Abstract
Study Objectives:
Sleep reduction normally causes a homeostatic response during subsequent recovery sleep, but this does not seem to be true for repeated partial sleep loss. The aim of the present study was to test the response to repeated partial sleep loss through detailed focus on spectral data and parts of sleep.
Design:
The experiment involved 4 h of sleep across 5 days in the laboratory (partial sleep deprivation [PSD]), followed by 3 days of recovery sleep. PSD was achieved through a delayed bedtime. Nine individuals participated. To avoid “laboratory monotony,” subjects were permitted to leave the lab for a few hours each day.
Measurements and results:
All sleep stages and the latencies to sleep and slow wave sleep (SWS) showed a significant reduction during PSD. However, SWS and TST (total sleep time) during the first half of sleep increased gradually across days with PSD. During the first recovery sleep, SWS was significantly increased, while stage 1 and latency to stage 3 were reduced. All were back to baseline on the second night of recovery sleep. Summed spectral power during the first 3.8 h of sleep showed a gradual and robust increase (50% above baseline) in the range 1.25–7.25 Hz across days with PSD up to first recovery sleep and then returned to baseline.
Conclusions:
SWS and summed power density in a broad low-frequency band respond to repeated partial sleep deprivation in a dose-response fashion during the first 4 h sleep, apparently reflecting a robust and stable homeostatic response to sleep loss.
Citation:
Åkerstedt T; Kecklund G; Ingre M; Lekander M; Axelsson J. Sleep homeostasis during repeated sleep restriction and recovery: support from EEG dynamics. SLEEP 2009;32(2):217–222.
Keywords: SWS, spectral analysis, delta band, partial, deprivation
ACUTE SLEEP REDUCTION NORMALLY CAUSES A HOMEOSTATIC RESPONSE DURING THE NEXT SLEEP OPPORTUNITY, CHARACTERIZED BY INCREASED amounts of stage 3 and 4 (slow wave sleep [SWS])1,2 This increase occurs at the expense of REM sleep, stage 2 sleep, stage 1 sleep, and stage wake. The latter study also showed that spectral power density in the 0.5–8 Hz range increased but was most pronounced in the 0.5–4 Hz band, called “delta power.”
However, repeated partial sleep restriction does not seem to cause the same homeostatic response of SWS or of delta activity. Thus, Webb and Agnew3 found that stage 4 sleep was maintained at baseline levels for 8 days with 3 h of sleep, while all other stages were reduced. Values returned to baseline on the first recovery night. Carskadon and Dement4 found similar results for 5 h/night across 7 days, except for an increase in REM sleep during recovery sleep. The same lack of SWS response was reported by Brunner et al.5 for 4 days of 4 h sleep, but total sleep time (TST), REM, SWS, and delta power (during the first 4 h of sleep) were increased for 2 days of recovery sleep. Interestingly, though, the span of 1/4 Hz bands with increased spectral power increased beyond the 0.5–4 Hz band during partial sleep deprivation (PSD) nights, suggesting a compensation for the partial sleep deprivation.
In a study across 14 days, Van Dongen et al.6 showed that a reduction to 6 or 4 h of sleep per day caused a reduction on the first restricted night of summed NREM power in the 0.5–4 Hz band, TST, and all sleep stages except SWS. The changes across the days with sleep restriction were marginal and mostly nonsignificant, but REM latency decreased by 2.2 min/day in the 4-h condition, and SWS increased marginally. Similar observations (mainly lack of significant change in SWS across the experiment) were made across 7 days with 5 h sleep.7 Recovery was apparently complete on the first recovery night, since no difference from baseline was seen. In rodents Kim et al.8 showed an increase of NREM sleep during the first PSD sleep (of 4 h of sleep/day), but this was followed by a decrease of NREM and delta power during the subsequent 3 days. During recovery sleep, NREM did not respond during the first day, whereas delta power increased. During the next day, delta power actually decreased.
