Abstract
Inserting the femoral intramedullary alignment rod during total knee arthroplasty (TKA) can generate high intramedullary pressure, which increases the risk of intraoperative complications caused by fat embolism. Despite modifications to the surgical procedure, the best method to prevent this increase in pressure remains unknown. The reamer/irrigator/aspirator is a surgical instrument designed for use during femoral canal entry to increase the canal size and remove intramedullary fat and may prevent this pressure increase. We posed two hypotheses: (1) using the reamer/irrigator/aspirator system will result in lower maximum femoral intramedullary pressure than using only conventional instrumentation during the initial steps of a TKA; and (2) using the reamer/irrigator/aspirator system in the initial steps of TKA will result in a mean maximum intramedullary pressure less than 200 mm Hg. We simulated a TKA on 14 cadaveric femurs to compare the femoral intramedullary pressure using both methods. Considerable decreases in femoral intramedullary pressure of 86% proximally and 87% distally were obtained by using the reamer/irrigator/aspirator system. The mean maximum pressure using the reamer/irrigator/aspirator system was less than 200 mm Hg. Additional clinical studies are needed to confirm any reduction in complications using the reamer/irrigator/aspirator system.
Introduction
Fat embolism is a common intraoperative occurrence detected in 46% to 65% of patients during TKA [11]. When embolism reaches clinically relevant levels, the most commonly observed symptoms are hypoxemia, shortness of breath, petechial rash, or an altered mental status [1, 5, 20]. If fat embolism becomes life-threatening, it is classified as fat embolism syndrome (FES) [1, 4, 5, 11, 19, 20]. Although FES is rare and the true incidence and mortality rates are unclear [13, 20], reported incidences of FES range from 0.1% to 1% of all TKAs, and mortality rates vary from 5% to 20% of diagnosed cases despite supportive care with anticoagulation therapy and ventilatory support [1, 20].
The etiology of fat embolism and FES is not completely known. Two theories have been proposed to describe the mechanism of FES: (1) the biochemical theory and (2) the mechanical theory [3, 5, 20]. The biochemical theory states circulating fatty acids directly affect the pneumocytes and disrupt gas exchange [3, 20]. The mechanical theory assumes fat particles from the medullary canal of long bones, like the femur, enter the circulation and obstruct the capillaries [5, 20].
It is accepted that inserting instruments into the femoral canal during TKAs causes high intramedullary pressures, causing intramedullary contents to enter the systemic circulation [4, 8, 13, 20]. The number of fat particles observed in the lungs postoperatively correlates with increased femoral intramedullary pressure when a TKA is performed using conventional instrumentation (eg, drill, intramedullary alignment guide, and so on) [10, 16]. Although the exact femoral intramedullary pressure threshold that leads to fat embolism has not been studied in humans [13], a sheep model suggests emboli (bone marrow surrounded by a thrombotic aggregate) appear at intramedullary pressures greater than 200 mm Hg [21].
Some researchers have explored the use of different shapes and sizes of TKA intramedullary instrumentation and different surgical steps to prevent elevating the femoral intramedullary pressure during surgery [6, 14, 19]. Previous experiments show oversizing the entry hole and using a fluted alignment rod had less increase in femoral intramedullary pressure than not oversizing the entry hole and using a rounded alignment rod [6, 19]. Overdrilling, combined with changes in shape and size of the alignment rod, has not yielded consistent reduction in intramedullary pressure below a threshold that may induce embolic phenomena. Mueller and Rahn [15] reported pressure from reaming the intramedullary femoral canal is transmitted through the intramedullary fat and a considerable reduction in pressure can occur if the fat is removed before reaming or introducing an unreamed nail. However, because of the high viscosity of the medullary particles, the suction tube used in the experiment clogged frequently and actually elevated femoral intramedullary pressure in some cases when the fat was being removed. They concluded new instrumentation should be developed to facilitate removal of the femoral intramedullary fat contents before reaming the femoral canal for intramedullary nailing of a femoral fracture.
