Abstract
Background & Objective
The authors examined college students’ perceptions regarding emergency contraception (EC) provision in light of the then-pending U.S. Food and Drug Administration decision regarding over-the-counter (OTC) status of EC.
Methods
We randomly sampled 7,000 male and female students who were enrolled full-time at the University of Michigan during the Winter 2006 semester. A total of 1,585 (22.6%) students responded to our web-based survey, and were included in these descriptive analyses.
Results
Nearly all (94%) respondents knew of EC. When asked whether EC should be made available OTC, 60% of respondents agreed, 23% disagreed, and 17% were unsure. If EC were to be made available OTC, 34% of respondents indicated that they (or their partner) would purchase EC in advance of need while 44% stated that they would purchase it only after unprotected sexual intercourse or contraceptive failure. Advance discussion and provision of EC is underutilized. Only 10% of all female respondents indicated that their current health care provider had spoken to them about EC in a routine health visit and just 5% of female respondents were offered a supply of EC in advance of need.
Conclusion
Continued efforts are needed to ensure timely access to EC in this population.
Keywords: contraception, postcoital, students, college, pregnancy, unplanned
Introduction
In the United States, nearly half of all pregnancies are unplanned, leading to 3.1 million unintended pregnancies and 1.3 million abortions annually.1-2 The highest rates of unintended pregnancy occur in college-age women, with 60% of pregnancies among 20-24 year olds being unintended.1 The percentage of unintended pregnancy is even higher among 18-19 year old women (79%).1
Emergency contraception (EC) is a safe and effective postcoital contraceptive method that can reduce the risk of an unintended pregnancy after unprotected sexual intercourse or contraceptive failure by at least 75% to 89% if taken within 72 hours of sexual intercourse.3-5 Recent research suggests that combined EC pills are moderately effective even if started between the third and fifth day (up to 120 hours) after unprotected sexual intercourse or contraceptive failure, with effectiveness rates ranging from 72% to 87% in one study.6-7 It may operate by inhibiting ovulation or preventing the implantation of a fertilized egg; however, it does not interfere with an established pregnancy.8 Plan B®, the only Food and Drug Administration (FDA)-approved product dedicated for EC, has been available only by prescription since 1999. Due to the limited time frame for taking EC treatment, there have been numerous efforts to expand access to EC in recent years. Such endeavors have included (i) over 70 organizations signing a Citizen’s Petition, submitted to the FDA in 2001, that EC become available over-the-counter (OTC) 9; (ii) the Women’s Capital Corporation submitting a Supplemental New Drug Application to the FDA in 2003 to change the status of Plan B® from prescription-only to OTC status 10; (iii) Planned Parenthood Federation of America encouraging its affiliates to provide prescriptions for EC over the telephone and in advance of need; and (iv) selected states allowing EC to be provided directly by pharmacists through collaborative drug therapy agreements.11
Efforts to expand EC access from prescription-only to OTC have been under consideration since 2003.12 Barr Pharmaceutical’s (formerly Women’s Capital Corporation) Supplemental New Drug Application for Plan B® was initially denied in May 2004, despite FDA advisory committee approval, amidst FDA safety concerns for adolescents under 17 years of age.13-14 A revised application, submitted in June 2004, proposed limiting OTC access to Plan B® to women 17 years of age and older. Two years later, the FDA approved OTC access to Plan B® on August 23, 2006 for adults aged 18 and older.15 It remains prescription-only for minors.
As there is a dearth of published information about individuals’ opinions regarding advance provision and OTC access to EC, a study exploring such avenues among an at-risk population prior to the FDA decision was both timely and appropriate. In doing so, this research built on the recent work by Sawyer and Thompson (2003) and Corbett and colleagues (2006), which assessed EC knowledge of university students.16-17 The purpose of this study was to assess college students’ perceptions about EC provision and in particular, their knowledge of and opinions regarding OTC access, including whether OTC availability of EC might change their personal birth control practices.
