Abstract
This Classic Article is a reprint of the original work by M. N. Smith-Petersen, Treatment of Malum Coxae Senilis, Old Slipped Upper Femoral Epiphysis, Intrapelvic Protrusion of the Acetabulum, and Coxa Plana by Means of Acetabuloplasty. An accompanying biographical sketch of M. N. Smith-Petersen, MD, is available at DOI 10.1007/s11999-008-0671-z. This article is ©1936 by the Journal of Bone and Joint Surgery, Inc. and is reprinted with permission from Smith-Petersen MN. Treatment of Malum Coxae Senilis, Old Slipped Upper Capital Femoral Epiphysis, Intrapelvic Protrusion of the Acetabulum, and Coxae Plana by Means of Acetabuloplasty. J Bone Joint Surg Am. 1936;18:869–880.
In February 1935 a patient, aged fifty-five, was admitted to the Orthopaedic Ward of the Massachusetts General Hospital with the diagnosis of “bilateral intrapelvic protrusion of the acetabulum”. The case was discussed on ward rounds and the general opinion was that nothing could be done for this patient, and that she would have to adapt her life to the hip-joint condition. This did not seem a constructive attitude, and the patient was allowed to stay on the ward in the hope that some operative procedure might be developed which would give her relief from pain.
The question to be answered was this: “What is the source of this patient’s pain?” The answer was: “The impingement of the femoral neck on the anterior acetabular margin”. Such impingement would result in “traumatic arthritis” with characteristic changes of the joint surfaces as well as of the synovia. Since the joint surfaces have no nerve endings, their function in itself cannot be the source of the pain; as they slide over one another, even though the hyaline cartilage is markedly thinned, they will not give rise to symptoms. What does give rise to pain? The impingement of two surfaces—one covered by synovia, the other by cartilage—will give rise to congestion of the synovia, synovitis, and, because of periosteal irritation, hypertrophic changes.
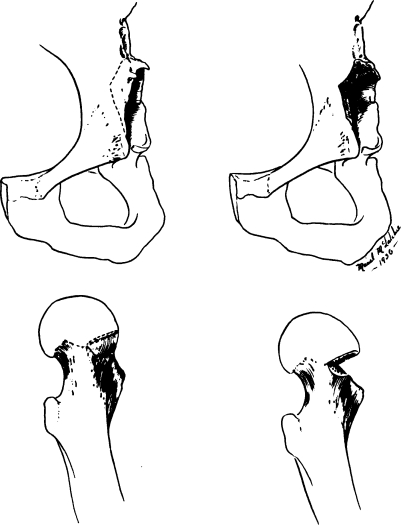
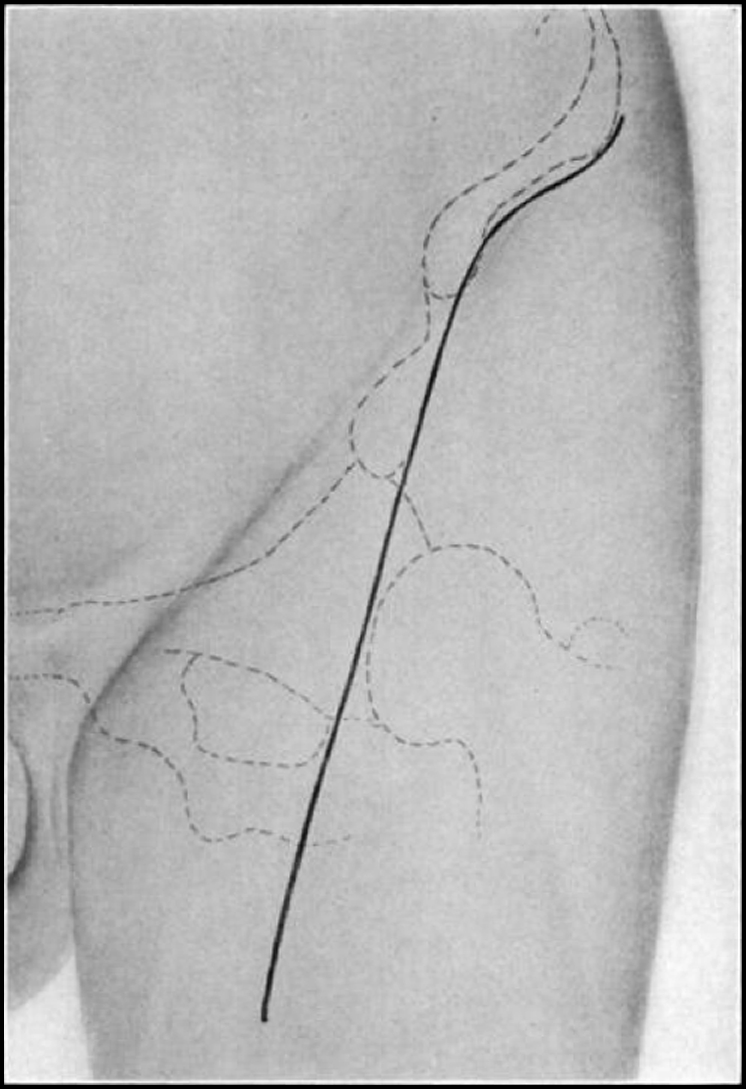
The following analysis gave us the answer to our problem: If we could eliminate this impingement, we should be able to eliminate the resultant reactions and, therefore, pain. To eliminate impingement two regions may be attacked,—the neck of the femur and the anterior margin of the acetabulum. To eliminate impingement by a plastic procedure on the neck of the femur would be impossible, since this would sacrifice too large a portion of the neck. (See Fig. 1.) What would be the effect of removing