A new instrument, the reamer/irrigator/aspirator system, was designed to be used after femoral canal entry to increase canal size and aspirate intramedullary fat and bony chips generated while reaming. The design uses irrigation to decrease viscosity of the fat while simultaneously aspirating the slurry that is created.
Our aim was to determine the effectiveness of this device in a TKA by posing two hypotheses: (1) using the reamer/irrigator/aspirator system will result in lower femoral intramedullary pressures than using only conventional instrumentation during the initial steps of a TKA; and (2) using the reamer/irrigator/aspirator system in the initial technique will result in a mean maximum intramedullary pressure less than 200 mm Hg.
Materials and Methods
We performed a simulated TKA on 14 femurs (seven pairs) from fresh-frozen cadavers. The specimens were from two female and five male donors between the ages of 45 and 91 years (Table 1). Using the results from Mueller and Rahn [15] as a guide, in which a 520 ± 279 mm Hg difference in femoral pressure was observed when fat was removed from the intramedullary canal, we conducted a power analysis and determined five cadaver specimens would be needed to ensure the experiment had a power of 0.86 to detect differences in pressure between the two techniques. We removed the soft tissues and the femurs were mounted diagonally in a bone clamp. Pressure ports, 7/16-inch diameter, were drilled into the specimens at 1/3 and 2/3 their lengths proximal and distal to the midshaft. We then connected the ports by tubing to pressure transducers (PX209-30V15G5V; Omega Engineering Inc, Stamford, CT). The tubing from the pressure transducers was thread-sealed to the femurs and back-filled with water to eliminate air bubbles in the line. The pressure transducers took readings that were recorded at a frequency of 100 Hz. The data were read into an IBM laptop (Armonk, NY) from the proximal and distal ports using data acquisition software (OMB-Tempbook-66; Omega Engineering Inc).
Table 1.
Peak femoral intramedullary pressure for initial steps of TKA with and without RIA
| Age (years) | Gender | Canal size (mm) | Cause of death | Left femur - without RIA | Right femur - with RIA | |||
|---|---|---|---|---|---|---|---|---|
| Left | Right | Peak proximal pressure (mm Hg) | Peak distal pressure (mm Hg) | Peak proximal pressure (mm Hg) | Peak distal pressure (mm Hg) | |||
| 86 | Male | 14 | 14 | Colorectal carcinoma | 277.51 | 230.43 | 8.41 | 44.26 |
| 74 | Male | 12 | 13 | Cardiorespiratory arrest | 359.82 | 272.75 | 25.83 | 37.91 |
| 91 | Male | 12 | 11 | Congestive heart failure | 815.71 | 687.40 | 98.64 | 56.95 |
| 45 | Female | 9 | 10 | Respiratory failure | 845.78 | 587.98 | 106.55 | 46.38 |
| 50 | Male | 12 | 11 | Ventricular tachycardia | 677.99 | 731.83 | 87.56 | 71.76 |
| 71 | Female | 12 | 11 | Acute myocardial infarction | 315.50 | 327.75 | 212.61 | 118.31 |
| 72 | Male | 13 | 15 | Hypertensive hemorrhagic stroke | 1118.00 | 911.66 | 87.56 | 95.04 |
| Mean | 630.04 | 535.69 | 89.59 | 67.23 | ||||
An experienced orthopaedic surgeon (CVG) performed the simulated TKA on all specimens. The specimens were divided so the initial steps of a TKA using conventional methods were performed on the left femurs and the initial steps of a TKA, including the reamer/irrigator/aspirator system (RIA; Synthes, West Chester, PA), were performed on the right femurs. On the left femurs, the surgeon opened the canal with an 8/12.7-mm step drill (Zimmer, Warsaw, IN) and inserted an 8-mm fluted alignment rod (Zimmer). Approximately 5 seconds after the rod was fully inserted, he slowly extracted the rod. He opened the canal on the seven right femurs with the same 8/12.7-mm step drill, but then inserted a 2.5-mm ball-tip reaming rod for the RIA, reamed the canal with a 12-mm RIA (Fig. 1), and then inserted an 8-mm fluted alignment rod. During all simulated TKAs, we continually recorded the intramedullary pressure from the proximal and distal pressure transducers.
