Abstract
Aim:
To compare the efficacy of intravenous methylprednisolone and intravenous dexamethasone on visual recovery and evaluate their side-effects for the treatment of optic neuritis.
Materials and Methods:
Prospective, randomized case-controlled study including 21 patients of acute optic neuritis presenting within eight days of onset and with visual acuity less then 20/60 in the affected eye who were randomly divided into two groups. Group I received intravenous dexamethasone 200 mg once daily for three days and Group II received intravenous methylprednisolone 250 mg/six-hourly for three days followed by oral prednisolone for 11 days. Parameters tested were pupillary reactions, visual acuity, fundus findings, color vision, contrast sensitivity, Goldmann visual fields and biochemical investigations for all patients at presentation and follow-up.
Results:
Both groups were age and sex-matched. LOGMAR visual acuity at presentation was 1.10 ± 0.52 in Group I and 1.52 ± 0.43 in Group II. On day 90 of steroid therapy, visual acuity improved to 0.28 ± 0.33 in Group I and 0.36 ± 0.41 in Group II ( P =0.59). At three months there was no statistically significant difference in the color vision, contrast sensitivity, stereoacuity, Goldman fields and the amplitude and latency of visually evoked response between the two groups. The concentration of vitamin C, glucose, sodium, potassium, urea and creatinine were within the reported normal limits.
Conclusion:
Intravenous dexamethasone is an effective treatment for optic neuritis. However, larger studies are required to establish it as a safe, inexpensive and effective modality for the treatment of optic neuritis.
Keywords: Dexamethasone; methylprednisolone, optic neuritis.
Optic neuritis is known to improve without treatment though it may also result in long-lasting defects in visual acuity and abnormalities in contrast sensitivity, color vision, stereopsis, light sensitivity, visual fields, pupillary responses, optic disc appearance and visual evoked potentials.1,2
The treatment of optic neuritis has always been controversial3 regarding the use of steroids. Steroids by oral, retrobulbar and intravenous routes have been used. The optic neuritis treatment trial (ONTT)4 a multi-centric collaborative study, compared oral steroids, oral placebo and high-dose intravenous methylprednisolone. The results of the study showed an early visual recovery in the intravenous methylprednisolone group but at the end of one year there was no difference in the visual functions between the three groups. Thus intravenous megadose steroids help towards an early recovery of vision and offer some advantage in preventing a recurrence and development of multiple sclerosis in the first year.2 Intravenous dexamethasone has been widely used post-transplant surgery and in dermatological and rheumatological diseases by the oral route as well as in long-duration intermittent pulse therapy.5,6 Dexamethasone is a highly selective glucocorticoid with flourination at C9 and methyl group at C16.7 It is a cheaper treatment option, with fewer side-effects and is easier to administer as compared to methylprednisolone.8
This study was carried out to compare the efficacy of intravenous methylprednisolone and intravenous dexamethasone on visual recovery, as well as to evaluate their side-effects.
Materials and Methods
This was a prospective, randomized case-controlled institution-based study including 21 patients of acute optic neuritis presenting within eight days of onset and with visual acuity less then 20/60 in the affected eye who were divided into two groups. Written informed consent regarding the nature of study and the treatment to be given was taken from all patients. The patients were randomized into two groups by block randomization and received the following treatment:
Group I: Intravenous dexamethasone 200 mg (in 150 ml 5% dextrose solution) given over one and a half to two hours once a day for three days.
Group II: Intravenous methylprednisolone 250 mg/six-hourly (in 150 ml 5% dextrose solution) given over one and a half to two hours for three days followed by oral prednisolone for 11 days.
Group I consisted of 11 patients and Group II consisted of 10 patients.
In view of the calculated power of the study in a similar pilot study done at our center earlier, a very large sample size was indeed statistically preferred for the present study. The prohibitive number of this calculated sample size was not possible to enroll in this case-controlled study due to the small number of patients presenting with previously untreated acute optic neuritis within eight days of onset and with visual acuity less then 20/60 in the affected eye, at a tertiary care center like ours.
