Dear Editor,
Anti vascular endothelial growth factor (VEGF) therapy has tremendously improved the management of wet age-related macular degeneration (AMD). With an increase in the usage of such agents over the last few years, complications have also been noted even though in few. It has been reported that retinal pigment epithelium (RPE) rip can occur following intravitreal injection of bevacizumab and other anti-VEGF agents.1,2
We would like to share our experience with intravitreal injection of bevacizumab (1.25 mg/0.05 ml) in a patient of AMD with fibrovascular pigment epithelial detachment (PED).
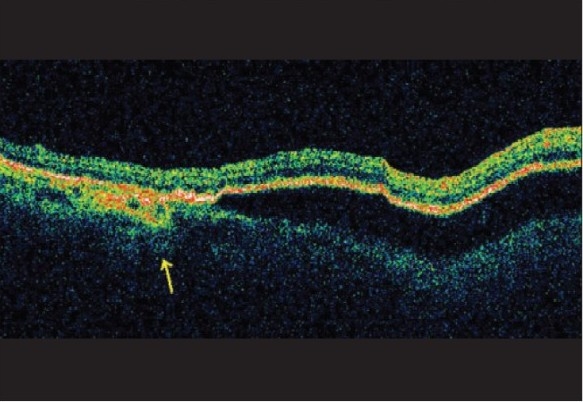
A 52-year-old lady presented a year back with complaints of central scotoma in the right eye of one week duration. Vision at presentation was 20/40; N12 in the right eye and 20/20; N6 in the left eye. Examination revealed a large PED approximately two and half disc diameters at the macula in the right eye with hard exudates superonasal to the PED in the peripapillary area and RPE defects with hard drusen at the macula in the left eye [Fig. 1A]. Fundus fluorescein angiography (FFA) revealed a large PED corresponding with the clinical picture, with ill-defined stippled late leakage temporal to the disc [Fig. 1B]. Indocyanine green angiography (ICG) revealed stippled fluorescence in the temporal peripapillary area with a network of ill-defined vessels [Fig. 1C]. Optical coherence tomography (OCT) showed the large PED with overlying subretinal fluid. A well-defined V-shaped depression (marked) in the contour of the PED corresponding to the tomographic ′notch′ delineated the superior high-domed PED from the adjacent shallow-domed PED. This feature was seen when the OCT scan was taken through the area of stippled hyperfluorescence and this area has been suggested to be indicative of the presence of an occult membrane3 [Fig. 1D].
Figure 1A.

A: Color photograph of the right eye showing the pigment epithelial detachment (PED) at the macula with surrounding exudates. Drusen are also seen
Figure 1B.
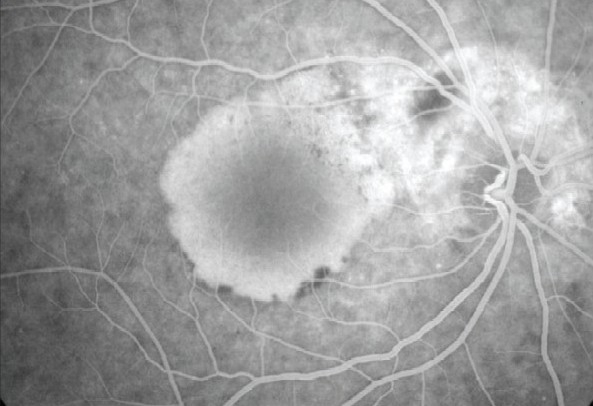
B: FFA photograph of the right eye showing the PED with late phase hyperfluorescence nasal to PED
Figure 1C.
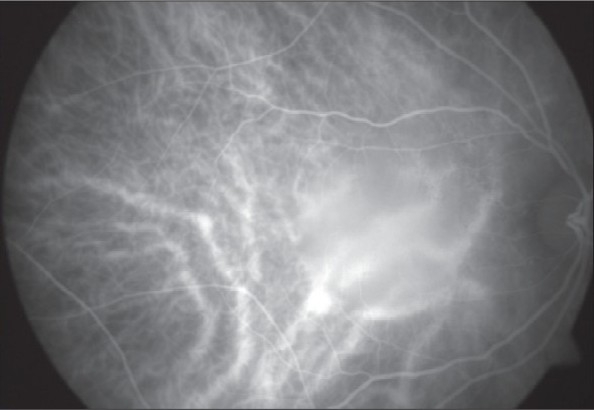
C: ICG early phase of the right eye. The central choroidal vasculature is blurred because of the PED. Stippled fluorescence seen at nasal edge of PED
Figure 1D.