Materials and Methods
The University of Michigan Medical School’s Institutional Review Board approved this study. A waiver of documentation of informed consent was granted by the Institutional Review Board, and text regarding the consent process was included in the initial email to students. A random sample of 7,000 students (both undergraduate and graduate level; 20% of all students) enrolled full-time at the University of Michigan during the Winter 2006 semester (January-April 2006) was drawn by the University’s Office of the Registrar, who sent an email on our behalf to invite students to participate in a web-based survey through SurveyMonkey (http://www.surveymonkey.com) in April 2006. A reminder email was sent to all 7,000 students one week later. No financial incentive was offered. We analyzed data from 1,585 college students who completed the survey within a 30-day period (response rate = 22.6%). The survey system was programmed to only allow one response per person.
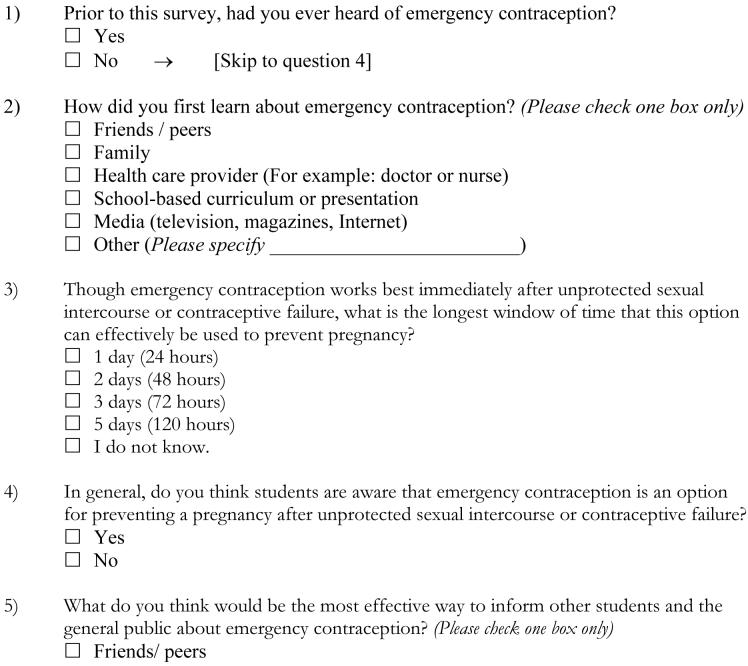
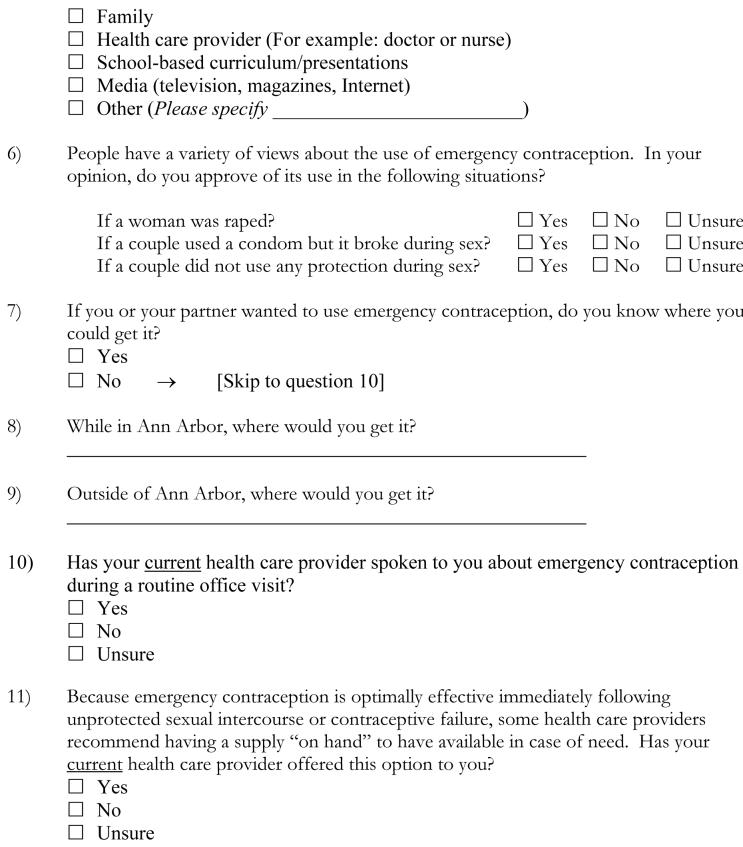
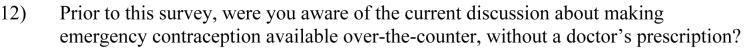
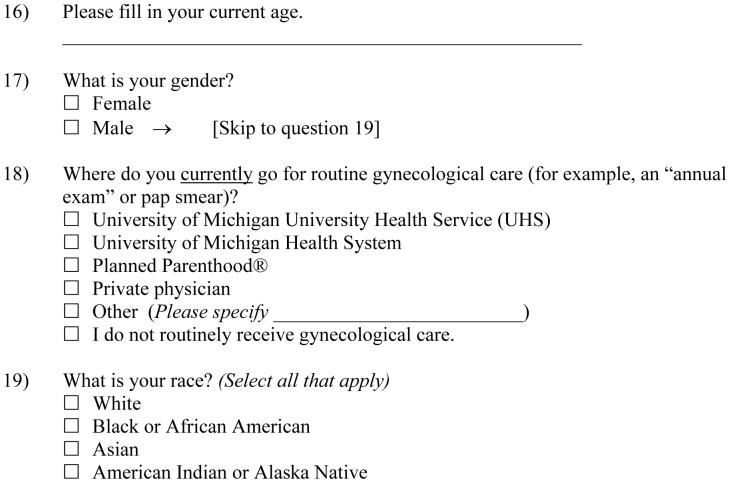
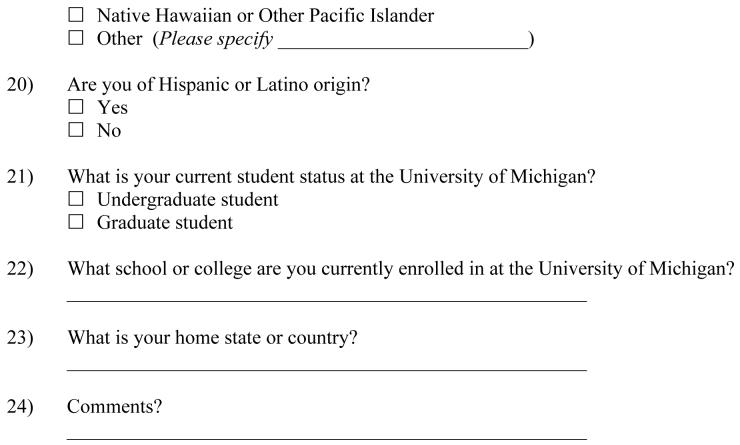
The survey instrument included questions about the respondents’ knowledge of and beliefs regarding EC provision. It was estimated to take 5-10 minutes to complete. Background information about EC, such as what it was, how it worked, and time frame for taking it was provided to all respondents prior to the first question. Next, respondents were asked to complete 11 multiple choice questions about their knowledge of and access to EC. Specific items asked about how they first learned of EC, whether they felt it should be used in cases of rape, contraceptive failure, or unprotected sexual