Abstract
FLT3 (fms-related tyrosine kinase 3) is a receptor tyrosine kinase class III that is expressed on by early hematopoietic progenitor cells and plays an important role in hematopoietic stem cell proliferation, differentiation and survival. FLT3 is also expressed on leukemia blasts in most cases of acute myeloid leukemia (AML). In order to determine the frequency of FLT3 oncogene mutations, we analyzed genomic DNA of adult de novo acute myeloid leukemia (AML). Polymerase chain reaction (PCR) and conformation-sensitive gel electrophoresis (CSGE) were used for FLT3 exons 11, 14, and 15, followed by direct DNA sequencing. Two different types of functionally important FLT 3 mutations have been identified. Those mutations were unique to patients with inv(16), t(15:17) or t(8;21) and comprised fifteen cases with internal tandem duplication (ITD) mutation in the juxtamembrane domain and eleven cases with point mutation (exon 20, Asp835Tyr). The high frequency of the flt3 proto-oncogene mutations in acute myeloid leukemia AML suggests a key role for the receptor function. The association of FLT3 mutations with chromosomal abnormalities invites speculation as to the link between these two changes in the pathogenesis of acute myeloid leukemiaAML. Furthermore, CSGE method has shown to be a rapid and sensitive screening method for detection of nucleotide alteration in FLT3 gene. Finally, this study reports, for the first time in Saudi Arabia, mutations in the human FLT3 gene in acute myeloid leukemia AML patients.
Keywords: AML, Flt3, ITD, CSGE, Mutational analysis
1. Introduction
The FLT3 gene (fms-like tyrosine kinase), is a member of the class III tyrosine kinase receptor family that includes c-kit, c-fms and the platelet-derived growth factor receptors (PDGFRs) [1–3]. Class III receptor tyrosine kinases (RTKs) share sequence homology and have a similar overall structure, with five immunoglobulin-like repeats in the extracellular domain, a single transmembrane domain (TM), a juxtamembrane domain (JM), two intracellular tyrosine kinase domains (TK1 and TK2) divided by a kinase insert domain (KI), and a C-terminal domain [4]. The genomic locus encoding the FLT3 receptor has recently been shown to comprise 24 rather than the expected 21 exons, ranging 83–562 bp [5]. Data from different sources suggest a pathogenic role of FLT3 in acute myeloid leukemia (AML). Hence functional analysis of FLT3 expression has been documented in many cases of AML, besides of immortalized human myeloid and monocytic cell lines [3, 6–8]. The ITD and activation loop mutations of the receptor have resulted in the constitutive FLT3 kinase activity and FLT3 receptors harboring such mutations when introduced into mammalian cells downstream signaling pathways lead to factor-independent growth in vitro and leukemogenesis in vivo [9, 10]. Thus the production of FLT3 mutant protein in primary murine bone marrow cells induces a lethal myeloproliferative phenotype [11]. It is known that FLT3 is a leukemia oncogene and activating FLT3 mutations are likely to contribute in the development of leukemia in humans.
In addition, several small molecule inhibitors have also been implicated in blocking the kinase activity of FLT3 effectively [11–14]. These can prolong the life span of mice harboring leukemia expressing mutant FLT3 receptors [11, 15]. In clinical trials, FLT3 inhibitors reduced FLT3 phosphorylation [16–18], and lowered leukemia blast counts in patients with advanced therapy-refractive AML [18, 19].
Until now, no study has reported the frequency and prevalence of FLT3 mutations in AML patients in the Kingdom of Saudi Arabia. This study was conducted with that objective in mind and was therefore undertaken using polymerase chain reaction-conformation sensitive gel electrophoresis (PCR-CSGE) on DNA extracted from archival bone marrow of Saudi AML patients.