The discrepancy between the homeostatic response of SWS delta power after acute sleep loss and that during repeated partial sleep loss is puzzling in view of the homeostatic response after acute sleep reduction, but it may reflect a basic property of sleep. However, it could also be due to a lack of depth of analysis—the previous studies did not focus on the dynamics of sleep architecture. It might, for example, be fruitful to examine a wider part of the EEG spectrum. It might also help to focus attention on the smallest common TST denominator (≈4 h), since modest responses may be lost when the entire sleep period is used for analysis. The purpose of the present study was, therefore, to emphasize the previous 2 points in a study of the effects of partial sleep deprivation (4 h/night) across 5 days, followed by 3 days of recovery sleep (8 h in bed), on sleep polysomnography and EEG spectral content. The design of the study was an attempt to reflect the working week, with cumulative sleep restriction and subsequent recovery during the weekend. The main finding to come out of this study was a clear homeostatic response in EEG power from 1.25 to 7.25 Hz (summed across each sleep) during the nights of partial sleep deprivation, as well a clear homeostatic recovery during the first night of recovery sleep.
METHODS
Participants and Design
Nine healthy males (age range 23–28 y) participated in the study. All were non-smokers, non-obese (BMI range 21–26), moderate alcohol and coffee consumers, had a normal sleep need (habitual sleep need ranged between 7.0 and 8.5 h), and were not taking regular medication. The study was approved by the local ethical committee at Karolinska Institutet, and the study was carried out in accordance with the Helsinki Committee rules. All participants gave their informed written consent after the procedures had been fully explained. Subjects were compensated economically for participation.
Subjects adhered to a sleep schedule, with bedtimes at 23:00 ± 30 min and rise times 07:00 ± 30 min in their own homes, starting 2 weeks prior to the first laboratory day. The habituation day (sleep 23:00–07:00) was followed by 4 days in their own homes (sleep 23:00–07:00). This was followed by 10 days in the sleep laboratory with 2 baseline days (B1-B2, sleep 23:00–07:00), 5 days with partial sleep deprivation (P1-P5, sleep 03:00–07:00), and 3 recovery days (R1-R3, sleep 23:00–07:00). Blood was drawn every hour from 23:00–08:00 and every third hour from 08:00–23:00 during 9 days (B1, B2, P1, P2, P5, R1, R2, R3, R7). The IV catheter was inserted 2 h prior to blood sampling at 20:00 each day. Sampling between 23:00 and 08:00 was conducted from an adjacent room through the wall of the sleep unit. R7 was used as a reference day to ensure that baseline levels were reached and that no systematic change occurred across the experimental days.
In the laboratory, subjects slept in separate, insulated bedrooms, and could watch video, play games, read books/magazines, use the internet, and were allowed light work or studies. To reduce possible effects of laboratory monotony, subjects spent time outdoors at least twice each day (between 09:00 and 19:00). All meals were consumed during the hour following each daytime blood sample. Subjects were not permitted to smoke, use alcohol, take naps, or engage in strenuous physical activity from 2 days before the experiment to its end. To facilitate recruitment of participants (Sweden has the second highest coffee consumption in the world), participants were permitted one standard cup of coffee each morning, after tests and blood drawing. During the excursions outside the laboratory participants were accompanied by an experimenter. The subjects were monitored through actigraphs starting 7 days before the start of the experiment and throughout.
Sleep Recording and Analysis
Sleep was recorded polysomnographically using Embla recorders (Flaga HF) with 2 EEG derivations C3–A2 and C4–A1, one chin electromyographic (EMG) derivation, and 2 electro-oculogram (EOG) oblique derivations. Ag/AgCl electrodes were used. The signal quality of the recordings was carefully checked before bedtime. The AD board used a 16-bit width, the sampling rate was 100 Hz, and filter settings were 0.5–32 Hz. Sleep stages were scored visually in 20-sec epochs according to Rechtschaffen and Kales.10 The standard polysomnographic parameters were computed: total sleep time (TST), of sleep stages 1-4 and REM; wake after sleep onset (WASO); time to onset of stage 1 (sleep latency); time to stage 3 from sleep onset (SWS latency); and time to first stage REM from sleep onset (REM latency).
The EEG was also subjected to spectral analysis using Somnologica software. The analysis was based on 4-sec epochs after careful artifact removal. Results are presented as spectral density in 1/4 Hz intervals during NREM sleep, summed across the entire sleep episode and expressed as percent change from the mean of the 2 baseline conditions. In addition, mean spectral power per 20-sec epoch for each 1/4 Hz band was computed for the first 3.8 h. The latter was the shortest common denominator for sleep duration.
