Abstract
Femoroacetabular impingement (FAI) is considered a cause of labrochondral disease and secondary osteoarthritis. Nevertheless, the clinical syndrome associated with FAI is not fully characterized. We determined the clinical history, functional status, activity status, and physical examination findings that characterize FAI. We prospectively evaluated 51 patients (52 hips) with symptomatic FAI. Evaluation of the clinical history, physical exam, and previous treatments was performed. Patients completed demographic and validated hip questionnaires (Baecke et al., SF-12, Modified Harris hip, and UCLA activity score). The average patient age was 35 years and 57% were male. Symptom onset was commonly insidious (65%) and activity-related. Pain occurred predominantly in the groin (83%). The mean time from symptom onset to definitive diagnosis was 3.1 years. Patients were evaluated by an average 4.2 healthcare providers prior to diagnosis and inaccurate diagnoses were common. Thirteen percent had unsuccessful surgery at another anatomic site. On exam, 88% of the hips were painful with the anterior impingement test. Hip flexion and internal rotation in flexion were limited to an average 97° and 9°, respectively. The patients were relatively active, yet demonstrated restrictions of function and overall health. These data may facilitate diagnosis of this disorder.
Level of Evidence: Level II, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Femoroacetabular impingement (FAI) results from morphological abnormalities of the proximal femur and/or acetabulum which produce abnormal abutment of the acetabular rim and femoral head-neck junction [2, 3, 10, 15, 17, 24, 29]. This mechanical abutment is most pronounced with hip flexion and internal rotation, and can be associated with pain, articular cartilage disease, labral abnormalities, and progressive secondary osteoarthritis [10, 17, 24]. FAI can be classified into two broad categories, namely cam (femoral-based) and pincer (acetabular-based). These can occur alone or in combination [2]. Typically, FAI affects young, active patients and is now recognized as a common cause of hip dysfunction in this patient population. Surgical treatment techniques are evolving [8, 9, 11, 14, 16, 27, 28], and early reports suggest a favorable response to surgery is associated with early surgery prior to secondary osteoarthritic changes [3, 26]. These findings underscore the importance of early diagnosis and timely treatment for symptomatic hips.
Prompt diagnosis can be challenging since many of these patients have insidious onset of symptoms, mild structural abnormalities, and symptoms overlap with other musculoskeletal conditions of the hip, pelvis, and lumbar spine. It is our impression that many patients with symptomatic FAI experience delays in diagnosis, incorrect diagnoses, and ineffective treatment recommendations. We propose there is a major need to better define and characterize the clinical syndrome associated with this disease.
Therefore, the purpose of this study was to describe the clinical history, functional and activity status, and physical examination findings associated with symptomatic FAI. Additionally, we defined the timeliness of diagnosis and treatment characteristics prior to definitive diagnosis.
Materials and Methods
We prospectively collected descriptive data on a cohort of patients with symptomatic FAI between January 2007 and January 2008. All 51 patients (52 hips) consented to participate prior to data collection. The diagnosis of FAI was made on clinical and radiographic grounds by the senior authors (JCC, DH, HP). We required the following to make the diagnosis: “hip pain,” evidence of hip joint irritability (hip pain elicited with range of motion, anterior impingement test, logroll maneuver, or straight leg raise against resistance), restricted hip motion on physical exam, and radiographic evidence suggestive of impingement. The diagnosis was made 3 months to 15 years after symptom onset. All patients were eventually evaluated by one author (JCC) in an attempt to standardize the examination and data collection process. Radiographic evaluation consisted of an anteroposterior pelvis, frog-leg lateral, and cross-table lateral views for all patients. Radiographic structural abnormalities consistent with FAI were present in all patients. These abnormalities included one or more of the following: acetabular retroversion, coxa profunda, coxa protrusio, aspherical femoral head, or femoral head-neck offset less than 9 mm on the cross-table lateral or frog lateral view [6, 7, 25, 30]. We excluded all patients with any hip symptoms of unclear etiology or advanced secondary osteoarthritis. All patients were scheduled for surgery. The average age of the 51 patients was 35 years (range, 15–61 years). Twenty-nine patients were male and 22 female. The average height was 175.3 ± 10.7 cm (range, 152.4–201 cm) and the average weight 78.6 ± 17.4 kg (range, 53.6–120.5 kg). Thirty-five of the symptomatic hips were right and 17 left. One patient had bilateral hip symptoms. We had prior approval of our study protocol by our Institutional Review Board (IRB).
