Abstract
We have used the ligamentum teres capitis to reconstruct the deficient or absent labrum in five patients with femoroacetabular impingement at the time of surgical hip dislocation. Two had a deficient labrum overlying a sectorial retroverted acetabulum causing pincer-type impingement. Three patients had the labrum previously resected arthroscopically. The minimum followup from surgery was 5 months (average, 10 months; range, 5–20 months). There were no intraoperative or postoperative complications related to the reconstruction. All patients had improvement in their clinical function and one patient underwent total hip arthroplasty at last followup for unresolved pain without radiographic progression of arthritis. Reconstruction of the labrum in patients with deficient or resected labrums at the time of surgical hip dislocation provides the theoretical advantage of sealing and stabilizing the hip joint, restoring the fluid layer which could potentially prevent continued cartilage degeneration.
Level of Evidence: Level II, prognostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Femoroacetabular impingement (FAI) has been well-described as a prearthritic hip condition [12, 15, 17]. The underlying structural problem leads to continued abutment between the femoral head and neck junction and acetabulum, which can lead to cartilage degeneration and labral damage [2, 13]. Two types of FAI have been described. Cam-type FAI is most common in men, physically active individuals, and heavy laborers [2, 13, 15, 17]. Patients have abnormally shaped proximal femurs and the “jamming” of the abnormally shaped femoral head into the acetabulum with flexion and internal rotation leads to abnormal sheer forces at the acetabular rim producing an outside in abrasion and avulsion of the cartilage from the subchondral bone most commonly in the anterosuperior rim area. This type of impingement is commonly associated with a labral tear which occurs late, and an avulsion of the cartilage from the base of the labrum. The labrum in this case is degenerated from its insertion into the acetabulum but the peripheral aspect is commonly preserved [14]. The second type of FAI is the pincer type which occurs in patients with abnormal acetabular morphology, most commonly caused by a retroverted acetabulum, but it can also be seen in patients with coxa profunda or protrusio [6, 18, 21]. This type of FAI may occur in patients who also perform activities in which the hip is placed into extreme ranges of motion. Sectorial or global overcoverage results in pincer FAI caused by abutment between the femoral head and neck junction and the pelvic rim with range of motion (which most commonly occurs with flexion and internal rotation but may occur in extension and external rotation). In this type of FAI, the labrum fails early and continued abutment results in labral degeneration, intrasubstance ganglion formation, or additional bone deposition at the rim of the socket.
Recently there has been increasing interest in the role and function of the acetabular labrum. There are new biomechanical data suggesting the effect of the labrum on hip stability [5, 7–10, 23]. One clinical study [5] also suggests the importance of preserving and refixing the labrum on the outcomes of impingement surgery. It would therefore seem reasonable that reconstruction of the labrum when deficient could theoretically provide a better biomechanical environment for the hip and could lead to improved outcomes.
We describe potential indications and surgical technique for reconstructing the labrum in patients with degenerated or absent labrum using the ligamentum teres. We also discuss the early clinical results and the potential pros and cons of this reconstruction.
Materials and Methods
We have used the ligamentum teres capitis to reconstruct the labrum in five patients undergoing open surgical management for FAI. There were three men and two women with an average age of 32.6 years (range, 19–50 years) (Table 1). The minimum followup from surgery was 5 months (average, 10 months; range, 5–20 months). No patients were lost to followup.
Table 1.
