Abstract
The rabbit model is commonly used to study carpal tunnel syndrome (CTS). It has been proposed that the subsynovial connective tissue (SSCT) in the carpal tunnel may play a role in the etiology of CTS, but the material properties of the rabbit SSCT are unknown. The purpose of this study was to develop a method to measure the shear properties of the rabbit SSCT. In six rabbit cadaver forepaws, the excursion of the third digit flexor digitorum superficialis (FDS) and load to failure of the SSCT were measured in a custom device. The mean excursion to full flexion in this model was 7.08 mm (SD 0.77). The mean shearing force at full flexion was 317 mN (SD 166). At full flexion percentage of maximum shear force in the SSCT was 54.5% (SD 19.4). The mean energy absorbed at full flexion was 0.29 mJ (SD 0.31). The mean excursion needed to reach 5% of the maximum shear force was 3.04 mm (SD 0.99). The testing model presented in this study demonstrates structural parameters to evaluate the shear properties of the SSCT in a rabbit model. The data presented could be used for estimating sample sizes in a more comprehensive study of the effect of CTS on the SSCT properties.
Keywords: Carpal Tunnel, Subsynovial Connective Tissue, Biomechanics, Rabbit, Flexor Tendon
Introduction
The subsynovial connective tissue (SSCT) in the carpal tunnel region consists of multiple thin layers of collagenous fibers, in which blood and lymphatic vessels are richly represented (Ettema et al., 2004; Guimberteau, 2001; Oh et al., 2005). The SSCT plays an important role as a gliding unit to diminish friction and protect the vascular system within the SSCT. Recently, the pathological changes of the SSCT in carpal tunnel syndrome (CTS) patients have been described (Lluch, 1992; Ettema et al., 2006a; Oh et al., 2006; Sud et al., 2002), suggesting that idiopathic CTS may be caused primarily by an injury to the SSCT, with secondary nerve involvement, rather than by direct damage of the nerve itself.
One such mechanism could be shearing of the SSCT, due to excessive differential tendon motion. There are many reports describing highly repetitive work as one of the risk factors for idiopathic CTS (Atcheson et al., 1998; Chin and Jones, 2002; Finkel, 1985). In addition to the tendon excursion caused by digit motion, the myofascial force transmission would exacerbate the shearing to the SSCT (Huijing, 2003; Yucesoy et al., 2003). Excessive shearing motion of adjacent tendons could rupture the fine microvascular collagen fibers. The thickening of the fibers, noted by Ettema et al (Ettema et al., 2004; Ettema et al., 2006a) could be the result of healing of such an injury, and could affect the material properties of the SSCT in a way likely to promote elevated carpal tunnel pressure, the final common pathway to the development of carpal tunnel syndrome. A better understanding of the SSCT mechanical properties under shear loading would help us understand how alterations to these properties might affect carpal tunnel pressure.
Recently, the carpal tunnel anatomy and subsynovial connective tissue of animals were also examined by light and scanning microscopy and compared to the relevant human anatomy and ultrastructure (Ettema et al., 2006b). The human and rabbit anatomy had very similar organization of the SSCT and content of the carpal canal. The purpose of this study was to present a method to measure the mechanical properties of the rabbit SSCT in response to shear stress.
Materials and Methods
A total of 6 rabbit cadavers with a mean weight of 4.6 kg (range, 3.6 to 5.4 kg) were used. The animals had been euthanized in the course of other IACUC approved studies. The forefeet, with intact carpal tunnels, including the flexor digitorum superficialis (FDS) tendons and surrounding SSCT, were obtained immediately after sacrifice. FDS tendons were exposed at the antebrachial level with the carpal tunnel intact. The third FDS tendon was divided 5 mm proximal to the proximal edge of the flexor retinaculum, and the proximal end of the third FDS tendon was sutured with 2-0 Vicryl. The Vicryl suture was used to connect the tendon to a load cell. On the distal side, the third FDS tendon was exposed 5 mm distal to the carpal tunnel. The specimen was held on a custom specimen holder (Figure 1). The wrist was fixed in neutral flexion/extension with a Kirschner wire. The second and forth digits were also fixed on the specimen holder, while the third digit was left free. The specimen holder with the specimen was mounted on a custom-made micro-tester for mechanical evaluation (Figure 1).