2. Results and Discussion
2.1. Detection of the FLT3-ITD mutation
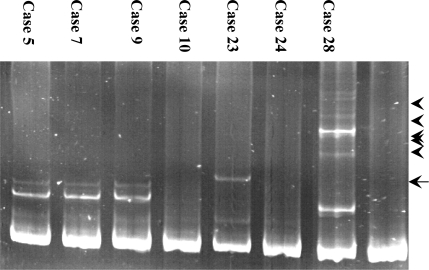
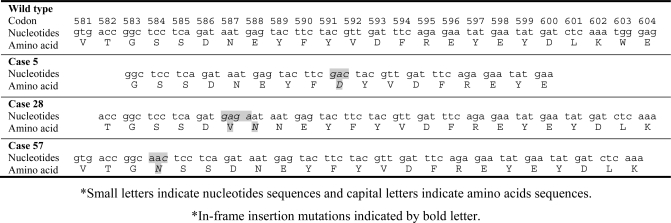
In order to screen for the FLT3-ITD mutation, exons 14 and 15 of the FLT3 gene were amplified from genomic DNA of 129 AML patients using PCR, followed by conformation sensitive gel electrophoresis (CSGE) analysis. Abnormal CSGE patterns in 15 AML patients were identified in PCR fragments and the remaining patients reported no such patterns. These abnormal patterns, shown in Figure 1, were due to conformational changes occurred in the gel indicating nucleotide alteration (in-frame insertion mutation) within the PCR fragment. When direct DNA sequencing analysis was carried out on all 15 AML cases with abnormal CSGE patterns, ITD mutations were detected in all cases with lengths varying between 24–60 bp. The FLT3-ITD mutations detected included either a part or whole stretch of tyrosine-rich sequence of the FLT3 gene located between codons 589–599 (Figure 2). Furthermore, these mutations were located in-frame of the JM domain of FLT receptor which gave the evidence of tandem duplications, thus confirming the ITD in the samples.
Figure 1.
CSGE analysis of exons 14 and 15 PCR product amplified from AML patients. CSGE gel demonstrating abnormal patterns (indicated by arrowheads) compared to normal pattern (lane N, PCR product amplified from healthy individual, indicated by arrow).
Figure 2.
Sequence analysis of exons 14 and 15 of FLT3 gene. Inserted nucleotides for tandem duplications of the Flt3 gene observed in AML cases with apparent CSGE patterns.
2.2. Detection of the Asp835Tyr mutation
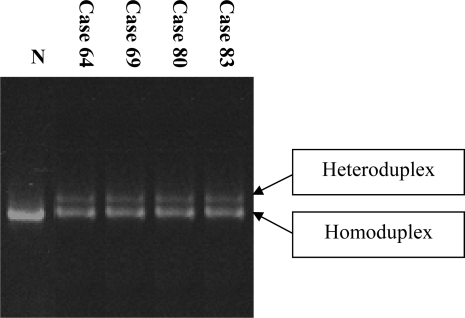
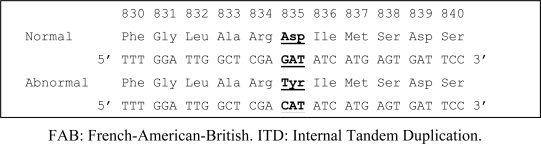
In addition to the FLT3-ITD mutation, the Asp835Tyr mutation is also prevalent in AML cases. To screen our cohort for the presence of this mutation, exon 20 of the FLT3 gene was subjected to PCR-CSGE followed by direct sequencing in all 129 AML cases. Eleven cases of AML (8.5%) exhibited an abnormal CSGE pattern (Figure 3), and sequencing revealed a G to C mutation in codon Asp835Tyr (Figure 4). Six of these were classified as AML M4, four of which demonstrated inv(16). In addition, FLT3 ITD mutations were identified in 15 patients; however, no case possessed both an ITD and Asp835 mutation jointly. The detailed clinical characteristics of AML patients forming the basis of this observation are summarized in Table 1.
Figure 3.
CSGE analysis of exon 20 of FLT3 gene demonstrating abnormal CSGE pattern compared to that seen in a normal individual (Lane N).
Figure 4.
Point mutation in exon 20 of FLT 3 gene in AML cases detected by direct DNA sequence analysis. Mutated nucleotides are represented by changed amino acid, (bold).
Table 1.