Fig. 1.
The reamer/irrigator/aspirator system is shown with the reamer head attached.
The pressure data from the RIA system were analyzed at four steps: (1) opening the canal; (2) inserting the ball-tip reaming rod; (3) reaming with the RIA; and (4) inserting the alignment rod. Similarly, the pressure data from the conventional instrumentation were analyzed at two steps: (1) opening the canal and (2) inserting the alignment rod.
We chose to investigate pressure differences at only certain points of the procedure after performing a complete TKA on two specimens, one using conventional instrumentation and the other using the RIA system in conjunction with conventional instrumentation. We noted the only detectable pressure increase in the femoral intramedullary canal occurred while opening the canal and inserting the alignment rod while using the conventional instrumentation. Similarly, the only detectable pressure increase while using the RIA system occurred while opening the canal, inserting the ball-tip reaming rod, reaming with RIA, and inserting the alignment rod. Therefore, the other specimens only had those steps of a TKA performed and analyzed.
We used Student’s t-test to compare the maximum recorded pressure from performing the procedure with the conventional methods against the maximum recorded pressure from using the RIA system. We also used a one-sample t-test to determine whether the maximum intramedullary pressure associated with both methods was different from 200 mm Hg at the specified steps of the procedure. All tests were performed using SPSS V 14.0 (SPSS Inc, Chicago, IL).
Results
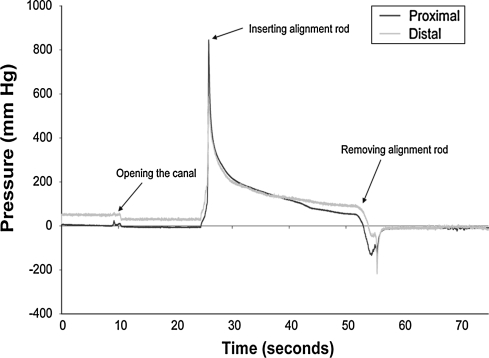
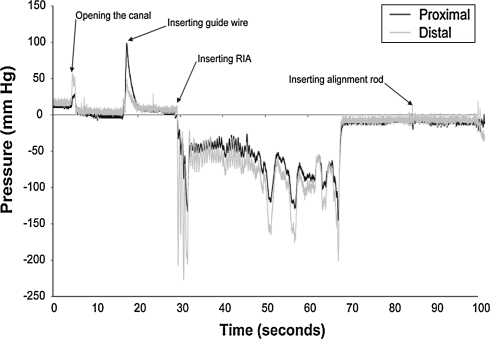
Using the RIA system resulted in lower (p = 0.0007) femoral intramedullary pressures compared with performing the steps of a TKA with conventional methods. Proximally, the average maximum pressure decreased from 630 mm Hg to approximately 90 mm Hg by integrating the RIA system into the initial steps (Table 1). Distally, the average maximum pressure decreased (p = 0.001) from 536 mm Hg to 67 mm Hg. Using the conventional methods, maximum intramedullary pressures occurred during insertion of the alignment rod (Fig. 2). While using the RIA system, the maximum intramedullary pressure occurred with the insertion of the ball-tip reaming rod in all of the specimens proximally and in four of the seven specimens distally (Fig. 3; Table 2). For conventional instrumentation and the technique using the RIA system, the average maximum pressure occurred at the proximal end of the femur; however, for some of the individual specimens, the maximum pressure was recorded at the distal end (three of seven on the right femurs and two of seven on the left femurs).
Fig. 2.
The largest femoral intramedullary pressure occurs while inserting the alignment rod when the initial steps of TKA are performed with conventional instrumentation.
Fig. 3.