Statistical Analysis
Repeated measures analysis of variance (ANOVA) was used to analyze subjective ratings and results of visual sleep scoring; the Huyhn-Feldt epsilon correction was applied to adjust for violations against the assumption of sphericity. The mean of the 2 baseline sleep periods were used as a baseline value (B). Separate analyses were made for B to R3, to test for overall change across the entire experiment, as well as for P1-P5 to test for gradual adjustment to partial sleep deprivation. The analyses were carried out for the full sleep episode as well as for the first 3.8 h, which was the lowest common denominator for sleep duration.
For the spectral power data, a different analysis was carried out to investigate what bands would show a significant change. For this purpose, the percentage change from the mean baseline was computed for each 1/4 Hz band, together with the 95% confidence interval (CI). This was done both for total accumulated power across the entire sleep episode and for the mean epoch power during the first 3.8 h. CI was interpreted as a significance test for deviation from baseline. In addition, spectral power density across the 0.5–4 Hz interval was integrated and analyzed using a repeated measures ANOVA. The same procedure was followed for the maximum bandwidth that showed changes with partial sleep deprivation. To support a discussion of dynamics significant overall F-ratios were followed up by t-test of change between baseline and subsequent days.
RESULTS
Sleep Architecture
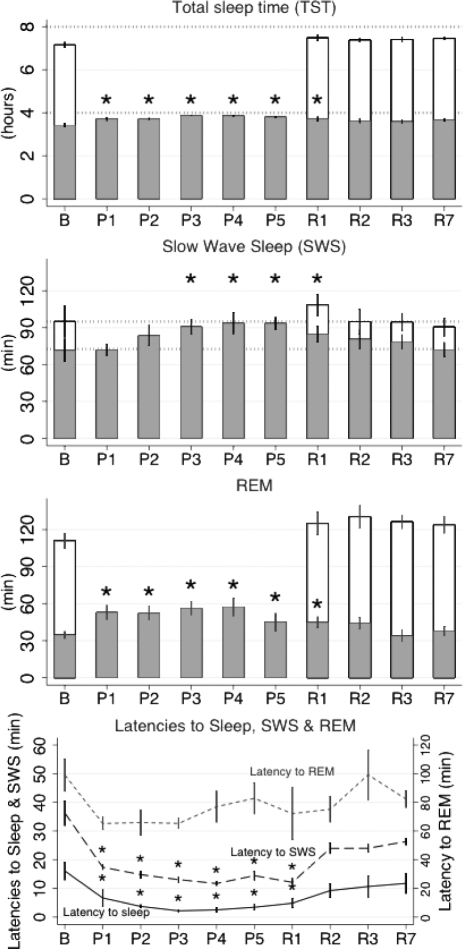
Table 1 shows that for the full sleep episode, TST, stage1, stage 2, SWS, REM, SWS latency, and sleep latency varied significantly across the experiment (Fig 1. displays the key variables). T-tests showed a significant fall from B to P1 for TST, stage 1, stage 2, REM, sleep latency, and SWS latency (P < 0.05), and the reduction remained significant up to P5, except for SWS, which was no longer significant from B by P2. Sleep latency and SWS latency remained significantly reduced up to and including R1. REM latency did not vary significantly (but a t-test showed that REM latency fell significantly from B to P1). During recovery sleep R1 differed significantly from B only for stage 1 and stage 3 latency (both reductions with P < 0.05). When only the 5 days of PSD were analyzed, SWS increased significantly across days, as did TST.
Table 1.
F and P-Values for ANOVAS for Spectral Analysis and Scored Values of Sleep Variables: Full Sleep Period Across the Total Protocol and PSD Nights, Respectively, as Well as for the First 3.8 h of Sleep Across the Total Protocol
| Full sleep Total prot | Full sleep PSD | First 3.8 h of sleep Total prot | |
|---|---|---|---|
| TST | 648*** | 3.5* | 4.7*** |
| SWS | 5.2*** | 4.8** | 3.3* |
| REM | 41.5*** | 0.9 | 4.0*** |
| Stage 1 | 11.9*** | 2.2 | 2.3* |
| Stage 2 | 124*** | 2.1 | 2.5* |
| Sleep latency | 4.4** | 1.6 | |
| SWS latency | 6.4*** | 0.9 | |
| REM latency | 1.2 | 1.6 | |
| Power 0.5–4.0 Hz | 4.2** | 0.8 | 1.3 |
| Power 1.25–7.25 Hz | 8.9*** | 1.8 | 2.9* |
PSD = 4 h between 03:00-07:00h, B = Baseline, R = Recovery, SWS = Slow wave sleep. P-values for ANOVA:
P < 0.05,
P < 0.01,
P < 0.001, after the Hyunh-Feldt correction. Degrees of freedom (df) for sleep stages and latencies across the entire protocol = 8,64; across PSD-days = 4,32
Figure 1.