Clinical characteristics of AML cases and accompanied mutations.
| Case no. | Age (years) | Sex | FAB subtype | Karyotype | Mutations |
|---|---|---|---|---|---|
| 5 | 73 | F | M3 | 46;XY, t(15;17) | ITD |
| 7 | 32 | M | M3 | 46;XY, t(15;17) | ITD |
| 9 | 48 | F | M3 | 46;XY, t(15;17) | ITD |
| 12 | 51 | F | M2 | 46;XY, t(8;21) | ITD |
| 18 | 24 | F | M3 | 46;XY, t(15;17) | ITD |
| 20 | 62 | F | M3 | 46;XY, t(15;17) | ITD |
| 23 | 32 | M | M4 | 46;XY, inv(16) | ITD |
| 25 | 33 | M | M4 | 46;XY, inv(16) | ITD |
| 28 | 38 | M | M3 | 46;XY, t(15;17) | ITD |
| 29 | 46 | F | M2 | 46;XY, t(8;21) | ITD |
| 41 | 48 | M | M3 | 46;XY, t(15;17) | ITD |
| 44 | 62 | F | M3 | 46;XY, t(15;17) | ITD |
| 49 | 64 | F | M4 | 46;XY, inv(16) | ITD |
| 53 | 43 | F | M2 | 46;XY, t(8;21) | ITD |
| 58 | 49 | M | M3 | 46;XY, t(15;17) | ITD |
| 64 | 48 | M | M4 | 46;XY, inv(16) | Asp 835 Tyr |
| 69 | 47 | M | M4 | 46;XY, inv(16) | Asp 835 Tyr |
| 80 | 34 | M | M4 | 46;XY, inv(16) | Asp 835 Tyr |
| 83 | 39 | M | M2 | 46;XY, t(8;21) | Asp 835 Tyr |
| 91 | 37 | M | M2 | 46;XY, t(8;21) | Asp 835 Tyr |
| 96 | 38 | F | M6 | 46;XY | Asp 835 Tyr |
| 108 | 35 | F | M5 | 46;XY | Asp 835 Tyr |
| 116 | 31 | F | M1 | 46;XY | Asp 835 Tyr |
| 118 | 33 | F | M4 | 46;XY | Asp 835 Tyr |
| 121 | 25 | M | M2 | 46;XY, inv(16) | Asp 835 Tyr |
| 128 | 45 | F | M6 | 46;XY | Asp 835 Tyr |
2.3. Analysis of correlation with survival
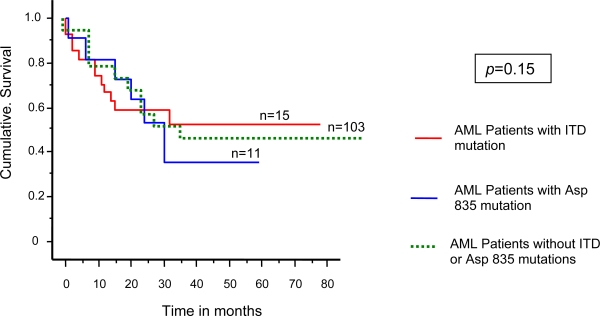
Survival analysis was calculated using Kaplan-Meier plot for comparison between Asp835Tyr and ITD AML patients. The survival curves were plotted for AML patients with Asp 835 mutation (n = 11) and ITD mutations (n = 15). The Mantel-Cox test demonstrated that the difference between the two groups of AML patients was not statistically significant (Figure 5).
Figure 5.
Kaplan-Meier cumulative survival analysis for AML patients with Asp 835 and ITD mutations and AML patients without mutations. Blue line indicates patients with Asp 835 mutation, red line indicates patients with ITD mutations and green line patients without flt3 mutations. The survival analysis showed no significance differences between the three groups (p = 0.15).