Detailed clinical history information was obtained by patient questionnaires that were completed after a definitive diagnosis was obtained. A comprehensive questionnaire [4] detailing the patient’s medical history and symptoms was utilized for hip symptoms. With this questionnaire, pain was characterized according to onset (acute/traumatic/insidious) [5], location, character, severity, duration, and aggravating and alleviating factors. Associated mechanical symptoms were also recorded. Patients also reported the time course and events leading up to their diagnosis of FAI including the age at symptom onset, previous diagnoses, the number and types of previous healthcare providers (physicians, physical therapist, chiropractor) seen for the problem, and the type of provider who made the final diagnosis. Additionally, standard measures of hip function (modified Harris hip score) [5, 12], overall health (SF-12) [31], and activity (Baecke et al. [1] and UCLA [32] scores) were obtained.
All patients underwent a standardized physical examination including bilateral hip range of motion and evaluation of pain with provocative hip maneuvers. Range-of-motion endpoints were determined by detecting motion through the pelvis rather than hip. A goniometer was used to determine the maximum motion achieved without initiating pelvic motion. Provocative tests included Patrick’s/FABERS (flexion abduction external rotation), hip log roll, resisted straight leg raise, anterior impingement [18], and posterior impingement signs. These maneuvers were considered positive when the test elicited groin pain. All patients received and failed nonoperative treatments that variably included nonsteroidal antiinflammatory medications, physical therapy, intraarticular steroid injections, and activity modifications.
We recommended surgery to all 51 patients. At the time of data analysis all patients had either had surgery (42 patients, 43 hips) or were scheduled (nine patients, nine hips) for surgery. For the 43 hips treated surgically, hip arthroscopy with acetabular and/or femoral osteochondroplasty was performed in 33 hips. The remaining 10 hips were treated with surgical dislocation. Intraoperative findings were documented and the presence of acetabular labral tears and articular cartilage disease was recorded by the surgeon (JCC). The degree of cartilage damage was graded according to the classification scheme described by Beck et al. [3], as Grade 0 (normal), Grade I (malacia), Grade II (pitting), Grade III (debonding), Grade IV (cleavage), or Grade V (full-thickness defect). Forty-two of the 43 hips (98%) treated surgically demonstrated articular cartilage and/or acetabular labral abnormalities. Thirty-six hips (84%) had an acetabular labral tear. Thirty-five hips (81%) had articular cartilage disease. Articular cartilage disease was Grade I in eight hips, Grade II in five hips, Grade III in five hips, and Grade IV in 17 hips.
Results
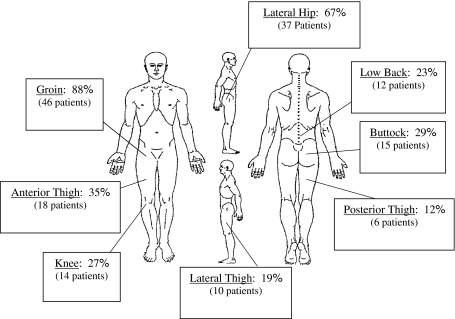
The majority of patients complained of an insidious onset of predominant groin pain that became moderate to severe by the time of presentation, and was worsened with activity (Table 1). The majority (65%) of patients had insidious onset of pain while 35% reported onset following a specific injury. The most common pain location was the groin region (83% of hips), yet many patients had associated discomfort in the lateral hip, thigh, buttock, and low back regions (Fig. 1). Eighty-seven percent of patients presenting with buttock pain had corresponding groin pain. No individual presented with isolated buttock pain. Pain severity was described as moderate, severe, or disabling in 81% of the hips. Aching pain and sharp pain were both present in 73% of the hips. A mechanical component to the pain (65%) and exacerbation with sitting (65%) were also common. Pain was activity-related in 71% of the hips with running (69%), pivoting (63%), and walking (58%) being most problematic. The most effective means of alleviating of pain was rest (67%) and frequent changing of position (52%).
Table 1.
