Abstract
Femoroacetabular impingement (FAI) causes abnormal contact at the anterosuperior aspect of the acetabulum in activities requiring a large hip range of motion (ROM). We addressed the following questions in this study: (1) Does FAI affect the motions of the hip and pelvis during a maximal depth squat? (2) Does FAI decrease maximal normalized squat depth? We measured the effect of cam FAI on the 3-D motion of the hip and pelvis during a maximal depth squat as compared with a healthy control group. Fifteen participants diagnosed with cam FAI and 11 matched control participants performed unloaded squats while 3-D motion analysis was collected. Patients with FAI had no differences in hip motion during squatting but had decreased sagittal pelvic range of motion compared to the control group (14.7 ± 8.4° versus 24.2 ± 6.8°, respectively). The FAI group also could not squat as low as the control group (41.5 ± 12.5% versus 32.3 ± 6.8% of leg length, respectively), indicating the maximal depth squat may be useful as a diagnostic exercise. Limited sagittal pelvic ROM in FAI patients may contribute to their decreased squatting depth, and could represent a factor amongst others in the pathomechanics of FAI.
Level of Evidence: Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Femoroacetabular impingement (FAI) is an increasingly recognized cause of hip pain in young, active adults [1, 40] and is believed to be a cause of hip osteoarthritis (OA) [10, 12, 21, 25, 38, 39]. In fact, in a study by Tanzer and Noiseux [38], all 125 hips with idiopathic OA had a pistol-grip deformity, which is indicative of cam FAI. There are two types of FAI, both of which are defined by an anatomic abnormality of the acetabulum and/or the proximal femur that causes abnormal contact at the hip, primarily at the anterosuperior acetabular rim. Pincer impingement is related to overcoverage of the acetabulum, such as with acetabular retroversion and coxa profunda [18]. Cam impingement is caused by increased bone volume at the femoral head-neck junction, most commonly in the anterosuperior region [2, 14, 22, 26]. Increased bone volume at the femoral head-neck junction causes impingement between the acetabulum and the proximal femur. Activities requiring large hip flexion cause the anterosuperior femoral head to roll into the acetabulum, but in patients with cam FAI the bulge on the femoral head-neck junction is also forcefully rolled into the peripheral acetabulum [10]. This causes shear forces which can produce an “outside-in” abrasion of the acetabular cartilage combined with a potential tearing of the articular cartilage from the acetabular labrum in the anterosuperior rim of the acetabulum [10]. This damage occurs at the limits of hip range of motion (ROM) during assisted flexion, internal rotation, and adduction [15, 24]. Many common daily activities, such as prolonged sitting, squatting, stair climbing, and athletic activities requiring a large ROM, produce hip pain in people with FAI [4, 10, 21, 24, 40]. This pain is thought to occur after the onset of cartilage damage caused by “outside-in” damage of the acetabular labral-chondral junction [2].
Cam impingement is most common in relatively young athletes [10, 11, 14, 28] who perform activities requiring extreme ROM of the hip that exacerbate the condition. The maximal depth squat is a controlled movement requiring a large ROM of the hip and pelvis, approaching the maximal hip ROM in people with FAI [9, 13, 20, 32, 34, 37, 41, 42]. Furthermore, squatting closely reproduces the movements required for sitting in a low chair which has been reported to cause hip pain in patients with FAI [21]. This makes it likely that the FAI condition will affect maximal depth squats. Being a demanding movement, maximal depth squatting acts as an appropriate test for lower limb functionality, which could be useful for diagnosis [9, 13]. Finally, although deep squatting is not itself a common daily activity, it is a component of frequent activities, such as tying shoes, getting in and out of cars, and getting on and off toilet seats all of which are relevant for the affected population.
This study addressed the following questions: (1) Does FAI affect the 3-D motion of the hip and pelvis during a maximal depth squat? (2) Does FAI decrease maximal normalized squat depth?