Figure 1.
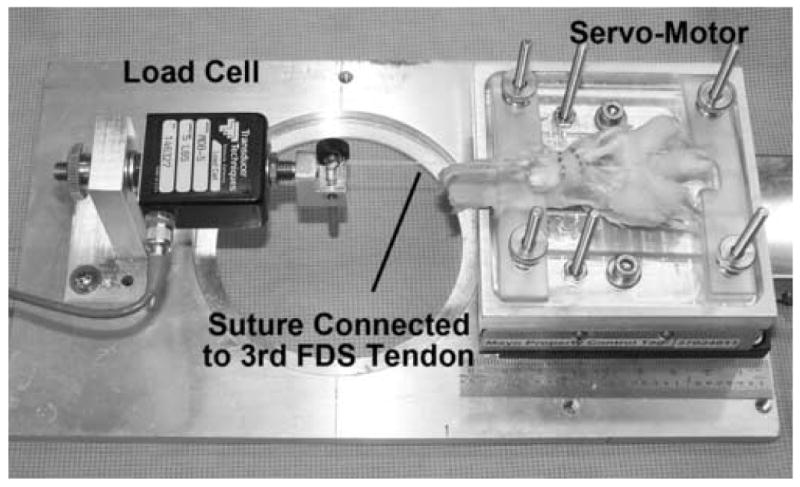
Experimental testing setup. The rabbit paw was clamped to a servo-motor. The third FDS tendon was connected to a fixed load cell. The motor moved the paw distally causing proximal tendon excursion of the third FDS tendon. The second and fourth digits were not allowed to flex.
The testing device consisted of a linear servo motor (model MX 80, Parker Hannifin Corp., Irwin, PA, USA) and a load cell (model MDB-5, Transducer Techniques, Temecula, CA, USA), accurate to 0.01 N. Throughout testing, the specimen was kept moist by spraying phosphate buffered 0.9% saline solution.
During testing the tensile force of the intact third digit FDS tendon was first measured by moving the FDS tendon, under displacement control using the linear servo motor at a rate of 0.5 mm/s, until maximum proximal interphalangeal joint flexion was achieved. The rate was selected so the measurement would characterize the elastic tissue response and minimize the influence of viscoelastic properties. Tensile force and displacement were recorded simultaneously, at a rate of 10 Hz and five cycles of motion were collected. This model is referred to as the Control Model. After this measurement, the third finger FDS tendon was cut distal to the carpal tunnel and the mechanical test was repeated, under displacement control using the linear servo motor at a rate of 0.5 mm/s, until the third finger FDS tendon was completely pulled through the carpal tunnel. The ultimate tensile force reflects the shearing strength of the SSCT connected to the third FDS tendon. This model is referred to as the Cut and Pullout Model.
The initial test was used to calculate the normal tendon excursion to full finger flexion. From the second test we evaluated the maximum force, the force at the excursion needed to produce full flexion in the baseline test, the percent of the maximum force at full flexion excursion, the energy absorbed at full flexion and the excursion at which the SSCT reached 5% of the maximum force (Figure 2). Although we did not confirm in this study, it is presumed that prior to this 5% threshold, the SSCT fibers have not all been loaded and thus would represent a point of loading with no tissue damage. For all parameters the mean and standard deviation were reported.
Figure 2.