the anterior wall of the acetabulum? By sacrificing a small portion of this structure, a wide range of motion would be gained. This, then, seemed to be the answer to our problem. The patient was informed that the operation had never been performed before, but that it did offer a chance of success. She accepted the operation willingly. In four weeks she left the hospital walking, and in four months she returned to her work as a housekeeper, free from pain and without a limp.
Fig. 1.
Diagrams demonstrating the amount of bone which must be removed from the acetabulum or from the neck of the femur in order to produce the same improvement in the range of motion. This amount of bone may be easily spared from the acetabulum, but not from the neck of the femur.
The success in this case naturally suggested that the same procedure might be successful in other types of cases in which similar impingement was present. Malum coxae senilis came to our minds first. Since the operation was one that did no harm, we felt justified in applying it to a condition for which we had no adequate treatment. It has now been performed in eight such cases and the response has been so favorable that we feel free to publish a description of the procedure, in spite of the fact that it has been used for too short a time to enable us to give “end results”.
The procedure has also been applied to two cases of “old slipped upper femoral epiphysis” with impingement of the projecting anterior femoral neck on the anterior acetabular margin. In each case there has been improvement in function and relief from pain.
Fractures of the acetabulum with intrapelvic displacement of the head of the femur present the same mechanical problem as did the first case,—that of intrapelvic protrusion of the acetabulum. Consequently this operative procedure might be very effective in relieving pain and restoring function in this type of case.
Operative Technique
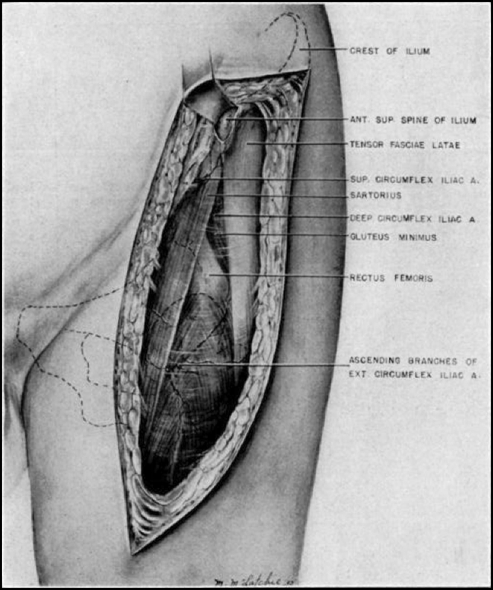
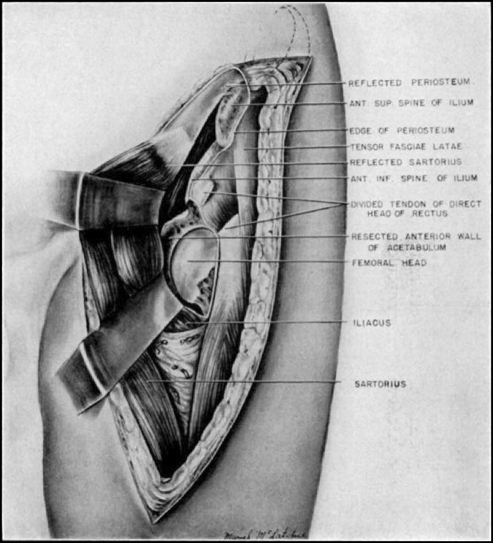
The incision extends along the anterior third of the iliac crest to the anterior superior spine, then curves slightly medially along the lateral border of the sartorius muscle. (See Fig. 2.) Immediately inferior to the anterior superior spine one finds the plane of division between the sartorius and the tensor fasciae femoris. The femoral fascia is incised along the lateral border of the sartorius, exposing the direct head of the rectus femoris. By sharp and blunt dissection the attachment of the direct head of the rectus femoris to the anterior inferior spine is defined.