Summary of hip symptoms associated with FAI (N = 52)
| Clinical parameters | Number of hips |
|---|---|
| Onset of symptoms | |
| Insidious | 34 (65%) |
| Trauma | 11 (21%) |
| Acute | 7 (14%) |
| Characteristics of pain | |
| Sharp | 38 (73%) |
| Ache | 38 (73%) |
| Burn | 13 (25%) |
| Numbness | 5 (10%) |
| Constant | 24 (46%) |
| Intermittent | 22 (42%) |
| Rest | 18 (35%) |
| Prevents sleep | 22 (42%) |
| Wakes from sleep | 19 (37%) |
| Moderate/severe/disabling symptoms | 42 (81%) |
| Mechanical features | |
| Any mechanical symptom | 33 (65%) |
| Pop | 24 (46%) |
| Snap | 23 (44%) |
| Catch | 17 (33%) |
| Lock | 15 (29%) |
| Subluxation/instability | 10 (19%) |
| Aggravating factors | |
| Activity related | 37 (71%) |
| Running | 36 (69%) |
| Sitting | 34 (65%) |
| Pivoting | 33 (63%) |
| Walking | 30 (58%) |
| Standing | 26 (44%) |
Fig. 1.
Pain location and frequency for patients with symptomatic FAI is shown.
This relatively young patient cohort had substantial limitations in function and activity levels (Tables 2, 3). Seventy-three percent of the patients limped, 42% were limited to sitting less than 30 minutes, 40% used a banister when climbing stairs, and 36% experienced limitations in walking distance. Baseline questionnaires, including the modified Harris hip, the Questionnaire of Habitual Physical Activity of Baecke et al. [1], the Short Form (SF)-12, and the UCLA activity score, were completed by all patients at the time of diagnosis (Table 3). The average modified Harris hip score was 63.9 (range, 39.6–92.4). The patients’ average work score of Baecke et al. [1] was 2.4 ± 0.9 (range, 0.75–5), total sport score was 2.7 ± 1.3 (range, 0.25–4.75), leisure index score was 2.6 ± 0.7 (range, 1.5–4), and a total score of Baecke et al. was 7.7 ± 2.3 (range, 2.5–12.25). Fifty-seven percent (29 patients) participated in regular sporting activities and 59% classified their sporting participation intensity as high while 28% reported it as moderate. The average UCLA activity score was 7.1 ± 2.8 (range, 2–10), consistent with patients participating in activities like fast walking, golfing, and bowling. Twenty-nine percent (15 patients) participated in impact activities like jogging, tennis, and ballet on a regular basis. The average baseline SF-12 physical functioning score was 43.5 ± 9.2 (range, 23.8–62.5) and 74% of patients reported a function score less than the average score of 50. Mental functioning score was 48.1 ± 11.6 (range, 17–66.9) with 43% of patients having a mental score less than the average score of 50.
Table 2.
Functional limitations associated with FAI (N = 51 patients)
| Limitation | Number of patients |
|---|---|
| Limp at any time during symptoms | 37 (73%) |
| Severity of limp | |
| Slight/Mild | 29 (57%) |
| Moderate | 7 (14%) |
| Severe | 0 (0%) |
| Use of cane, crutches, or assistive devices at any time during symptoms | 2 (4%) |
| Limitation in walking distance | 19 (37%) |
| Limited to 6 blocks | 11 (22%) |
| Limited to 2 blocks | 6 (12%) |
| Limited to indoors | 1 (2%) |
| Stairs | |
| Requires use of banister | 20 (39%) |
| Unable | 0 (0%) |
| Sitting tolerance | |
| 1 hour | 19 (37%) |
| > 30 Minutes | 10 (20%) |
| < 30 Minutes | 22 (43%) |
| Donning shoes and socks | |
| Difficult | 16 (31%) |
| Unable | 2 (4%) |
| Unable to use public transportation | 3 (6%) |
Table 3.
