Abstract
We evaluated the healing rate, complications, and functional outcomes in 32 adult patients with very short metaphyseal fragments in fractures of the distal tibia treated with a polyaxial locking system. The average distance from the distal extent of the fracture to the tibial plafond was 11 mm. All fractures healed and the average time to union was 14 weeks. Six patients (19%) reported occasional local disturbance over the medial malleolus. There were two cases of postoperative superficial infections and evidence of delayed wound healing. Using the American Orthopaedic Foot and Ankle Society ankle score, the average functional score was 87.3 points (of 100 total possible points). Our results show the polyaxial locking plates, which offer more fixation versatility, may be a reasonable treatment option for distal tibia fractures with very short metaphyseal segments.
Level of Evidence: Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
The treatment of fractures of the distal tibia with or without intraarticular involvement is associated with high complication rates and provides a management challenge to orthopaedists [5, 23, 25]. The fixation options for a distal tibial fracture include hybrid external fixation, limited internal fixation with external fixation, traditional open reduction internal fixation (ORIF), minimally invasive plate osteosynthesis (MIPO), fine-wire fixation, or possibly intramedullary nailing [2, 4, 11, 28, 33]. Although new changes in intramedullary nail design have extended distal metaphyseal fractures amenable to this type of fixation, difficulties with reduction, distal propagation of the fracture, inadequate distal fixation, and potentially complex articular involvement can limit its applicability in some distal metaphyseal fractures [28]. External fixation of such injuries may be associated with a high incidence of complications with pin infection and loosening in as much as 50% of cases and malunion rates as much as 45% [32]. Encouraging results for closed reduction and percutaneous plating of distal tibial fractures have been reported using contoured dynamic compression plates [6, 19, 31]. Recently, there has been an increasing trend toward use of a locking plate for treatment of complex fractures of the distal part of the tibia [10, 17, 18, 23, 27]. This device allows the screws to lock to the plate, thereby creating a stable, fixed-angle device.
Compared with a conventional plate, a locking plate imparts a higher degree of stability and provides better protection against primary and secondary losses of reduction and minimization of bone contact [12, 20]. Although a monoaxial locking plate with the screw locked into the threaded hole at a predetermined angle allows multiple points of fixed-angle support, the fixed-trajectory of the periarticular screws can make it difficult to ideally fix the infinite variety of fracture patterns seen in the distal tibia [13, 20]. The mechanical advantage of the polyaxial locking mechanism is the benefit of free choice of screw angle which allows screws to be placed in vital and strong bone in a wider variety of fracture patterns. However, to date, little has been published regarding treatment of fractures of the distal tibia with a polyaxial locking plate.
We reviewed a series of patients with very short metaphyseal segments in the distal tibia treated with polyaxial locking plates to document the bone union rate, complications, and functional outcomes using this technique. These results are compared with those achieved using a monoaxial locking plate to evaluate whether polyaxial locking plating can be recommended for treatment of fractures of the distal tibia.
Materials and Methods
From May 2006 to August 2007, 32 adult patients who sustained distal tibial fractures were treated with a polyaxial locking plate (Fig. 1). Indications for fixation with a polyaxial locking plate were skeletal maturity, a fracture involving the distal 4.2 cm of the tibia, and an intraarticular or extraarticular fracture requiring coronal or sagittal plane stability and/or support of articular fragments. Ethical approval was obtained from the Institutional Review Board. All patients were treated by two senior surgeons (GH, ZZB). There were 23 male and nine female patients with an average age of 44 years (range, 19–64 years). The minimum followup was 6 months with an average followup of 12.1 months (range, 6–22 months). The average distance from the distal extent of the fracture to the tibial plafond was 11 mm (range, 0–42 mm). The right tibia was involved in 13 patients and the left in 19 patients. The mechanism of injury included motor vehicle accident (n = 15), fall (n = 13), hit by heavy metal (n = 3), and industrial accident (n = 1). All fractures involved the metaphyseal part of the distal tibia, and in 14 cases, the fracture extended distally into the ankle. According to the American Orthopaedic and Orthopaedic Trauma Association (AO/OTA) Classification [30], there were seven 43A1, five 43A2, five 43A3, one 43B2, nine 43C1, three 43C2, and two 43C3 fractures. In the nine patients who had an open fracture, there were four Type I, four Type II, and one Type III according to the criteria of Gustilo and Anderson [15]. None required major soft tissue reconstruction or vascular repair. No bone grafting was used at the time of the initial procedure. Open fractures were treated with emergent débridement, irrigation, tetanus prophylaxis, and intravenous antibiotics.