Materials and Methods
We recruited 32 volunteers for this study: 16 diagnosed with cam FAI and 16 control participants matched by age, gender, and body mass index. We analyzed patients only with cam FAI to prevent there being multiple independent variables. The sample size was determined from a power analysis using pilot data from the first 10 volunteers (five FAI and five control participants) to determine the effect size and with squat depth as the key dependent variable. A total sample size of 22 was calculated using G*POWER 3 [8] with an alpha value set at 0.05 and minimal power set at 80%. The calculated sample size was the minimum required number of participants to achieve desired power based on our pilot data of squat depth, but since we were looking at other variables as well, a larger sample size was chosen to maximize the power of the study. The cam impingement participants were recruited after having a positive impingement test and visible cam morphology on anteroposterior and Dunn view radiographs [7, 21, 27, 35]. The alpha angle of Notzli et al. [30] was measured on each hip, with a value greater than 50.5° diagnostic of cam-type FAI. Matched control participants were recruited from the Ottawa region using online advertising and through interaction with various community groups. They had no history of serious lower limb injury or surgery and had spherical femoral heads, which were assessed by an AP radiograph [27]. Participants from both groups were excluded if hip osteoarthritis was visible on the radiographs or if they had substantial hip joint space narrowing. All FAI patients had only one symptomatic hip. We excluded five of the 16 recruited control participants: three had at least one aspherical femoral head based on an AP radiograph, and the other two could not have the required screening radiographs. One of the patients with FAI was excluded due to the presence of hip osteoarthritis. This left 11 control participants and 15 FAI participants (Table 1). All participants filled out a WOMAC [3] questionnaire. Before participating in the study, which was approved by the Ottawa Hospital Research Ethics Board and the University of Ottawa Health Sciences and Science Research Ethics Board, all participants signed an informed written consent.
Table 1.
Descriptive characteristics of femoroacetabular impingement and control participants
| Condition | Participants | Age (years) | Body mass index (kg/m2) | WOMAC (%) | Flexibility (cm) |
|---|---|---|---|---|---|
| Control | 11 (6 men) | 34.5 ± 10.1 | 23 ± 2.2 | 99.9 ± 0.3 | 29.8 ± 6.7 |
| Cam FAI | 15 (9 men) | 35.3 ± 9.1 | 23.4 ± 2.2 | 75.5 ± 15.7 | 21.9 ± 6.4 |
Values are expressed as mean ± standard deviation.
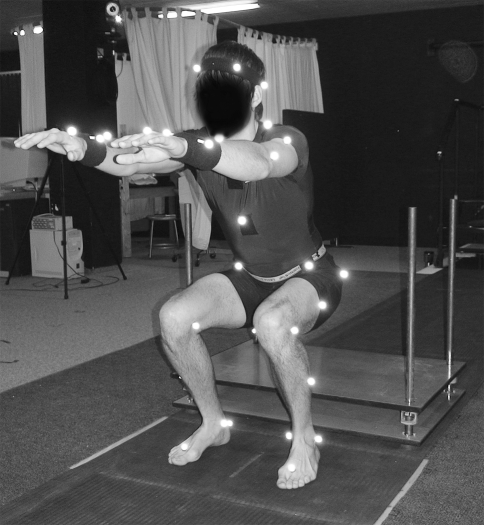
The 3-D motions involved with squatting were recorded with seven Vicon® MX-13 cameras (Vicon, Los Angeles, CA) at 200 Hz with retroreflective markers placed on anatomic landmarks according to a modified Helen-Hayes marker set [16] with additional greater trochanter, medial knee, and medial ankle markers to enhance joint center determination accuracy and upper body markers for display purposes only (Fig. 1). A height-adjustable bench was used to control squat depth acting as a maximal depth indicator.
Fig. 1.
An instrumented participant performs a maximal depth squat with feet positioned in front of the height-adjustable bench, which is lowered to 1/3 tibial height.
For the squat, the participants stood with their feet 10 cm directly in front of the height-adjustable bench. Bench height was lowered to 1/3 of the participant’s tibial height, acting as both a maximal depth indicator and a safety mechanism to prevent falling backwards (Fig. 1). Participants were asked to stand with feet shoulder width apart, parallel to each other, and facing anteriorly. Starting from standing, participants were asked to extend both arms anteriorly [13], squat down to a maximal depth, and return to a standing position at a self-selected and controlled pace [31], maintaining heel contact throughout the movement. Extending both arms anteriorly prevented the temptation to use them for support during the squat and helped with balance during the maneuver. If participants could squat down to the maximal depth, they were told to only touch their buttocks to the bench without transferring any weight and then to ascend back to a standing position. All participants performed five squat trials, and the hip and pelvic motions and peak squat depth were calculated for each (Fig. 2).