The function of block randomization randomizes ′n′ individuals into ′k′ treatments, in blocks of size ′m′. Random allocation can be made in blocks in order to keep the sizes of treatment groups similar. Randomization reduces opportunities for bias and confounding in experimental designs and leads to treatment groups which are random samples of the population sampled, thus helping to meet assumptions of subsequent statistical analysis.
All cases with known systemic disease other than multiple sclerosis that might be the cause of the optic neuritis were excluded. Cases were also excluded if they had a history of previous attacks of optic neuritis or diagnosis of multiple sclerosis for which the patient had already received corticosteroids or evidence of optic disc pallor in the currently affected eye. Cases with preexisting ocular abnormalities that might affect assessment of visual functions or evidence of any systemic condition for which corticosteroids would be contraindicated were also excluded.
A detailed history, including history of disorders known to cause secondary optic neuritis e.g. sinusitis, syphilis was taken. Patients were requested to be on their regular diet schedule and not take extra helpings of foods rich in vitamin C. This was done so that diet did not bias any possible protective effect of high-dose steroids on plasma vitamin C estimation.
A thorough systemic and neurological examination was performed. A complete ophthalmic examination was performed with slit-lamp evaluation of the anterior segment and evaluation of the posterior segment with slit-lamp biomicroscopy and indirect opthalmoscopy. The pupillary reactions, visual acuity and fundus findings were assessed before and during institution of treatment. Color vision, contrast sensitivity and Goldman fields were recorded for all patients after giving full refractive correction whenever the visual acuity permitted. Magnetic resonance imaging was done where deemed a necessity and in those who could afford the investigation
Visual acuity was assessed using ETDRS (at a distance of 4m) and Snellen (at a distance of 6m) visual acuity charts. Patients with vision of finger counting and less were arbitrarily assigned a LOGMAR score of 1.70.1 Color vision was recorded using Ishihara pseudoisochromatic color vision plates where the visual acuity permitted the assessment of it. The color vision was quantified as the number of plates read on Ishihara pseudoisochromatic plates. Contrast sensitivity was recorded using Pelli-Robson charts (Clement Clarke, UK) at a distance of 1 m. Goldmann visual fields using Goldmann perimeter for both the eyes were done. Stereoacuity was quantified using the Randot stereoacuity test (Wirt circle). visually evoked response (VER) was done with a Lace electronica EREV m99 machine at a distance of 33 cm. Other investigations carried out were complete hemogram, fasting blood glucose, Venereal diseases research laboratory, immuno histocytological analysis for toxoplasmosis, chest X-ray, X-ray paranasal sinuses and aerobic and anaerobic blood cultures.
Serum samples to measure levels of sodium, potassium, urea, creatinine and vitamin C were drawn prior to treatment (day 1) and after completion of treatment (day 4) with a large bore needle so as to avoid hemolysis. All levels were analyzed using standard laboratory procedure with vitamin C levels in serum analyzed using DNP method (2-4 dinitrophenylhydrazine).
Cases not showing any improvements with standard therapy in either group were subjected to additional investigations like orbital ultrasound and neuroimaging as appropriate.
The intravenous steroids were infused by slow intravenous drip over a period of one and a half to two hours. The pulse and blood pressure were recorded prior to the institution of pulse therapy and monitored throughout at 30-min intervals till the completion of the infusion and for one hour thereafter. The doses were repeated on day 2 and day 3.
The patients in both groups were examined every day during the institution of treatment and later at one week, one month and three months.
Data were recorded on a pre-designed proforma and managed on an Excel spreadsheet. Mean and SD summarized variables in the two groups. Baseline values for the visual parameters were statistically different in the two groups; therefore we used analyses of covariance (ANOCOVA) to adjust the mean values of the visual parameters obtained at follow-up time points for the imbalance at baseline. The adjusted mean values were compared using the student′s t test. STATA 7.0 Intercooled version was used for statistical analysis. In this study P value < 0.05 was considered statistically significant.
Results
The mean age of patients in Group I was 31.2 ± 10.1 years and in Group II was 26.6 ± 11.5 years [Table 1]. There was one patient in the pediatric age group in each treatment group. Group I consisted of six males and five females and Group II consisted of six males and four females. Both the groups were age and sex-matched [Table 1].