Fig. 2.
The incision extends along the anterior third of the ilium and curves mesially along the lateral border of the sartorius.
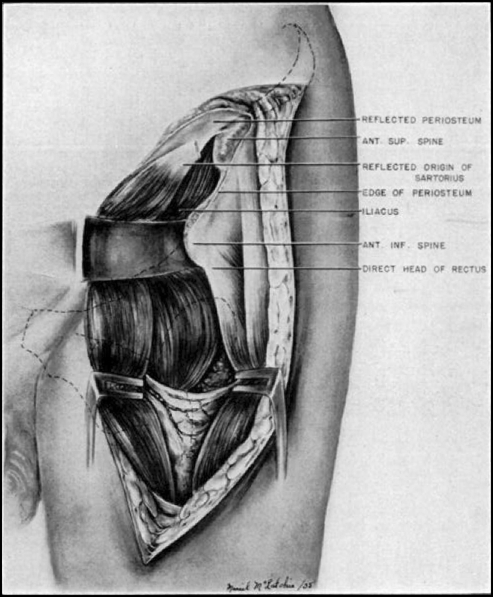
The next step (Fig. 3) is to identify the plane of division between the iliopsoas muscle and the proximal portion of the reflected head of the rectus femoris; the latter takes origin from the anterior acetabular wall as well as from the anterior capsule. The iliopsoas muscle is retracted mesially (Fig. 4), exposing the anterior intrapelvic wall of the acetabulum. In order to obtain a better exposure of the lateral portion of the acetabulum, the tendon of the direct head of the rectus femoris is divided, leaving sufficient tendon attached to the anterior inferior spine to allow for suture. When the distal portion of this muscle is retracted, the reflected head of the rectus comes into view, partly fused with the anterior capsule, partly attached to the anterior acetabular margin. This is dissected free and retracted laterally with the direct head of the rectus femoris.
Fig. 3.
Exposure of the anterior superior spine, of the lateral border of the sartorius, and of the mesial border of the tensor fasciae latae. Between these muscles is a compartment of fat with the rectus femoris as its floor.
Fig. 4.
Reflection of the abdominal oblique, sartorius, and iliopsoas muscles mesially, exposing the anterior aspect of the hip joint.
By the procedures described sufficient exposure of the anterior acetabular wall is usually obtained, but in some cases the iliopsoas muscle remains too taut to be retracted. In these cases it is advisable to reflect subperiosteally the origin of the sartorius and the abdominal oblique muscle from the anterior crest of the ilium, exposing the anterior portion of the iliac fossa. The iliacus may then be reflected subperiosteally down to the upper margin of the anterior acetabular wall, but at this point the periosteum is divided along the line of the intended osteotomy.
