Abstract
Aim:
To investigate the coefficient of repeatability (CR) for corneal parameters evaluated with Pentacam after laser in situ keratomileusis (LASIK) in myopic eyes.
Design and Setting:
Prospective, non-interventional, non-comparative study in an institutional setup.
Materials and Methods:
Forty eyes of 40 consecutive subjects who had undergone LASIK for myopia were assessed with the Scheimpflug system (Pentacam 70700: Oculus, Wetzlar Germany). The mean of five consecutive measurements of all the corneal parameters was recorded and CR was calculated as standard deviation of the difference from the mean of these repeat measurements divided by the mean response. The statistical significance of the CR was calculated for these parameters at 5% significance level.
Results:
The best CR was observed for the periphery of the anterior corneal curvature (0.18%) and the least for the horizontal meridian of the posterior corneal curvature (1.29%). Despite being significantly different ( P < 0.001), both the measurements were highly repeatable in post-LASIK eyes. The central, apical and minimal corneal thickness had a CR of 1%, 0.78% and 0.77% respectively. These were equally repeatable ( P >0.323). The CR of the mean radius of curvature of the anterior cornea (0.29%) was significantly better ( P < 0.001) than the posterior corneal curvature (0.57%).
Conclusion:
The CR for the post-LASIK cornea with Pentacam was the best for the anterior corneal curvature. Significantly, Pentacam has a high degree of repeatability for the posterior corneal curvature, which has a potential for early detection of keratectasia in these eyes. Post-LASIK pachymetry with Pentacam also showed excellent repeatability.
Keywords: Corneal curvature, pachymetry, pentacam, post-LASIK, repeatability
The Oculus Pentacam (Pentacam 70700: Oculus, Wetzlar Germany) is a rotating Scheimpflug camera that offers a noninvasive way of assessing the anterior chamber of the eye. Topographic corneal thickness, corneal curvature, anterior chamber angle, volume and height are calculated from up to 25,000 data points.
It is important for an anterior segment surgeon to know accurately about the corneal curvature for laser in situ keratomileusis (LASIK) and intraocular lens (IOL) power calculations. For precise assessment of post-LASIK keratectasia accurate elevation maps from the anterior as well as posterior surface of cornea are required. For serial follow-up of post-LASIK curvature changes of cornea, the instrument needs to have high repeatability.
Apical pachymetry is helpful for calculating ablation depth in LASIK and intraocular pressure (IOP) correction factor. Repeatability on Pentacam for pachymetry and anterior chamber depth (ACD) has already been reported in normal eyes.1 The relation of apical, central and thinnest pachymetry is another tool for early detection of keratoconus/ keratectasia.2,3 Post-LASIK eyes need to be closely monitored for changes in corneal parameters like curvature and corneal thickness on an instrument which generates repeatable and accurately reproducible data. Repeatability is defined as a consistency between readings obtained on the same instrument by the same observer or a different observer under conditions that are as constant as possible.3 Orbscan has been shown to be quite inadequate in post-LASIK eyes.4,5,6,7 The purpose of this investigation was to determine the repeatability of corneal parameters in post-LASIK eyes using Pentacam.
Materials and Methods
Forty eyes of consecutive subjects who underwent LASIK for myopia were recruited from the LASIK clinic of the institute. The subjects included had normal ocular examination except for having undergone LASIK for myopia. The exclusion criteria included any optical opacities or pathology on slit-lamp; previous ocular trauma or intraocular surgery; corneal disease or ocular infection; history of ocular disease such as dry-eye syndrome, glaucoma, optic atrophy, macular degeneration, retinopathy or ocular tumor; a follow-up period of less than six weeks and a loss of two or more lines of best spectacle corrected visual acuity. Only the undilated right eye was included in the analysis. LASIK was carried out on Allegretto Wave LASIK 200.