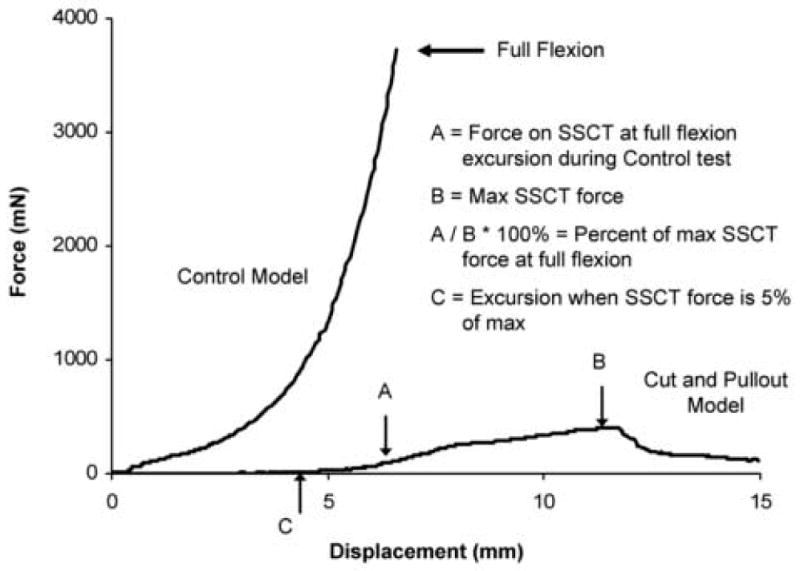
Typical force-excursion curves for Control and Cut and Pullout Models. Point A is the force on the SSCT at full flexion excursion during the Control test. Point B is the maximum SSCT force. A/B*100% is the percent of maximum SSCT force at full flexion. Point C is the excursion when SSCT force is 5% of the maximum.
Results
Typical force-excursion curves for the Control and the Cut and Pullout Models are shown in Figure 2. For the six specimens tested in this study, the mean excursion to full flexion in this model was 7.08 mm (SD 0.77). The mean force at full flexion was 317 mN (SD 166). The percent maximum force at full flexion was 54.5% (SD 19.4). The mean energy absorbed at full flexion was 0.29 mJ (SD 0.31). The mean excursion needed to reach 5% of the maximum force was 3.04 mm (SD 0.99).
Discussion
In this study, we have described a method to measure the shear properties of the rabbit SSCT attached to the third FDS tendon. The testing mode mimics the force to which the SSCT is exposed clinically. The relevance of the data is for use of the rabbit model in studying CTS as done previously (Diao et al., 2005), but with the goal of assessing the role of the SSCT in CTS etiology and pathogenesis.
In this model we used the FDS tendons as these are the ones closest to the median nerve, the most independent anatomically, and also the tendons about which there are known changes in the SSCT in human cases of CTS (Ettema et al., 2004; Ettema et al., 2006a). The FDS tendon excursion during full flexion is important as a measure of the physiological limit of motion to which the intact FDS and its SSCT can be exposed. However, clinical manifestation of CTS commonly follows repetitive motion activities. Therefore, in addition to the quasi-static testing performed in this study, studying the dynamic fatigue properties of the SSCT may yield insight into the safe threshold levels of stress during repetitive activity. It is hypothesized that damage to the SSCT may damage the fine microvascular network and thus, intensity and duration of the loading may both be factors.
The SSCT force at the point of third FDS tendon excursion corresponding to maximum proximal interphalangeal joint flexion is a reflection of the maximum loading borne by the normal SSCT when one digit is flexed and the two adjacent ones are fully extended. This parameter may be important in acute injury models of CTS, as well as in looking at changes over time in models of chronic CTS. The percent maximum force at full flexion represents how close the SSCT is to its ultimate breaking strength at that point. It is recognized that in the presented testing mode, the force to break the SSCT may be affected by factors other then the intrinsic SSCT material properties. For example, inflammation of the carpal tunnel contents may increase the gliding resistance and impede the tendon excursion, thus requiring a higher force to pull the tendon out of the carpal tunnel. In such a scenario, an additional test could be performed, after the tendon had been pulled out of the carpal tunnel, to measure the gliding resistance of the tendon without the attached SSCT.
The energy absorbed at full flexion is a reflection of the work expended to move the SSCT to that limit; this may be an important factor, for example, in repetitive motion models of CTS. The excursion needed to reach 5% of the maximum force might be useful in establishing some sort of “safe harbor”, again in chronic and repetitive models of CTS. Both of these measurements will be studied in the future to assess the tolerance of the SSCT tissue under various loading scenarios in a rabbit model of progressive SSCT fibrosis.
In summary, we have described parameters for measuring SSCT material properties in the rabbit model. We believe that these data will be useful to help design future studies of CTS pathology in the rabbit model.
Acknowledgments
Funding for this study was provided by the NIH (NIAMS AR49823), and the Mayo Foundation. The study funding sponsors were not involved in the study design, collection, analysis or interpretation of the data, nor were they included in the decision to submit this work for publication.
