Abstract
Purpose:
To understand the reasons why people in rural south India with visual impairment arising from various ocular diseases do not seek eye care.
Materials and Methods:
A total of 5,573 persons above the age of 15 were interviewed and examined in the South Indian state of Andhra Pradesh covering the districts of Adilabad, West Godavari and Mahaboobnagar. A pre-tested structured questionnaire on barriers to eye care was administered by trained field investigators.
Results:
Of the eligible subjects, 1234 (22.1%, N=5573)) presented with distant visual acuity < 20/60 or equivalent visual field loss in the better eye. Of these, 898 (72.7%, N=1234) subjects had not sought treatment despite noticing a decrease in vision citing personal, economic and social reasons. The analysis also showed that the odds of seeking treatment was significantly higher for literates [odds ratio (OR) 1.91, 95% confidence interval (CI) 1.38 to 2.65], for those who would be defined as blind by visual acuity category (OR 1.35, 95% CI 0.96 to 1.90) and for those with cataract and other causes of visual impairment (OR 1.50, 95% CI 1.11 to 2.03). Barriers to seeking treatment among those who had not sought treatment despite noticing a decrease in vision over the past five years were personal in 52% of the respondents, economic in 37% and social in 21%.
Conclusion:
Routine planning for eye care services in rural areas of India must address the barriers to eye care perceived by communities to increase the utilization of services.
Keywords: Barriers, eye care, service uptake, visual impairment
Visual impairment and blindness due to ocular diseases is a significant public health problem in many parts of the world including the Indian state of Andhra Pradesh.1 Refractive errors and cataracts are the leading causes of avoidable blindness and visual impairment.2 Uncorrected refractive errors and cataract are most commonly found in rural, often remote, underdeveloped areas.3 This could be one of the important reasons for low uptake of eye care services. We have shown that only 18% of those with refractive error in rural areas had received correction as compared to 82% in urban areas.2 Moreover, in India, more than 80% patients with cataract blindness who were advised surgery did not take the advice over a two-year follow-up period because of economic or social constraints.4 If elimination of avoidable blindness is to be achieved in India, all the components, namely disease control, human resource development and infrastructure development must work in concert for an effective eye care delivery system. This would be possible if attempts were made to continually obtain and use good quality population-based data on blindness, perceived barriers to eye care services and effectiveness of various eye care delivery systems.
A variety of socio-cultural factors have been reported to affect the utilization of healthcare services in urban areas.5 In India, however, most of the studies provide data only on utilization patterns perceived by cataract patients.6,7,8 A systematic effort to produce good quality data on barriers to eye care as perceived by visually impaired subjects in rural areas is a prerequisite to design locally suitable programs that aim to eradicate avoidable blindness.
The role of demographic variables in vision loss and treatment-seeking behavior for visual impairment caused by easily treatable refractive errors and cataract in rural areas must be understood and taken into account while implementing programs under the global initiative, VISION 2020: The Right to Sight.9 The rationale for the inclusion of refractive errors and cataracts is that in combination, these form the leading cause of blindness and the treatments available for them are among the most successful and cost-effective of all health interventions.10 Since the majority of Indians live in rural areas (http://www.censusindia.net/results/summaryindia.html/) and are less likely to use eye care services,6,8 they are likely to suffer the loss of more disability adjusted life years and heavier economic loss.11
Andhra Pradesh is one of the four states of Southern India. It had an estimated population of 76 million in 2001 (http://www.censusindia.net/results/summaryindia.html/). The rural areas in Andhra Pradesh under the Andhra Pradesh Eye Disease Study (APEDS) included the districts of Adilabad, West Godavari and Mahaboobnagar. To our knowledge, there has been no systematic study on the perceived barriers to eye care in patients with visual impairment due to various ocular diseases in the rural areas of India. In this paper, we report the combined results from the three rural areas included in the APEDS to understand the perceived reasons why visually impaired people in rural Andhra Pradesh either utilize or do not utilize eye care services.
Materials and Methods
APEDS
This study aimed to obtain reliable population-based epidemiological data regarding prevalence and causes of eye diseases and the perceptions of people regarding visual impairment and barriers to eye care.