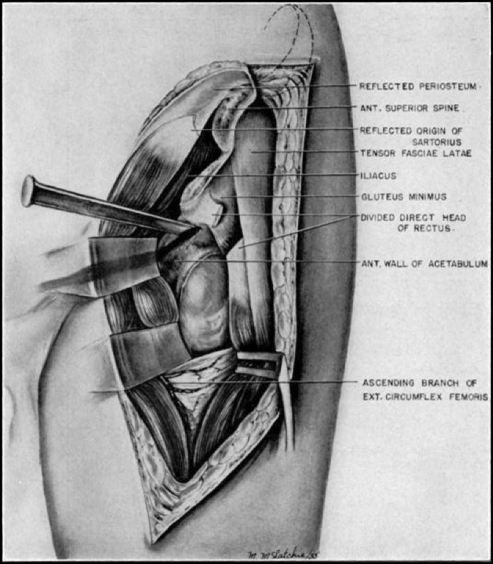
The above procedures allow for retraction of the iliopsoas muscle and of the sartorius mesially, and of both the direct and the reflected heads of the rectus femoris, and of the tensor fasciae femoris laterally. If the retraction mesially of the iliopsoas muscle is found difficult, the hip may be flexed, adducted, and externally rotated; by this procedure, the iliopsoas becomes relaxed and consequently may be retracted more easily. (See Fig. 5.)
Fig. 5.
Showing the line of osteotomy of the anterior acetabular wall immediately below the attachment of the direct head of the rectus femoris.
The next step is the osteotomy of the anterior acetabular wall; this may be done with a thin osteotome or gouge. The osteotomy starts just below the attachment of the direct head of the rectus femoris and is carried mesially a distance of approximately an inch and a half and is then curved inferiorly clown to the cotyloid notch. As soon as the fragment thus outlined becomes mobile the anterior superior capsule is incised down to the region of the distal neck. It is also incised inferiorly from the cotyloid notch along a line just proximal to the capsular attachment to the neck of the femur. (See Fig. 6.) When the anterior acetabular wall with its attached capsule is lifted out, there is obtained a beautiful exposure of the articular surface of the head of the femur and of the anterior aspect of the neck.
Fig. 6.
Result of plastic procedure: exposure of the mesial portion of the femoral head and of the anterior femoral neck.
By moving the hip in flexion, extension, abduction, and internal rotation, the surgeon now determines if the plastic procedure has been sufficient. If not, further excision of the superior acetabular margin and of the superior anterior capsule is done. The surgeon must be radical in performing this plastic procedure, but he should not remove so much of the superior aspect of the acetabulum as to allow the head of the femur to become displaced anteriorly. Of this there is relatively little danger, since hyperextension is rarely obtained and this is the motion which would allow the femoral head to dislocate.
The procedure follows structural planes throughout and consequently there is little or no shock. The two blood vessels encountered are the deep iliac circumflex and the ascending branch of the internal femoral circumflex. The former is easily eliminated; the latter sometimes gives rise to a little difficulty because of its extensive ramifications in the fat anterior and inferior to the hip joint. Furthermore, it is accompanied by motor branches from the femoral nerve.
The closure of the wound is very simple indeed. When the retractors are removed the iliopsoas drops back into place over the anterior aspect of the head and neck of the femur. The direct apposition of the posterior surface of this muscle to the anterior aspect of the head and neck of the femur is of great advantage,—two moving surfaces are very much less liable to form adhesions to one another than are two surfaces in more or less constant apposition, such as would be true of the capsule and of the underlying joint surface. The direct head of the rectus is sutured to its origin, and the superficial portion of the wound is closed in layers.
Postoperative convalescence is remarkable because of the relative absence of pain. The patient complains of soreness, but rarely of acute pain. The extremity is suspended with five pounds of traction, simply to overcome muscle spasm and thereby to diminish pain. The position should be one of extension with maximum abduction and maximum internal rotation. At the end of two weeks the patient is allowed up on crutches and, as a rule, he leaves the hospital at the end of three weeks; the maximum period of hospitalization is four weeks. He is taught exercises which he thoroughly understands by the time he leaves the hospital and which he carries on at home.
As already stated the main effect of this procedure is relief from pain: however, there is also considerable improvement in function. The increased function is the direct result of the removal of the acetabular wall, thus preventing impingement. If the anterior femoral head and neck are very prominent, it may at times be advisable to do a plastic operation on these as well as on the acetabulum. There is no danger of new bone formation or exostoses as a result of this procedure, since mechanical interference has been eliminated and since medullary bone is in apposition to the moving posterior surface of the iliopsoas muscle. The removal of the anterior capsule is probably an important factor in eliminating pain, because of its sensory innervation. It is important to remove sufficient capsule, including the Y ligament of Bigelow, to diminish the chances of adhesions and of scar formation. Another point to be emphasized in the technique is this: The acetabular wall should not be exposed subperiosteally, but its periosteum should be removed with it. This will tend to prevent new bone formation.