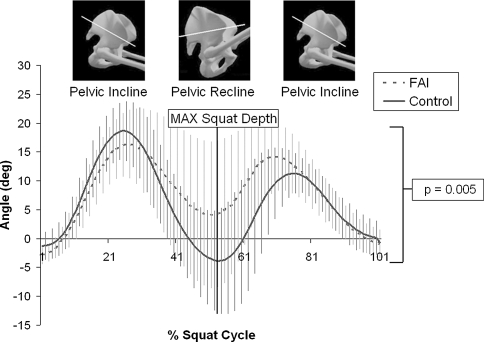
Fig. 2.
Mean pelvic pitch of the control group (solid line) and FAI group (dotted line) was plotted during maximal depth squat with vertical lines representing standard deviation. The control group had a higher range of pelvic pitch (p = 0.005) than the FAI group.
Lower limb 3-D motions were calculated according to the methods explained by Kadaba et al. [16, 17] and Davis et al. [5] using Vicon® Workstation processing software. Hip joint angles were based on local Euler coordinate systems as defined by the aforementioned studies, and pelvic angles were measured relative to a global coordinate system. Joint and segment angles were zeroed based on each participant’s neutral position as determined by a standing static trial where feet were parallel and facing anteriorly approximately shoulder width apart.
Squat motion variables consisted of the peak hip angle in each plane at maximal squat depth, the peak 3-D pelvic angles during descent, ascent, and at peak depth, the total pelvic ROM in each plane, and the maximal attained squat depth. The 3-D hip angles were only assessed at maximal squat depth because they tended to only have one peak, which occurred at peak squat depth. The 3-D pelvic angular displacements, however, tended to have a peak during descent, peak squat depth, and again during ascent. Peak squat depth was defined as the lowest point the hip joint centers reached during the squat divided by the participant’s total leg height, which was the averaged linear distance from the left and right medial malleoli to their respective anterior superior iliac spine. All five individual squat trials were averaged, and ensemble averaged for each group.
All dependent variables were tested for normality and had skewness and kurtosis values ranging between −1.5 and +1.5, indicating normally distributed data. Differences in maximal hip angular displacement in each plane at peak squat depth and in peak pelvic angles during descent, ascent, and peak squat depth, as well as at total pelvic ROM in each plane between the control and cam FAI groups, were determined using one-way between-subjects analysis of variances (α = 0.05). When we identified significant differences (p < 0.05) in the aforementioned dependent variables between the two groups we also performed an analysis of covariance run with squat depth included as a covariate. This was to ensure the differences in joint motions resulted from the presence or absence of cam FAI, rather than from discrepancies in squat depth. All calculations were processed using SPSS 15.0 software (SPSS Inc, Chicago, IL).
Results
The FAI group had a decreased (p = 0.005) sagittal pelvic ROM of 14.7 ± 8.4° (mean ± standard deviation) compared to 24.2 ± 6.8° in the control group (Fig. 2). When squat depth was included as a covariate, mean sagittal pelvic ROM remained reduced (p < 0.01) in the FAI group compared to the control group. However, there were no differences in any of the 3-D hip angles at maximal squat depth.
The control group also squatted to a lower (p = 0.037) mean maximal squat depth of 32.3 ± 6.8% of leg length, compared to the 41.5 ± 12.5% attained by the FAI group. Only five participants from the FAI group (33%) reached the lowest attainable squat depth compared to 10 controls (91%), as indicated by buttocks contact with the height-adjustable bench.
Discussion
This study evaluated squat motion since it is an important component of daily activities and a valuable indicator of lower limb mobility [9, 13]. As mentioned previously, the maximal depth squat is a relatively demanding activity that requires a high level of hip mobility [9, 13], and our results suggest it also requires a large sagittal ROM of the pelvis.