The largest pressure occurs during insertion of the guide wire for the RIA when the initial steps of TKA are performed with conventional instrumentation and the reamer/irrigator/aspirator (RIA) system. Inserting the alignment rod causes a negligible pressure increase after evacuating the contents of the medullary canal.
Table 2.
Maximum pressure through initial steps of TKA
| Steps | Location | Maximum pressure in mm Hg (mean ± standard deviation) | |
|---|---|---|---|
| Conventional methods | Using RIA with conventional method | ||
| Opening the canal | Proximal | 4.34 ± 13.18 | 8.86 ± 33.95 |
| Distal | 41.54 ± 17.00 | 50.61 ± 34.18 | |
| Inserting ball tip reaming rod | Proximal | — | 89.59 ± 66.04 |
| Distal | — | 60.88 ± 22.83 | |
| Inserting RIA | Proximal | — | 12.93 ± 9.82 |
| Distal | — | 43.05 ± 24.58 | |
| Inserting alignment rod | Proximal | 630.04 ± 320.85 | 2.53 ± 10.08 |
| Distal | 535.68 ± 261.77 | 23.41 ± 11.87 | |
The mean maximum pressure of a simulated TKA using the RIA system was less than 200 mm Hg (p = 0.004 proximally and p < 0.001 distally). The mean maximum pressure during the initial steps of a simulated TKA using the RIA system was 89.6 mm Hg proximally and 67.2 mm Hg distally with a 95% confidence interval between 28.5 and 150.7 mm Hg proximally and 39.8 and 82.0 mm Hg distally. With the conventional methods, the intramedullary pressure was greater than 200 mm Hg when the alignment rod was inserted into the canal for all specimens (Table 1).
Discussion
Inserting the femoral intramedullary alignment rod during TKA generates high intramedullary pressure, which increases the risk of fat embolism. Despite modifications to the surgical procedure, the best method to prevent this increase in pressure remains unknown. We examined whether the reamer/irrigator/aspirator could effectively increase the canal size and remove intramedullary fat to prevent this pressure increase. We hypothesized using the RIA system in addition to traditional instrumentation during the initial steps of a simulated TKA would result in lower maximum intramedullary pressure compared with performing TKA with only traditional instrumentation. We also asked if using the RIA system with the initial steps of a TKA would prevent the maximum pressure from exceeding 200 mm Hg.
We note several limitations to this study. The use of cadaver bone cleaved of soft tissue may not perfectly model in vivo pressures. Soft tissues may increase the resistance to outflow of intramedullary contents, and stripping of these soft tissues may have falsely depressed the intramedullary pressures recorded while inserting instrumentation into the canal. Additionally, there was no recording of the insertion force or speed of the alignment rods; previous experiments have established these two parameters play a role in increasing femoral intramedullary pressure [14, 19]. Despite these potential limitations, the maximum intramedullary pressures recorded during insertion of the alignment rod using conventional techniques in our experiment (630.04 ± 320.85 mm Hg proximally and 535.69 ± 261.77 mm Hg distally) were comparable to the values recorded by Ries et al. [19] (649.3 ± 218.5 mm Hg) using a similar technique in vivo.
There might be some concern associated with removing the fat and bone marrow in the femoral intramedullary canal with the device. Previous in vivo studies suggest there are no negative effects of removing the fat and bone marrow in the femoral intramedullary canal [2, 12, 18]. Also, removal of healthy cortical bone through reaming into a narrow femoral intramedullary canal could have some consequences; these biomechanical effects of removing healthy cortical bone cannot be ignored. Harwin [7] reported thinning of anterior metaphyseal bone to a critical level increased the risk of fracture. Aware of this risk, future design modifications of the RIA should seek to minimize bone loss as it reams.
In addition to design modifications, procedural modifications could improve the modified technique in this experiment. In one of the seven cases of the modified technique (Table 1), the pressure was greater than 200 mm Hg (213 mm Hg) when the ball-tip reaming rod was inserted. Mousavi et al. [14] reported that as the speed of the reamer heads increases, the increase in femoral intramedullary pressure decreases. Because the peak intramedullary pressure occurred most often when leading with the ball-tip reaming rod for the modified technique, leading with the RIA could reduce that peak intramedullary pressure.