intercourse, respectively, and advance provision. Questions on how the respondents first learned about EC and in what cases EC should be used were adapted from a 2003 Kaiser Family Foundation (KFF) Survey.18 Then respondents were provided with information about the current status of EC provision in Michigan and the potential for OTC access. Four multiple choice questions asked respondents about their awareness of the debate about OTC access, whether they believed that it should be available OTC, and whether OTC availability of EC might change their personal birth control practices. For female respondents, we also inquired about their current interaction with the health care system and whether they received information and/or a supply of EC in advance of need as part of these visits. The survey concluded with a series of questions to ascertain demographic information about the study population (e.g., age, gender, race and Hispanic origin classification, undergraduate/graduate status). The survey instrument was pilot tested among a small convenience sample of students and family planning providers, who provided suggestions for refining the instrument that were incorporated into the final version. A copy of the survey instrument is provided in the Appendix. No personal identifying information was collected; thus, individual responses were anonymous.
Frequencies were calculated for all items, and comparisons were made between male and female respondents and by age (17-22 years vs. 23-51 years) about their attitudes towards EC provision. Chi-square tests and student t-tests were performed where appropriate to test for statistical significance (p < 0.05). Statistical Analysis Software (SAS) Version 9.1 (SAS Institute Inc., Cary, NC) was used for all analyses.