There are some limitations inherent to joint kinematic studies resulting from generic calculations, marker misplacements [6], joint center determination, and skin or clothing artefacts [23, 33]. However, precautions were used to minimize the potential errors caused by these limitations. All marker placements were performed by the same investigator (MK), which decreased interparticipant variability [6]. According to Della Croce et al. [6] the intra-observer 3-D variability in the placement of anterior superior iliac spine markers—which were the primary reference markers for hip joint center calculations—was up to two centimeters. This would inevitably affect the determination of hip joint center location and thus the calculated hip angles. Although, since the same variability of marker positions was common to both groups the systematic error was minimized. Furthermore, the primary effect of misplaced markers is an incorrect joint offset, which was corrected by zeroing all joint angles based on a neutral static trial. Finally, participants wore skin-tight clothing to minimize trunk and pelvic clothing artifacts, and the slow controlled nature of the squatting movement minimized skin artifacts [23]. A further limitation was posed by only analyzing the squat maneuver. This may reduce the extent to which our results may be generalized. However, this activity was chosen because we believe it is an important component of various common daily activities, and because of its potential in helping to diagnose FAI. Squatting requires a large sagittal hip and pelvic ROM that most control participants, but few FAI patients can fully achieve making it a useful diagnostic exercise. Finally, any limitations in hip or pelvic mobility that prevent the accomplishment of maximal squat depth could be indicative of a general restriction in joint mobility.
Surprisingly, we observed no differences in any of the hip motion variables between the impingement group and the control group. However, we observed more than one squat strategy in both groups. The majority of both groups used one modality, but five impingement participants and two control participants used different techniques. The main differences occurred in the frontal plane. The dominant strategy consisted of hip abduction throughout the squat maneuver, whereas the less dominant strategy consisted primarily of hip adduction throughout the maximal depth squat. Grouping these varying squat strategies increased variability and may explain the lack of differences between the two groups.
Perhaps the most important finding was the difference in the total sagittal pelvic ROM during the maximal depth squat between the control and FAI groups. Not only was the pelvic ROM lower in the FAI group, it was also independent of squat depth. As previously mentioned, all motion data were zeroed based on a standing trial, so the values are relative and give no insight on neutral pelvic orientation. The control group had much more sagittal pelvic ROM than the FAI group, with an increased incline during descent and ascent and increased recline at peak squat depth. The largest difference occurred in recline at peak depth (Fig. 2). The more the pelvis is reclined, the less acetabular retroversion occurs, which is associated with anterior FAI [29, 34–36]. In fact, it has been suggested pelvic retroversion may be caused by pelvic incline [34]. This indicates pelvic recline orients the acetabulum in such a way as to minimize contact between the acetabular rim and the anterosuperior femoral head-neck junction by decreasing anterior femoral head coverage [19]. Sagittal pelvic mobility is integral in flexing the torso to maintain balance and in allowing the large hip flexion angles essential for deep squats. Since the FAI group had decreased pelvic pitch in a maximal capacity maneuver requiring high levels of sagittal pelvic ROM, it is reasonable to assume cam FAI causes a general decrease in sagittal pelvic ROM. Reduced sagittal pitch may predispose the hip to premature contact between the proximal femur and the acetabular rim, especially in movements requiring high levels of hip flexion.
There was also a difference in maximal squat depth, with the control group squatting deeper than the FAI group. However, as mentioned previously, there were no differences in hip motion between the two groups. Since pelvic orientation does not directly contribute to squat depth, it was not responsible for the discrepancy in squat depth. The decreased squat depth in the impingement group was likely attained with a small combined contribution of the hip, knee, and ankle. Explaining the exact mechanism for the discrepancy in squat depth is outside the scope of this study, but decreased maximal squat depth in the cam FAI population could make maximal squat depth a useful exercise for diagnosing hip impingement.
The observation of reduced sagittal pelvic ROM in patients diagnosed with cam FAI provides new insight regarding the multifactorial nature of FAI. It is well-documented that cam FAI is a result of decreased concavity of the femoral head-neck junction [2, 14, 22, 26], which causes jamming of the proximal femur into the acetabulum [15, 24]. There is further evidence that cam impingement is caused by decreased femoral anteversion [15], which reduces femoral neck clearance from the acetabular rim during hip flexion and internal rotation [15, 24]. However, the idea that pelvic mobility may also be partially responsible for the abnormal contact between the anterosuperior acetabulum and the proximal femur is novel. Decreased sagittal pelvic mobility is an important manifestation of cam FAI, which highlights the multifactorial nature of this condition. Furthermore, it may represent a key feature in the pathomechanics of FAI and is an area of ongoing research.
