Abstract
Angioid streaks are crack-like dehiscences in the Bruch′s membrane, which predispose to the development of a choroidal neovascular membrane (CNVM) that carries a poor visual outcome. We report successful treatment in a 25-year-old woman with bilateral angioid streaks and subfoveal CNVM in the left eye who received two doses of intravitreal bevacizumab (1.25 mg) injections six weeks apart, resulting in rapid regression of the CNVM.
Keywords: Angioid streaks, intravitreal bevacizumab, subfoveal choroidal neovascular membrane
Angioid streaks are the result of a crack-like dehiscence in the Bruch′s membrane, which itself is brittle and calcified, and are seen as linear gray lesions radiating from the peripapillary area.1 Visual impairment often occurs as a result of a subfoveal choroidal neovascular membrane (CNVM) with subsequent serous and hemorrhagic detachment of the overlying neurosensory retina. These neovascular membranes associated with angioid streaks present a major challenge in management. Argon laser treatment of the CNVM shows a drop in visual acuity (VA) with high rates of recurrence and persistence.2 Photodynamic therapy using verteporfin has been tried extensively in such eyes with very poor results with most eyes undergoing enlargement and disciform transformation of the neovascularization process.3,4 Poor success and high recurrence rates have been seen after submacular surgery for removal of CNVM in such cases.5 In this case report, we present a case of CNVM associated with angioid streaks treated with intravitreal bevacizumab, an anti-vascular endothelial growth factor (VEGF) molecule.
Case Report
A 25-year-old woman presented with progressive blurring of vision in the left eye of two months duration. There was no history of any systemic illness or previous ocular trauma. Ocular examination revealed a best corrected VA of 20/20 in the right eye and 20/40 in the left eye. The pupillary reactions as well as the slit-lamp biomicroscopic examination of the anterior segment were normal in both the eyes. The posterior segment findings included bilateral, multiple, grayish, subretinal, linear branching streaks extending centrifugally from the peripapillary area and multiple areas of "Peau d′orange" pigmentary changes in the temporal midperipheral fundus. In the left eye one of these streaks passed through the fovea and was associated with a small, grayish, subfoveal lesion with a surrounding bleed [Fig. 1A].
Figure 1.
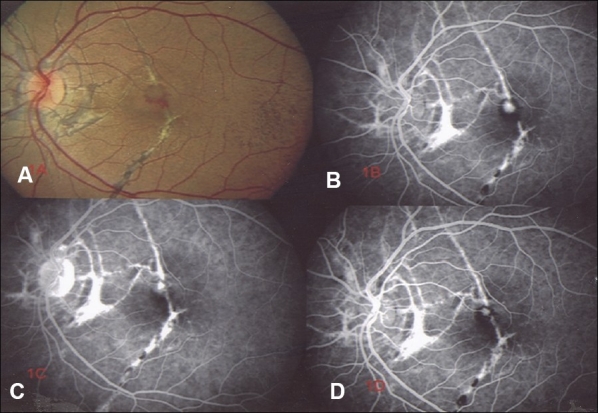
(A) Baseline fundus picture (left eye) showing multiple angioid streaks, with a small, subfoveal lesion; (B) The lesion shows expanding hyperfluorescence and late leakage on angiogram suggestive of choroidal neovascular membrane; (C) Six weeks after the first injection, fundus fluorescein angiography shows reduction in leakage; (D) Two weeks after the second injection, fundus fluorescein angiography shows only transmission hyperfluorescence and no leakage
Fundus fluorescein angiography showed transmission hyperfluorescence corresponding to the linear streaks and an area of expanding hyperfluorescence, with late leakage in the subfoveal location in the left eye [Fig. 1B]. Optical coherence tomography (OCT) confirmed the presence of a subfoveal CNVM with a central retinal thickness (CRT) of 392 microns in the left eye [Fig. 2A].
Figure 2.
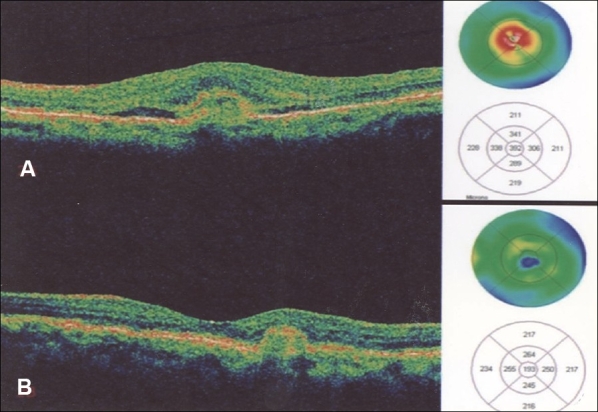
(A) Baseline optical coherence tomography (horizontal line scan through the fovea of left eye) showing a subretinal choroidal neovascular membrane, thin streak of subfoveal fluid, loss of foveal contour, with central retinal thickness of 392 microns; (B) Post-treatment optical coherence tomography (repeat scan two weeks after the second injection) showing reduction in size of lesion, absence of subretinal fluid with normal foveal contour and reduction in central retinal thickness to 193 microns
A detailed systemic workup revealed the presence of multiple hyperpigmented papules on the back of the neck with a highly elastic skin, suggestive of pseudoxanthoma elasticum.