Fig. 1A–G.
A 49-year-old man sustained a closed metaphyseal distal tibia fracture (Orthopaedic Trauma Association 43-A1) from a fall. Preoperative (A) anteroposterior and (B) lateral radiographs and (C) computed tomography scan show a relatively small fracture fragment of the distal tibia. (D) Anteroposterior and (E) lateral radiographs show the tibia after the fracture was reduced indirectly and fixed with a polyaxial locking plate using a minimally invasive plate osteosynthesis technique. (F) Anteroposterior and (G) lateral radiographs taken 4 months after surgery show satisfactory union and alignment.
Associated trauma occurred in nine patients. One patient with polytrauma presented with a closed head injury, thoracic contusion, closed ipsilateral acetabular and first and second metatarsal fractures, and traumatic ipsilateral sciatic nerve palsy. Four patients presented with contralateral tibia fractures. Three other patients presented with closed ipsilateral talar, calcaneal, and patellar and olecranon fractures, respectively, and one other patient had a closed head injury.
If primary osteosynthesis with a polyaxial locking plate was not suitable, the distal tibial fracture was managed with an external fixator, a temporary calcaneal traction with Braun’s frame, or a plaster splint with elevation. Once the soft tissues were quiescent, definitive internal fixation of distal tibial fractures was performed. The waiting time from the day of injury until definitive internal fixation varied from 0 to 11 days. The average was 6.2 days. Twenty-one distal tibial fractures were treated with a MIPO technique and 11 were treated with a traditional ORIF technique with the technique determined at the discretion of the treating surgeon.
The polyaxial locking plate used was the Numelock II® Polyaxial Locking System (Stryker, Selzach, Switzerland). The screw holes of the polyaxial distal tibial plate are composed of polyaxial locking holes in the epiphyseal/metaphyseal section and neutral holes in the diaphyseal portion. The anterior part of the distal plate consists of two polyaxial locking screw holes into which are inserted 4.5-mm polyaxial screws designed to control certain anterior or posterior bone fragments and provide subchondral support in comminuted articular fractures by virtue of their proximity to the articular surface (Fig. 2). These locking screws combined with other locking screws at the distal part of the plate can form multidirectional intersection fixation construction and provide very strong angular and axial stability for the distal tibia fracture, even for the very distal, comminuted fracture. Each polyaxial screw hole contains a threaded ring. As the conical threaded head of the screw engages with the corresponding threads in the ring, the ring in turn expands into the plate and creates the circumferential forces, securely locking the position of the screw at the chosen angle and direction. This polyaxial locking mechanism allows the surgeon to aim the screw at an optional trajectory within an approximately 30° cone of angulation.
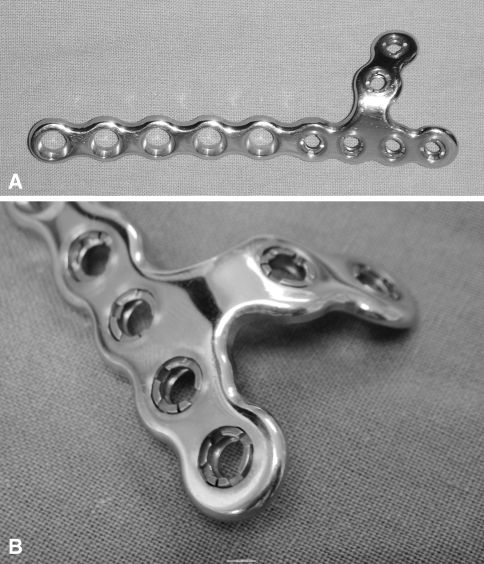
Fig. 2A–B.
