the use of an orthopaedic traction table and also the 30° scope which allowed full visualization of the acetabular cavity without dislocation using minimal traction duration. The posterior femoral lesions may be more difficult to visualize and to treat entirely. However, this type of lesion is rare.
The FAI lesions substantially improved function in almost all the cases and therefore we presume properly treated the lesion. However, in six patients, osteochondroplasty was incomplete probably because of the learning curve. In fact, at the opposite of the dislocation technique, it may be difficult to check head sphericity after osteochondroplasty, because of the minimally invasive approach. As proposed by some authors [1, 15], a specially designed spherometer gauge can be of valuable help. Fluoroscopic control may also be used at the beginning of the experience in order to assess the femoral osteochondroplasty. This is why, in case of major deformity, we still use the surgical dislocation approach to perform an osteotomy of the femoral neck or the femoral metaphysis but the more we became confident in this technique, the less we performed trochanteric flip osteotomy.
Only one femoral neck fracture was observed. No others fractures have been reported in the literature when using the dislocation technique [1, 3, 10, 18–21, 25]. However, in contrast to these studies, our patients had immediate full weight bearing. In the technique described by Ganz et al. [11], the 6 to 8 weeks of discharge may prevent femoral neck fracture. In a recent study, Mardones [16] concluded a resection of less than 30% of the femoral neck was not related to an increased risk of fracture. However, application of that conclusion should be made cautiously. Therefore, we now recommend using crutches for a longer period of about 6 weeks for patients older than 40 years and in cases of poor bone mechanical quality.
There were no avascular necrosis nor trochanteric complications in this cohort. This seems an improvement because Beaule et al. [1] reported 3% of nonunion and 26% of bursitis with subsequent screw removal. Furthermore Peters and Erickson [19] observed 26% of incomplete union. We suspect we had no complications related to the orthopaedic table because traction was applied during a short duration and only after the capsule incision at the opposite to the classical hip arthroscopic surgery [5].
At the last follow up, functional scores improved in our cohort which is consistent with the literature [1, 3, 4, 8–10, 17, 18, 20]. However, it is difficult to compare our outcomes with those in the literature because we used the NAHS score which assessed the quality of life. Usually, the reported studies about FAI treatment [3, 18, 19] use the HHS or PMA score which are not particularly good outcome instruments for the young adult with hip pain [6, 22]. We are aware of only one study reported by Beaulé et al. [1] about the quality of life after FAI surgical treatment and they reported results similar to ours.
In contrast to the data reported by Espinosa et al. [9, 10], we observed no difference in clinical results between patients with labral refixation and those without, although we noted a tendency for a higher NAHS score with labral fixation. It is still unclear if labral refixation is necessary when the acetabular rim does not need trimming and further studies are required to investigate this point. We suspect refixation of a damaged labrum responsible for persistent pain resulting in revision with débridement for eight patients in our study. The failure of the labral fixation may be related to the fact that full immediate weight bearing was allowed postoperatively. This is why, as suggested by Philippon et al. [20], we now ask patients who had a labrum refixation to use crutches for 4 weeks with total discharge.
Only 11% of patients were converted to THA at a mean followup of 58 months, which is the lowest rate reported in the literature. In fact, Peters and Erickson [19] reported 22% at 32 months followup, Beck et al. [3] 26% at 56 months followup and Murphy et al. [18] 30% at 62.4 months.
