Abstract
We report a case series of endophthalmitis by an organism hitherto not reported in the eye. Nineteen of 63 cataract patients operated in a high-volume setup were urgently referred to us with acute onset of decreased vision one to two days following cataract surgery. All patients had clinical evidence of acute endophthalmitis with severe anterior chamber exudative reaction. Vitreous tap was done in three representative patients and repeated intravitreal injections were given as per established protocol. The vitreous sample from all three patients grew Enterobacter amnigenus Biogroup II, a gram-negative bacillus which, to the best of our knowledge, has never been reported in the eye. With prompt and accurate microbiological support, it was possible to salvage 17 of these eyes without performing vitrectomy. Six eyes regained 6/200 or better vision.
Keywords: Endophthalmitis, Enterobacter amnigenus, gram-negative bacillus
Endophthalmitis following cataract surgery in a high-volume surgery setting is distressing due to the large numbers of patients involved and the resultant publicity issues. Post-surgical or post-traumatic infection with Enterobacter cloacae or Enterobacter aerogenes has been reported, mostly with dismal results.1,2,3 We report 19 cases of endophthalmitis caused by Enterobacter amnigenus : Biogroup II, an organism hitherto unreported in literature.
Case Report
Nineteen of 63 patients, operated in a high-volume cataract surgery setting at a nearby hospital were referred to us with acute onset of redness and decreased vision. At admission, all patients underwent slit-lamp examination, applanation tonometry, dilated fundus evaluation and B-scan ultrasonography.
Our cohort comprised the last few cases operated on day 2 and almost all patients from Day 3 of the surgical "camp". All patients had undergone sutureless manual small-incision cataract extraction with single-piece polymethylmethacrylate intraocular lens (IOL) implantation. The only reported intraoperative complication was vitreous loss in two eyes. Of these, one was left aphakic while the other had the IOL implanted in the ciliary sulcus. All patients were on topical gentamycin 0.3% six-hourly, topical prednisolone acetate 1% hourly, homatropine 2% drops three times daily and oral ciprofloxacin 500 mg twice daily.
At presentation [Table 1], lid edema, gross corneal edema with severe exudative reaction was seen in all cases [Figs 1 and 2]. Hypopyon was present in 15 eyes. Relative afferent pupillary defect was noted in all the nine patients who had inaccurate projection of rays. Four patients had raised intraocular pressure. The fundal glow was visible in only one patient. B-scan ultrasonography at admission revealed anterior to mid-vitreous echoes in all patients at 60% gain. A retinal detachment was present in patient number 9. Three patients were found to have hitherto undetected diabetes mellitus.
Table 1.
Patient demographics
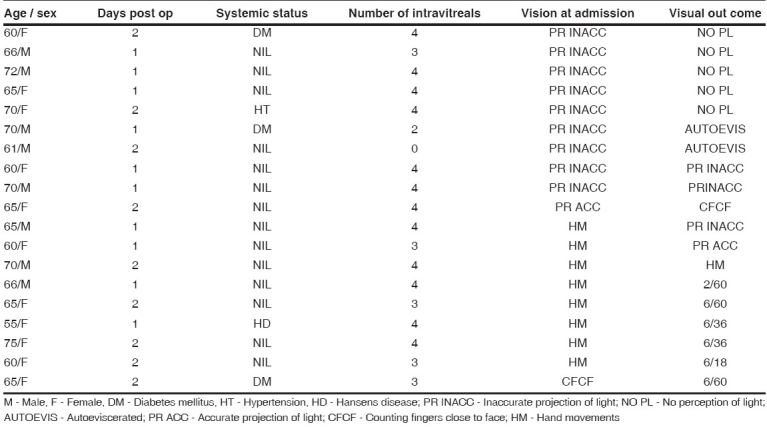
Figure 1.
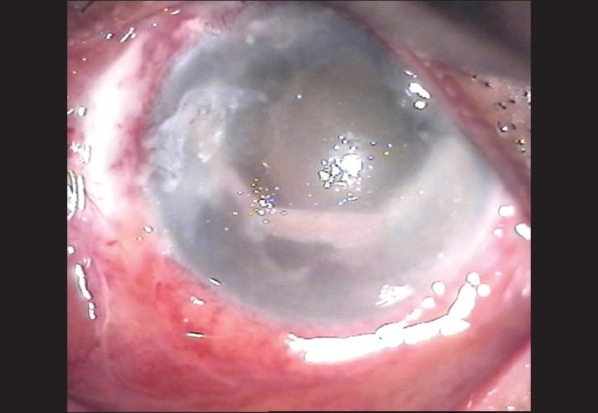
Eye with endophthalmitis showing gross corneal edema and severe anterior chamber exudation
Figure 2.