D: OCT of right eye showing high-domed pigment epithelial detachment (PED) with V-shaped notch delineating it from the shallower PED. Hyper-refl ectivity is seen under the shallow PED
Based on the above features (OCT and FFA correlation), a diagnosis of fibrovascular PED with occult membrane at the nasal edge of the PED was made. The patient was explained the different modalities of treatment. Due to economic constraints, the patient chose to undergo intravitreal bevacizumab injection. Two weeks post injection of intravitreal bevacizumab, she recovered to 20/20; N6 in right eye and clinically, PED reduced in size.
She was stable for six months, when she had a recurrence of the symptoms. Her vision was 20/60, N12, the PED had re-occurred at the same location and was comparable to the size on initial presentation. Optical coherence tomography was repeated which showed findings similar to the first presentation [Fig. 2]. Intravitreal injection of bevacizumab was repeated. She reported three months after the injection with further loss of vision in the right eye to 20/200, N36.The size of PED had increased significantly [Figs. 3A and B]. No other clinical change was noted. At this stage it was decided to repeat injection bevacizumab in her eye while monitoring her clinical response. She was stable after two injections, after the third injection she reported a significant improvement in vision. Documented best corrected visual acuity was 20/30; N6 in the right eye and fundus evaluation revealed a reduced height of the PED with a crescentric area of denuded RPE in the temporal region of the PED, away from the fovea [Figs. 4A]. FFA was done which confirmed the large RPE rip within the PED margins [Figs. 4B and C]. Optical coherence tomography was done which revealed the dome-shaped PED, much shallower as compared to the initial OCT images. The foveal scan showed a well-maintained foveal contour of the neurosensory retina over the PED. The scan when taken through the area of the rip showed a focal interruption of the RPE layer and hyper-reflective double layering of the RPE layer indicative of the rolled but flattened RPE rip at the edge of the PED.4 The PED was shallowest towards the edge of the rip [Figs. 4D]. The patient′s vision did not deteriorate as the rip was well away from the fovea.
Figure 2.

OCT picture of the right eye showing high-domed PED six months after bevacizumab injection
Figure 3A.

A: Color photograph of the right eye showing PED with hard exudates temporal to the disc three months after 2nd bevacizumab injection
Figure 3B.

B: OCT of right eye showing high-domed PED after 2nd bevacizumab injection
Figure 4A.

A: Color photograph of the right eye showing the PED with temporal large, crescentric RPE rip after 3rd injection of bevacizumab
Figure 4B.

B: Early phase fluorescein angiography showing the RPE rip with denuded RPE. Autofluorescing Drusen also seen after 3rd bevacizumab injection
Figure 4C.

C: Late Phase FFA with filled PED and RPE rip temporally. Rolled up RPE better delineated along the superior border of the crescent after 3rd bevacizumab injection
Figure 4D.
D: OCT of the right eye showing shallow PED with hyper-reflective double layer of the rolled up edge of the RPE after 3rd bevacizumab injection
Pigment epithelial detachments have been known to develop RPE rips, either spontaneously or following laser photocoagulation and photodynamic therapy. It is usually seen to occur at or along the border of the serous RPE detachment on the side opposite to the location of the choroidal neovascular membrane (CNVM). Spontaneous PEDs are explained by the hydrostatic pressure of leaking exudates from the sub-RPE occult membranes, leading to the formation of RPE detachments as well as the acute RPE tears or rips. The RPE tears post laser and photodynamic therapy are explained by contraction of the fibrovascular tissue comprising the membrane.5,6
In our case, the occult CNVM was located in the peripapillary area, at the nasal edge of the PED and the RPE rip was seen at the temporal border of the PED. The free edge of the RPE had rolled under and retracted towards the area of neovascular tissue.
Anti-VEGF agents act by reducing angiogenesis and arresting the CNVM and thus the same pathology of fibrovascular tissue contraction may be at work in RPE rips following anti-VEGF therapy. Thus the risk of an RPE rip should be considered with treatment with anti-VEGF agents in cases with fibrovascular PEDs.
References
- 1.Spandau UH, Jonas JB. Retinal pigment epithelium tear after intravitreal bevacizumab for exudative age-related macular degeneration. Am J Ophthalmol. 2006;142:1068–70. doi: 10.1016/j.ajo.2006.06.048. [DOI] [PubMed] [Google Scholar]
- 2.Shah CP, Hsu J, Garg SJ, Fischer DH, Kaiser R. Retinal pigment epithelial tear after intravitreal Bevacizumab injection. Am J Ophthalmol. 2006;142:1070–2. doi: 10.1016/j.ajo.2006.07.037. [DOI] [PubMed] [Google Scholar]
- 3.Sato T, Iida T, Hagimura N, Kishi S. Correlation of optical coherence tomography with angiography in retinal pigment epithelial detachment associated with age related macular degeneration. Retina. 2004;24:910–4. doi: 10.1097/00006982-200412000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Giovannini A, Amato G, Mariotti C, Scassellati-Sforzolini B. Optical coherence tomography in the assessment of retinal pigment epithelial tear. Retina. 2000;20:37–40. doi: 10.1097/00006982-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Gass John Donald M. Stereoscopic Atlas of Macular Diseases Diagnosis and treatment. 4 th ed. Mosby Publication; Chapter 3, section on ARMD; pp. 88–91. [Google Scholar]
- 6.Axer-Siegel R, Ehrlich R, Rosenblatt I, Kramer M, Priel E, Yassur Y, et al. Photodynamic therapy for occult choroidal neovascularization with pigment epithelium detachment in age-related macular degeneration. Arch Ophthalmol. 2004;122:453–9. doi: 10.1001/archopht.122.4.453. [DOI] [PubMed] [Google Scholar]