Table 1.
Clinical profile of the cases
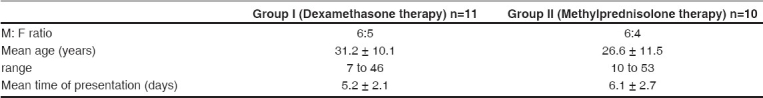
All patients in both the groups presented with abrupt loss of vision. The mean time of presentation in Group I was 5.2 ± 2.1 days, while in Group II was 6.1 ± 2.7 days. Six cases (54.5%) in Group I and six cases (60%) in Group II complained of pain in the affected eye [Table 1]. Unilateral optic neuritis dominated the study group. There were eight patients in each group with unilateral optic neuritis and three patients in Group I and two patients in Group II with bilateral optic neuritis. Retrobulbar neuritis was the more common presentation while 38.09% of patients had disc edema.
The visual acuity [Table 2] was recorded with the ETDRS visual acuity charts. The mean LOGMAR visual acuity in Group I at initial presentation was 1.10±0.52 (range: no perception of light to 20/60) and in Group II was 1.52±0.43 (no perception of light to 20/80). There was a statistically significant difference in the presenting visual acuity of the two groups owing largely to the larger number of patients with poorer vision in Group II. On day 3 of the megadose steroid therapy the visual acuity showed improvement to a level of mean LOGMAR value (after adjustment for baseline difference) of 0.68±0.54 in Group I and 1.10±0.55 in Group II. Although the visual acuity was better in the dexamethasone group, it did not reach statistical significance. Similar result was also seen on follow-up on day 7, day 30 and day 90.
Table 2.
The trend in visual parameters (mean value ± standard deviation)
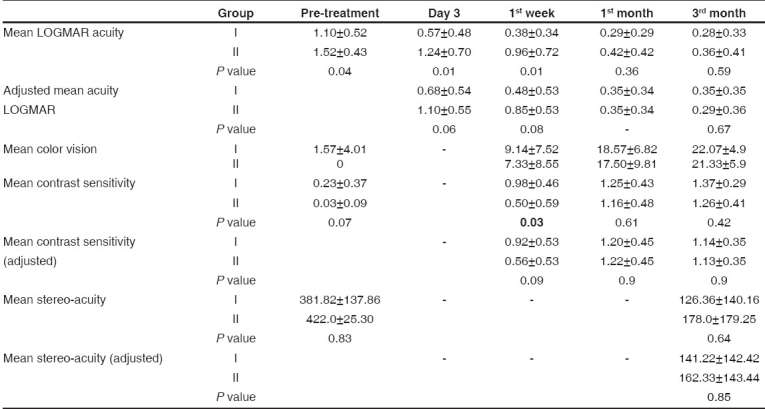
At presentation, the mean color vision was 1.57±4.01 in Group I and 0 in Group II [Table 2]. In Group I a red green color deficiency was noted in three patients who had defective color vision. Fellow eye abnormalities could not be picked up with this test in any patient who presented with unilateral optic neuritis in Group I but was present in one patient in Group II who had a red green color deficiency in that eye. Following treatment the color vision improved in both the groups. At completion of three-month follow-up two patients in Group I and three patients in Group II continued to have defect in color vision and were unable to read all plates on the Ishihara pseudoisochromatic color vision plates. As the mean color vision at baseline was 0 in Group II no statistical comparison of baseline was possible. At follow-up there was no statistically significant difference in the two groups in color vision on day 7, 30 and 90.
The mean value of pretreatment contrast sensitivity [Table 2] by the Pelli-Robson chart was 0.23±0.37 in Group I and 0.03 ± 0.09 in Group II ( P = 0.07). The contrast sensitivity showed significant improvement with treatment during subsequent follow-up to 1.37±0.29 in Group I ( P < 0.001) and to 1.26±0.41 in Group II ( P < 0.001) at three months [Table 2]. Fellow eye defect was noted in three patients in Group I and in one patient in Group II amongst the patients who presented with unilateral optic neuritis. These resolved completely after treatment by day 7. After adjusting for baseline difference in contrast sensitivity, there was no statistically significant difference between the two groups on day 7, 30 and 90.