All measurements were taken between the hours of 9:00 AM and 5:00 PM. The subjects had been awake for at least one hour. The volunteers were explained the purpose of the study and informed consent was obtained. The study was performed in adherence to the tenets of the Declaration of Helsinki. Institutional Review Board (IRB) approval was obtained for the study.
The Pentacam captures images of the anterior segment of the eye using blue light emitting diode (LED) and a rotating Scheimpflug camera. The patient was seated with his or her chin on the chinrest and forehead against the forehead strap and asked to fixate straight ahead on the fixation target (blue circular ring). The room lights were switched off for all examinations to get a reflex-free image. The operator focused and aligned real-time image of the patient′s eye on the computer monitor, with the machine marking the pupil edge, center and the corneal apex. Arrows displayed on the screen guided the operator to align the instrument in the horizontal, vertical and translatory axes. To reduce operator-dependent variables, the automatic release mode was used. The rotating camera captured up to 25 slit images of the anterior segment in less than two seconds. Only the scans with quality factor (QS) of >95% were chosen for analysis.
In this study, Pentacam Software V 2.73 r15 was used. The parameters analyzed were apical, central and thinnest pachymetry; horizontal, vertical, peripheral and mean radii of curvature from anterior as well as posterior corneal surface. Apical pachymetry was defined as the pachymetry at the point of highest elevation in the cornea while central pachymetry corresponded to the pupillary center. The peripheral radii of curvature was the mean radii of the zone between the 7 mm and 9mm ring and mean radii of curvature was the mean central radii in the 3 mm zone. The ACD was calculated in the 3-D model from the back surface of the cornea to the anterior lens surface with undilated pupil and the anterior chamber volume (ACV) was calculated based on the integrated distances between the back surface of the cornea and the iris and lens in a 12 mm diameter around the corneal apex.
Our definitions of repeatability were based on the definitions adopted by the British Standards Institution.8,9
Repeatability of the data on Pentacam was evaluated based on five successive scans obtained by the same operator in the right eye of each of the 40 patients. After every reading the Pentacam was moved backwards and realigned for the next scan to eliminate interdependence of the readings. For each patient, the coefficient of repeatability (CR) was defined as the standard deviation of the difference from the mean of these repeat measurements divided by the mean response. For repeatability, conditions were standardized by ensuring that independent test results were obtained with the same method, on the same subject, by the same operator and on the same set of equipment with the shortest possible time lapse between successive sets of readings.
Statistical analyses: Parametric tests were applied for analysis of difference as the distribution of data was not significantly different from normal (Q-Q plot for normal). Plots of the intra-observer differences against their means and the 95% limits of agreement (LoA) (mean difference ± 1.96 SD) were determined as suggested by Bland and Altman.10 Levene′s test was applied for testing the homogeneity of variances. The one-sample t-test, paired t test and one-way ANOVA were used for statistical significance. P values of less than 0.05 were considered to be statistically significant. Statistical analysis was performed using Microsoft Excel and SPSS 13.0 software (SPSS Inc, Chicago, Illinois, USA).
Results
The mean age of subjects enrolled was 24.3 ± 2.3 years (15 to 28 years) and included 12 males and 28 females. The mean ablation depth was 63.54 ± 30.2 microns (34 to 139 microns). The mean spherical equivalent (SEQ) after LASIK was -0.34 ± 0.14D and mean BCVA was 20/20. Mean values of all the parameters post LASIK are summarized in Table 1.
Table 1.