Eye with endophthalmitis showing gross corneal edema and a lesser degree of anterior chamber reaction
Diagnostic vitreous tap was done in three patients; one representing those with hypopyon, one without hypopyon and one with severe pain. Eighteen patients were given intravitreal injections of vancomycin (1.0 mg / 0.1 ml saline) and ceftazidime (2.25 mg / 0.1 ml saline). One patient refused surgical intervention (patient no. 7). All patients were continued on oral ciprofloxacin 500 mg twice daily. Topical ciprofloxacin (0.3%) hourly, dexamethasone-chloramphenicol combination hourly and atropine sulphate 1% three times daily were started. Oral acetazolamide 250 mg six-hourly, anti-diabetic and anti-hypertensive medication were used as required.
Vitrectomy could not be performed in any patient due to corneal edema and severe anterior chamber exudative reaction.
All three vitreous samples revealed gram-negative bacilli on smear and profuse growth on culture. The organism was identified as Enterobacter amnigenus : Biogroup II. Susceptibility testing (as per the clinical laboratory standards institute)4 revealed identical sensitivity patterns in all three samples. It was resistant to penicillin, vancomycin, gentamicin, norfloxacin, ciprofloxacin, tetracyclin, chloramphenicol, lomifloxacin, ofloxacin and tobramycin and sensitive to ceftazidime, cefotaxime, imipenem and meropenem.
Intravitreal injections were repeated at 48h intervals. Sixteen patients received four doses, two patients refused the last two doses and one patient refused all surgical intervention. Following the sensitivity report, only ceftazidime was given as the third and fourth doses. In poor responders and those patients who developed corneal infiltrates, the topical antibiotic was changed to ceftazidime (50 mg/ml). Duration of hospitalization was 14 to 18 days depending on their response to treatment.
Fig. 3 depicts the vision at admission and discharge. Patients with poorer vision at presentation did worse than those with better vision. Four patients developed corneal infiltrates, which eventually resolved in two patients. The other two resulted in autoevisceration, one a newly detected diabetic who allowed only two intravitreal injections and the other who refused any surgical intervention.
Figure 3.
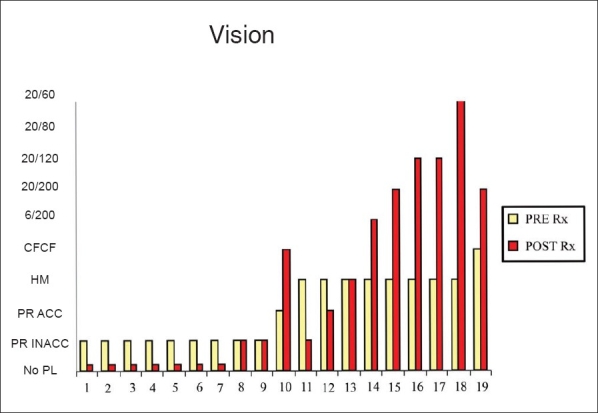
Diagrammatic representation of pre-treatment and post-treatment vision; X axis - patient number; Y axis - vision
Five out of 19 eyes regained 20/200 or better vision [Table 1] within 18 days even without vitrectomy. The globe was preserved in 17 patients. All the diabetics and patients having only two or less intravitreal injections performed poorly.
Discussion
Gram-negative endophthalmitis is a devastating complication following cataract surgery. Pseudomonas is the commonest gram-negative causative organism.5,6 Successful management depends on rapid recognition and prompt intervention.7 Vitreous tap for smear and culture, followed by immediate intravitreal administration of broad-spectrum antibiotics and, a vitrectomy if indicated is the current standard of care. Although most patients in this series qualified for immediate vitrectomy according to the Endophthalmitis Vitrectomy Study protocol,8 this was deferred due to severe stromal edema obscuring the view.