APEDS was a population-based epidemiological study of 10,000 people in four areas representative of the Indian state of Andhra Pradesh between October 1996 and February 2000. The APEDS methodology has been described in detail elsewhere.12 In brief, the sample size was determined on the eye diseases of interest with the least assumed prevalence and power to detect odds ratios for risk factors. In all, 7,771 subjects were sampled for the rural segment of APEDS using a systematic, stratified, random and cluster sampling strategy. The Ethics Committee of the L.V. Prasad Eye Institute, Hyderabad, India, approved this study.
After a pilot conducted on a sub-sample in the West Godavari district, a structured questionnaire was administered by trained bilingual field investigators to participants> 15 years of age in their homes and in hospitals to those who responded to an invitation to go through an ocular examination. After the pilot test, the variables in the questionnaire were not changed but the list of barriers was modified slightly. The quality control measures taken are described elsewhere.12 Briefly, reliability was tested amongst the field investigators for administration of the APEDS instruments, especially those related to visual function, quality of life and barriers, as their subjective nature is well understood. The principal investigator (LD) and co-investigator (RD) randomly checked the administration of the questionnaire to ensure quality control. The field investigators were familiar with the different dialects spoken in the three rural areas and were not aware of the visual acuity and ocular diagnosis prior to interviewing the subject. Ophthalmologists and refractionists had access to the completed questionnaires before they conducted the ocular examination. The sequence of the questionnaire is shown in Figure 1. Participants were asked if they had noticed any change in vision over the past five years. Those who said yes were asked if they had sought treatment for the noticed change in vision. We then further explored the barriers to obtaining a regular eye checkup among those who did not find any change in vision and those who had perceived a decrease in vision but who had not sought treatment. The questionnaire included a list of barriers, which were later categorized into personal, social and economic. The investigators documented multiple responses and marked with a separate code the most important reason as perceived by the subjects. The subjects were then invited to undergo a detailed eye examination at a local site. Objective and subjective refraction were done for all those who presented with distant/or near visual acuity worse than 20/20 in either eye. Written informed consent was obtained from participants before the examination.
Figure 1.
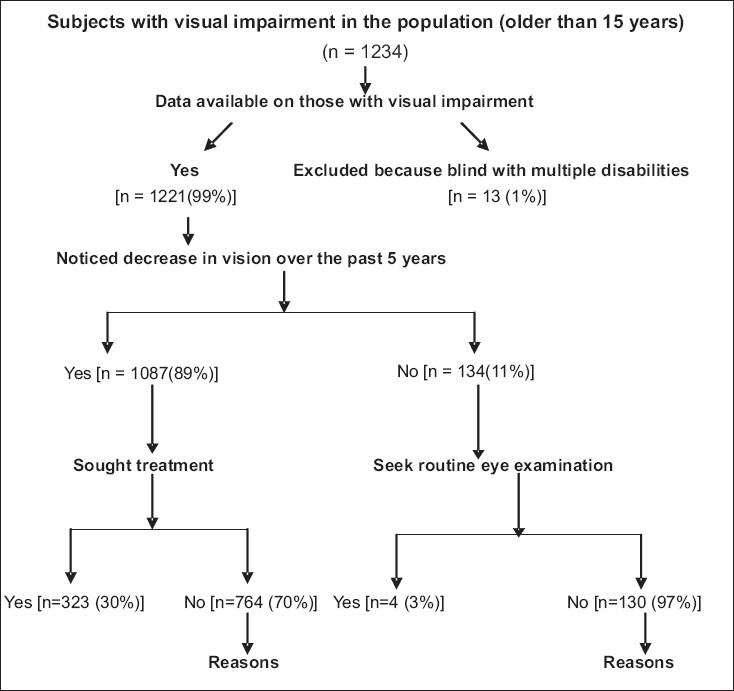
Barriers to eye care in rural areas
Method used for visual acuity and visual field
Distance and near visual acuity both presenting and best corrected after refraction were measured for each eye separately using log MAR (logarithm of minimum angle of resolution) charts. Presenting visual acuity was measured with currently used refractive correction or no correction if the participant was using none. English alphabet log MAR chart was used for those who could read the English alphabet and E-type charts were used for those who could not read the English alphabet. Distance visual acuity was measured in a standardized manner using illumination of at least 200 lux, which was checked with a photometer. If presenting visual acuity was worse than 20/20, objective refraction was performed with a streak retinoscope followed by subjective acceptance with which the best-corrected visual acuity was measured and recorded. Automated visual fields were done with the Humphrey visual field analyzer using the central 24-2 threshold strategy in those participants assessed to have any suspicion of glaucoma or other optic nerve pathology. All unreliable or abnormal visual fields were repeated on another day.