Coefficient of repeatability and limits of agreement for anterior segment parameters on Pentacam in post-LASIK eyes
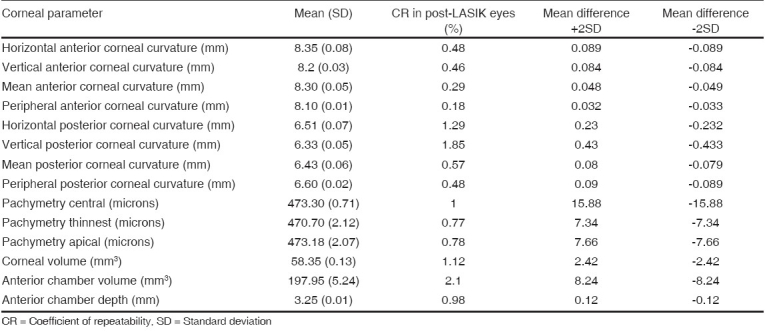
The central, apical and minimal corneal thickness had a CR of 1 %, 0.78 % and 0.77 % respectively [Table 1]. These were equally repeatable ( P =0.323). The 95% LoA plots as suggested by Bland and Altman indicated that 95% of the readings in the same session by the same observer were within ±2 SD. The LoA for the central, apical and thinnest pachymetry were ±15.88 micron, ±7.66 micron and ±7.34 micron, respectively [Fig. 1].
Figure 1.

Bland Altman plot (limits of agreement) for repeatability of central pachymetry (A), apical pachymetry (B) and thinnest pachymetry (C) on Pentacam
The CR was 0.48%, 0.46%, 0.29% and 0.18% for horizontal, vertical, mean and peripheral radii of curvature of the anterior corneal surface [Table 1]. The LoA were ±0.089 mm, ±0.084 mm, ±0.048 mm and ±0.032 mm respectively for horizontal, vertical, mean and peripheral radii of curvature of the anterior corneal surface [Fig. 2]. The CR on ANOVA was statistically different with CR for peripheral corneal curvature being significantly different from CR of horizontal and vertical radii ( P < 0.001) while CR for mean radii of curvature and peripheral corneal curvature were not statistically different from each other ( P =0.16). The CR for horizontal and vertical radii of corneal curvature was also statistically insignificant ( P =0.97).
Figure 2.
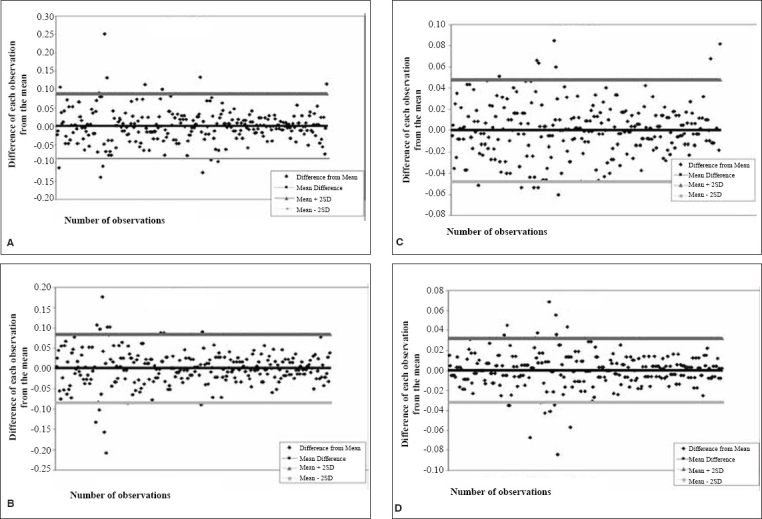
Bland Altman plot (limits of agreement) for repeatability of horizontal meridian of the anterior corneal curvature (A), vertical meridian of anterior corneal curvature (B), mean anterior corneal curvature (C) and peripheral anterior corneal curvature (D) on Pentacam
The CR was 1.29%, 1.85%, 0.57% and 0.48% for horizontal, vertical, mean and peripheral radii of curvature of the posterior cornea, respectively [Table 1]. The LoA were ±0.23 mm, ±0.43 mm, ±0.08 mm and ±0.09 mm, respectively for horizontal, vertical, mean and peripheral radii of curvature of the posterior cornea [Fig. 3]. The CR for vertical meridian on ANOVA was statistically different from mean ( P =0.016) and peripheral corneal curvature ( P =0.007) while CR for horizontal and mean radii of curvature and peripheral corneal curvature were not significantly different from each other ( P =0.885). The CR for horizontal and vertical radii of corneal curvature was also statistically insignificant ( P =0.49).