Results
Table 1 describes the characteristics of our study population. The average age of our respondents was 22.5 years. Sixty-six percent of respondents were female and 60% were undergraduates. The race and Hispanic origin composition of our study population was representative of the broader University of Michigan student population.
Table 1.
Characteristics of study population (N=1585)
| N | % | |
|---|---|---|
| Age | ||
| Mean ± SD | 22.5 ± 4.3 | |
| 17-22 | 947 | 59.7 |
| 23-51 | 532 | 33.6 |
| Missing | 106 | 6.7 |
| Sex | ||
| Female | 1045 | 65.9 |
| Male | 451 | 28.5 |
| Missing | 89 | 5.6 |
| Student Status | ||
| Undergraduate | 957 | 60.4 |
| Graduate | 531 | 33.5 |
| Missing | 97 | 6.1 |
| Race * | ||
| White | 1144 | 72.2 |
| Black / African American | 66 | 4.2 |
| Asian | 168 | 10.6 |
| American Indian / Alaska Native | 14 | 0.9 |
| Native Hawaiian / Other Pacific Islander | 8 | 0.5 |
| Other | 76 | 4.8 |
| Missing | 109 | 6.9 |
| Hispanic Origin | ||
| Yes | 59 | 3.7 |
| No | 1413 | 89.2 |
| Missing | 113 | 7.1 |
Percentages add to more than 100% because participants could select more than one category.
Nearly all respondents (94%) said that they had heard of EC prior to receiving the survey. However, 12% indicated that they did not know the longest time window for effectiveness and 45% of respondents stated that EC must be taken within 3 days or 72 hours after unprotected sexual intercourse or contraceptive failure. Only 5% responded that EC must be taken within 5 days or 120 hours (shown in research studies 6-7, 19 to be the longest time window that EC can be effective). Respondents first learned of EC from a variety of sources, including the media (43%), friends or peers (22%), and school-based curriculum (18%). When students were asked what would be the most effective way to inform their peers and the public about EC, a similar response was given, with 14% of respondents also indicating health care providers as a source of information. Nearly three-fourths of respondents believed that students were aware of EC as an option.
Table 2 describes the attitudes and beliefs of the respondents regarding when to use EC, overall and by sex and age. Ninety-three percent of respondents approved of the use of EC in the case a woman was raped. Eighty-six percent approved of its use in the instance of contraceptive failure, but only 68% approved of its use after unprotected sexual intercourse. Female and older students were more likely to approve of the use of EC in each instance, compared to male and younger students, respectively. Results stratified by the respondent’s sex were statistically significant for questions regarding the instance of rape and contraceptive failure, while those stratified by the respondent’s age were statistically significant for questions regarding the instance of contraceptive failure and unprotected sexual intercourse and marginally significant in the instance of rape.
Table 2.
Attitudes and beliefs of university students regarding emergency contraception
| Topic | By Sex |
By Age |
|||||
|---|---|---|---|---|---|---|---|
| Overall (n=1585) | Female (n=1045) | Male (n=451) | P-Value | 17-22 (n=947) | 23-51 (n=532) | P-Value | |
| Do you approve of the use of EC if a woman was raped? | 0.02 | 0.07 | |||||
| Yes | 93.2 | 94.4 | 90.5 | 92.5 | 94.9 | ||
| No | 4.1 | 3.2 | 6.2 | 4.4 | 3.2 | ||
| Unsure | 2.7 | 2.4 | 3.3 | 3.1 | 1.9 | ||
| Do you approve of the use of EC if a couple used a condom, but it broke during sex? | 0.02 | 0.01 | |||||
| Yes | 85.8 | 87.9 | 81.6 | 84.9 | 88.7 | ||
| No | 9.3 | 7.2 | 13.5 | 9.1 | 8.3 | ||
| Unsure | 4.9 | 4.9 | 4.9 | 6.0 | 3.0 | ||
| Do you approve of the use of EC if a couple did not use any protection during sex? | 0.32 | < 0.01 | |||||
| Yes | 68.3 | 70.0 | 64.7 | 66.0 | 73.6 | ||
| No | 20.2 | 17.9 | 24.7 | 21.5 | 16.4 | ||
| Unsure | 11.5 | 12.1 | 10.6 | 12.5 | 10.0 | ||
Table 3 summarizes the knowledge and opinions of college students regarding the federal government’s plans to make EC available OTC. Only 57% of respondents indicated that they were aware of this policy debate prior to receiving the survey. A significantly higher proportion of women and older students were aware of the debate, in comparison to men and younger students, respectively. More than half of respondents (60%) believed that EC should be available OTC. However, nearly one-quarter (23%) disagreed and 17% were unsure. When asked what they would do if EC was available OTC, 33% of respondents indicated that they would purchase a supply in advance of need and 44% responded that they would purchase a supply after unprotected sex. Nineteen percent of respondents stated that they would not purchase EC.