In one case the iliopsoas bursa was encountered. It was distended and inflamed, and unquestionably had been a source of pain.
Case Reports
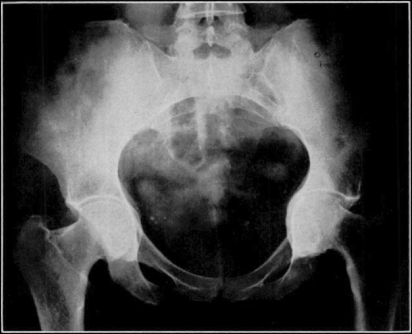
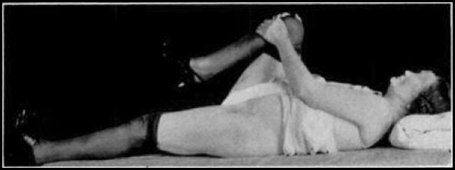
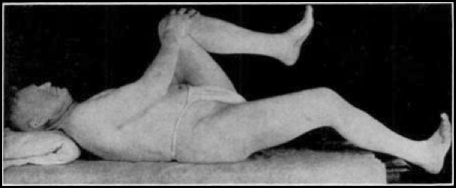
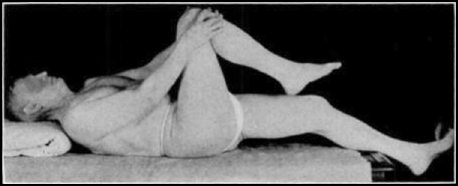
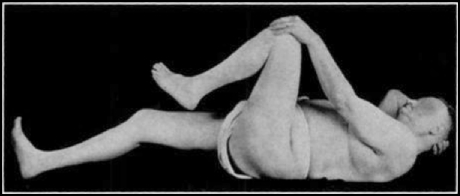
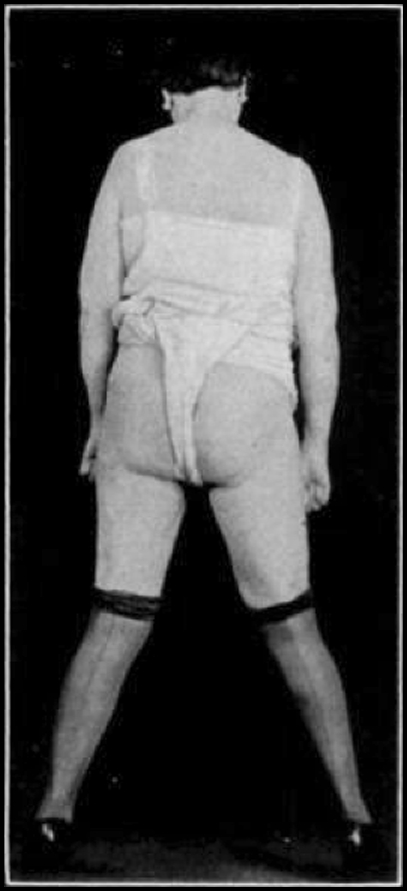
The first case treated by this operative method was a case of “bilateral intrapelvic protrusion of the acetabulum” (Fig. 7). The patient was a woman, fifty-five years of age, who for months had been disabled for her occupation as a housekeeper. She was in pain lying in bed, sitting, standing, and walking. As a result of the operation she was able to return to work, free from pain and without even a limp. The postoperative range of motion was definitely but not markedly increased. Figure 7 shows very definite protrusion of the acetabulum on the left and the same condition, but to a lesser extent, on the right. The postoperative roentgenogram shows no essential change. Ten months after the operation function was as follows: complete extension (Fig. 8), flexion to 90 degrees (Fig. 9), and a perfectly definite amount of abduction (Fig. 10).
Fig. 7.
Preoperative roentgenogram showing definite protrusion of the acetabula, more marked on the left than on the right.
Fig. 8.
Fig. 9.
Fig. 10.
As has been stated in the introduction, the success in the above case led us to apply it to cases of malum coxae senilis.