Definition of visual impairment
Visual impairment was defined as presenting distance visual acuity < 20/60 or equivalent visual field loss in the better eye. For distance visual acuity of < 20/200, the equivalent visual field loss was considered as central visual field < 20˚;13 the criteria used for visual field loss equivalent to distance visual acuity < 20/60 -20/200 are described in detail elsewhere.14 The causes of moderate visual impairment were classified as described previously.14 In brief, if cataract and a posterior-segment lesion of the optic nerve or retina were present and removal of cataract would not restore vision, the cause of visual impairment was considered to be the posterior-segment lesion. If nuclear cataract of LOCS 3 grade nuclear opalescence # 3.5 or more was present and vision improved from moderate visual impairment to no visual impairment category with myopic correction in the absence of myopic fundus changes (such as peripapillary chorioretinal atrophy), the cause of visual impairment was considered to be cataract and not refractive error because the former was the underlying cause of this index myopia.2,13 This seemed reasonable to the APEDS investigators because in their experience cataract surgery is usually considered for this grade of cataract since spectacles correction in such cases of index myopia does not provide good visual acuity for more than a few months. If a subject had visual impairment from different causes in the two eyes, both were given 50% weightage.2,13
The software SPSS for windows (SPSS Inc, Chicago, IL) was used for statistical analysis to assess the use of eye care services by subjects in rural areas with visual impairment due to cataract and refractive errors. Our experience in the same geographical region where the L V Prasad Eye Institute provides primary and secondary eye care services is that the majority of young people (15 to 35 age group) presented with visual acuity < 20/60 and therefore we perceived that the results are not skewed in favor of aged visually impaired.
The odds ratios at 95% CI for noticing decrease in vision and seeking treatment were adjusted for demographic factors, level of visual impairment and cause of visual impairment, thus adjusting for the confounding variables in the multiple regression model.
The barriers to eye care were also assessed based on the level of visual impairment. These barriers perceived by subjects were categorized into personal, social and economic for convenience of analysis . Individual perceptions (severity of problem and knowledge of eye care services) for not seeking treatment were categorized as personal. The reasons connected with money (loss of wages, traveling and treatment cost) were grouped under economic reasons linked to the support of family members or lack thereof, and obligations related to family/harvest/business were categorized as social. Univariate analyses were done followed by multivariate analysis using multiple logistic regression. Keeping the first or the last category as the reference we assessed the effect of each category of a multi-categorical variable. Age, gender, education, socioeconomic status, religion, level of visual impairment and cause of visual impairment were included in the multivariate model.