Patient demographics, radiographic findings, and followup
| Patient | Gender/age | FAI | Previous arthroscopy | Radiographic findings | Followup from surgery |
|---|---|---|---|---|---|
| 1 | M/19 | Combined | No | Femoral head-neck offset abnormalities. Retroversion. | 13 months |
| 2 | M/28 | Combined | No | Retroversion. Cam lesion. | 17 months |
| 3 | M/33 | Combined | Yes | Retroversion. Small cam lesion. | 5 months |
| 4 | F/33 | Pincer | Yes | Coxa profunda | 5 months |
| 5 | F/50 | Pincer | Yes | Coxa profunda | 20 months |
All of the patients had a positive impingement sign on physical examination [13]. Preoperative radiographic evaluation consisted of anterosuperior pelvic and cross-table lateral radiographs. All patients underwent MRI gadolinium arthrography. Three patients had evidence of retroversion as a positive crossover sign seen on the AP pelvis (patients 1, 2, and 3). Two patients had global overcoverage consistent with coxa profunda (patients 4 and 5), two patients had substantial cam lesions seen on the AP as well as on the cross-table lateral radiographs (patients 2 and 3). One patient had evidence of an impingement trough over the femoral head and neck junction consistent with pincer-type impingement (Patient 5). One had considerable head and neck offset abnormality but no true cam lesion (Patient 1). All five patients had MRI findings which confirmed FAI. Two patients had labral tears which were diagnosed with MRI arthrography (patients 1 and 2). The other three patients had abnormal or absent labrums seen on MRI (patients 3, 4, and 5). These three patients had undergone a previous arthroscopic labral resection.
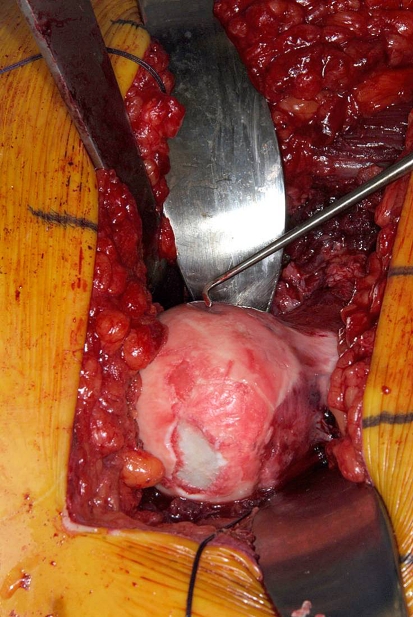
All patients underwent open surgical hip dislocation as described by Ganz et al. [11]. In summary, the patient was placed on the lateral decubitus position. A straight incision was carried distal from the iliac crest over the greater trochanter anteriorly over the proximal femur. The fascial incision was a routine extension of the Kocher gluteus maximus split. We incised the trochanteric bursa over the posterior border of the trochanter in line with the fascia. A digastric trochanteric osteotomy was then performed [11]. We took care to perform the osteotomy within the trochanter proximally to protect the deep branch of the medial femoral circumflex artery as it courses superiorly behind the greater trochanter and to ensure the majority of the tendon fibers of the piriformis remain on the stable trochanter. Capsular exposure was carried out in a Z-shaped fashion. We placed a bone hook underneath the neck of the femur, and subluxated the hip. Palpation of the round ligament was then carried out with the tip of a scissors. Blindly, but using the tip of scissors to palpate the ligament, we cut the ligamentum teres capitis at the level of its insertion into the transverse ligament and acetabular fossa in order to get its greatest length (Fig. 1). The head was then dislocated and leg placed in a pocket. The pathology was inspected. At the time of surgery all patients had associated acetabular chondral damage (Table 2) [2]. According to Beck’s criteria, three patients had Type II with roughening of the surface and fibrillation of the impingement area. Two patients had Type IV with a cleavage lesion which showed a loss of fixation to the subchondral bone. One patient had a full-thickness defect in the cartilage of the femoral head (Fig. 2). In three of the five cases (Patients 3, 4, and 5), no labrum was present anterosuperiorly as it had been previously resected arthroscopically. Two patients had ossification of the rim of the acetabulum (patients 4 and 5). In two patients (patients 1 and 2) with acetabular retroversion, a thin labral remnant was seen in the area of impingement and bony overgrowth. This thin labral remnant typical of prolonged sectorial pincer impingement was difficult to refix to the new rim. Acetabular trimming of femoral head and neck offset abnormalities were corrected as previously described [5].