The stereoacuity was estimated by the Randot test [Table 2]. The mean value of stereoacuity was 381.82 ± 137.86 seconds of arc in Group I and 422.0 ± 25.30 in Group II ( P =0.83). There was a significant improvement in stereoacuity in both the groups with therapy ( P < 0.001 for both groups). There was no significant difference between the two groups in the mean stereoacuity at any of the follow-up time points.
Pretreatment visual fields could be charted in only six patients in Group I and in two patients in Group II. A central scotoma in four patients and diffuse constriction of field in two patients of Group I was seen while both patients in Group II had a central scotoma. At three months follow-up all the patients had fully recovered except for two patients of Group I who had residual central scotoma and one patient in Group II who had persistent relative central scotoma.
There were eight patients in each group with unilateral optic neuritis. In Group I patients with unilateral optic neuritis, fellow eye abnormalities included contrast sensitivity abnormality in three patients and increased VER latency was present in two of these patients. No fellow eye defect in color vision or fields was noted in any patient. In Group II abnormal contrast sensitivity, abnormal color vision and increased VER latency was recorded in one patient. No fellow eye defect in fields was noted in this patient.
None of the parameters showed any significant variation from the pretreatment values in both the groups. The concentration of vitamin C, glucose, sodium, potassium, urea and creatinine were within the reported normal limits with no statistically significant difference between the two groups.
Two patients were found to be hyperglycemic in Group I on initial investigation on day 1. None of the patients had history of diabetes or any evidence of diabetic retinopathy. Blood glucose was normal in these two patients on subsequent investigations.
All of the investigations for infection including VDRL, IHA for toxoplasmosis and anaerobic cultures were negative in all the patients in both the groups. Chest X-rays were either normal or had nonspecific changes. The X-rays of the paranasal sinuses did not show evidence of sinusitis. All other investigations were within normal limits.
None of the patients complained of positive visual phenomenon. Other phenomena such as Uhthoff′s phenomena, Lhermitte′s sign and phosphenes were not reported by any of our patients even on direct questioning. All the patients presented with decreased vision.
On administration of the pulse steroids two patients in Group I and four in Group II complained of generalized weakness. Sleep disturbance and weight gain was noted in one patient of Group II. One patient in Group I and two in Group II had depression. Gastric irritation occurred in two patients of Group I and in three patients of Group II.
Discussion
The present study compared the outcome of visual parameters after treatment with dexamethasone as compared to methylprednisolone in cases of optic neuritis.
The demographic data of the patients enrolled in the study was in accordance with the published figures. The males and females were equally represented in both groups. None of the patients complained of positive visual phenomenon. Other phenomena such as Uhthoff′s phenomena, Lhermitte′s sign and phosphenes were not reported by any of our patients even on direct questioning. All the patients presented with decreased vision.
Unilateral optic neuritis dominated the study group. Retrobulbar neuritis was the more common presentation while 38.09% of patients had disc edema. Other studies also report retrobulbar neuritis as the commonest presentation of optic neuritis. In the ONTT, only 1.8% of its study patients had retinal exudates, while 35.3% manifested disc edema, and the rest had retrobulbar neuritis.9 None of our patients had vitritis, optic disc hemorrhages or sheathing of venules. These are unusual findings in optic neuritis, though sheathing of venules may be noted in multiple sclerosis.
The mean presenting visual acuity of patients in Group II (mean LOGMAR 1.52±0.43) was significantly lower than the mean visual acuity of patients in Group I (mean LOGMAR 1.10± 0.52) ( P value 0.04). This owed largely to the greater number of patients with visual acuity of close to perception of light in Group II. The analysis of covariance (ANOCOVA) was used to adjust the mean values of the visual parameters obtained at follow-up time points for the imbalance at baseline. The ONTT had noted that patients with a poorer initial visual acuity tended to have a poorer visual outcome. This was also observed in both the groups in our study.