Table 3.
Knowledge and attitudes of university students regarding over-the-counter access to emergency contraception
| Topic | By Sex |
By Age |
|||||
|---|---|---|---|---|---|---|---|
| Overall (n=1585) | Female (n=1045) | Male (n=451) | P-Value | 17-22 (n=947) | 23-51 (n=532) | P-Value | |
| Were you aware of the over-the-counter debate? | < 0.01 | < 0.01 | |||||
| Yes | 57.5 | 61.6 | 48.2 | 54.1 | 63.7 | ||
| No | 42.5 | 38.4 | 51.8 | 45.9 | 36.3 | ||
| Do you think that emergency contraception should be available over-the-counter? | 0.45 | 0.08 | |||||
| Yes | 60.2 | 59.7 | 61.6 | 58.5 | 63.3 | ||
| No | 22.8 | 22.9 | 22.4 | 23.4 | 21.1 | ||
| Unsure | 17.0 | 17.4 | 16.0 | 18.1 | 15.6 | ||
| If emergency contraception were available over-the-counter, which of the following would you do? | 0.30 | 0.08 | |||||
| Purchase in advance of need | 33.6 | 33.4 | 34.2 | 35.5 | 30.0 | ||
| Purchase after unprotected sex | 44.2 | 46.1 | 39.6 | 43.8 | 45.8 | ||
| Would not purchase | 18.7 | 16.9 | 22.8 | 16.7 | 21.6 | ||
| Other | 3.5 | 3.6 | 3.4 | 4.0 | 2.6 | ||
Overall, only 10% of all female respondents indicated that their current health care provider had spoken to them about EC in a routine visit and just 5% of female respondents were offered a supply in advance of need. Nearly one in four female respondents indicated that they do not currently receive routine gynecological care. Among the 346 female respondents who responded that they would purchase a supply in advance of need if EC were to become available OTC, only 15% indicated that their health care provider had spoken to them about it during a routine office visit and approximately 7% were offered a supply in advance of need.
Discussion
While EC is now available OTC to individuals aged 18 years and older, there remains a critical need for continued health education about EC. Previous studies on EC knowledge and utilization show that while the general public and university students have heard of EC, they generally lack sufficient knowledge about what it is, how it works, and how to access it.16-18, 20 Our findings are comparable to this body of research. While OTC availability of EC may allow for increased access, its success is linked to the dissemination of accurate information about EC via trusted informational sources, such as through family, friends, health care providers, and the media. One challenge in educating college students and other young adults about EC is the identified lack of information about EC shared by health care providers with this population. The challenge to health care providers is to increase awareness and utilization of such preventive services.21-22 While increasing the number of women who take postcoital contraception is not likely to reduce risky sexual behaviors, it may reduce the number of unwanted pregnancies and abortions that occur each year in the United States.
Our findings on awareness and knowledge about EC are comparable to those of other studies that included a college student population.16-17 Sawyer and Thompson (2003) reported that nearly 86% of their undergraduate respondents stated that they had heard about EC, but the majority indicated that their perceived knowledge was low.16 Similarly, Corbett and colleagues (2006) indicated that 96% of respondents (college students of ages between 18 and 21 years) stated that they had heard about EC, but only 18% had previously discussed EC with their health care provider.17
In contrast, our findings regarding gender differences in EC decision-making were different from those presented by Corbett and colleagues, who reported that 67% of their female respondents and only 46% of their male respondents stated that they would be likely to use (or recommend) EC in the event of contraceptive failure. 17 In our study, while female respondents (88%) were more likely than male respondents (82%) to approve of the use of EC in the event of contraceptive failure, overall 86% of respondents approved of its use in this instance.