Mean ± SE per night across the experiment for TST, SWS, REM sleep, Latency to stage 1, REM, and stage 3. Shaded = first 3.8 h of sleep; unfilled = remainder of full sleep (8 h TIB). Asterisks indicate significant difference (t-tests) from B for the first 3.8 h of sleep. B = baseline, P = partial sleep deprivation days, R = recovery days.
When only the first 3.8 h were analyzed, the change across the experiment was significant for TST, SWS, REM, and stage 1 and 2. Compared to baseline, REM increased abruptly on P1 (P < 0.05), remained significantly increased (at least P < 0.05) across all days with PSD and on R1. SWS did not change significantly from baseline to P1 but rose gradually towards a significant difference from B at P3 and remained significantly increased until and including R1. Stage 1 and 2 decreased during PSD. (Figure 1)
Spectral Analysis
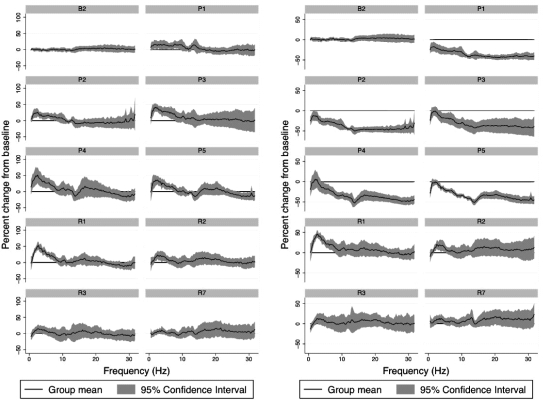
The spectral analysis was first applied to the full sleep period in order to reflect accumulation of power. Figure 2 (right panel) shows the percentage change and 95% CI of spectral power in 1/4 Hz bands summed across the NREM epochs of full sleep duration, presented relative to the mean of the 2 baseline sleep periods. Night B2 has been included in the figure to give an impression of the baseline variability. The results show that during P1, all frequencies were significantly reduced, but during the remaining PSD nights, small portions of the bands remained at baseline levels while the rest were reduced. In P2, this was true for the 1.50–1.75 Hz interval, in P3 the 1.00–3.25 Hz band, in P4 the 0.75 Hz–3.50 Hz band, and in P5 the 1.00–3.00 Hz band. The first recovery sleep (R1) showed a significant rebound above baseline for the interval 1.25–7.75 Hz. By recovery night 2 the 1.75–5.00 Hz band remained significantly increased, and by R3 only the 1.50–1.75 Hz interval remained significantly elevated.
Figure 2.
Mean and 95% confidence interval per 1/4 Hz band of spectral power summed across NREM stages for each full sleep episode (left) and across the first 3.8 h of sleep (right). B = baseline, P = partial sleep deprivation days, R = recovery days.
Figure 2 (left panel) shows a similar analysis for the first 3.8 h of sleep. For P1 the 1.5 Hz–9.25 Hz range was significantly increased (CI not overlapping baseline) with a few exceptions. In addition, the 13–13.5 Hz interval was increased. For P2 the range 1.00–7.25 Hz was significantly increased, for P3 the 0.75–7.75 Hz range, for P4 the 1.00–7.50 Hz range, and for P5 the 1.25–7.00 Hz range. The peak frequency in P1 was rather indistinct, with one peak occurring at 1.75 Hz and another one at 4.50 Hz. For P2 the peak was at 2.5 Hz, for P3 at 2.0 Hz, for P4 at 2.5 Hz, and for P5 at 2.5 Hz. For the recovery days, R1 showed a significant increase above baseline for the range 1.00 Hz–8.00 Hz. R2 was significantly increased for the range 1.75–5.26 Hz, R3 for 2.25–3.75 Hz, while R7 showed no significant elevation.