We undertook in this study the analysis of ITD and Asp 835 mutations of the FLT3 gene in Saudi AML patients in order to better understand the prevalence of these mutations in our cohort of cases. FLT3-ITD mutation is thought to cause the constitutive and ligand-independent activation of the receptor, but Fenski et al. [20] have shown that FLT3 oncogene is constitutively activated in 3/18 cases of AML patients and only 1/3 of those cases exhibited the FLT3-ITD mutation. It was therefore suggested that some other mechanisms are operational for the activation of the receptor, either because of mutations elsewhere in the gene or due to autocrine mechanisms. This prompted us to include in our screen exon 20 and identify mutations involving Asp 835. Previous studies indicated that Asp 835 highly conserved homologues, are probably playing a crucial role in the function of the activating loop of the JM region and kinase domain of class III RTKs [20–26]. The frequency of FLT3-ITD mutation identified in this study is much lower than reported for other ethnic populations which range between 20%–25% in Japanese [27], Chinese [28], Thai [29] or German [30] populations. It is interesting to find that all the detected cases of FLT3-ITD mutations exhibited cytogenetic aberrations, in particular t(15;17), t(8;21) and Inv(16). These chromosomal rearrangements are commonly found in adult AML cases as in our cohort inv(16) is the most common event at 26.3%, followed by the presence of t(15;17) translocation (17.8%). The t(8;21) translocation constituted only 8.5% of the cases in our cohort. The FLT3-ITD mutations were all detected in cases with cytogenetic translocations. Whether this reflects a case of global genomic instability or not is unknown. Screening of a larger cohort of samples may shed some light into the potential association between FLT3-ITD mutations and genomic instability.
The first aim of this study was to screen the FLT3 gene for previously reported mutations in AML using a sensitive and simple method to determine the frequency of the mutations. Efficiency and sensitivity were the main criteria to be considered in the selection of the method of mutation detection to be used in the analysis of the FLT3 gene. CSGE was the method of choice for screening the FLT3 gene because of its high sensitivity and simplicity as reviewed by Ganguly [31]. The technique has been used in different studies for the analysis of factor VIII gene in hemophilia A patients [32–33] and other genes including the von Willebrand factor (VWF) gene [34], factor IX [35]. For example, the sensitivity of CSGE in the detection of mutations was 100% in 21 hemophilia B patients [35] and 88% in patients with VWD [34]. Moreover, CSGE was selected as the method of choice to ensure all previously known FLT3 mutations can be detected.
3. Conclusions
In conclusion, we report mutations in the human FLT3 gene in a cohort of Saudi AML patients. These mutations are likely to lead to constitutive activation of the FLT3 receptor. The FLT3-ITD mutation rates reported in this study are lower than expected which would justify that future studies will need to screen the complete coding and regulatory sequence of the FLT3 gene to determine whether additional mutations are associated with the pathogenesis of myeloid malignancy.
4. Experimental Section
4.1. Patient DNA samples
Sample DNA was collected from 129 routinely-processed unstained bone marrow slides diagnosed as Acute myeloid leukemia (AML), which had been stored in a box at room temperature in an air-conditioned storage room for up to 20 years (from 1987 to 2007) in the archives of Hematology Laboratory at King Abdulaziz University Hospital. Genomic DNA was extracted (as optimized by Gari, et al. [36]) from the scraped material of each bone marrow slide using the Nucleon BACC1 DNA extraction kit (Nucleon Biosciences). Theses samples of genomic DNA were selected at presentation from 129 cases of AML (53 women, 76 men, and mean age 40.3 years, range 22–65). The cases were classified according to the FAB criteria [37] as M0 (n = 5), M1 (16), M2 (n = 38), M3 (n = 23), M4 (n = 34), M5 (n = 9) and M6 (n = 4). Sixty-eight patients had good risk and 61 had intermediate risk disease, as defined by standard cytogenetic analysis [38]; inv(16) (n = 34), t(15;17) (n = 23) and t(8;21) (n = 11).
4.2. Genomic DNA amplification
DNA amplification was performed by polymerase chain reaction (PCR). All exons, and intron/exon boundaries of the FLT3 gene involved in this study were amplified independently. The entire coding sequence and intron/exon boundaries corresponding to exons 14, 15 (ITD) and 20 (Asp835) of the FLT3 gene were amplified independently, using oligonucleotide primers as shown in Table 2.
Table 2.