Patient function and activity data (51 patients, 52 hips)
| Questionnaire | Patient’s score | Minimum and maximum possible scoring |
|---|---|---|
| UCLA activity score | 7.1 (± 2.8) | 1 (low)–10 (high activity) |
| SF-12 | ||
| Physical component | 43.5 (± 9.2) | < 50 below average, > 50 above average health |
| Mental component | 48.1 (± 11.6) | < 50 below average, > 50 above average mental health |
| Modified Harris hip | 63.9 (± 12) | 0 (poor)–100 (excellent function) |
| Baecke | ||
| Work score | 2.4 (± 0.9) | 0 (none)–5 (high activity) |
| Total sport score | 2.7 (± 1.3) | 0 (none)–5.6 (high activity) |
| Leisure index score | 2.6 (± 0.7) | 0 (none)–5 (high activity) |
| Total score | 7.7 (± 2.3) | 0 (none)–15.6 (high activity) |
Physical examination demonstrated reduced hip flexion and a positive impingement test in the majority of patients. Hip range of motion was similar in both the symptomatic and asymptomatic hips (Table 4). In symptomatic hips, flexion was 97° (± 9°) and internal rotation in flexion was 9° (± 8°). Thirty-three percent (17 hips) demonstrated a Trendelenburg sign. Five different types of provocative tests were performed in a variable number of patients (Table 5). The anterior impingement test reproduced anterior groin pain in 46 of 52 (88%) tested. Thirty-six of the 52 hips (69%) demonstrated a positive FABER test, and 23 of 41 hips (56%) had a positive resisted straight leg raise. The log roll test and posterior impingement test reproduced hip pain in 30% and 22% of hips, respectively.
Table 4.
Hip range of motion
| Range of motion | Symptomatic hip | Asymptomatic hip | Average difference | ||
|---|---|---|---|---|---|
| Degrees | Standard deviation | Degrees | Standard deviation | ||
| Flexion | 97° | ±9° | 101° | ±11° | 3.7° |
| Extension | 4° | ±6° | 4° | ±6° | 0.1° |
| Abduction | 38° | ±11° | 41° | ±10° | 3.6° |
| Adduction | 17° | ±7° | 19° | ±8° | 1.6° |
| Internal rotation (neutral) | 15° | ±9° | 18° | ±11° | 2.9° |
| External rotation (neutral) | 26° | ±12° | 27° | ±12° | 1.2° |
| Internal rotation (90° flexion) | 9° | ±8° | 12° | ±8° | 2.7° |
| External rotation (90° flexion) | 28° | ±15° | 30° | ±16° | 3.3° |
Table 5.
Provocative test results (N = 53)
| Provocative test | Positive test/ number of hips tested | Percent positive |
|---|---|---|
| Anterior impingement test | 47/53 | 88.6% |
| FABER’s/Patrick’s | 52/53 | 98.7% |
| Resisted straight leg raise | 23/41 | 56.1% |
| Log roll | 12/40 | 30.0% |
| Posterior impingement test | 10/47 | 21.2% |
Many of the 51 patients experienced prolonged symptoms, delays in diagnosis, incorrect diagnoses, and unsuccessful treatments. The average duration of symptoms prior to obtaining a definitive diagnosis of FAI was 3.1 years (median, 2 years; range, 3 months to 15 years). Patients saw an average of 4.2 ± 2.9 healthcare providers (range, 1–16) before the diagnosis was made. A total of 220 healthcare providers were seen prior to a definitive diagnosis made by our group. Healthcare providers seen included 34 (16%) primary care physicians, four (2%) nurse practitioners, 15 (7%) physician assistants, 102 (46%) orthopaedic specialists, 33 (15%) physical therapists, 12 (5%) chiropractors, 20 (9%) physiatrists, pain management physicians, neurologists, neurosurgeons, and massage therapists. Nineteen different types of diagnoses were given to the patients prior to the diagnosis of FAI (Table 6). The most common diagnoses offered were “soft tissue injury” (10 patients/hips, 19%), hip osteoarthritis (five patients/hips, 10%), and hip dysplasia (four patients/hips, 8%). Additional non-hip-related diagnoses given included knee pain, low back pain, osteitis pubis, and fibromyalgia. The most frequent treatment prescribed during this time was nonsteroidal antiinflammatory medicines (34 hips, 65%). Physical therapy (30 hips, 58%) and chiropractic treatment (13 hips, 25%) were also common therapies. Injections were performed in 35% of the hips. Surgery (other than for FAI) was performed in 13% (seven hips) of these cases without resolution or improvement of symptoms.
Table 6.
Other diagnoses offered by healthcare providers as recalled by the patient
| Condition | Number of patients who received diagnosis* |
|---|---|
| Soft tissue | 10 |
| Hip osteoarthritis | 5 |
| Dysplasia | 4 |
| Labral tear | 4 |
| Bursitis | 3 |
| Back pain | 3 |
| Groin | 2 |
| Length discrepancy | 2 |
| Snapping psoas | 1 |
| Snapping hip | 1 |
| Psoas | 1 |
| Sacroiliac nerve | 1 |
| Hernia | 1 |
| Stress fracture | 1 |
| Hip shape | 1 |
| Knee pain | 1 |
| Iliac syndrome | 1 |
| Fibromyalgia | 1 |
| Osteitis pubis | 1 |
* Several patients received more than one diagnosis.