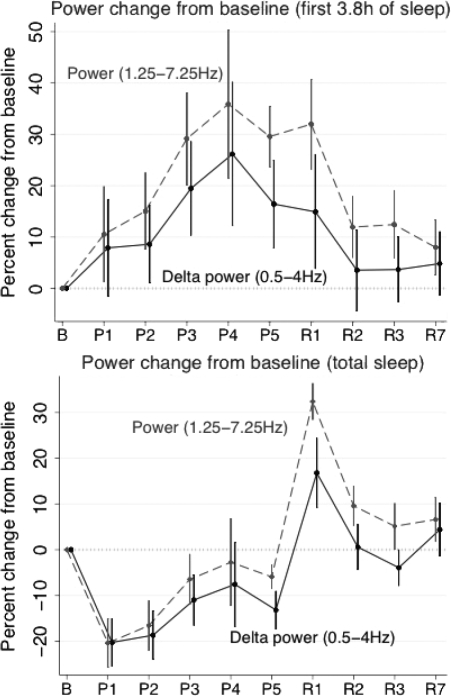
The traditional 0.5–4 Hz band summed across the full sleep episodes was also subjected to the same ANOVA for repeated measures as the visually scored polysomnography (Table 1 and Figure 3). The variation across the experiment was significant, but the change across PSD nights was not. Since the bandwidth of significant response, as demonstrated above, extended across the 1.25–7.25 Hz interval, ANOVA was carried out based on that interval. This showed a significant change across the experiment, but not for the change across PSD.
Figure 3.
Mean ± SE for spectral power in the 0.5–4 Hz and 1.25–7.25 Hz bands summed across each full sleep episode (bottom) and across the first 3.8 h of sleep (top). B = baseline, P = partial sleep deprivation days, R = recovery days.
Applying the same analysis as above to the first 3.8 h of each sleep episode yielded a highly significant change across the experiment for the 1.25–7.25 Hz band. The increase was gradual from B to R1 and thereafter a gradual decrease was seen. The change for the 0.5–4 Hz band was not significant.
DISCUSSION
With respect to conventional sleep scoring parameters, there was a significant variation across the experiment for TST, stage 1, stage 2, REM, SWS, latency to stage 1, and latency to SWS. These results resemble those of Van Dongen et al.6 and Belenky et al.,7 but there are differences. None of the studies found any change in SWS amounts. In the present analysis, SWS showed a gradual increase across the PSD nights; this was not found in the studies of Van Dongen et al. and Belenky et al.6,7 Neither of those studies analyzed the latencies to stage 1 and 3, which, in the present study were reduced during PSD and on R1, suggesting an increased pressure for sleep. The reduction of the SWS latency was abrupt on P1 and remained significantly reduced up to R1. The results suggest that SWS amounts respond, albeit rather weakly, to PSD but more strongly in terms of SWS latency. REM sleep, however, does not seem to change homeostatically in response to PSD, but only shows a truncation due to reduced TIB. The increased sleep pressure is also visible in the increase of TST across the PSD nights.
The analysis across the entire protocol, using the first 3.8 h, indicates a dynamic response of SWS to partial sleep deprivation. There was significant variation across the experiment for SWS and REM. The PSD increase and recovery decrease of SWS was gradual, while the increase of REM sleep was abrupt on P1, remained increased up to R1, and was back to baseline by R2. The observation that REM increased on P1 while there was no significant change for SWS from B to P1 seem paradoxical, given the well-established sensitivity of SWS to prior sleep loss. This lack of response in SWS minutes during P1, together with the decreased SWS latency, seems counterintuitive; however, it may reflect SWS pressure being counteracted by an increased need for REM caused by the delayed bedtime. Such an increase in REM priority during morning/late night is well established and related to the circadian rhythm of core temperature.11 REM-initiated interference with SWS would be expected to curtail the maintenance of SWS, but not necessarily the latency to SWS. Even if REM responds homeostatically to selective REM deprivation,12 the increased REM amount on P1 is unlikely to be due to such influences, since SWS is given priority after sleep reduction.1,13 Still, very little is known about REM homeostasis in connection with partial sleep loss without a delayed bedtime.
Regarding recovery sleep, the impression is that all visually scored sleep variables had returned to baseline level by night 2. Brunner et al.5 found that REM, sleep latency, and SWS were increased for at least 2 days of recovery. Recovery was not reported in the study by Van Dongen et al.,6 but Belenky et al.7 reported a return to baseline sleep levels on the first recovery night. Thus, it appears that one to two nights of normal sleep may be sufficient to recover from a week of restriction to 4 hours in bed per night. Repeated weeks of partial sleep deprivation may show other results, however. Looking only at the first 3.8 h of sleep, one arrives at the same conclusion. This does not necessarily mean that also sleepiness or performance capacity would show the same pattern.