Photographs show the Numelock II® polyaxial locking medial distal tibia plate. (A) The anterior and distal parts of the plate consist of two and four polyaxial locking screw holes, respectively, and allow a 30° cone of screw angulation before locking. (B) Each polyaxial screw hole contains a threaded ring.
A polyaxial locking plate osteosynthesis with the MIPO technique for the distal tibial fracture was performed with the patient placed in the supine position on a radiolucent operating table. Indirect and direct techniques of fracture reduction were used, depending on the nature and pattern of the fracture. Reduction techniques used included manual traction, an external fixator, and direct reduction with fracture reduction forceps inserted percutaneously. A gently, curving 3-cm incision was made over the medial malleolus, sparing the saphenous vein and nerve. Another 3-cm incision was made at the proximal end of the plate position. An extraperiosteal, subcutaneous tunnel then could be fashioned between the two incisions using blunt dissection. Care was taken to make this passage in one pass in the right orientation exactly, if necessary using C-arm control. A selected anatomic distal tibial polyaxial locking plate was inserted through the distal incision in a retrograde fashion and the end of the plate could be visualized adequately for insertion of the first three screws. Once the plate had been inserted into the passage, final adjustments to the plate could be made using C-arm control to ensure an exact meet to the bony contour, especially at the very distal tibia, with no tension in the overlying skin. Then assessment of the fracture reduction was performed again. This was achieved indirectly with the image intensifier to assess length and axial and rotational alignment. A locking screw or a conventional screw was used in the juxtaarticular segment, whereas a standard cortical screw closer to the fracture was used in the diaphyseal segment to pull the plate and bone together. At this stage, fracture alignment was reconfirmed before inserting any more screws. Subsequent screws were inserted close to either side of the fracture through stab incisions or the incisions already made for plate insertion. With fractures extending into the ankle, initial attention was paid to restoration of the articular surface continuity. These articular fragments were anatomically reduced either by percutaneous means, using fluoroscopy and pointed reduction forceps, or through a small anterior incision, arthrotomy, and direct reduction. Once articular reduction had been achieved, the articular fragments were stabilized with locking screws through screw holes at the anterior and distal parts of the plate, if necessary adding some cannulated screws. Additional screws might be used depending on the characteristics of the fracture. The associated fibular fracture was repaired to facilitate indirect reduction of the tibia fracture and provide additional stability unless it was believed fibular repair would place the soft tissue at an unacceptable risk. In 25 of 29 (86%) cases, the fibula was fixed and used to aid in indirect reduction of the tibia. For the patient treated with a traditional ORIF technique, an anteromedial approach was used for considerably displaced fractures after direct inspection and restoration of articular and metaphyseal segments. The polyaxial plate was placed at the medial point of the distal tibia. The directions of polyaxial locking screws were adjusted to obtain secure purchase in the short distal segments. The surgical incisions were irrigated and closed. Sterile dressings were applied and the limb was immobilized in a well-padded plaster splint with the ankle maintained in a neutral position. The drains were removed after 24 to 48 hours. A removable cast was exchanged and physiotherapy was started. Protected weightbearing was allowed only once signs of progress toward union were evident, usually at 6 weeks postoperatively. Full weightbearing was allowed after 10 to 12 weeks, depending on the radiographic signs of fracture healing.
Patients were followed postoperatively until fracture healing was achieved. One independent observer (LCF) who was not involved in the clinical care of the patients performed a complete followup assessment. Union was assessed clinically and radiographically. The fracture was defined as clinically united when it was no longer tender. Radiographic union was defined as bridging trabeculation across the fracture line(s) on three of four cortices seen on anteroposterior and lateral views.
Clinical outcome was assessed at final followup using validated limb-specific measures established by Kitaoka et al. [22]. The American Orthopaedic Foot and Ankle Society (AOFAS) ankle score is the contemporary standard score in foot and ankle regional outcome measurement [8]. This scoring system classified the evaluated items into three major categories: pain, function, and alignment. In this scale, 50 points have been assigned to function, 40 points to pain, and 10 points to alignment. Each category is scored independently and an overall score can be calculated with high scores indicating better function. These scores are obtained from direct questioning and examination.