Results
Total subjects
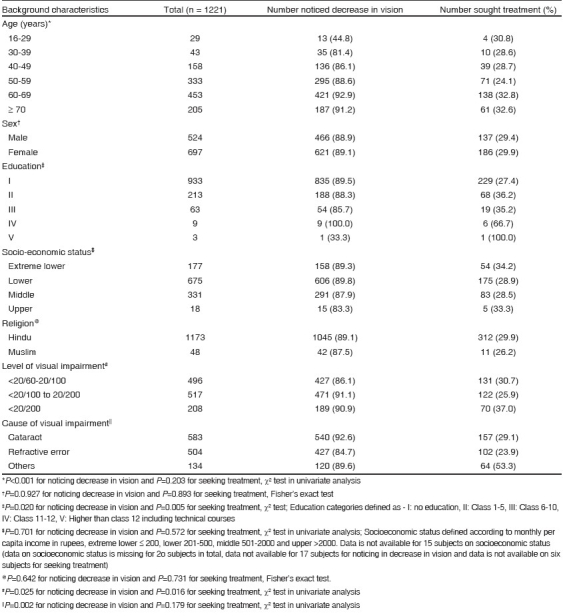
The questionnaire was administered to 5,573 (71%) of the participants who were above 15 years of age at home. One thousand two hundred and thirty-four subjects presented with distant visual acuity < 20/60 or equivalent visual field loss in the better eye. Thirteen visually impaired subjects were not considered for analysis for the following reasons: these participants were blind (n=1), blind and deaf (n=1) blind and dumb (n=1), mentally disabled (n =2) and deaf (n =8). Data were available for 1221 subjects with visual impairment. Of them, 1087 (89%) noticed a decrease in vision over the past five years and 134 (11%) subjects had not noticed any change in vision. The participants included 697 (57%) females and 1173 (96%) Hindus, 933 (76%) illiterates and 852 (69.7%) from the lower socioeconomic groups [Table 1].
Table 1.
Distribution of subjects who noticed a change in vision in the preceding five years and treatment sought by background characteristics
Prevalence
The prevalence of visual impairment was 16.2% (95% CI 12.28 to 17.22%) in the subjects> 15 years of age. The prevalence of not seeking treatment despite noticing a change in vision was 68.6%, (95% CI 65.93 to 71.45%), while the prevalence of not seeking treatment among those with refractive error as cause of visual impairment was 71.2%, (95% CI 69.31 to 75.21%), and 36.7%, (95% CI 32.84 to 40.66%) among participants with cataract as cause of visual impairment.
Level of visual impairment
Of the participants with visual impairment, 1013 (85.30%) had moderate visual loss (visual acuity of < 20/60 to 20/200) and 208 (14.60%) subjects were blind (visual acuity < 20/200) [Fig. 1] according to the WHO definition of severe visual impairment.
Cause of visual impairment
Of all the visually impaired subjects, 583 (47.70%) had cataract and 504 (41.20%) had refractive errors as causes of visual impairment. In 134 (10.90%) participants, the visual impairment was due to other reasons (retina, glaucoma, corneal disease, optic atrophy, amblyopia and congenital eye anomaly).
Subjects with noticed decrease in vision
On applying multiple logistic regression [Table 2], the odds of noticing decrease in vision significantly increased with the increasing age (OR 1.85, 95% CI 1.24 to 2.76). We also found a significant association between cataract and "other" causes of visual impairment and noticing decrease in vision (OR 1.72, 95% CI, 1.15 to 2.55).
Table 2.
Effect of demographic and functional visual acuity levels on noticing decrease in vision in the preceding five years and on seeking treatment (Multivariate logistic regression analysis)

Subjects with treatment
Of all the visually impaired subjects in rural areas, 323 (30%) had sought treatment after noticing a decrease in vision. On applying multiple logistic regression [Table 2], the odds of seeking treatment were significantly higher for literates (OR 1.91, 95% CI 1.38 to 2.65) and for those with cataract and other causes as cause of visual impairment (OR 1.50, 95% CI 1.36 to 2.39). We did not find any significant association between seeking treatment and higher socioeconomic status, religion or gender. The odds of seeking treatment were high for those with a level of visual impairment < 20/200 but did not reach statistical significance (OR 1.35, 95% CI 0.96 to 1.90).
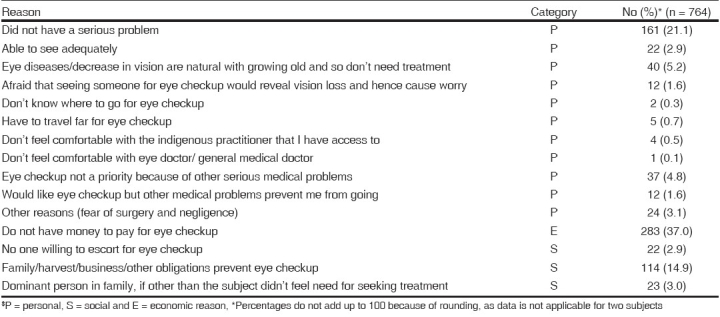
Barriers to seeking treatment
Barriers to seeking treatment for those who had not sought it [Table 3] despite noticing a decrease in vision [Table 4] over the past five years were personal in 52%, economic in 37% and social in 21% respectively. Data were unavailable for two subjects who were uncooperative [Table 4].