The main goal of the RIA design was to substantially reduce intramedullary pressure during canal preparation, thereby reducing risks associated with supraphysiologic values. Even though this is the first case, to our knowledge, using the RIA with a TKA, based on the results of similar studies, we anticipated there would be a substantial reduction in maximum femoral intramedullary pressure using the modified technique in comparison to the conventional technique. Experiments have been conducted on femoral intramedullary pressure during reaming and nail insertion in femoral fractures using the RIA or with a similar device on animal models that had similar results as our experiment. Husebye et al. [9] reported a lower maximum intramedullary pressure reaming with the RIA (33 ± 8 mm Hg) versus using a traditional reamer (188 ± 38 mm Hg) while reaming pig femurs. Joist et al. [10] used a rinsing-suction reamer for reamed intramedullary nailing in which physiologic pressure (40 mm Hg) was exceeded only during insertion of the guide wire. This rinsing-suction reamer achieved considerably lower levels of intravenous fat, as measured by Gurd criteria, compared with a standard AO reamer. Although they did not use a specialized device like the RIA, Amro et al. [2], using only a suction device, reported a decrease in intramedullary pressure of cadaver models and incidence of fat embolism in vivo from a TKA. Although the RIA was not specifically designed to be used before inserting an intramedullary alignment rod for TKA, our study yielded promising results.
The intramedullary pressure during canal entry using an 8/12.7-mm step drill was similar with the left and right femurs proximally and distally. This is noteworthy because even though measurements were not made to compare the force that the surgeon used in opening the canal, his approach was similar for both methods.
We chose to use 200 mm Hg as the threshold for fat embolism based on the work of Wenda et al. [21] in a sheep model. Pape et al. [17] attempted to validate the sheep model and concluded the effect of intramedullary instrumentation in sheep is less pronounced than in humans because the ratios of the femur and vertebral column differ. Although the exact threshold that leads to fat embolism in humans is unknown, it is reasonable to assume if a pressure increase is deleterious for a sheep, then it also would be so in humans. Additional work is needed to determine the pressure threshold that leads to fat embolism in humans.
Using the RIA reduced the femoral intramedullary pressure during the initial steps of a TKA and suggested a high probability the pressure would not exceed a critical threshold leading to FES. Although these results are promising, clinical studies are required to confirm the approach reduces the risk of emboli.
Acknowledgment
We thank Jim Green for assistance with preparation of the manuscript.
Footnotes
One or more of the authors (CVG, SJK) has received funding from Synthes, Inc.
References
- 1.Alfonso DT, Toussaint RJ, Alfonso BD, Strauss EJ, Steiger DT, Di Cesare PE. Nonsurgical complications after total hip and knee arthroplasty. Am J Orthop. 2006;35:503–510. [PubMed]
- 2.Amro RR, Nazarian DG, Norris RB, Kelly MP, Booth RE Jr. Suction instrumentation decreases intramedullary pressure, pulmonary embolism during total knee arthroplasty. Univ Penn Orthop J. 2001;14:55–59.