Figure 3.
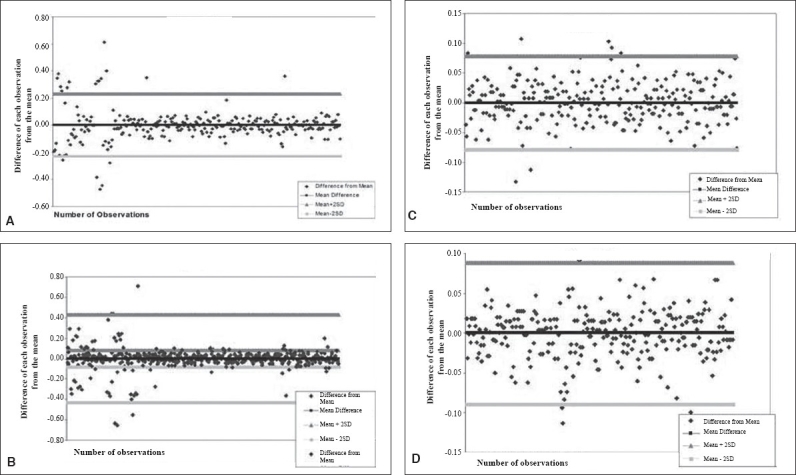
Bland Altman plot (limits of agreement) for repeatability of horizontal meridian of posterior corneal curvature (A), vertical meridian of posterior corneal curvature (B), mean corneal radii of posterior corneal curvature (C) and periphery of posterior corneal curvature (D) on Pentacam
The CR was 2.1% and 0.98% for ACV and ACD respectively. The 95% LoA for ACV were ±8.24 mm 3 and for ACD was ±0.12 mm, respectively [Fig. 4].
Figure 4.
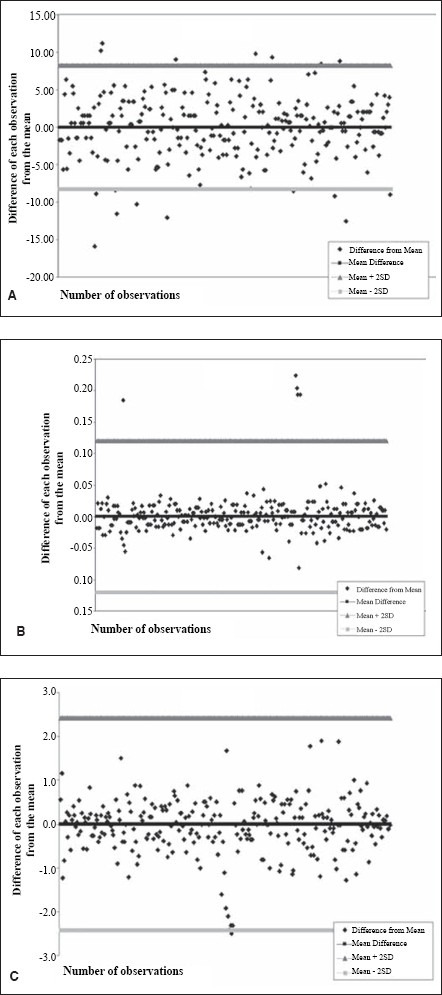
Bland Altman plot (limits of agreement) for repeatability of anterior chamber volume (A), internal anterior chamber depth (B) and corneal volume (C) on Pentacam
The CR for posterior corneal curvature was higher than that of anterior curvature, thereby indicating better repeatability for anterior corneal curvature and on paired t test was significantly different for horizontal ( P < 0.001), vertical ( P =0.005), mean ( P < 0.001) and peripheral radii of curvature ( P < 0.001).