Table 3.
Reasons for not utilizing routine eye examination services
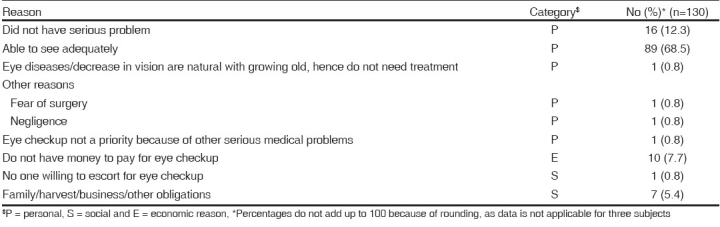
Table 4.
Reasons for not utilizing eye care services even after noticing a change in vision
Association between demographic variables and percentage of perceived barriers to seeking treatment is shown in Fig. 2.
Figure 2.
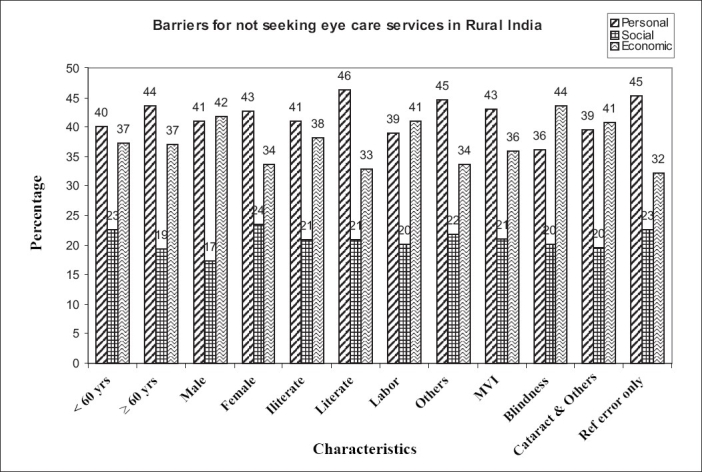
Others: Cataract and other causes (corneal diseases, glaucoma, retinal diseases and others) of visual impairment
MVI: Moderate visual impairment (VA: < 20/100 to - 20/200)
Discussion
These data show that a majority of the participants with visual impairment had noticed a decrease in vision but had not sought treatment, suggesting that vision problems are not a priority for a high proportion of the rural population. Approximately three-quarters of those with visual impairment due to cataract and refractive errors had not sought treatment despite noticing the decrease in vision, mainly because of personal reasons followed by economic and social reasons. The odds for seeking treatment were significantly lower among illiterates and those with refractive error as the cause of visual impairment.
The significant association between age and noticeable decrease in vision over the past five years in this study indicates that in spite of increasing age and perceived decrease in vision, no treatment is sought [Table 2]. As reported earlier, this might be due to the health-seeking priorities in relation to age in rural areas as age influences the decision to seek health.15
It is interesting to report that although subjects with refractive errors as cause of visual impairment noticed a decrease in vision, it translated into seeking treatment only when vision fell to the blindness category level. These findings corroborate reports that subjects with refractive error as cause of visual impairment probably first accommodate with symptoms for a period of time before seeking treatment and seek treatment only when the symptoms become more severe.7,16 This indicates that most people do not try to get treatment despite noticing decreased vision mainly due to factors related to awareness and certain predominant personal reasons [Table 3]. The low service levels (refraction, spectacles and surgical services) in rural areas along with issues of affordability may also have resulted in very few people using eye care services; this in turn has resulted in low levels of appreciation of the need of and benefits from routine eye examination, use of spectacles and surgical services. Half the subjects cited personal reasons for not seeking treatment even after having noticed decreased vision followed by economic and social reasons, similar to the earlier reported urban data of APEDS.16 The predominance of personal reasons demonstrates that greater awareness regarding the importance of seeking treatment for visual impairment is needed to facilitate uptake of eye care services. We did not find any statistically significant association between seeking treatment and socioeconomic status, similar to the urban data reported earlier.16 However, in this study, since the economic and social reasons were found to be other important reasons for not seeking treatment, this study indicates that to increase the uptake of services, we also need to understand the link between social and economic factors (such as "dependency on an earning family member") and impact of direct and indirect costs on seeking treatment in the social context of rural people. This finding is of particularl importance because in the same population refractive errors and cataract were found to be the leading causes of avoidable visual impairment. These conditions are easily treatable if a system is developed to provide routine eye examination services, spectacles and referral services while addressing accessibility and affordability of eye care.