- 3.Baker PL, Pazell JA, Peltier LF. Free fatty acids, catecholamines, and arterial hypoxia in patients with fat embolism. J Trauma. 1971;11:1026–1030. [DOI] [PubMed]
- 4.Caillouette JT, Anzel SH. Fat embolism syndrome following the intramedullary alignment guide in total knee arthroplasty. Clin Orthop Relat Res. 1990;251:198–199. [PubMed]
- 5.Dobrjanski D, Saghir Z, Behdinan K, Zalzal P, de Beer J, Papini M. Intramedullary canal pressure distribution: an experimental parametric study. J Arthroplasty. 2007;22:417–427. [DOI] [PubMed]
- 6.Fahmy NR, Chandler HP, Danylchuk K, Matta EB, Sunder N, Siliski JM. Blood-gas and circulatory changes during total knee replacement: role of the intramedullary alignment rod. J Bone Joint Surg Am. 1990;72:19–26. [PubMed]
- 7.Harwin SF. Recognizing anterior metaphyseal femoral bone loss during uncemented total hip arthroplasty: the skylight sign. Orthopedics. 2007;30:218–221. [DOI] [PubMed]
- 8.Hofmann S, Huemer G, Salzer M. Pathophysiology and management of the fat embolism syndrome. Anaesthesia. 1998;53(suppl 2):35–37. [DOI] [PubMed]
- 9.Husebye EE, Lyberg T, Madsen JE, Eriksen M, Roise O. The influence of a one-step reamer-irrigator-aspirator technique on the intramedullary pressure in the pig femur. Injury. 2006;37:935–940. [DOI] [PubMed]
- 10.Joist A, Schult M, Ortmann C, Frerichmann U, Frebel T, Spiegel HU, Kropfl A, Redl H. Rinsing-suction reamer attenuates intramedullary pressure increase and fat intravasation in a sheep model. J Trauma. 2004;57:146–151. [DOI] [PubMed]
- 11.Kim YH. Incidence of fat embolism syndrome after cemented or cementless bilateral simultaneous and unilateral total knee arthroplasty. J Arthroplasty. 2001;16:730–739. [DOI] [PubMed]
- 12.Koessler MJ, Fabiani R, Hamer H, Pitto RP. The clinical relevance of embolic events detected by trasesophageal echocardiography during cemented total hip arthroplsaty: a randomized clinical trial. Anesth Analg. 2001;92:49–55. [DOI] [PubMed]
- 13.Martin R, Leighton RK, Petrie D, Ikejiani C, Smyth B. Effect of proximal and distal venting during intramedullary nailing. Clin Orthop Relat Res. 1996;332:80–89. [DOI] [PubMed]
- 14.Mousavi M, David R, Ehteshami J, Pajenda G, Vecsei V. Pressure changes during reaming with different parameters and reamer design. Clin Orthop Relat Res. 2000;373:295–303. [DOI] [PubMed]
- 15.Mueller CA, Rahn BA. Intramedullary pressure increase and increase in cortical temperature during reaming of the femoral medullary cavity: the effect of draining the medullary contents before reaming. J Trauma. 2003;55:495–503. [DOI] [PubMed]
- 16.Orsini EC, Byrick RJ, Mullen JB, Kay JC, Waddell JP. Cardiopulmonary function and pulmonary microemboli during arthroplasty using cemented or non-cemented components. J Bone Joint Surg Am. 1987;69:822–832. [PubMed]
- 17.Pape HC, Hildebrand F, Krettek C, Green J, Giannoudis PV. Experimental background: review of animal studies. Injury. 2006;37(suppl 4):S25–S38. [DOI] [PubMed]
- 18.Pitto RP, Hamer H, Fabiani R, Radespiel-Troeger M, Koessler M. Prophylaxis against fat and bone-marrow embolism during total hip arthroplasty reduces the incidence of postoperative deep-vein thrombosis: a controlled, randomized clinical trial. J Bone Joint Surg Am. 2002;84:39–48. [DOI] [PubMed]
- 19.Ries MD, Rauscher LA, Hoskins S, Lott D, Richman JA, Lynch F Jr. Intramedullary pressure and pulmonary function during total knee arthroplasty. Clin Orthop Relat Res. 1998;356:154–160. [DOI] [PubMed]
- 20.Taviloglu K, Yanar H. Fat embolism syndrome. Surg Today. 2007;37:5–8. [DOI] [PubMed]
- 21.Wenda K, Runkel M, Degreif J, Ritter G. Pathogenesis and clinical relevance of bone marrow embolism in medullary nailing: demonstrated by intraoperative echocardiography. Injury. 1993;24(suppl 3):S73–S81. [DOI] [PubMed]