One unresolved issue in FAI is the explanation of what causes the anatomic abnormality of cam FAI to be symptomatic in some but asymptomatic in others with the same hip morphology. Approximately 8% to 12% of hips with the anatomic variation indicative of cam FAI are asymptomatic [11, 28, 41]. The prevalence of asymptomatic FAI is further supported by the fact that three of our healthy controls were excluded due to the presence of aspherical femoral heads consistent with cam-type impingement but had no hip pain or physical limitations. Since decreased pelvic mobility may be a contributing factor of symptomatic cam FAI but is not assessed in current diagnosis, it could provide pathologic insight into the cause of symptomatic cam FAI. However, since this study provides no insight on the sagittal pelvic ROM of asymptomatic patients with decreased femoral head-neck concavity, no conclusions can be made. Future research should compare the pelvic mobility of symptomatic and asymptomatic patients with FAI anatomic variations.
Acknowledgment
We thank Anna Fazekas Conway, research assistant of the adult reconstruction division of the orthopedic surgery department at the Ottawa Hospital.
Footnotes
One or more of the authors (ML & PB) have received funding from the Canadian Institutes of Health Research.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Beaule PE, Le Duff MJ, Zaragoza E. Quality of life following femoral head-neck osteochondroplasty for femoroacetabular impingement. J Bone Joint Surg Am. 2007;89:773–779. [DOI] [PubMed]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. [DOI] [PubMed]
- 3.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed]
- 4.Crawford JR, Villar RN. Current concepts in the management of femoroacetabular impingement. J Bone Joint Surg Br. 2005;87:1459–1462. [DOI] [PubMed]
- 5.Davis RB, Ounpuu S, Tyburski D, Gage JR. A gait analysis data collection and reduction technique. Hum Mov Sci. 1991;10:575–587. [DOI]
- 6.Della Croce U, Leardini A, Chiari L, Cappozzo A. Human movement analysis using stereophotogrammetry. Part 4: assessment of anatomical landmark misplacement and its effects on joint kinematics. Gait Posture. 2005;21:226–237. [DOI] [PubMed]
- 7.Eijer H, Myers SR, Ganz R. Anterior femoroacetabular impingement after femoral neck fractures. J Orthop Trauma. 2001;15:475–481. [DOI] [PubMed]
- 8.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. [DOI] [PubMed]
- 9.Flanagan S, Salem GJ, Wang MY, Sanker SE, Greendale GA. Squatting exercises in older adults: kinematic and kinetic comparisons. Med Sci Sports Exerc. 2003;35:635–643. [DOI] [PMC free article] [PubMed]
- 10.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003:112–120. [DOI] [PubMed]
- 11.Goodman DA, Feighan JE, Smith AD, Latimer B, Buly RL, Cooperman DR. Subclinical slipped capital femoral epiphysis. Relationship to osteoarthrosis of the hip. J Bone Joint Surg Am. 1997;79:1489–1497. [DOI] [PubMed]
- 12.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986:20–33. [PubMed]
- 13.Isear JA, Jr., Erickson JC, Worrell TW. EMG analysis of lower extremity muscle recruitment patterns during an unloaded squat. Med Sci Sports Exerc. 1997;29:532–539. [DOI] [PubMed]
- 14.Ito K, Leunig M, Ganz R. Histopathologic features of the acetabular labrum in femoroacetabular impingement. Clin Orthop Relat Res. 2004:262–271. [DOI] [PubMed]
- 15.Ito K, Minka MA, 2nd, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect. A MRI-based quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. [DOI] [PubMed]
- 16.Kadaba MP, Ramakrishnan HK, Wootten ME. Measurement of lower extremity kinematics during level walking. J Orthop Res. 1990;8:383–392. [DOI] [PubMed]
- 17.Kadaba MP, Ramakrishnan HK, Wootten ME, Gainey J, Gorton G, Cochran GV. Repeatability of kinematic, kinetic, and electromyographic data in normal adult gait. J Orthop Res. 1989;7:849–860. [DOI] [PubMed]
- 18.Kassarjian A, Brisson M, Palmer WE. Femoroacetabular impingement. Eur J Radiol. 2007;63:29–35. [DOI] [PubMed]