We cannot comment on those variables used in the multivariate analysis with which we did not find a significant association, as the power of the sample to detect associations among these variables was low. We did not find any significant association of gender with seeking treatment, similar to the reports based on the urban data from APEDS14 and dissimilar to the other studies.8,17 The authors also agree that the weakness of this study was that visual acuity was measured differently among those who could read English and those who could not because one group had LogMar charts while the other had Snellen′s charts being used.
The APEDS (2000), a population-based epidemiological survey, found that the prevalence of blindness in the rural areas of Andhra Pradesh was quite high at 2.4; 80% of this blindness was treatable or preventable.2,10 Our analysis also clearly shows that the majority of the rural population studied is illiterate and by definition blind (mainly due to cataract) and did not seek eye care mainly due to personal followed by economic reasons. Therefore, it is imperative that we use new approaches that combine the strategies of prevention and treatment to address these barriers. Since most of the blindness is avoidable and treatable, to make this happen, perhaps what we need is a system that can provide appropriate, accessible and affordable care which meets patients′ eye care needs in a comprehensive and competent manner both at their first contact and on follow-up, throughout their lifetime.
Newer approaches like setting up permanent eye care facilities closer to people like Satellite Eye Centers,18 to provide affordable secondary level eye care and the more recent innovation of establishing "Vision Centers" linked vertically to secondary eye care centers and horizontally to primary health centers to provide primary level eye care may be good ways to overcome the personal and economic barriers which, in turn, would lead to optimum utilization of eye care services. Each Vision Center is run by a trained vision technician who can screen patients free of cost, correct refractive errors by dispensing low-cost spectacles and detect blinding conditions that are referred for further medical and surgical management while addressing issues of accessibility and affordability of eye care at the grassroots. However, to overcome social barriers, we may need to have long-term strategies of community development.
In conclusion, our findings underscore the importance of understanding demographic variables like age, education, level of visual impairment and causes of visual impairment and their significant association with noticing a decrease in vision and seeking treatment in addition to barriers to eye care in rural areas while implementing suitable eye care programmes. If "VISION 2020 target groups/diseases have been identified and 4 tier service delivery model already proposed" is to succeed where it matters, we have to think in terms of finding out what groups are to be targeted and how eye care services are provided.
Acknowledgments
The authors gratefully acknowledge the subjects who participated in the study and the APEDS team which included Lalit Dandona, Rakhi Dandona, Rishita N, VN Naidu, P Giridhar, MNKE Prasad, Partha Mandal, Rohit Khanna, Praveen K Nirmalan, Prashant Sahare, M Srinivas, M Srikanth, Srinivas and Vision CRC Ltd, UNSW, Australia, and Usha Ramana for preparation of manuscript.