Fig. 1.
The resected ligamentum teres has been obtained at its greatest length by detachment from its insertion on the acetabular transverse ligament.
Table 2.
Intraoperative findings
| Patient | Intraoperative findings | Treatment | Round ligament reconstruction “clock-face” for right hip (3 ___ ant, noon ___ sup) |
|---|---|---|---|
| 1 | Thin labrum over sectorial retroversion; Type II cartilage damage; Femoral head-neck offset abnormality. | Femoral head offset correction; Acetabular trimming. | Two to 3 |
| 2 | Thin labrum over sectorial retroversion; Type II. | Femoral head offset correction; Acetabular trimming. | Noon to 3 |
| 3 | Absent labrum over sectorial retroversion; Cam lesion; Type IV. | Femoral head offset correction; Acetabular trimming; Femoral head microfracture. | One to 3 |
| 4 | Absent labrum with rim ossification; Type II. | Global rim trimming. | Nine to 3 |
| 5 | Ossified rim with absent labrum; Type IV. | Global rim trimming. | Noon to 3 |
Fig. 2.
Patient 4, who had undergone previous arthroscopic débridement of the hip, shows a large femoral head defect and two other areas of what appear to be chondral damage of the femoral head.
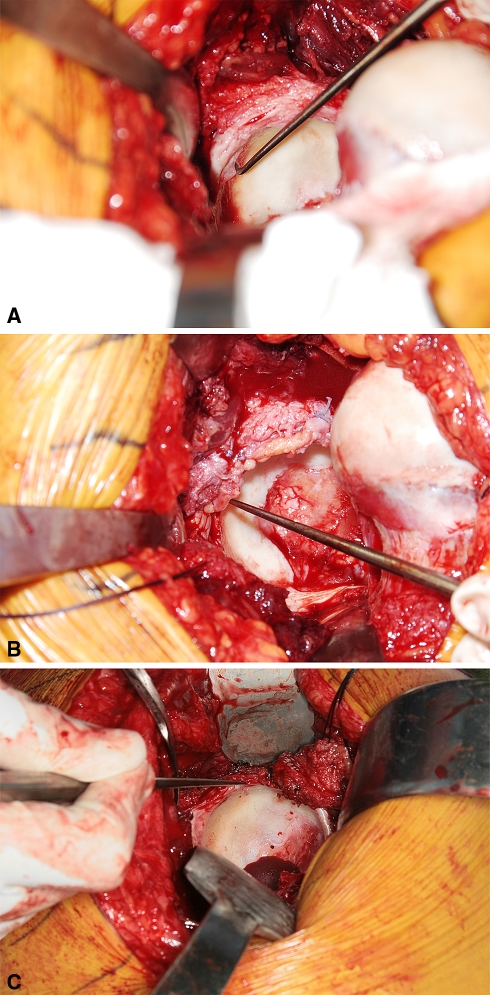
We resected the ligamentum teres from the fovea of the femoral head sharply with a knife, taking care to keep the longest possible length. Synovial tissue was removed as best as possible from the side that will be refixed to bone. In cases in which the ligament was short but wide and major reconstruction was necessary, the ligament can be opened longitudinally (Fig. 3A–B), keeping it attached from one edge. We usually freshened the rim as it has undergone, in most cases, rim trimming (acetabuloplasty) and bleeding bone should be evidenced. This provided a freshened rim for fixation of the remaining labrum and ligament. We fixed the ligamentum teres capitis to the acetabular rim using 2-mm suture anchors in the same way as labral refixation was performed during the course of this surgical procedure (Fig. 4A–B). Depending on the size of the round ligament to be reconstructed, usually the suture was placed approximately 7 to 10 mm apart. Additional 2–0 Monocryl sutures can be placed between the ligamentum teres and the adjacent capsule and native labrum to obtain stable fixation of the ligamentum teres to the rim.
Fig. 3A–B.