Our data suggest high NAHS scores can be obtained in most patients with our technique, which is less invasive than the Bernese surgical approach. The mini-open approach allowed us to get used to the hip arthroscopy techniques, and so we have switched progressively to a full arthroscopic technique.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Beaule PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773–779. [DOI] [PubMed]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. [DOI] [PubMed]
- 3.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73. [DOI] [PubMed]
- 4.Bizzini M, Notzli HP, Maffiuletti NA. Femoroacetabular impingement in professional ice hockey players: a case series of 5 athletes after open surgical decompression of the hip. Am J Sports Med. 2007;35:1955–1959. [DOI] [PubMed]
- 5.Byrd JW, Pappas JN, Pedley MJ. Hip arthroscopy: an anatomic study of portal placement and relationship to the extra-articular structures. Arthroscopy. 1995;11:418–423. [DOI] [PubMed]
- 6.Christensen CP, Althausen PL, Mittleman MA, Lee JA, McCarthy JC. The nonarthritic hip score: reliable and validated. Clin Orthop Relat Res. 2003;406:75–83. [DOI] [PubMed]
- 7.Clohisy JC, Beaule PE, O’Malley A, Safran MR, Schoenecker P. AOA symposium. Hip disease in the young adult: current concepts of etiology and surgical treatment. J Bone Joint Surg Am. 2008;90:2267–2281. [DOI] [PubMed]
- 8.Clohisy JC, McClure JT. Treatment of anterior femoroacetabular impingement with combined hip arthroscopy and limited anterior decompression. Iowa Orthop J. 2005;25:164–171. [PMC free article] [PubMed]
- 9.Espinosa N, Beck M, Rothenfluh DA, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. Surgical technique. J Bone Joint Surg Am. 2007;89 Suppl 2 Pt.1:36–53. [DOI] [PubMed]
- 10.Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925–935. [DOI] [PubMed]
- 11.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip: a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. [DOI] [PubMed]
- 12.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. [DOI] [PMC free article] [PubMed]
- 13.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed]
- 14.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73:423–429. [DOI] [PubMed]
- 15.Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66. [DOI] [PubMed]
- 16.Mardones RM, Gonzalez C, Chen Q, Zobitz M, Kaufman KR, Trousdale RT. Surgical treatment of femoroacetabular impingement: evaluation of the effect of the size of the resection. Surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1 Pt 1):84–91. [DOI] [PubMed]
- 17.May O, Matar WY, Beaule PE. Treatment of failed arthroscopic acetabular labral debridement by femoral chondro-osteoplasty: a case series of five patients. J Bone Joint Surg Br. 2007;89:595–598. [DOI] [PubMed]
- 18.Murphy S, Tannast M, Kim YJ, Buly R, Millis MB. Débridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;429:178–181. [DOI] [PubMed]
- 19.Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and debridement in young adults. J Bone Joint Surg Am. 2006;88:1735–1741. [DOI] [PubMed]
- 20.Philippon M, Schenker M, Briggs K, Kuppersmith D. Femoroacetabular impingement in 45 professional athletes: associated pathologies and return to sport following arthroscopic decompression. Knee Surg Sports Traumatol Arthrosc. 2007;15:908–914. [DOI] [PMC free article] [PubMed]
- 21.Philippon MJ, Yen YM, Briggs KK, Kuppersmith DA, Maxwell RB. Early outcomes after hip arthroscopy for femoroacetabular impingement in the athletic adolescent patient: a preliminary report. J Pediatr Orthop. 2008;28:705–710. [DOI] [PubMed]
- 22.Rothenfluh DA, Reedwisch D, Muller U, Ganz R, Tennant A, Leunig M. Construct validity of a 12-item WOMAC for assessment of femoro-acetabular impingement and osteoarthritis of the hip. Osteoarthritis Cartilage. 2008;16:1032–1038. [DOI] [PubMed]
- 23.Sariali E, Leonard P, Mamoudy P. Dislocation after total hip arthroplasty using Hueter anterior approach. J Arthroplasty. 2008;23:266–272. [DOI] [PubMed]
- 24.Siebenrock KA, Gautier E, Woo AK, Ganz R. Surgical dislocation of the femoral head for joint debridement and accurate reduction of fractures of the acetabulum. J Orthop Trauma. 2002;16:543–552. [DOI] [PubMed]
- 25.Spencer S, Millis MB, Kim YJ. Early results of treatment of hip impingement syndrome in slipped capital femoral epiphysis and pistol grip deformity of the femoral head-neck junction using the surgical dislocation technique. J Pediatr Orthop. 2006;26:281–285. [DOI] [PubMed]