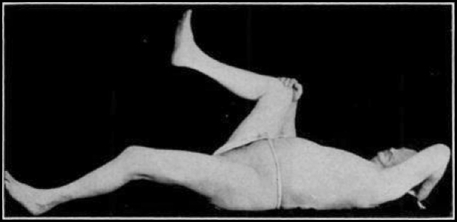
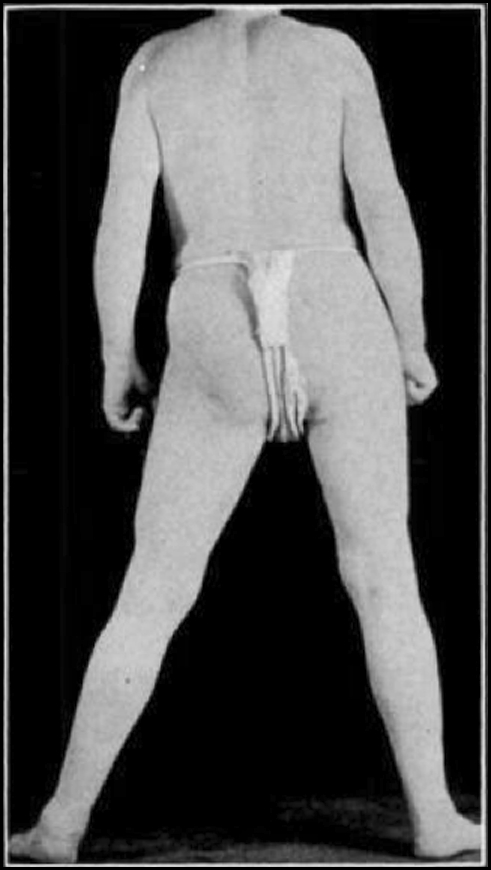
The first case was a man of fifty-eight, whose occupation was that of a brakeman. He had symptoms from the right hip for a period of years and had been disabled for several months. Roentgenographic examination (Figs. 11 and 12) showed changes in both hips,—hypertrophic changes and thinning of the joint cartilage, more marked on the right than on the left. Postoperatively the patient never at any time complained of pain. He was allowed up on crutches in seventeen days and was discharged on the twenty fifth day. At the time of discharge he got about very well indeed and was able to put on his right shoe for the first time in years. In five months he returned to his former occupation, which required jumping on and off trains. He was allowed to do this by promising that he would not jump on his right foot. When last seen, eight months after the operation, he had been back at work for three months; he complained of no pain and walked with a scarcely noticeable limp. Figures 13, 14, and 15 show this patient’s function at this time. There was permanent flexion of 20 degrees, motion in flexion to a good 90 degrees, and very little abduction (it was estimated as 10 to 15 degrees).
Fig. 11.
Preoperative roentgenogram showing proliferative changes with thinning of the joint cartilage.
Fig. 12.
Postoperative roentgenogram. The line of osteotomy of the acetabulum is indicated by arrows.
Fig. 13.
Fig. 14.
Fig. 15.
This case is important because the patient had two more years to go before he could obtain a pension. If it is proved that this procedure does not give permanent relief, it may at least be useful in producing temporary relief and improved function over an important period of time.
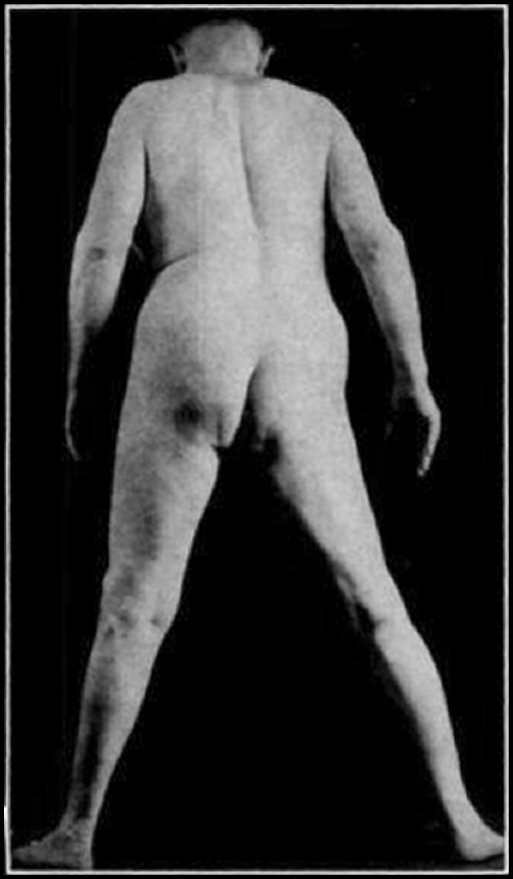
The second case was a blacksmith, fifty-eight years old. He had been in constant pain for several months before admission to the hospital. According to his story, he was unable to lie. sit, stand, or walk without pain. Figure 16 shows the condition before operation. The same procedure was performed. (See Fig. 17.) In the course of five months the patient returned to his blacksmith shop to do a couple of hours’ work a day. At the end of nine months he worked all day when he could find the work to do. Even at the time when this report was written, ten months after the operation, he walked with a very distinct limp, but this limp was unaccompanied by pain. He was comfortable lying, sitting, standing, and walking. Function at the end of nine months was as follows: 30 degrees of permanent flexion, motion in flexion to a good 90 degrees, abduction of approximately 10 degrees (Figs. 18, 19, and 20).