The spectral analysis of the full sleep episode showed reduced power in all bands except for 1–3 Hz during day 3 to 5 of PSD. During R1 there was an increase in the 1.25–7.75 Hz range, during R2 in the 1.75–5 Hz range, and during R3 only in the 1.50–1.75 Hz range. Thus much less low-frequency power was accumulated during PSD compared to baseline levels, but much of this deficit seems to be recovered during recovery nights. The fact that the 1–3 Hz range retained its original accumulated power after the initial decrease during P1 and P2 suggests, together with the strong increase in that range when power was analyzed during the first 3.8 h, that the response to PSD was particularly strong in that frequency band. Note, however, that the power density is highest in the lower frequencies, in which there was only a limited loss of accumulated power. The loss was mainly restricted to the higher frequencies, which account for a smaller part of the total power. This suggests that the loss of power density may be less severe than suggested by Figure 2.
The results above, together with other similar observations,2,14 suggest that the measurement of sleep homeostasis should include higher frequencies than the formal delta band. This conclusion is further supported by the more pronounced effect observed in the power analysis for the 1.25–7.25 Hz band, compared to the traditional 0.5–4.0 Hz band. The latter did not even reach significance for the analysis of the first 3.8 h of sleep, which agrees with the results of Van Dongen et al.6
The behavior of SWS and power in the 1.25–7.25 Hz band gives the impression of a dynamic response to repeated partial sleep deprivation. It is seen to some extent in the analysis of full sleep as the gradual SWS increase across PSD nights and in the rebound of power on R1. This effect is particularly clear when only the first 3.8 h of sleep are considered, since SWS shows a gradual increase from B to P5/R1 and thereafter a gradual fall, with the same pattern seen for spectral power. The effect on SWS may have been even larger without the putative interference by REM sleep. The increase in SWS or power in the delta/theta band for the 3.8 h analysis peaked on P4 and remained the same on P5 and R1, implying that the additional SWS and delta/theta power during the full R1 sleep occurred in the second half of sleep. A similar observation was made for power in the 1.25–7 Hz band. Thus, there must have been a need for SWS that was not satisfied during the first half of sleep, presumably because the need was not strong enough in relation to the already increased level of SWS. As VanDongen et al. has shown,6 a strongly increased need, as for example, after total sleep loss, is able to increase SWS far above the levels produced after many days of 4 h sleep. This comparison of full sleep with its first half suggests that sleep adjusts its rate of recovery of SWS to an expectation of a full duration (7–8 h) sleep episode. Therefore, the low-frequency power accumulated during each night of PSD probably represents an “appropriate” and homeostatic response to sleep given that a full duration (7–8 h) sleep is (mistakenly) “anticipated” by the sleep mechanism.
It should be emphasized that the width of the spectral band that is “sensitive” to sleep loss was selected somewhat arbitrarily, in the sense that the range from 1.00 to 7.75 seemed to be affected, but in a less stable way. Thus, we selected a slightly more conservative interval. The optimal range will be determined in future studies.
The present study has several limitations. Firstly, the study only used one PSD condition (4 h) and one duration of time in bed (8 h) for baseline and recovery, respectively. This restricts any generalizations to these specific conditions. Similarly, generalizations must be restricted to young and healthy adult Swedish volunteers. Also, the modest size of the study may affect generalizability.
Another limitation is that the design used the individuals as their own controls and did not employ a control group. This may affect the interpretation of the results, but since 3 consecutive recovery days were used, as well as a seventh day of recorded recovery sleep for reference, a bias in interpretation seems less likely. One might also argue that permitting subjects some hours away from the laboratory each day may have affected the results compared to being exposed to a highly controlled laboratory situation. This excursion was, however, repeated each day and should not have had systematic effects on the PSD days only, particularly since they were supervised by an experimenter and monitored through actigraphy. Another factor that might have interfered with the results is the blood sampling procedure. It may have counteracted some of the homeostatic effects, even if SWS and delta power seems relatively unaffected in males.16
In summary, the present results show that a reduction of time in bed to 4 hours across 5 nights will result in a homeostatic response in SWS and spectral power in the 1.25–7 Hz band, particularly evident during the first 4 h of sleep. By recovery night 2, sleep appears to be back to baseline.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Åkerstedt is on the advisory board for Nycomed AB. Dr. Kecklund has participated in a speaking engagement for Boehringer Ingelheim, Sweden. Dr. Axelsson has participated in industry sponsored speaking engagements. The other authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
This study was supported by the Swedish Council for Working Life and Social Sciences and the Bank of Sweden Tercentenary Fund.