Footnotes
Conflict of Interest Statement: The authors have no conflicts of interest regarding any of the material in the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Atcheson SG, Ward JR, Lowe W. Concurrent medical disease in work-related carpal tunnel syndrome. Archives of Internal Medicine. 1998;158:1506–1512. doi: 10.1001/archinte.158.14.1506. [DOI] [PubMed] [Google Scholar]
- Chin DH, Jones NF. Repetitive motion hand disorders. Journal of the California Dental Association. 2002;30:149–160. [PubMed] [Google Scholar]
- Diao E, Shao F, Liebenberg E, Rempel D, Lotz JC. Carpal tunnel pressure alters median nerve function in a dose-dependent manner: a rabbit model for carpal tunnel syndrome. Journal of Orthopaedic Research. 2005;23:218–223. doi: 10.1016/j.orthres.2004.05.014. [DOI] [PubMed] [Google Scholar]
- Ettema AM, Amadio PC, Zhao C, Wold LE, An KN. A histological and immunohistochemical study of the subsynovial connective tissue in idiopathic carpal tunnel syndrome. Journal of Bone and Joint Surgery [Am] 2004;86:1458–1466. doi: 10.2106/00004623-200407000-00014. [DOI] [PubMed] [Google Scholar]
- Ettema AM, Amadio PC, Zhao C, Wold LE, O'Byrne MM, Moran SL, An KN. Changes in the functional structure of the tenosynovium in idiopathic carpal tunnel syndrome: a scanning electron microscope study. Plastic and Reconstructive Surgery. 2006a;118:1413–1422. doi: 10.1097/01.prs.0000239593.55293.c7. [DOI] [PubMed] [Google Scholar]
- Ettema AM, Zhao C, An KN, Amadio PC. Comparative anatomy of the subsynovial connective tissue in the carpal tunnel of the rat, rabbit, dog, baboon, and human. Hand. 2006b;1:78–84. doi: 10.1007/s11552-006-9009-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkel ML. The effects of repeated mechanical trauma in the meat industry. American Journal of Industrial Medicine. 1985;8:375–379. doi: 10.1002/ajim.4700080418. [DOI] [PubMed] [Google Scholar]
- Guimberteau J. New Ideas in Hand and Flexor Tendon Surgery. Institut Aquitain de la Main; Bordeaux: 2001. The sliding system. [Google Scholar]
- Huijing PA. Muscular force transmission necessitates a multilevel integrative approach to the analysis of function of skeletal muscle. Exercise & Sport Sciences Reviews. 2003;31:167–175. doi: 10.1097/00003677-200310000-00003. [DOI] [PubMed] [Google Scholar]
- Lluch AL. Thickening of the synovium of the digital flexor tendons: cause or consequence of the carpal tunnel syndrome? Journal of Hand Surgery [Br] 1992;17:209–212. doi: 10.1016/0266-7681(92)90091-f. [DOI] [PubMed] [Google Scholar]
- Oh J, Zhao C, Amadio PC, An KN, Zobitz ME, Wold LE. Immunolocalization of collagen types in the subsynovial connective tissue within the carpal tunnel in humans. Journal of Orthopaedic Research. 2005;23:1226–1231. doi: 10.1016/j.orthres.2005.02.009. [DOI] [PubMed] [Google Scholar]
- Oh J, Zhao C, Zobitz ME, Wold LE, An KN, Amadio PC. Morphological changes of collagen fibrils in the subsynovial connective tissue in carpal tunnel syndrome. Journal of Bone and Joint Surgery [Am] 2006;86:824–831. doi: 10.2106/JBJS.E.00377. [DOI] [PubMed] [Google Scholar]
- Sud V, Tucci MA, Freeland AE, Smith WT. Absorptive properties of synovium harvested from the carpal tunnel. Microsurgery. 2002;22:316–319. doi: 10.1002/micr.10051. [DOI] [PubMed] [Google Scholar]
- Yucesoy CA, Koopman BH, Baan GC, Grootenboer HJ, Huijing PA. Effects of inter- and extramuscular myofascial force transmission on adjacent synergistic muscles: Assessment by experiments and finite-element modeling. Journal of Biomechanics. 2003;36:1797–1811. doi: 10.1016/s0021-9290(03)00230-6. [DOI] [PubMed] [Google Scholar]