(A) Short and wide ligamentum teres is shown. (B) The ligamentum can be opened longitudinally, preserving its attachment to one side so that it can be expanded over the rim.
Fig. 4A–C.
(A) Patient 5 had severe ossification of the rim and Type IV cartilage damage to the acetabular rim. (B) After rim trimming and release of global over-coverage, the ligamentum teres has been attached to the acetabular rim to provide a sealing of the hip joint. (C) The round ligament has remodeled, healing to the rim, and no longer looks like ligament but resembles labrum.
Postoperatively, we instituted routine surgical hip dislocation rehabilitation. This entailed limiting flexion to 70° and limiting internal and external rotation for 6 weeks. To protect the trochanter fixation, the patients were toe-touch weightbearing for the first 4 weeks with advancement to partial weight bearing at 6 weeks. All patients were full weight bearing at 8 weeks by the time they obtained their first postoperative radiograph. Range of motion of the hip to prevent adhesions was encouraged. A continuous passive motion machine was used for 8 hours a day for 6 weeks, and patients were started on an exercise bike at low resistance starting on week 2.
The patients were seen at 2 and 4 months after surgery and then at 1 year for those patients at least 1 year past surgery. All evaluations were performed by one of the author surgeons (RJS). At the time of followup, clinical examination was performed, and an activity rating using the UCLA score was obtained [1]. In addition, patients underwent radiographic assessment for evaluation of trochanteric healing and stability of the suture anchors. An MRI was obtained selectively in patients to evaluate healing of the labrum to the acetabular rim.
Results
There were no intraoperative or postoperative complications. All trochanters healed. There was no evidence of anchor displacement. One patient underwent removal of screws 1 year after surgery because of trochanteric pain and continued pain with internal rotation of the hip; this patient subsequently underwent THA.
All patients reported improvement in their symptoms prior to surgery. Before surgery, three patients reported severe pain in the groin region, and two patients reported moderately severe pain. At final followup, three patients had no pain. One complained of moderate pain over the trochanter but not groin pain. One complained of continued pain in the groin with internal rotation of the hip, similar to preoperative pain and was not satisfied with the outcome.
The mean UCLA score [1] preoperatively was an average of 5 (range, 2–6); postoperatively the UCLA score increased to an average of 8.2 (range, 6–10). One patient had a perfect score of 10 and participated regularly in impact activities including running and cutting and decelerating three or four times a week (Patient 1). One patient had a score of 8 and participated in activities such as fast walking and performed activities such as running or cutting or decelerating at least once a month (Patient 2). One patient had a score of 9 and was back to daily heavy labor but was taking medication (on occasion, as needed) (Patient 3). Patient 4, who is 5 months from surgery, has no groin pain, no limp, and is extremely happy with the operation. She is riding a bike several hours a day (UCLA 8). Patient 5 had a postoperative UCLA score of 6. This patient had substantial preoperative cartilage damage, was improved somewhat with the offset but was limited in sporting activities. Her score improved from 4 to 6. Despite this modest improvement, the patient continued to have considerable pain with internal rotation of the hip which had not changed from prior to surgery. A decision was made to proceed with a total hip arthroplasty 20 months after the index procedure. At the time of total hip arthroplasty, we did not see progression in the patient’s arthritis. The area of chondromalacia at the 3 o’clock level was unchanged. In addition, we were able to get a second look at the reconstructed labrum. The round ligament did not appear as such but looked more like a labrum well-attached to the rim (Fig. 4C). Three months after THA the patient had no pain and was taking no medication.