Oligonucleotide primers used in PCR analysis.
| Primer sequences | Fragment size (bp) | ||
|---|---|---|---|
| F | 5′-TCTGTTTCATCGCTGAGTGAC-3′ | ||
| ITD | 396 | ||
| R | 5′-AGCCTTGAAACATGGCAAAC-3′ | ||
| F | 5′-CCAGGAACGTGCTTGTCA-3′ | ||
| Exon 20 | 352 | ||
| R | 5′-TCAAAAATGCACCACAGTGAG-3′ |
F: forward; R: reverse.
The PCR reactions contained the following: genomic DNA (500 ng), (NH4)2SO4 (16.6 mM), Tris HCL (pH 8.0, 67 mM), β-mercaptoethanol (10 mM), bovine serum albumin (BSA, 100 μg), each primer (300 ng), dNTPs (200 μM), MgCl2 (1.50 mM), and Taq DNA polymerase (1 U) in a final volume of 50 μL. Samples were initially denatured at 94°C for 5 minutes. DNA amplification was performed by 35 cycles of denaturation at 94°C for 1 minute, annealing at 55°C for 30 second and extension at 72 °C for 30 second. Five μL of each PCR products was loaded onto 5% polyacrylamide gel or agarose gel to ensure the amplification had occurred.
4.3. Mutation detection
Conformation sensitive gel electrophoresis (CSGE) was used to screen for mutations as described in [31]. Briefly, PCR products were denatured by heating to 95°C for 5 minutes and then incubated at 65°C for 30 minutes. These PCR products were resolved on 10% polyacrylamide gels; 99:1 ratio acrylamide (BDH):bis-acrolypiperazine (BAP; Fluka), 10% ethylene glycol (Sigma), 15% formamide (Sigma) and 0.5 × TTE buffer (1 × TTE = 89 mM Tris, 28.5 mM taurine, 0.2 mM EDTA). Samples displaying abnormal CSGE profiles compared to that obtained from a normal individual were directly sequenced using automated DNA sequencer (API 310 prizm).
Acknowledgments
The authors are grateful to Mr. A. Abdulbaqi at hematology laboratory for providing archival bone marrow slides of AML cases. This project is supported by a grant from Deanship of Scientific Research, King Abdulaziz University, Saudi Arabia.
References
- 1.Ullrich A, Schlessinger J. Signal transduction by receptors with tyrosine kinase activity. Cell. 1990;61:203–212. doi: 10.1016/0092-8674(90)90801-k. [DOI] [PubMed] [Google Scholar]
- 2.Matthews W, Jordan CT, Wiegand GW, Pardoll D, Lemischka IR. A receptor tyrosine kinase specific to hematopoietic stem and progenitor cell-enriched populations. Cell. 1991;65:1143–1152. doi: 10.1016/0092-8674(91)90010-v. [DOI] [PubMed] [Google Scholar]
- 3.Rosnet O, Schiff C, Pébusque MJ, Marchetto S, Tonnelle C, Toiron Y, Birg F, Birnbaum D. Human FLT3/FLK2 gene: cDNA cloning and expression in hematopoietic cells. Blood. 1993;82:1110–1119. [PubMed] [Google Scholar]
- 4.Yarden Y, Ullrich A. Growth factor receptor tyrosine kinase. Annu. Rev. Biochem. 1988;57:443–478. doi: 10.1146/annurev.bi.57.070188.002303. [DOI] [PubMed] [Google Scholar]
- 5.Abu-Duhier FM, Goodeve AC, Wilson GA, Care RS, Peake IR, Reilly JT. Identification of novel FLT-3 Asp835 mutations in adult acute myeloid leukaemia. Br. J. Haematol. 2001;113:983–988. doi: 10.1046/j.1365-2141.2001.02850.x. [DOI] [PubMed] [Google Scholar]
- 6.Birg E, Courcoul M, Rosnet O, Bardin F, Pebusque MJ, Marchetto S, Tabilio A, Mannoni P, Birnbaum D. Expression of the FMS/KIT-like gene FLT3 in human acute leukemias of the myeloid and lymphoid lineages. Blood. 1992;80:2584–2593. [PubMed] [Google Scholar]