Statistical analysis was performed with the SPSS software package (SPSS Inc, Chicago, IL). An independent sample t test was used to determine differences in union time between fracture with the MIPO technique and with the ORIF technique and between open and closed fractures. A p value of 0.05 or less was considered significant.
Results
All fractures healed without the need for a second operative procedure. The average time to union for all fractures was 14 weeks (range, 10–20 weeks). The average healing time was 13 weeks (range, 10–18 weeks) for fractures using the MIPO technique and 15.6 weeks (range, 10–20 weeks; p = 0.0045) for fractures using the ORIF technique. Closed fractures healed on average in 13 weeks (range, 10–20 weeks) and open fractures in 15.8 weeks (range, 14–20 weeks; p = 0.013).
The final ranges of motion averaged 17° (range, 0°−30°) ankle dorsiflexion and 34° (range, 20°−46°) ankle plantar flexion. No fractures were malaligned on the postoperative radiographs. All fractures healed within acceptable limits of alignment (less than 5° varus, less than 10° valgus, less than 10° procurvatum/recurvatum).
There were 10 postoperative complications. Six patients (19%) reported occasional local disturbance over the medial malleolus. Four patients (12.5%) had the implant removed partially or completely. At latest followup, no other patients desired implant removal. Two superficial infections occurred in the immediate postoperative period in fractures in which the ORIF technique was used, one in an open fracture and another in a closed fracture. All of the infections resolved with a course of antibiotics for 10 days. No deep infection was noted in any of the 32 patients. The overall rate of infection was 6.7% (two of 32). Two patients had evidence of delayed wound healing. One patient with an AO Type C closed fracture had delayed wound healing of the fibular incision, which resolved with local wound care. Another patient, whose distal tibia fracture was treated with the ORIF technique, had delayed wound healing of the anterior incision which needed wound débridement and a fasciocutaneous rotation flap to cover the wound. All other soft tissue wounds healed uneventfully. There were no plate fractures. There was also no evidence of loss of fixation of any polyaxial screw.
Using the AOFAS ankle-hindfoot scale, the average functional score was 87.3 points (range, 72–98 points). The patient with the lowest score was a patient with polytrauma with an ipsilateral limb fracture and nerve lesion.
Discussion
Currently, locking plate osteosynthesis has become widely accepted for treatment of periarticular fractures [1, 3, 9, 14, 16, 17, 24, 27]. For relatively smaller distal tibia fracture fragments, especially with an average distance of 11 mm from the distal extent of the fracture to the tibial plafond in the current series, a monoaxial locking plate with fixed-trajectory locking screws sometimes may not provide anticipated fixation for the distal fragment [13, 20]. However, a polyaxial locking plate system with the ability to adjust locking screw trajectories can disperse multidirectional locking screws in the end segment and provide a larger volume for fixation to maximize periarticular fragment fixation, thus providing better pullout strength and angular stability around the small distal fragment in comparison to a monoaxial locking plate system with inappropriate alignment [20]. Moreover, the anterior and distal parts of the Numelock II® polyaxial locking plate offer additional ability to control certain anterior or posterior bone fragments and some coronal plane fractures (Fig. 3). This may be particularly difficult in the fixation of some coronal plane fractures for a monoaxial locking system needing other adjunctive implants such as cannulated screws, which in turn may become obstacles to the insertion of screws at a predetermined angle. Thus, polyaxial locking plate osteosynthesis seems to be a logical option for these injuries.
Fig. 3A–G.
A 54-year-old man sustained an open displaced distal tibia fracture (Orthopaedic Trauma Association 43-C1) in a motor vehicle accident. Preoperative (A) anteroposterior and (B) lateral radiographs and (C) computed tomography scan show a relatively small fracture fragment of the distal tibia and a coronal plane fracture line in the metaphyseal part. (D) Anteroposterior and (E) lateral radiographs show the tibia after the fracture was reduced indirectly and fixed with a polyaxial locking plate using a minimally invasive plate osteosynthesis technique. (F) Anteroposterior and (G) lateral radiographs taken 8 months after surgery show a well-healed distal tibia and fibula. A conventional screw was removed for medial skin irritation.