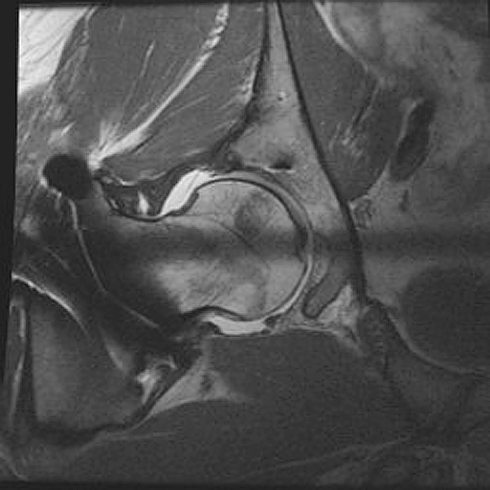
There was no progression in radiographic arthritis postoperatively. However, followup was quite short in all patients, and therefore we would not expect radiographic evidence of progression of arthritis even if the labrum had not been grafted. Postoperative MRIs in three patients showed healing of round ligament to bone and no progression in cartilage damage (Fig. 5). We did not obtain MRIs in the other two patients.
Fig. 5.
Radiosequence MRI shows the anterosuperior ligamentum teres which is well-attached to the acetabular rim with a good view of the posterior labrum as well. As can be seen on this figure, there is no extravasation of the fluid in between the ligamentum teres and acetabular bone suggesting that complete healing has occurred.
Discussion
There is clear clinical and biomechanical evidence to suggest that the labrum has an important role in hip mechanics and stability. A resected labrum, or one that cannot be repaired at the time of surgery, may lead to altered intraarticular pressures that could predispose to cartilage damage or progression of arthritis. Reconstruction of the absent or deficient labrum at the time of surgical dislocation has the potential of recreating the intraarticular pressure and sealing properties of the hip joint that could prevent progression of arthritis.
We believe that reconstruction of the labrum with the round ligament has the potential of restoring the seal to the hip joint, presuming sealing improves function. Limitations of this technique include the fact that the round ligament does not have the same structure as the labrum, and it is unlikely that it will function in the same way as the labrum does. The round ligament mostly serves as a “pseudolabrum” on the acetabular rim that could potentially prevent leaking of the synovial fluid and maintaining appropriate intraarticular pressures [7, 8], fluid film lubrication [7, 8], and thus minimize cartilage-on-cartilage contact which could lead to cartilage damage. We were able to see the results of our reconstruction in one patient that underwent a total hip arthroplasty, in this case the round ligament was well attached to the rim appeared more like a “pseudolabrum” than ligament. We do not know for sure if the negative intraarticular pressure was recreated though, which limits our conclusions. One limitation with using the ligament to reconstruct the labrum is its length. If extensive reconstruction is required, then other autograft tissue could be a better option.
The acetabular labrum is a fibrocartilaginous structure that is attached to the bony acetabular rim and physically deepens the acetabulum [22]. It is a triangular structure and in cross-section is widest in the anterior half and thickest in its superior half [19, 22]. The blood supply to the labrum derives from the joint capsule [16, 19]. From the capsule, blood vessels enter the peripheral part of the labrum and travel circumferentially around the structure at its attachment to bone. The inner two-thirds of the articular side is essentially avascular tissue.
A series of computer and in-vitro experiments [23, 24] have expanded the knowledge on the biomechanical properties of the acetabular labrum. Ferguson et al. [10], in their studies on the material properties of the bovine acetabular labrum, demonstrated that the labrum’s low permeability compared to the adjoining acetabular cartilage contributes to the sealing property attributed to the structure. They demonstrated that because of its high circumferential cell stiffness, the labrum also functions as a stabilizer of the joint. This function is even better seen if the osseous coverage is deficient, such as in a dysplastic hip. More recently, Crawford et al. [4] demonstrated that hip stability is affected by whether the hip labrum is intact or not. Using a 3-D motion analysis system, they compared the stability of six cadaver hips during loading maneuvers, and they repeated the measurements after venting the capsule and after creating a 15-mm tear into the intact labrum. When compared to the intact hip, approximately 43% to 60% less force was required to distract the femur by 3 mm after venting the capsule and after creating a tear in the labrum. They also demonstrated that external rotation in these hips increased when compared to the intact specimen. They concluded that a breach of the labrum affected femoral stability, especially during extreme range of motion. Although the reconstructed labrum does not have the same structure of the native labrum, the addition of a structure that heals to the trimmed acetabular rim could theoretically restore the sealing of properties of the hip joint. At this time we do not have conclusive evidence that this was restored with labral grafting.