There were some limitations to this study that may limit the validity of our findings. The results of our study are dependent on the accuracy of our participants’ responses. Our study population consisted of a random sample of students that were enrolled full-time at the University of Michigan. Thus, our findings may not reflect the opinions of all U.S. college students. Our survey response rate (22.6%) was lower than anticipated. As information on non-responders was not available to the research team, we can only speculate as to why some students chose not to respond to the survey. Factors such as the timing of survey administration (a few weeks prior to the end of the semester), the subject matter of the survey, and/or the lack of an incentive may have contributed to the response rate we achieved.
Conclusion
Advance discussion and provision of EC is underutilized. Because of the higher risk for an unplanned pregnancy with unprotected sexual intercourse or contraceptive failure among college women, continued efforts are needed to enhance timely access to EC in this population. Findings from this study suggest that there are multiple avenues from which to educate young adults about EC. Health care providers and health educators would be invaluable resources for informing campus communities about EC and its OTC availability and for reinforcing ongoing health communication campaigns in the popular press.
Acknowledgements
Funding Sources: This study was supported by a small grant from the Institute for Research on Women and Gender at the University of Michigan. Dr. Vahratian was supported by the Building Interdisciplinary Research Careers in Women’s Health (BIRCWH) program, National Institutes of Health (1 K12 HD01438). Dr. Xu was partly supported by a National Institutes of Health Roadmap Initiative Grant (1 P20 RR020682-01). The authors thank Dr. Susan Ernst and Annie-Laurie McRee for their feedback on the survey design.
Appendix. Web-Based Survey Instrument
Section I- Knowledge & Access
There are several methods of contraception (birth control) currently available, such as birth control pills, condoms, diaphragms, and Depo-Provera®. In some instances, a couple may need a method of contraception after unprotected sexual intercourse or in cases of contraceptive failure (for example: if a condom breaks). Emergency contraception (sometimes called the “morning after pill” or Plan B®) is one such contraceptive option, and is thought to prevent a pregnancy by delivering hormones that delay ovulation, inhibit fertilization, and/or change the endometrial lining of the uterus. Emergency contraception does not abort an established pregnancy.
The following questions ask you about your knowledge and opinions about pills used for emergency contraception.
Section II- Over-the-Counter Access
In Michigan, emergency contraception is only available by doctor’s prescription (although in a few other states, women can obtain emergency contraception from pharmacists without a doctor’s prescription). Recently, legal action at the federal level has been sought to make emergency contraception available over-the-counter (like Advil® or Tylenol®).
Section III- Demographics
Thank you for your participation in this survey! All responses will be kept confidential.
References
- 1.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 2.Raine TR, Harper CC, Rocca CH, Fischer R, Padian N, Klausner JD, Darney PD. Direct access to emergency contraception through pharmacies and effect on unintended pregnancy and STIs: A randomized controlled trial. JAMA. 2005;293:54–62. doi: 10.1001/jama.293.1.54. [DOI] [PubMed] [Google Scholar]
- 3.Camp SL, Wilkerson DS, Raine TR. The benefits and risks of over-the-counter availability of levonorgestrel emergency contraception. Contraception. 2003;68:309–317. doi: 10.1016/j.contraception.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Croxatto HB, Brache V, Pavez M, Cochon L, Forcelledo ML, Alvarez F, Massai R, Faundes A, Salvatierra AM. Pituitary-ovarian function following the standard levonorgestrel emergency contraceptive dose or a single 0.75 mg dose given on the days preceding ovulation. Contraception. 2004;70:442–450. doi: 10.1016/j.contraception.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 5.Grimes DA, Raymond EG. Emergency contraception. Ann Intern Med. 2002;137:180–189. doi: 10.7326/0003-4819-137-3-200208060-00010. [DOI] [PubMed] [Google Scholar]
- 6.Rodrigues I, Grou F, Joly J. Effectiveness of emergency contraception pills between 72 and 120 hours after unprotected sexual intercourse. Am J Obstet Gynecol. 2001;184:531–537. doi: 10.1067/mob.2001.111102. [DOI] [PubMed] [Google Scholar]
- 7.Ellertson C, Evans M, Ferden S, Leadbetter C, Spears A, Johnstone K, Trussel J. Extending the time limit for starting the Yuzpe regimen of emergency contraception to 120 hours. Obstet Gynecol. 2003;101:1168–1171. doi: 10.1016/s0029-7844(03)00352-1. [DOI] [PubMed] [Google Scholar]
- 8.Glassier A. Emergency postcoital contraception. NEJM. 1997;337:1058–1064. doi: 10.1056/NEJM199710093371507. [DOI] [PubMed] [Google Scholar]
- 9.Grimes DA. Switching emergency contraception to over-the-counter status. NEJM. 2002;347:846–849. doi: 10.1056/NEJMsb020913. [DOI] [PubMed] [Google Scholar]
- 10.Zernike K. National Briefing, Health and Science: Morning-After Pill. [Accessed December 7, 2006];The New York Times. 2003 April 22; Available at: http://query.nytimes.com/gst/fullpage.html?res=9C02EFD6103AF931A15757C0A9659C8B63.