Discussion
Femoroacetabular impingement (FAI) is an under-recognized cause of hip pain and secondary osteoarthritis. There is an increasing body of literature [2–4, 6–8, 10, 11, 14–17, 24–29] regarding its structural characteristics, secondary articular disease, and surgical treatment options. Nevertheless, there is limited information regarding the clinical presentation of this disorder. The purpose of this study was to determine the clinical history, functional status, activity status, and physical examination findings associated with symptomatic FAI.
The limitations of our study include the characteristics of the patient cohort in that all patients were definitively diagnosed and treated by one group of physicians. It is possible these physicians have similar biases regarding the diagnostic characteristics of this disease and patients with atypical characteristics could have been misdiagnosed and excluded. If this did occur, we suspect that it was uncommon due to our high awareness of this diagnosis and our standard radiographic assessment for impingement abnormalities. Second, the physical exam findings are based upon the evaluation of a few physicians. These findings may be biased by the method of examination in our practice. Clearly, the clinical examination of hip range of motion and provocative tests has not been standardized for all physicians [20], and some may perform these tests with different techniques. Additionally, despite the prospective study design, the provocative tests were not recorded on all patients (Table 5). Finally, we have not confirmed the clinical resolution of impingement symptoms with surgical intervention. Despite the limitations, we did collect a unique dataset prospectively and present what we believe are comprehensive data regarding this patient population.
Our data demonstrate symptomatic FAI is commonly manifested as insidious onset of groin pain. As symptoms progress most patients experience moderate to marked pain and substantial limitations of activity (Tables 2, 3). These data are consistent with the previous work by Phillippon et al. [27, 28]. They reported on the clinical symptoms and exam findings in 301 patients treated for FAI. Eighty-five percent had moderate or marked pain, 81% had groin pain, and 99% a positive anterior impingement test. These data are consistent with our values of 81%, 83%, and 88%, respectively. Restricted hip flexion and internal rotation were also noted in our study. For example, ROM testing for our patients demonstrated deficits when compared with those for normal subjects described by Magee [19]. Specifically, our symptomatic hips had an average 97° of flexion and 9° of internal rotation in flexion. These values are lower than the 110° to 120° of flexion and 30° to 40° of internal rotation reported by Magee. Additional data from our study highlighted common delays in diagnosis and inaccurate diagnoses. Many patients are evaluated and treated by multiple healthcare providers before obtaining an accurate diagnosis.
Our patients were diagnosed at an average age of 35 years and they tended to be highly active, with over 50% participating in regular sporting activities such as soccer, softball, and golf. Twenty-nine percent of patients characterized their activity level as high as assessed by UCLA activity score. Sport activities requiring hyperflexion, hyperextension, and external rotation of the hip may place abnormal forces on the acetabular rim and therefore inflict microtrauma and injury to the labrochondral complex [13, 21–23]. These pathomechanics are accentuated in hips with structural impingement abnormalities. The relatively active patient population we have identified underscores the concept that high-demand activity may be a risk factor for development of symptomatic FAI (in the mechanically “jeopardized” hip). Importantly, activity limitations seem to have a substantial negative impact on these patients since 74% reported their physical activity level to be less than average.
The knowledge and awareness of FAI as a clinical entity is growing. The abnormal force patterns transmitted through the femoral head/neck junction and the acetabular rim predispose these individuals to functional limitations, articular cartilage damage, and subsequent secondary osteoarthritis. It is therefore paramount that the clinical presentation of FAI as outlined in this and other studies be recognized to establish a timely diagnosis. This will facilitate improved orthopaedic care of this disease, and will provide an opportunity for joint preservation surgical intervention when indicated.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article. Partial support was received from a Zimmer Clinical Research Grant (JCC). This work was supported in part by Award Number UL1RR024992 from the National Center for Research Resources (JCC). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health. This work was also supported in part by the Curing Hip Disease Fund (JCC).