There is early clinical evidence that labral refixation should be performed. Espinosa et al. [5] demonstrated a higher clinical success rate in patients who had open surgical hip dislocation with labral repair versus excision. Although the study was not randomized and the patients were operated in a sequential manner, this study does demonstrate the importance of labral repair and cannot overemphasize the importance of preserving the labrum when possible. The ligamentum teres may therefore help seal the joint and restore intraarticular pressures which could theoretically provide a better hip environment preserving cartilage from further degeneration.
Based on the theoretical biomechanical advantages and early clinical advantages seen in patients when the hip labrum is preserved, we believe reconstruction of the labrum when absent is reasonable. Although we did document healing of the ligament to the adjacent acetabular rim, it is very well possible that MRI may not be sensitive enough to determine the viability of the graft itself. Potential current indications for reconstructing the labrum with the ligamentum teres capitis include previously resected labrum; substantial rim ossification in pincer-type impingement; thin labrum with difficult refixation to the acetabular rim after trimming; and excessively torn degenerative labrum.
Chandler et al. [3] described the anatomy of the ligamentum teres in his 1932 paper. He dissected 114 femoral heads and ligaments. The average length of these ligaments was 2.5 cm with an average width of 1.5 cm. Histologically, they all had true ligamentous tissues and all ligaments contained vessels. It is our experience that the ligament is sometimes smaller than needed and if length is required such as in an ossified rim with no labrum, then it can be opened longitudinally and made longer (Fig. 3A–B).
The mechanism and action of the ligamentum teres is partly unknown. It may function as a secondary stabilizer of the hip. It is thought to tighten in hip abduction, flexion, and external rotation. On occasion disruption of the ligamentum teres may become painful. The patient may complain of episodes of giving way and pain predominantly in the thigh. Symptoms, however, are nonspecific [20]. The ligamentum teres is excised in all patients that undergo surgical hip dislocation. After a number of surgical hip dislocations performed at this institution and others there has been no mention whether excising the ligamentous teres has a deleterious effect on hip function, and especially there has been no evidence of clinically apparent hip instability associated with ligamentous teres excision.
To date no deleterious effect of using the ligamentum teres to reconstruct the labrum has been seen. The pain improvement was likely due to the FAI surgery and not necessarily due to the labral graft. The labral reconstruction with the round ligament has the potential of sealing the hip joint and decreasing progression of arthritis, but there is no doubt that the improvement in the pain and function of these patients was due to management of the underlying structural anomaly. Theoretically, it may provide the advantage of sealing the hip joint and creating a fluid layer which could prevent continued cartilage degeneration. It remains to be seen whether this is true, but theoretically this seems the most prudent thing to do in patients with an absent or severely damaged labrum at the time of surgical hip dislocation undergoing offset procedures.
Acknowledgments
We thank Professor Reinhold Ganz for contribution to the knowledge and care of patients with FAI and Karen Fasbender for her help with manuscript preparation.
Footnotes
Each author certifies that he has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the reporting of these cases, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Amstutz HC. Treatment of primary osteoarthritis of the hip: A comparison of total joint surface replacement arthroplasty. J Bone Joint Surg Am. 1984;66:228–241. [PubMed]
- 2.Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87:1012–1018. [DOI] [PubMed]
- 3.Chandler SB, Kreuscher PH. A study of the blood supply of the ligamentum teres and its relation to the circulation of the head of the femur. J Bone Joint Surg Am. 1932;14:834–846.