- 7.Meierhoff G, Dehmel U, Gruss HJ, Rosnet O, Birnhaum D, Quentmeier H, Dirks W, Drexler HG. Expression of FLT3 receptor and FLT-3 ligand in human leukemia-lymphoma cell lines. Leukemia. 1995;9:1368–1372. [PubMed] [Google Scholar]
- 8.Drexler HG. Expression of FLT3 receptor and response of to FLT3 ligand by leukemic cells. Leukemia. 1996;10:588–599. [PubMed] [Google Scholar]
- 9.Ihle JN, Witthuhn BA, Quelle FW, Yamamoto K, Silvennoinen O. Signaling through the hematopoietic cytokine receptors. Annu. Rev. Immunol. 1995;13:369–398. doi: 10.1146/annurev.iy.13.040195.002101. [DOI] [PubMed] [Google Scholar]
- 10.Kelly LM, Kutok JL, Williams IR, Boulton CL, Amaral SM, Curley DP, Ley TJ, Gilliland DG.PML/RARalpha and FLT3-ITD induce an APL-like disease in a mouse model Proc. Natl. Acad. Sci.USA2002998283–8288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kelly LM, Liu Q, Kutok JL, Williams IR, Boulton CL, Gilliland DG. FLT3 internal tandem duplication mutations associated with human acute myeloid leukemias induce myeloproliferative disease in a murine bone marrow transplant model. Blood. 2002;99:310–318. doi: 10.1182/blood.v99.1.310. [DOI] [PubMed] [Google Scholar]
- 12.Zhao M, Kiyoi H, Yamamoto Y, Ito M, Towatari M, Omura S, Kitamura T, Ueda R, Saito H, Naoe T. In vivo treatment of mutant FLT3-transformed murine leukemia with a tyrosine kinase inhibitor. Leukemia. 2000;14:374–378. doi: 10.1038/sj.leu.2401680. [DOI] [PubMed] [Google Scholar]
- 13.Tse KF, Novelli E, Civin CI, Bohmer FD, Small D. Inhibition of FLT3-mediated transformation by use of a tyrosine kinase inhibitor. Leukemia. 2001;15:1001–1010. doi: 10.1038/sj.leu.2402199. [DOI] [PubMed] [Google Scholar]
- 14.Levis M, Tse KF, Smith BD, Garrett E, Small D. A FLT3 tyrosine kinase inhibitor is selectively cytotoxic to acute myeloid leukemia blasts harboring FLT3 internal tandem duplication mutations. Blood. 2001;98:885–887. doi: 10.1182/blood.v98.3.885. [DOI] [PubMed] [Google Scholar]
- 15.Weisberg E, Boulton C, Kelly LM, Manley P, Fabbro D, Meyer T, Gilliland DG, Griffin JD. Inhibition of mutant FLT3 receptors in leukemia cells by the small molecule tyrosine kinase inhibitor PKC412. Cancer Cell. 2002;1:433–443. doi: 10.1016/s1535-6108(02)00069-7. [DOI] [PubMed] [Google Scholar]
- 16.O’Farrell AM, Foran JM, Fiedler W, Serve H, Paquette RL, Cooper MA, Yuen HA, Louie SG, Kim H, Nicholas S, Heinrich MC, Berdel WE, Bello C, Jacobs M, Scigalla P, Manning WC, Kelsey S, Cherrington JM. An innovative phase I clinical study demonstrates inhibition of FLT3 phosphorylation by SU11248 in acute myeloid leukemia patients. Clin. Cancer Res. 2003;9:5465–5476. [PubMed] [Google Scholar]
- 17.Fiedler W, Mesters R, Tinnefeld H, Loges S, Staib P, Duhrsen U, Flasshove M, Ottmann OG, Jung W, Cavalli F, Kuse R, Thomalla J, Serve H, O’Farrell AM, Jacobs M, Brega NM, Scigalla P, Hossfeld DK, Berdel WE. A phase 2 clinical study of SU5416 in patients with refractory acute myeloid leukemia. Blood. 2003;102:2763–2767. doi: 10.1182/blood-2002-10-2998. [DOI] [PubMed] [Google Scholar]