- 11.The Henry J. Kaiser Family Foundation [Accessed December 7, 2006];Emergency contraception. 2005 November; Available at: http://www.kff.org/womenshealth/upload/3344-03.pdf.
- 12.Guttmacher Institute [Accessed May 14, 2007];State policies in brief: Emergency contraception. 2007 May; Available at: http://www.guttmacher.org/statecenter/spibs/spib_EC.pdf.
- 13.Krisberg K. Panel favors providing emergency contraception without a prescription. [Accessed on December 7, 2006];The Nation’s Health. 2004 Available at: http://www.apha.org/tnh/index.cfm?fa=ADetail&ID=633.
- 14.Krisberg K. FDA rejects over-the-counter emergency contraception sales: Reproductive rights march draws crowd. [Accessed on December 7, 2006];The Nation’s Health. 2004 Available at: http://www.apha.org/tnh/index.cfm?fa=ADetail&ID=411.
- 15.U.S. Food and Drug Administration [Accessed on December 7, 2006];FDA approves over-the-counter access for Plan B for women 18 and older; Prescription remains required for those 17 and under. 2006 Available at: http://www.fda.gov/bbs/topics/NEWS/2006/NEW01436.html.
- 16.Sawyer RG, Thompson E. Knowledge and attitudes about emergency contraception in university students. College Student Journal. 2003;37:523–531. [Google Scholar]
- 17.Corbett PO, Mitchell CP, Taylor JS, Kemppainen J. Emergency contraception: knowledge and perceptions in a university population. J Am Acad Nurse Pract. 2006;18:161–168. doi: 10.1111/j.1745-7599.2006.00114.x. [DOI] [PubMed] [Google Scholar]
- 18.The Henry J. Kaiser Family Foundation . Emergency contraception in California: Findings from a 2003 Kaiser Family Foundation Survey. Kaiser Family Foundation; Menlo Park, CA: Feb, 2004. [Google Scholar]
- 19.Trussell J, Ellertson C, Stewart F, Raymond EG, Shochet T. The role of emergency contraception. Am J Obstet Gynecol. 2004;190:S30–S38. doi: 10.1016/j.ajog.2004.01.063. [DOI] [PubMed] [Google Scholar]
- 20.Harper CC, Ellertson CE. The emergency contraceptive pill: a survey of knowledge and attitudes among students at Princeton University. Am J Obstet Gynecol. 1995;173:1438–1445. doi: 10.1016/0002-9378(95)90630-4. [DOI] [PubMed] [Google Scholar]
- 21.Brening RK, Dalve-Endres AM, Patrick K. Emergency contraception pills (ECPs): current trends in United States college health centers. Contraception. 2003;67:449–456. doi: 10.1016/s0010-7824(03)00045-3. [DOI] [PubMed] [Google Scholar]
- 22.Miller LM, Sawyer RG. Emergency contraceptive pills: a 10-year follow-up survey of use and experiences at college health centers in the mid-Atlantic United States. J Am College Health. 2006;54:249–256. doi: 10.3200/JACH.54.5.249-256. [DOI] [PubMed] [Google Scholar]