- 4.Crawford MJ, Dy CJ, Alexander JW, Thompson M, Schroder SJ, Vega CE, Patel RV, Miller AR, McCarthy JC, Lowe WR, Noble PC. The 2007 Frank Stinchfield Award. The biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res. 2007;465:16–22. [DOI] [PubMed]
- 5.Espinosa N, Rothefluh DA, Beck M, Ganz R, Leunig M. Treatment of femoroacetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88:925–935. [DOI] [PubMed]
- 6.Ezoe M, Naito M, Inoue T. The prevalence of acetabular retroversion among various disorders of the hip. J Bone Joint Surg Am. 2006;88:372–379. [DOI] [PubMed]
- 7.Ferguson SJ, Bryant JT, Ganz R, Ito K. The acetabular labrum seal: a poroelastic finite element model. Clin Biomech (Bristol, Avon). 2000;15:463–468. [DOI] [PubMed]
- 8.Ferguson SJ, Bryant JT, Ganz R, Ito K. The influence of the acetabular labrum on hip joint cartilage consolidation: a poroelastic finite element model. J Biomech. 2000;33:953–960. [DOI] [PubMed]
- 9.Ferguson SJ, Bryant JT, Ganz R, Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36:171–178. [DOI] [PubMed]
- 10.Ferguson SJ, Bryant JT, Ito K. The material properties of the bovine acetabular labrum. J Orthop Res. 2001;19:887–896. [DOI] [PubMed]
- 11.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip: a technique with full access to femoral head and acetabulum without the risk of avascular necrosis J Bone Joint Surg Br. 2001;83:1119–1124. [DOI] [PubMed]
- 12.Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466:264–272. [DOI] [PMC free article] [PubMed]
- 13.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. [DOI] [PubMed]
- 14.Ito K, Leunig M, Ganz R. Histopathologic features of the acetabular labrum in femoroacetabular impingement. Clin Orthop Relat Res. 2004;429:262–271. [DOI] [PubMed]
- 15.Ito K, Minka II MA, Leunig M, Werlen S, Ganz R. Femoroacetabular impingement and the cam-effect: a MRI-based, quantitative anatomical study of the femoral head-neck offset. J Bone Joint Surg Br. 2001;83:171–176. [DOI] [PubMed]
- 16.Kelly BT, Shapiro GS, Digiovanni CW, Buly RL, Potter HG, Hannafin JA. Vascularity of the hip labrum: a cadaveric investigation. Arthroscopy. 2005;21:3–11. [DOI] [PubMed]
- 17.Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoroacetabular impingement: Part I: techniques of joint preserving surgery. Clin Orthop Relat Res. 2004;418:61–66. [DOI] [PubMed]
- 18.Li PL, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res. 2003;416:245–253. [DOI] [PubMed]
- 19.Petersen W, Petersen F, Tillmann B. Structure and vascularization of the acetabular labrum with regard to the pathogenesis and healing of labral lesions. Arch Orthop Trauma Surg. 2003;123:283–288. [DOI] [PubMed]
- 20.Rao J, Zhou YX, Villar RN. Injury to the ligamentum teres: mechanism, findings, and results of treatment. Clin Sports Med. 2001;20:791–799. [DOI] [PubMed]
- 21.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum: a cause of hip pain. J Bone Joint Surg Br. 1999;81:281–288. [DOI] [PubMed]
- 22.Seldes RM, Tan V, Hunt J, Katz M, Winiarsky R, Fitzgerald Jr RH. Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop Relat Res. 2001;382:232–240. [DOI] [PubMed]
- 23.Takechi H, Nagashima H, Ito S. Intra-articular pressure of the hip joint outside and inside the limbus. J Japan Orthop Assoc. 1982;56:529–536. [PubMed]
- 24.Weber W, Weber E. Ueber die mechanik der menschlichten gehwerkzeuge nebst der beschreibung eines versuches ueber das herausfallen des schenkelkopfes aus der pfanne im luftverduennten raum. Annals Physics Chem. 1837;40:1–13. [DOI]