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Baecke JA, Burema J, Frijters JE. A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr. 1982;36:936–942. [DOI] [PubMed]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. [DOI] [PubMed]
- 3.Beck M, Leunig M, Parvizi J, Boutier V, Wyss D, Ganz R. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;418:67–73. [DOI] [PubMed]
- 4.Burnett RS, Della Rocca GJ, Prather H, Curry M, Maloney WJ, Clohisy JC. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88:1448–1457. [DOI] [PubMed]
- 5.Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578–587. [DOI] [PubMed]
- 6.Clohisy JC, Nunley RM, Otto RJ, Schoenecker PL. The frog-leg lateral radiograph accurately visualized hip cam impingement abnormalities. Clin Orthop Relat Res. 2007;462:115–121. [DOI] [PubMed]
- 7.Eijer H, Myers SR, Ganz R. Anterior femoroacetabular impingement after femoral neck fractures. J Orthop Trauma. 2001;15:475–481. [DOI] [PubMed]
- 8.Espinosa N, Rothenfluh DA, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925–935. [DOI] [PubMed]
- 9.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. [DOI] [PubMed]
- 10.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed]
- 11.Guanche CA, Bare AA. Arthroscopic treatment of femoroacetabular impingement. Arthroscopy. 2006;22:95–106. [DOI] [PubMed]
- 12.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed]
- 13.Hunt D, Clohisy J, Prather H. Acetabular labral tears of the hip in women. Phys Med Rehabil Clin N Am. 2007;18:497–520, ix–x. [DOI] [PubMed]
- 14.Ilizaliturri VM, Jr., Nossa-Barrera JM, Acosta-Rodriguez E, Camacho-Galindo J. Arthroscopic treatment of femoroacetabular impingement secondary to paediatric hip disorders. J Bone Joint Surg Br. 2007;89:1025–1030. [DOI] [PubMed]
- 15.Ito K, Minka MA, 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. [DOI] [PubMed]
- 16.Larson CM, Giveans MR. Arthroscopic management of femoroacetabular impingement: early outcomes measures. Arthroscopy. 2008;24:540–546. [DOI] [PubMed]
- 17.Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66. [DOI] [PubMed]
- 18.MacDonald S, Garbuz D, Ganz R. Clinical evaluation of the symptomatic young adult hip. Semin Arthroplasty. 1997;8:3–9.
- 19.Magee D. Orthopedic Physical Assessment. Philadelphia, PA: Saunders; 1997:463.
- 20.Martin RL, Sekiya JK. The interrater reliability of 4 clinical tests used to assess individuals with musculoskeletal hip pain. J Orthop Sports Phys Ther. 2008;38:71–77. [DOI] [PubMed]
- 21.Mason JB. Acetabular labral tears in the athlete. Clin Sports Med. 2001;20:779–790. [DOI] [PubMed]
- 22.McCarthy J, Noble P, Aluisio FV, Schuck M, Wright J, Lee JA. Anatomy, pathologic features, and treatment of acetabular labral tears. Clin Orthop Relat Res. 2003;406:38–47. [DOI] [PubMed]
- 23.McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001;393:25–37. [DOI] [PubMed]
- 24.Parvizi J, Leunig M, Ganz R. Femoroacetabular impingement. J Am Acad Orthop Surg. 2007;15:561–570. [DOI] [PubMed]
- 25.Peelle MW, Della Rocca GJ, Maloney WJ, Curry MC, Clohisy JC. Acetabular and femoral radiographic abnormalities associated with labral tears. Clin Orthop Relat Res. 2005;441:327–333. [DOI] [PubMed]
- 26.Peters CL, Erickson JA. Treatment of femoro-acetabular impingement with surgical dislocation and debridement in young adults. J Bone Joint Surg Am. 2006;88:1735–1741. [DOI] [PubMed]
- 27.Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1041–1047. [DOI] [PubMed]
- 28.Philippon MJ, Stubbs AJ, Schenker ML, Maxwell RB, Ganz R, Leunig M. Arthroscopic management of femoroacetabular impingement: osteoplasty technique and literature review. Am J Sports Med. 2007;35:1571–1580. [DOI] [PubMed]
- 29.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286. [DOI] [PubMed]
- 30.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999;81:1747–1770. [DOI] [PubMed]
- 31.Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. [DOI] [PubMed]
- 32.Zahiri CA, Schmalzried TP, Szuszczewicz ES, Amstutz HC. Assessing activity in joint replacement patients. J Arthroplasty. 1998;13:890–895. [DOI] [PubMed]