Fig. 16.
Preoperative roentgenogram showing hypertrophic changes with thinning of the joint cartilage.
Fig. 17.

Postoperative roentgenogram. Not much change is demonstrable.
Fig. 18.
Fig. 19.
Fig. 20.
Eleven cases have been treated by this method,—eight of “malum coxae senilis”, two of “old slipped femoral epiphysis”, and one of “intrapelvic protrusion of the acetabulum”. They have all done well; the relief from pain is the outstanding feature; gain in motion is definite but not marked. Most of the patients still have a perfectly definite, noticeable limp.
Postoperative Treatment
The outstanding feature of the postoperative period is the slight amount of pain complained of; some patients state that they have no “pain” at all, others say they have “soreness”, but none complain of acute pain.
The affected extremity is suspended with five pounds of traction in the optimum position,—maximum abduction and internal rotation, minimum flexion.
Following two weeks of recumbency the patient is gradually allowed to sit up and is trained to use crutches. The period of hospitalization should be a minimum of three weeks, a maximum of four. When the patient leaves the hospital he should be thoroughly trained in exercises to maintain the corrected position.
Comments
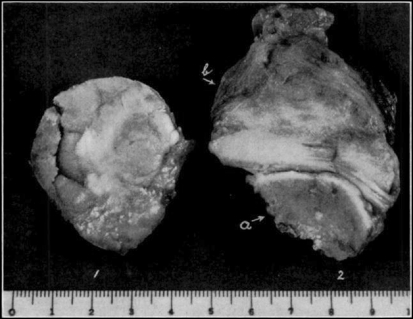
In the cases so far operated upon, the author’s attention has been directed chiefly to the anterior acetabular wall and to the anterior capsule of the hip joint. (See Fig. 21.) In some cases a plastic procedure has been performed on the anterior femoral head and neck, when they have been the seat of advanced proliferative changes. The inferior portion of the head and neck has likewise been removed for the same reason; this has been done in two cases only. The posterior aspect of the head and neck has been left untouched. This may be one reason why a greater improvement in range of motion has not been obtained. The writer considers it unwise to attack this region.
Fig. 21.
Characteristic appearance of specimen removed, consisting of: a, acetabular wall; b, attached capsule. 1 shows the specimen as viewed from the outside; 2 shows the intra-articular synovial surface.
Gentle manipulation for the sake of increasing the range of motion has been carried out in some of the cases at the end of the operative procedure. It is the author’s feeling that this is distinctly worth while and should be done routinely.
Summary
A plastic procedure has been proposed for the relief of hip-joint conditions resulting from interference with the normal mechanics of the hip joint. Such conditions are “malum coxae senilis”, “intrapelvic protrusion of the acetabulum”, “old slipped upper femoral epiphysis”, “fractures of the neck of the femur with malposition”, “Legg-Calvé-Perthes disease”, and “fractures of the acetabulum”.
Sufficient time has not elapsed to obtain true end results, but the author feels justified in rendering this preliminary report because the method is non-destructive and seems effective in relieving pain in conditions for which there is no other adequate treatment.
Footnotes
Richard A. Brand MD ✉ Clinical Orthopaedics and Related Research, 1600 Spruce Street, Philadelphia, PA 19103, USA e-mail: dick.brand@clinorthop.org
Read at the Annual Meeting of the American Academy of Orthopaedic Surgeons, St. Louis, Missouri, January 14, 1936.