REFERENCES
- 1.Webb WB, Agnew JHW. Stage 4 sleep: influence of time course variables. Science. 1971;174:1354–6. doi: 10.1126/science.174.4016.1354. [DOI] [PubMed] [Google Scholar]
- 2.Borbély AA, Baumann F, Brandeis D, Strauch I, Lehmann D. Sleep deprivation: effects on sleep stages and EEG power density in man. Electroencephalogr Clin Neurophysiol. 1981;51:483–93. doi: 10.1016/0013-4694(81)90225-x. [DOI] [PubMed] [Google Scholar]
- 3.Webb WB, Agnew HW. Sleep: Effects of a restricted regime. Science. 1965;150:1745–7. doi: 10.1126/science.150.3704.1745. [DOI] [PubMed] [Google Scholar]
- 4.Carskadon MA, Dement WC. Cumulative effects of sleep restriction on daytime sleepiness. Psychophysiology. 1981;18:107–13. doi: 10.1111/j.1469-8986.1981.tb02921.x. [DOI] [PubMed] [Google Scholar]
- 5.Brunner P, Dijk D-J, Borbély AA. Repeated partial sleep deprivation progressively changes the EEG during sleep and wakefulness. Sleep. 1993;16:100–13. doi: 10.1093/sleep/16.2.100. [DOI] [PubMed] [Google Scholar]
- 6.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 7.Belenky G, Wesensten NJ, Thorne DR, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003;12:1–12. doi: 10.1046/j.1365-2869.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- 8.Kim Y, Laposky AD, Bergmann BM, Turek FW. Repeated sleep restriction in rats leads to homeostatic and allostatic responses during recovery sleep. Proc National Academy of Sciences, USA. 2007;104:10697–702. doi: 10.1073/pnas.0610351104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McEwen BS. Sleep deprivation as a neurobiologic and physiologic stressor: allostasis and allostatic load. Metabolism Clinical and Experimental. 2006;55:S20–S3. doi: 10.1016/j.metabol.2006.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Rechtschaffen A, Kales A. Bethesda: US Department of Health, Education and Welfare, Public Health Service; 1968. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. [Google Scholar]
- 11.Weitzman ED, Czeisler CA, Zimmerman JC, Ronda JM. Timing of REM and stages 3 + 4 sleep during temporal isolation in man. Sleep. 1980;2:391–407. [PubMed] [Google Scholar]
- 12.Beersma DGM, Dijk DJ, Blok CGH, Everhardus I. REM sleep deprivation during 5 hours leads to an immediate REM sleep rebound and to suppression of non-REM sleep intensity. Electroencephalogr Clin Neurophysiol. 1990;76:114–22. doi: 10.1016/0013-4694(90)90209-3. [DOI] [PubMed] [Google Scholar]
- 13.Agnew HW, Webb WB. The influence of time course variables on REM Sleep. Bulletin of the Psychonomic Society. 1973;3:131–3. [Google Scholar]
- 14.Brunner DP, Dijk D-J, Tobler I, Borbély AA. Effect of partial sleep deprivation on sleep stages and EEG power spectra: evidence for non-REM and REM sleep homeostasis. Electroencephalogr Clin Neurophysiol. 1990;75:492–9. doi: 10.1016/0013-4694(90)90136-8. [DOI] [PubMed] [Google Scholar]
- 15.Van Dongen HPA, Dinges DF. Sleep debt and cumulative excess wakefulness. Sleep. 2003;26:249. [Google Scholar]
- 16.Vitiello MV, Larsen LH, Moe KE, Borson S, Schwartz RS, Prinz PN. Objective sleep quality of healthy older men and women is differentially disrupted by nighttime periodic blood sampling via indwelling catheter. Sleep. 1996;19:304–11. doi: 10.1093/sleep/19.4.304. [DOI] [PubMed] [Google Scholar]