After an informed consent, 1.25 mg intravitreal bevacizumab (Avastin TM , Genetech INA, California, USA) was injected in the left eye under aseptic conditions. Post-injection, her best corrected visual acuity improved to 20/30 and the CRT on OCT reduced to 331 microns at one week and to 211 microns at six weeks. Fundus fluorescein angiogram confirmed reduction in leakage [Fig. 1C].
A second dose of intravitreal bevacizumab (1.25 mg) was repeated six weeks after the first injection. Two weeks after the second dose, her best corrected visual acuity improved to 20/20. Fluorescein angiogram confirmed total absence of any leakage [Fig. 1D] with CRT of 190 microns on OCT [Fig. 2B].
Discussion
Most patients with angioid streaks may remain asymptomatic till development of subfoveal CNVM or a choroidal rupture which carries an extremely poor visual prognosis whether treated or not.2,3,4,5
Recently, vascular endothelial growth factor (VEGF) has been implicated in the pathogenesis of CNVM.6 Bevacizumab is a humanized monoclonal antibody that inhibits all isoforms of VEGF and is FDA-approved for the treatment of colorectal cancer.7 Recently, bevacizumab has been used to treat CNVM due to age-related macular degeneration (ARMD).8,9 These exudative ARMD patients treated with two or three injections of intravitreal bevacizumab showed marked improvement in visual acuity with reduction in angiographic leakage and CRT after 12 weeks of follow-up. These studies showed no untoward effects even after three injections.
As development of CNVM in angioid streaks may also involve similar mechanisms of neovascularization, it prompted us for a trial of the above drug. A literature review using MEDLINE failed to reveal any mention of a case of choroidal neovascularization due to angioid streaks treated with intravitreal bevacizumab. This case illustrates that intravitreal bevacizumab has a possible role in the treatment of the above condition with regression of neovascular membrane and subsequent visual improvement, although a much longer follow-up and a large prospective study is required to reach a conclusive result.
References
- 1.Shields JA, Federman JL, Tomer TL, Annesley WH., Jr Angioid streaks. I. Ophthalmoscopic variations and diagnostic problems. Br J Ophthalmol. 1975;59:257–66. doi: 10.1136/bjo.59.5.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lim JI, Bressler NM, Marsh MJ, Bressler SB. Laser treatment of choroidal neovascularization in patients with angioid streaks. Am J Ophthalmol. 1993;116:414–23. doi: 10.1016/s0002-9394(14)71398-4. [DOI] [PubMed] [Google Scholar]
- 3.Shaikh S, Ruby AJ, Williams GA. Photodynamic therapy using verteporfin for choroidal neovascularization in angioid streaks. Am J Ophthalmol. 2003;135:1–6. doi: 10.1016/s0002-9394(02)01835-4. [DOI] [PubMed] [Google Scholar]
- 4.Arias L, Pujol O, Rubio M, Caminal J. Long-term results of photodynamic therapy for the treatment of choroidal neovascularization secondary to angioid streaks. Graefes Arch Clin Exp Ophthalmol. 2006;244:753–7. doi: 10.1007/s00417-005-0131-3. [DOI] [PubMed] [Google Scholar]
- 5.Thomas MA, Dickinson JD, Melberg NS, Ibanez HE, Dhaliwal RS. Visual results after surgical removal of subfoveal choroidal neovascular membranes. Ophthalmology. 1994;101:1384–96. doi: 10.1016/s0161-6420(94)31172-9. [DOI] [PubMed] [Google Scholar]
- 6.Hangai M, Murata T, Miyawaki N, Spee C, Lim JI, He S, et al. Angiopoietin-1 upregulation by vascular endothelial growth factor in human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci. 2001;42:1617–25. [PubMed] [Google Scholar]
- 7.Chen HX, Mooney M, Boron M, Vena D, Mosby K, Grochow L, et al. Phase II multicenter trial of bevacizumab plus fluorouracil and leucovorin in patients with advanced refractory colorectal cancer: An NCI Treatment Referral Center Trial TRC-0301. J Clin Oncol. 2006;24:3354–60. doi: 10.1200/JCO.2005.05.1573. [DOI] [PubMed] [Google Scholar]
- 8.Bashshur ZF, Bazarbachi A, Schakal A, Haddad ZA, El Haibi CP, Noureddin BN. Intravitreal bevacizumab for the management of choroidal neovascularization in age-related macular degeneration. Am J Ophthalmol. 2006;142:1–9. doi: 10.1016/j.ajo.2006.02.037. [DOI] [PubMed] [Google Scholar]
- 9.Avery RL, Pieramici DJ, Rabena MD, Castellarin AA, Nasir MA, Giust MJ. Intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmology. 2006;113:363–72. doi: 10.1016/j.ophtha.2005.11.019. [DOI] [PubMed] [Google Scholar]