Following treatment, all visual parameters recovered rapidly in both the groups. On comparing the adjusted mean values on follow-up, the patients given dexamethasone fared better in contrast sensitivity on Day 7, (mean contrast sensitivity Group I on day 7 was 0.92±0.53 and in Group II, 0.56 ± 0.53) though the difference was not statistically significant. There was no significant difference in the relative improvement of contrast sensitivity.
The change in color vision in terms of number of plates read was significantly more in Group II. The patients in Group II improved from a value of mean zero plates read [Table 2]. All patients who had a recordable color vision defect had a red green color deficiency.
While comparing dexamethasone and methylprednisolone, recovery in visual parameters was similar till three months of follow-up. In a study carried out in cases of multiple sclerosis,10 dexamethasone and high-dose methylprednisolone were similarly efficacious in promoting recovery. Dexamethasone was earlier found to be efficacious in patients with optic neuritis.11 Taking into consideration the difference in cost [Methylprednisolone (Solumedrol Rs. 990 for 1g), dexamethasone (Decamycin Rs. 160 for 200 mg)] of administration of both the treatments, dexamethasone can be considered as an alternative to methylprednisolone for treatment of optic neuritis in our country.
Other eye involvement in cases with unilateral optic neuritis included contrast sensitivity abnormality in three patients and increased VER latency was seen in two of these patients. The optic neuritis study group noted fellow eye defects in around 40% of patients and stated that these need not necessarily be clinically manifest.9 Therefore it is important to test for fellow eye defects as they may present sub-clinically. Evaluation of contrast sensitivity by Pelli-Robson chart can be an important modality to pick up sub-clinical fellow eye defects.
All patients were negative for serological investigations. None of the patients yielded a positive blood culture. Chest X-ray was normal or had nonspecific changes. The ONTT had concluded that laboratory investigations and CSF examination were not required routinely.9 However, from the present study it is difficult to make any such conclusions. Also, in this study we included only typical cases and such investigations are more necessary in the atypical cases and non-responding cases.
In our study, one patient in the dexamethasone group developed recurrence at eight months of follow-up. This patient recovered good vision on treatment with intravenous dexamethasone. One patient in the methylprednisolone group developed overt clinically diagnosed multiple sclerosis. Both these patients had MRI lesions suggestive of multiple sclerosis prior to enrolment in the study. It has been said that recurrence rate and the probability of developing clinically defined multiple sclerosis (CDMS) is higher in presence of MRI lesions.9,12
All the side-effects were of a mild nature not requiring any treatment. In the ONTT the adverse effects of treatment included insomnia, mood changes, gastritis, facial flushing and weight gain.13
Vitamin C is considered the principal antioxidant of the nervous system. Steroids are known to have an antioxidant effect when given at megadoses.14,15 Therefore at times of stress, steroids may have a possible effect in sparing of vitamin C. All patients in our study had normal levels of vitamin C values, in comparison to Ichibe,16 wherein the authors had shown that a significant number of patients had low plasma levels of ascorbic acid. In our study a low level of ascorbic acid in serum was not found to be associated with optic neuritis. The values of serum potassium, urea, creatinine were within normal limits in both groups and the change that did occur, was minor and in accordance with previously published studies.
A comparison of dexamethasone and methylprednisolone in cases of untreated idiopathic optic neuritis has been tried for the first time. Our study showed intravenous dexamethasone to be as effective as megadose intravenous methylprednisolone therapy as recommended by the ONTT study. Patients on dexamethasone responded well to therapy with prompt recovery of visual parameters and no serious side-effects. Dexamethasone can be considered as an alternative to methylprednisolone for treatment of optic neuritis. However, larger studies should be carried out to establish the efficacy and safety of intravenous dexamethasone as an alternative to intravenous methylprednisolone.