- 18.DeAngelo DJ, Stone RM, Heaney ML, Nimer SD, Paquette RL, Klisovic RB, Caligiuri MA, Cooper MR, Lecerf JM, Karol MD, Sheng S, Holford N, Curtin PT, Druker BJ, Heinrich MC. Phase 1 clinical results with tandutinib (MLN518), a novel FLT3 antagonist, in patients with acute myelogenous leukemia or high-risk myelodysplastic syndrome: Safety, pharmacokinetics, and pharmacodynamics. Blood. 2006;108:3674–3681. doi: 10.1182/blood-2006-02-005702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stone RM, de Angelo J, Galinsky I, Estey E, Klimek V, Grandin W, Lebwohl D, Yap A, Cohen P, Fox E, Neuberg D, Clark J, Gilliland DG, Griffin JD. PKC 412 FLT3 inhibitor therapy in AML: Results of a phase II trial. Ann. Hematol. 2004;83:89–90. doi: 10.1007/s00277-004-0850-2. [DOI] [PubMed] [Google Scholar]
- 20.Fenski R, Flesch K, Serve S, Mizuki M, Oelmann E, Kratz A, Kienast J, Leo R, Schwartz S, Berdel WE, Serve H. Constitutive activation of FLT3 in acute myeloid leukaemia and its consequences for growth of 32D cells. Br. J. Haematol. 2000;108:322–330. doi: 10.1046/j.1365-2141.2000.01831.x. [DOI] [PubMed] [Google Scholar]
- 21.Kiyoi H, Towatari M, Yokota S, Hamaguchi M, Ohno R, Saito H, Naoe T. Internal tandem duplication of the FLT3 gene is a novel modality of elongation mutation which causes constitutive activation of the product. Leukemia. 1998;12:1333–1337. doi: 10.1038/sj.leu.2401130. [DOI] [PubMed] [Google Scholar]
- 22.Yamamoto Y, Kiyoi H, Nakano Y, Suzuki R, Kodera Y, Miyawaki S, Asou N, Kuriyama K, Yagasaki F, Shimazaki C, Akiyama H, Saito K, Nishimura M, Motoji T, Shinagawa K, Takeshita A, Saito H, Ueda R, Ohno R, Naoe T. Activating mutation of D835 within the activation loop of FLT3 in human hematologic malignancies. Blood. 2001;97:2434–2439. doi: 10.1182/blood.v97.8.2434. [DOI] [PubMed] [Google Scholar]
- 23.Xu F, Taki T, Yang HW, Hanada R, Hongo T, Ohnishi H, Kobayashi M, Bessho F, Yanagisawa M, Hayashi Y. Tandem duplication of the FLT3 gene is found in acute lymphoblastic leukaemia as well as acute myeloid leukaemia but not in myelodysplastic syndrome or juvenile chronic myelogenous leukaemia in children. Br. J. Haematol. 1999;105:155–162. [PubMed] [Google Scholar]
- 24.Abu D, Goodeve AC, Wilson GA, Gari MA, Peake IR, Rees DC, Vandenberghe EA, Winship PR, Reilly JT. FLT3 internal tandem duplication mutations in adult acute myeloid leukaemia define a high-risk group. Br. J. Haematol. 2000;111:190–195. doi: 10.1046/j.1365-2141.2000.02317.x. [DOI] [PubMed] [Google Scholar]
- 25.Horiike S, Yokota S, Nakao M, Iwai T, Sasai Y, Kaneko H, Taniwaki M, Kashima K, Fujii H, Abe T, Misawa S. Tandem duplications of the FLT3 receptor gene are associated with leukemic transformation of myelodysplasia. Leukemia. 1997;11:1442–1446. doi: 10.1038/sj.leu.2400770. [DOI] [PubMed] [Google Scholar]
- 26.Kiyoi H, Naoe T, Nakano Y, Yokota S, Minami S, Miyawaki S, Asou N, Kuriyama K, Jinnai I, Shimazaki C, Akiyama H, Saito K, Oh H, Motoji T, Omoto E, Saito H, Ohno R, Ueda R. Prognostic implication of FLT3 and N-RAS gene mutations in acute myeloid leukemia. Blood. 1999;93:3074–3080. [PubMed] [Google Scholar]
- 27.Yokota S, Kiyoi H, Nakao M, Iwai T, Misawa S, Okuda T, Sonoda Y, Abe T, Kahsima K, Matsuo Y, Naoe T. Internal tandem duplication of the FLT3 gene is preferentially seen in acute myeloid leukemia and myelodysplastic syndrome among various hematological malignancies. A study on a large series of patients and cell lines. Leukemia. 1997;11:1605–1609. doi: 10.1038/sj.leu.2400812. [DOI] [PubMed] [Google Scholar]