Footnotes
Source of Support: Hyderabad Eye Research Foundation, Hyderabad, India and Christoffel-Blindenmission, Bensheim, Germany
Conflict of Interest: None declared
References
- 1.Balasubramanian D, Bhat KD, Rao GN. Factors in the prevalence of cataract in India: Analysis of a recent Indo - US study of age related cataracts. Curr Sci. 1990;59:498–505. [Google Scholar]
- 2.Dandona R, Dandona L, Srinivas M, Giridhar P, Vilas K, Prasad MN, et al. Blindness in the Indian state of Andhra Pradesh. Invest Ophthalmol Vis Sci. 2001;42:908–16. [PubMed] [Google Scholar]
- 3.Thylefors B. A simplified methodology for the assessment of blindness and its main causes. World Health Stat Q. 1987;40:129–41. [PubMed] [Google Scholar]
- 4.Venkataswamy G, Brilliant G. Social and economic barriers to cataract surgery in rural south India. Visual Impairment Blindness. 1981:405–68. [Google Scholar]
- 5.Fassin D, Jeannee E, Cèbe D, Réveillon M. Who consults and where? Sociocultural differentiation in access to health care in urban Africa. Int J Epidemiol. 1988;17:858, 64. doi: 10.1093/ije/17.4.858. [DOI] [PubMed] [Google Scholar]
- 6.Brilliant GE, Briliant LB. Using social epidemiology to understand who stays blind and who gets operated for cataract in a rural setting. Soc Sci Med. 1985;21:553–8. doi: 10.1016/0277-9536(85)90040-1. [DOI] [PubMed] [Google Scholar]
- 7.Gupta SK, Murthy GV. Where do people with blindness caused by cataracts in rural areas of India seek treatment and why? Arch Ophthalmol. 1995;113:1337–40. doi: 10.1001/archopht.1995.01100100125046. [DOI] [PubMed] [Google Scholar]
- 8.Brilliant GE, James M, Lepakowski , Zurita B, Thulsiraj RD. Social determinants of cataract surgery. The operations research group. Arch Ophthalmol. 1991;109:584–9. doi: 10.1001/archopht.1991.01080040152048. [DOI] [PubMed] [Google Scholar]
- 9.Pararajasegaram R. Vision 2020 - The right to sight: From strategies to action. Am J Ophthalmol. 1999;128:359–60. doi: 10.1016/s0002-9394(99)00251-2. [DOI] [PubMed] [Google Scholar]
- 10.Rao GN. Vision 2020 The right to sight. Indian J Ophthalmol. 2000;48:1. [PubMed] [Google Scholar]
- 11.Shamanna BR, Dandona L, Rao GN. Economic burden of blindness in India. Indian J Ophthalmol. 1998;46:263–8. [PubMed] [Google Scholar]
- 12.Dandona R, Dandona L, Naduvilath TJ, Nanda A, McCarty CA. Design of a population based study of visual impairment in India: The Andhra Pradesh Eye Disease Study. Indian J Ophthalmol. 1997;45:251–7. [PubMed] [Google Scholar]
- 13.Dandona L, Dandona R, Naduvilath TJ, McCarty CA, Nanda A, Srinivas M, et al. Is current eye care policy focus almost exclusively on cataract adequate to deal with blindness in India? Lancet. 1998;351:1312–6. doi: 10.1016/S0140-6736(97)09509-3. [DOI] [PubMed] [Google Scholar]
- 14.Dandona L, Dandona R, Naduvilath TJ, McCarty CA, Srinivas M, Mandal P, et al. Burden of moderate visual impairment in an urban population in southern India. Ophthalmology. 1999;106:497–504. doi: 10.1016/S0161-6420(99)90107-0. [DOI] [PubMed] [Google Scholar]
- 15.Morgan M, Calnan M, Manning N. Sociological approaches to health and illness. London: Routledge and Kegan Paul; 1985. p. 81. [Google Scholar]
- 16.Dandona R, Dandona L, Naduvilath TJ, McCarty C, Rao GN. Utilization of eye care services in an urban population in southern India. Br J Ophthalmol. 2000;84:22–7. doi: 10.1136/bjo.84.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fletcher AE, Donoghue M, Devavaram J, Thulasiraj RD, Scott S, Abdalla M, et al. Low uptake of eye services in rural India: A challenge for programs of blindness prevention. Arch Ophthalmol. 1999;117:1393–9. doi: 10.1001/archopht.117.10.1393. [DOI] [PubMed] [Google Scholar]
- 18.Shamanna BR. Establishing sustainable eye care programs in India- some issues and thoughts. JKSOS. 2000;12:105–7. [Google Scholar]