Our study had several limitations such as the retrospective nature, small sample size, and lack of control group making it difficult to draw a definitive conclusion. More than half of the fractures in the current series were simple types; thus, more complications may have occurred if more complicated fractures had been included. In addition, one possible concern with a polyaxial locking plate is the implant cost. The high cost of the polyaxial locking system will hinder its widespread acceptance. However, in some selected patients with very short fracture segments, the new technology may offer substantial potential benefits, including increased stability of segment fixation, decreased need for adjunctive implants, and improved early functional recovery. Additionally, the followup was relatively short and 14 of the 32 patients had fractures with articular involvement. Therefore, although union could be documented in all patients, a longer followup period would help quantify to what extent, if any, posttraumatic arthritis develops. A strength of our study is the data analyzed pertain to a specific type of injury with relatively smaller distal tibia fracture fragments.
Because the distal tibia is covered only by a very thin layer of soft tissue, precise anatomic contouring of a locking plate and good match between the plate and the distal part of the tibia are important to reduce prominence and soft tissue trauma. Two major local problems have been observed in patients with monoaxial locking plates for distal tibial fractures: skin irritation from wearing tall boots and pain over the medial malleolus, both attributed to the monoaxial locking compression plate [10, 17, 18, 25]. For the polyaxial locking plate, it is not necessary to adjust the subcutaneous location of the plate to gain adequate fixation of very distal fractures or to avoid impingement between these locking screws and those inserted for articular reconstruction; therefore, a perfect match between the plate and the distal part of the tibia can be achieved, which in turn may further reduce tension in the soft tissue. With MIPO (nonlocking or monoaxial locking plate) of the distal fractures of the tibia, 8% to 100% of patients reported discomfort around the medial tibia shin region, whereas 8% to 66% of patients needed hardware removal [5, 10, 17, 25]. Although the Numelock II® polyaxial locking plate is a little thicker than the monoaxial locking compression plate, soft tissue irritation and the need for removal of hardware were less frequent in our series, which may be attributed to this good match between the plate and the distal part of the tibia.
Even if technically more demanding and requiring higher exposure to radiation because of closed indirect reduction, MIPO may have a biologic advantage over classic ORIF, especially when dealing with critical soft tissue conditions. With monoaxial locking plate osteosynthesis for metaphyseal fractures of the distal tibia using a long conventional incision, 23.5% of the patients had severe soft tissue damage with exposed plates and all needed flap coverage owing to the choice of an inappropriate surgical exposure technique rather than to the features of the locking compression plate system [27]. Using the MIPO technique for management of fractures of the distal tibia, some studies had infection rates of 5% to 18% and a rate of delayed wound healing of 10% [10, 18, 25]. Our study, using the same technique with polyaxial locking plating, showed similar or better results. The fracture healing time was shorter in the MIPO technique group than in the ORIF technique group, which might be related to minimizing soft tissue trauma to the injured zone and preserving better blood supply around the fracture area [7].
The functional results of the ankle seen in our study were mostly good according to a limb-specific assessment tool for the injured ankle [22]. Our results of a mean score of 87.3 points were comparable with the results of two recent series in which a nonlocking or monoaxial locking plate was used [10, 33]. Collinge et al. [10] showed patients with high-energy metaphyseal distal tibia fractures treated with MIPO had an average AOFAS foot and ankle score of 83 points. Sheerin et al. [33] performed staged treatment of high-energy distal tibia fractures with soft tissue injury and reported an average score of 81 points.