- 28.Wang L, Lin D, Zhang X, Chen S, Wang M, Wang J. Analysis of FLT3 internal tandem duplication and D835 mutations in Chinese acute leukemia patients. Leuk. Res. 2005;29:1393–1398. doi: 10.1016/j.leukres.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 29.Auewarakul CU, Sritana N, Limwongse C, Thongnoppakhun W, Yenchitsomanus PT. Mutations of the FLT3 gene in adult acute myeloid leukemia: determination of incidence and identification of a novel mutation in a Thai population. Cancer Genet. Cytogenet. 2005;162:127–134. doi: 10.1016/j.cancergencyto.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 30.Thiede C, Steudel C, Mohr B, Schaich M, Schäkel U, Platzbecker U, Wermke M, Bornhäuser M, Ritter M, Neubauer A, Ehninger G, Illmer T. Analysis of FLT3 activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood. 2002;99:4326–4335. doi: 10.1182/blood.v99.12.4326. [DOI] [PubMed] [Google Scholar]
- 31.Ganguly A. An update on conformation sensitive gel electrophoresis. Hum. Mutat. 2002;19:334–342. doi: 10.1002/humu.10059. [DOI] [PubMed] [Google Scholar]
- 32.Williams IJ, Abuzenadah A, Winship PR, Preston FE, Dolan G, Wright J, Peake IR, Goodeve AC. Precise carrier diagnosis in families with haemophilia A: Use of conformational sensitive gel electrophoresis for mutation screening and polymorphism analysis. Thromb. Haemost. 1998;79:723–726. [PubMed] [Google Scholar]
- 33.Goodeve AC, Williams I, Bray GL, Peake IR. Relationship between factor VIII mutation type and inhibitor development in a cohort of previously untreated patients treated with recombinant factor VIII (Recombinate). Recombinate PUP Study Group. Thromb. Haemost. 2000;83:844–848. [PubMed] [Google Scholar]
- 34.Hashemi Soteh M, Peake IR, Marsden L, Anson J, Batlle J, Meyer D, Fressinaud E, Mazurier C, Goudemand J, Eikenboom J, Goodeve A. MCMDM-1VWD Study Group. Mutational analysis of the von Willebrand factor gene in type 1 von Willebrand disease using conformation sensitive gel electrophoresis: a comparison of fluorescent and manual techniques. Haematologica. 2007;92:550–553. doi: 10.3324/haematol.10606. [DOI] [PubMed] [Google Scholar]
- 35.Hinks JL, Winship PR, Makris M, Preston FE, Peake IR, Goodeve AC. Rapid method for haemophilia B mutation detection using conformation sensitive gel electrophoresis. Br. J. Haematol. 1999;104:915–918. doi: 10.1046/j.1365-2141.1999.01274.x. [DOI] [PubMed] [Google Scholar]
- 36.Gari MA, Abuzenadah AM, Chaudhary AG, Al-Qahtani MH, Al-Says FM, Dmanhouri G. Pilot study of DNA extraction from archival unstained bone marrow slides: comparison of three rapid methods. Af J. Biotech. 2006;5:532–535. [Google Scholar]
- 37.Bennett JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, Sultan C. Proposal for the classification of the acute leukaemias. French American British (FAB) cooperative group. Br. J. Haematol. 1976;33:451–458. doi: 10.1111/j.1365-2141.1976.tb03563.x. [DOI] [PubMed] [Google Scholar]
- 38.Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, Rees J, Hann J, Hann I, Stevens R, Burnett A, Goldstone A. The importance of diagnostic cytogenetics on outcome in AML: Analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical research Council Adult and Children's Leukaemia Working Parties. Blood. 1998;92:2322–2333. [PubMed] [Google Scholar]