High-volume surgery still has a role in reducing the cataract load in India.9 When endophthalmitis occurs in these settings, every effort should be made to trace the source of infection. Ideally, the efficacy of the sterilizer using test strips, sterility of the air using settle plates and culturing of the swabs, instruments and remaining fluids should be done. In another series of endophthalmitis caused by Entrobacter species, inadvertent use of unsterilized swabs was found to be responsible.2 Investigation into the outbreak however, could not be done fully as the patients came from an independent center. The actual containers of fluids used had been discarded immediately following the surgeries. Only unopened containers from the batch of viscoelastic and intraocular fluids used for the surgeries were provided for culture. These were microbiologically sterile. The causative organism, Enterobacter amnigenus isolated in our series, is an environmental pathogen10 and normally results in infection only if inoculated in high doses. This implies a serious breach of aseptic measures during surgery in these patients.
Lack of follow-up after discharge was another limitation of our study. The patients were absorbed into the referral system of the neighboring state to which they belonged and could not be subsequently followed up by us.
The similar clinical presentation and the fact that all three samples grew the same rare organism, of identical subtype and identical sensitivity patterns, strongly suggests that this organism was responsible for the entire epidemic.
As highlighted by this report, investigating outbreaks of endophthalmitis even in a high-volume surgical setup thus becomes important from the diagnostic, therapeutic and public health point of view.
Acknowledgments
Dr. Thomas Kuriakose DO, DNB, FRCS (Edin) and Dr. Mary S Mathews MD for support and help with preparation of the manuscript.
References
- 1.Okhravi N, Ficker L, Matheson MM, Lightman S. Enterobacter cloacae Endophthalmitis: Report of Four Cases. J Clin Microbiol. 1998;36:48–51. doi: 10.1128/jcm.36.1.48-51.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mirza GE, Karakucuk S, Doganay M, Caglayangil A. Postoperative endophthalmitis caused by an Enterobacter species. J Hosp Infect. 1994;26:167–72. doi: 10.1016/0195-6701(94)90039-6. [DOI] [PubMed] [Google Scholar]
- 3.Milewski SA, Klevjer-Anderson P. Endophthalmitis caused by Enterobacter cloacae. Ann Ophthalmol. 1993;25:309–11. [PubMed] [Google Scholar]
- 4. Performance Standards for Antimicrobial Susceptibility testing: Clinical Laboratory Standards Institute Document M100-S15;15th informational supplement. Vol. 25;No. 1. Pennsylvania: CLSI Press; 2005. pp. 35–8. [Google Scholar]
- 5.Kunimoto DY, Das T, Sharma S, Jalali S, Majji AB, Gopinathan U, et al. Endophthalmitis Research Group. Microbiologic spectrum and susceptibility of isolates: Part I. Postoperative endophthalmitis. . Am J Ophthalmol. 1999;128:240–2. doi: 10.1016/s0002-9394(99)00112-9. [DOI] [PubMed] [Google Scholar]
- 6.Irvine WD, Flynn HW, Jr, Miller D, Pflugfelder SC. Endophthalmitis caused by gram negative organisms. Arch Ophthalmol. 1992;110:1450–4. doi: 10.1001/archopht.1992.01080220112031. [DOI] [PubMed] [Google Scholar]
- 7.Peyman GA, Vastine DW, Raichand M. Post operative endophthalmitis: Experimental aspects and their applications. Ophthalmology. 1978;85:374–85. doi: 10.1016/s0161-6420(78)35659-1. [DOI] [PubMed] [Google Scholar]
- 8.Endophthalmitis Vitrectomy Study Group. Results of the Endophthalmitis Vitrectomy Study. A randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis. Arch Ophthalmol. 1995;113:1479–96. [PubMed] [Google Scholar]
- 9.Venkatesh R, Muralikrishnan R, Balent LC, Prakash SK, Prajna NV. Outcomes of high volume cataract surgeries in a developing country. Br J Ophthalmol. 2005;89:1079–83. doi: 10.1136/bjo.2004.063479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abbot S. Klebsiella, Enterobacter, Citrobacter and Serratia. In: Murray PR, editor. Manual of Clinical Microbiology. 7th ed. Washington DC: American society for Microbiology; 2005. pp. 475–82. [Google Scholar]