Caution should be taken to prevent or minimize complications. When using the Numelock II® polyaxial locking plate for treatment of fractures of the distal tibia, an image intensifier should be used intraoperatively to avoid prominence of the anterior part of the plate on the distal tibia at the anterior plane of the ankle to prevent ankle impingement. Malalignment has been recognized as a potential pitfall when using MIPO techniques because the bone is not directly visualized. With the MIPO technique and conventional or monoaxial locking plate osteosynthesis for fractures of the distal tibia, 7% to 35% of distal tibia fractures have been reported to have problems with malalignment [6, 19, 21, 23, 26, 29, 31]. In our series, no cases of postoperative malalignment were observed and no cases of postoperative stability failure were seen. We found careful intraoperative scrutiny of alignment was necessary to avoid malalignment during MIPO surgery. Furthermore, stabilization of the associated displaced fibula fractures facilitated not only indirect reduction of the distal tibia fracture, but also judgment of alignment [19].
Our results show the polyaxial locking plate offering more fixation versatility can provide a high degree of angular and axial stability to very short articular segments and metaphyseal comminution, achieves high rates of fracture union, and has complication rates similar to those of fixed-trajectory locking plates. Therefore, polyaxial locking plating may be a reasonable treatment option for distal tibia fractures with very short metaphyseal segments.
Acknowledgments
We thank Dr. Yao Chen and Chen Zheng for assistance in data collection and preparation of the manuscript.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Agudelo J, Schürmann M, Stahel P, Helwig P, Morgan SJ, Zechel W, Bahrs C, Parekh A, Ziran B, Williams A. Analysis of efficacy and failure in proximal humerus fractures treated with locking plates. J Orthop Trauma. 2007;21:676–681. [DOI] [PubMed]
- 2.Anglen JO. Early outcome of hybrid external fixation for fracture of the distal tibia. J Orthop Trauma. 1999;13:92–97. [DOI] [PubMed]
- 3.Arora R, Lutz M, Hennerbichler A, Krappinger D, Espen D, Gabl M. Complications following internal fixation of unstable distal radius fracture with a palmar locking-plate. J Orthop Trauma. 2007;21:316–322. [DOI] [PubMed]
- 4.Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibia pilon fractures: a study of three techniques. J Orthop Trauma. 2001;15:153–160. [DOI] [PubMed]
- 5.Borens O, Kloen P, Richmond J, Roederer G, Levine DS, Helfet D. Minimally invasive treatment of pilon fractures with a low profile plate: preliminary results in 17 cases. Arch Orthop Trauma Surg. 2006 Sep 2 [Epub ahead of print]. [DOI] [PubMed]
- 6.Borg T, Larsson S, Lindsjö U. Percutaneous plating of distal tibial fractures: preliminary results in 21 patients. Injury. 2004;35:608–614. [DOI] [PubMed]
- 7.Borrelli J Jr, Prickett W, Song E, Becker D, Ricci W. Extraosseous blood supply of the tibia and the effects of different plating techniques: a human cadaveric study. J Orthop Trauma. 2002;16:691–695. [DOI] [PubMed]
- 8.Button G, Pinney S. A meta-analysis of outcome rating scales in foot and ankle surgery: is there a valid, reliable, and responsive system? Foot Ankle Int. 2004;25:521–525. [DOI] [PubMed]
- 9.Cole PA, Zlowodzki M, Kregor PJ. Treatment of proximal tibia fractures using the less invasive stabilization system (LESS): surgical experience and early clinical results in 77 fractures. J Orthop Trauma. 2004;18:528–535. [DOI] [PubMed]
- 10.Collinge C, Kuper M, Larson K, Protzman R. Minimally invasive plating of high-energy metaphyseal distal tibia fractures. J Orthop Trauma. 2007;21:355–361. [DOI] [PubMed]