Footnotes
Presentation at a meeting: 30th North American Neuro Ophthalmology Society meeting, Orlando, USA, 30th March 2004
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Miller NR, Newman NJ, Valerie, Biousse, Kerrison JB, Walsh FB, Hoyt WF, editors. Clinical neuroophthalmology. Singapore: Lippincott Williams and Wilkins; 2004. [Google Scholar]
- 2.Beck RW. The optic neuritis treatment trial: Three year follow-up results. Arch Ophthalmol. 1995;113:136–7. doi: 10.1001/archopht.1995.01100020014004. [DOI] [PubMed] [Google Scholar]
- 3.Brusaferri F, Candelise L. Steroids for multiple sclerosis and optic neuritis: A meta-analysis of randomized controlled clinical trials. J Neurol. 2000;247:435–42. doi: 10.1007/s004150070172. [DOI] [PubMed] [Google Scholar]
- 4.Cleary PA, Beck RW, Anderson MM, Jr, Kenny DJ, Backlund JY, Gilbert PR. Design, methods and conduct of the ONTT. Control Clin Trials. 1993;14:123–42. doi: 10.1016/0197-2456(93)90015-6. [DOI] [PubMed] [Google Scholar]
- 5.Pasricha JS, Thanzama J, Khan UK. Intermittent high-dose dexamethasone-cyclophosphamide therapy for pemphigus. Br J Dermatol. 1988;119:73–7. doi: 10.1111/j.1365-2133.1988.tb07104.x. [DOI] [PubMed] [Google Scholar]
- 6.Mussot-Chia C, Flechet ML, Napolitano M, Herson S, Frances C, Chosidow O. Methylprednisolone-induced acute generalized pustulosis. Ann Dermatol Venereol. 2001;128:241–3. [PubMed] [Google Scholar]
- 7.Hardman JG, Limbird LE, Gilman AG, editors. The pharmacological basis of therapeutics. New York: Macmillan; 2006. [Google Scholar]
- 8.Hari P, Srivastava RN. Pulse corticosteroid therapy with methylprednisolone or dexamethasone. Indian J Pediatr. 1998;65:557–60. doi: 10.1007/BF02730894. [DOI] [PubMed] [Google Scholar]
- 9.Optic Neuritis Study Group. The clinical profile of optic neuritis. Experience of the Optic Neuritis Treatment Trial. Arch Ophthalmol. 1991;109:1673–8. doi: 10.1001/archopht.1991.01080120057025. [DOI] [PubMed] [Google Scholar]
- 10.La Mantia, Eoli M, Milanese C, Salmaggi A, Dufour A, Torri V. Double-blind trial of dexamethasone versus methylprednisolone in multiple sclerosis acute relapses. Eur Neurol. 1994;34:199–203. doi: 10.1159/000117038. [DOI] [PubMed] [Google Scholar]
- 11.Sethi HS, Menon V, Sharma P, Khokhar S, Tandon R. Visual outcome after intravenous dexamethasone therapy for idiopathic optic neuritis in an Indian population: A clinical case series. Indian J Ophthalmol. 2006;54:177–83. doi: 10.4103/0301-4738.27069. [DOI] [PubMed] [Google Scholar]
- 12.High-dose corticosteroid regimen retards development of multiple sclerosis in optic neuritis treatment trial. Arch Ophthalmol. 1994;112:35, 6. doi: 10.1001/archopht.1994.01090130045014. [DOI] [PubMed] [Google Scholar]
- 13.Chrousos GA, Kattah JC, Beck RW, Cleary PA. Side effects of glucocorticoid treatment. Experience of the optic neuritis treatment trial. JAMA. 1993;269:2110, 2. [PubMed] [Google Scholar]
- 14.Spoor TC, Hartel WC, Lensink DB, Wilkinson MJ. Treatment of traumatic optic neuropathy with corticosteroids. Am J Ophthalmol. 1990;110:665–9. doi: 10.1016/s0002-9394(14)77065-5. [DOI] [PubMed] [Google Scholar]
- 15.Braakman R, Schouten HJ, Blaauw-van Dishoeck M, Minderhoud JM. Mega dose steroids in severe head injury. Results of a prospective double-blind clinical trial. J Neurosurg. 1983;58:326, 33. doi: 10.3171/jns.1983.58.3.0326. [DOI] [PubMed] [Google Scholar]
- 16.Ichibe Y, Ishikawa S. Optic neuritis and vitamin C. Nippon Ganka Gakkai Zasshi. 1996;100:381–7. [PubMed] [Google Scholar]