- 19.Konishi N, Mieno T. Determination of acetabular coverage of the femoral head with use of a single anteroposterior radiograph. A new computerized technique. J Bone Joint Surg Am. 1993;75:1318–1333. [DOI] [PubMed]
- 20.Kubiak-Langer M, Tannast M, Murphy SB, Siebenrock KA, Langlotz F. Range of motion in anterior femoroacetabular impingement. Clin Orthop Relat Res. 2007;458:117–124. [DOI] [PubMed]
- 21.Laude F, Boyer T, Nogier A. Anterior femoroacetabular impingement. Joint Bone Spine. 2007;74:127–132. [DOI] [PubMed]
- 22.Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: part I. Techniques of joint preserving surgery. Clin Orthop Relat Res. 2004:61–66. [PubMed]
- 23.Leardini A, Chiari L, Della Croce U, Cappozzo A. Human movement analysis using stereophotogrammetry. Part 3. Soft tissue artifact assessment and compensation. Gait Posture. 2005;21:212–225. [DOI] [PubMed]
- 24.Leunig M, Beck M, Kalhor M, Kim YJ, Werlen S, Ganz R. Fibrocystic changes at anterosuperior femoral neck: prevalence in hips with femoroacetabular impingement. Radiology. 2005;236:237–246. [DOI] [PubMed]
- 25.Leunig M, Casillas MM, Hamlet M, Hersche O, Notzli H, Slongo T, Ganz R. Slipped capital femoral epiphysis: early mechanical damage to the acetabular cartilage by a prominent femoral metaphysis. Acta Orthop Scand. 2000;71:370–375. [DOI] [PubMed]
- 26.Mardones RM, Gonzalez C, Chen Q, Zobitz M, Kaufman KR, Trousdale RT. Surgical treatment of femoroacetabular impingement: evaluation of the effect of the size of the resection. J Bone Joint Surg Am. 2005;87:273–279. [DOI] [PubMed]
- 27.Meyer DC, Beck M, Ellis T, Ganz R, Leunig M. Comparison of six radiographic projections to assess femoral head/neck asphericity. Clin Orthop Relat Res. 2006;445:181–185. [DOI] [PubMed]
- 28.Murray RO, Duncan C. Athletic activity in adolescence as an etiological factor in degenerative hip disease. J Bone Joint Surg Br. 1971;53:406–419. [PubMed]
- 29.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999:93–99. [PubMed]
- 30.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. [DOI] [PubMed]
- 31.Pai YC, Rogers MW. Speed variation and resultant joint torques during sit-to-stand. Arch Phys Med Rehabil. 1991;72:881–885. [DOI] [PubMed]
- 32.Philippon MJ, Maxwell RB, Johnston TL, Schenker M, Briggs KK. Clinical presentation of femoroacetabular impingement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1041–1047. [DOI] [PubMed]
- 33.Reinschmidt C, van den Bogert AJ, Nigg BM, Lundberg A, Murphy N. Effect of skin movement on the analysis of skeletal knee joint motion during running. J Biomech. 1997;30:729–732. [DOI] [PubMed]
- 34.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. [DOI] [PubMed]
- 35.Siebenrock KA, Kalbermatten DF, Ganz R. Effect of pelvic tilt on acetabular retroversion: a study of pelves from cadavers. Clin Orthop Relat Res. 2003:241–248. [DOI] [PubMed]
- 36.Siebenrock KA, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am. 2003;85:278–286. [DOI] [PubMed]
- 37.Tannast M, Kubiak-Langer M, Langlotz F, Puls M, Murphy SB, Siebenrock KA. Noninvasive three-dimensional assessment of femoroacetabular impingement. J Orthop Res. 2007;25:122–131. [DOI] [PubMed]
- 38.Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;429:170–177. [DOI] [PubMed]
- 39.Wagner S, Hofstetter W, Chiquet M, Mainil-Varlet P, Stauffer E, Ganz R, Siebenrock KA. Early osteoarthritic changes of human femoral head cartilage subsequent to femoro-acetabular impingement. Osteoarthritis Cartilage. 2003;11:508–518. [DOI] [PubMed]
- 40.Wisniewski SJ, Grogg B. Femoroacetabular impingement: an overlooked cause of hip pain. Am J Phys Med Rehabil. 2006;85:546–549. [DOI] [PubMed]
- 41.Wyss TF, Clark JM, Weishaupt D, Notzli HP. Correlation between internal rotation and bony anatomy in the hip. Clin Orthop Relat Res. 2007;460:152–158. [DOI] [PubMed]
- 42.Zebala LP, Schoenecker PL, Clohisy JC. Anterior femoroacetabular impingement: a diverse disease with evolving treatment options. Iowa Orthop J. 2007;27:71–81. [PMC free article] [PubMed]