- 11.Collinge C, Sanders R, DiPasquale T. Treatment of complex tibial periarticular fractures using percutaneous techniques. Clin Orthop Relat Res. 2000;375:69–77. [DOI] [PubMed]
- 12.Egol KA, Kubiak EN, Fulkerson E, Kummer FJ, Koval KJ. Biomechanics of locked plates and screws. J Orthop Trauma. 2004;18:488–493. [DOI] [PubMed]
- 13.Frigg R, Appenzeller A, Christensen R, Frenk A, Gilbert S, Schavan R. The development of the distal femur less invasive stabilization system (LESS). Injury. 2001;32:SC24–SC31. [DOI] [PubMed]
- 14.Gosling T, Schandelmaier P, Muller M, Hankemeier S, Wagner M, Krettek C. Single lateral locked screw plating of bicondylar tibial plateau fractures. Clin Orthop Relat Res. 2005;439:207–214. [DOI] [PubMed]
- 15.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–458. [PubMed]
- 16.Haidukewych G, Sems SA, Huebner D, Horwitz D, Levy B. Results of polyaxial locked-plate fixation of periarticular fractures of the knee. J Bone Joint Surg Am. 2007;89:614–620. [DOI] [PubMed]
- 17.Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007;38:365–370. [DOI] [PubMed]
- 18.Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia: results in 20 patients. Injury. 2006;37:877–887. [DOI] [PubMed]
- 19.Helfet DL, Shonnard PY, Levine D, Borrelli J Jr. Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury. 1997;28(suppl 1):A42–A47; discussion A47–A48. [DOI] [PubMed]
- 20.Kaab MJ, Frenk A, Schmeling A, Schaser K, Schutz M, Haas NP. Locked internal fixator: sensitivity of screw/plate stability to the correct insertion angle of the screw. J Orthop Trauma. 2004;18:483–487. [DOI] [PubMed]
- 21.Khoury A, Liebergall M, London E, Mosheiff R. Percutaneous plating of distal tibial fractures. Foot Ankle Int. 2002;23:818–824. [DOI] [PubMed]
- 22.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 1994;15:349–353. [DOI] [PubMed]
- 23.Krackhardt T, Dilger J, Flesch I, Hontzsch D, Eingarter C, Weise K. Fractures of the distal tibia treated with closed reduction and minimally invasive plating. Arch Orthop Trauma Surg. 2005;125:87–94. [DOI] [PubMed]
- 24.Kregor PJ, Stannard JA, Zlowodzki M, Cole PA. Treatment of distal femur fractures using the less invasive stabilization system: surgical experience and early clinical results in 103 fractures. J Orthop Trauma. 2004;18:509–520. [DOI] [PubMed]
- 25.Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in the distal tibia fractures. Int Orthop. 2007 June 16 [Epub ahead of print]. [DOI] [PMC free article] [PubMed]
- 26.Maffulli N, Toms AD, McMurtie A, Oliva F. Percutaneous plating of distal tibial fractures. Int Orthop. 2004;28:159–162. [DOI] [PMC free article] [PubMed]
- 27.Namazi H, Mozaffarian K. Awful considerations with LCP instrumentation: a new pitfall. Arch Orthop Trauma Surg. 2007;127:573–575. [DOI] [PubMed]
- 28.Nork SE, Schwartz AK, Agel J, Holt SK, Schrick JL, Winquist RA. Intramedullary nailing of distal metaphyseal tibial fractures. J Bone Joint Surg Am. 2005;87:1213–1221. [DOI] [PubMed]
- 29.Oh CW, Kyung HS, Park IH, Kim PT, Ihn JC. Distal tibia metaphyseal fractures treated by percutaneous plate osteosynthesis. Clin Orthop Relat Res. 2003;408:286–291. [DOI] [PubMed]
- 30.Orthopaedic Trauma Association Committee for Coding and Classification. Fracture and dislocation compendium. J Orthop Trauma. 1996;10(suppl 1):v-ix, 1–154. [PubMed]
- 31.Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia. Injury. 2004;35:615–620. [DOI] [PubMed]
- 32.Russell TA. Fractures of the tibia and fibula. In: Rockwood CA, Green DP, Buckolz RW, Heckman JD, eds. Fractures in Adults. 4th ed. Philadelphia, PA: Lippincott; 1996:2139–2157.
- 33.Sheerin DV, Turen CH, Nascone JW. Reconstruction of distal tibia fractures using a posterolateral approach and a blade plate. J Orthop Trauma. 2006;20:247–252. [DOI] [PubMed]