The most repeatable parameter with Pentacam was peripheral anterior corneal curvature (0.21%) and the least, the vertical posterior corneal curvature (1.42%), thereby indicating that the least variations were between the different readings for peripheral anterior corneal curvature taken in the same session by the same observer.
The CR for intra-observer repeatability in 49 normal subjects was not statistically different ( P =0.25) from post-LASIK eyes for all parameters.
Discussion
The easy to use Pentacam is a rotating camera that captures and analyzes Scheimpflug images. It calculates the anterior corneal topography and pachymetry along with additional information on posterior corneal curvature and keratometric power. There is adequate comparative data in the literature but data are scarce regarding the repeatability of the measurements made by each instrument. Previous studies have reported the values to be consistent with existing standards like ultrasound pachymeter. Keeping in view the limitations of the various previous studies on three-dimensional (3-D) testing, the present study has been specifically designed to address the issue of repeatability of measurements made by Pentacam in post-LASIK eyes. The advantage of Pentacam over existing instruments is that it measures and derives all data and calculations from an internal 3-D mathematical software model using the measured height data (elevation). The elevation profile of the cornea is a more accurate representation of the true shape of corneal surface and is a more efficient system to locate the apex of cornea in post-LASIK keratectasia as compared to placido-based curvature measurement systems.
Despite the overall success of LASIK, some issues still remain to be resolved. The biomechanical stability of the cornea is related to residual corneal thickness; therefore, postoperative pachymetry is very important, especially in candidates for enhancement surgery.11,12,13 Literature review reveals that there is considerable inter-instrument variation in post-LASIK pachymetry measurement.
In post-LASIK corneas Orbscan II underestimates the corneal thickness by 35 to 40 microns.4,14 This has been attributed to changes in the refractive index,15 magnification ratio of the posterior cornea,16 stromal haze,5,17 anterior contour of the cornea and inappropriate reconstruction algorithms18 in post-LASIK eyes. Non-contact specular microscopy has been used to measure pachymetry post-LASIK and reported to have no inter-observer difference.19,20 The authors, however, did not analyze the intra-observer repeatability of post-LASIK ultrasonic or Orbscan measurements.
Limits of agreement for the repeatability of central corneal thickness post LASIK was ±58.6 microns. Access to accurate, repeatable/reproducible, noninvasive pachymetry techniques would provide invaluable information, especially in the assessment of refractive surgery patients for stabilization of corneal parameters and also for early detection of post-LASIK keratectasia.
Our findings on Pentacam reveal excellent repeatability for central pachymetry with a variation of ±15.88 microns and even better for the thinnest pachymetry (of utmost significance in post-LASIK eyes) with an intra-observer variation of ±7.66 microns.
The changes in the anterior curvature may not directly be indicative of general corneal protrusion after refractive surgery. Mild degrees of post-LASIK keratectasia at an early stage may be better detected at the level of the posterior corneal surface, which is presumed to remain unchanged after uncomplicated LASIK.21,22,23,24 It is thus prudent to be able to accurately evaluate any change in posterior corneal curvature (for accurate evaluation, the measurements also need to be repeatable). Corneal ectasia after LASIK is reportedly uncommon with the prevalence estimated to be 0.66%.23
In our analysis, Pentacam demonstrated the highest repeatability for the anterior corneal curvature and a very high degree of repeatability for the flat, steep and peripheral meridians of the posterior corneal curvatures. This shows that Pentacam can be used in serial follow-up of the posterior corneal curvature changes in post-LASIK eyes, which could help to identify and predict keratectasia following LASIK. The accuracy of these measurements, however, needs further evaluation and comparisons with the existing standards
A change in ACD or ACV is not expected in post-LASIK eyes. The ACD/ACV measurements may be indirect predictors of forward protrusion of cornea. Although the accuracy of post-LASIK Orbscan measurements has not been reported, bulging or forward shifting of the posterior cornea after refractive surgery is believed to occur.24,25,26 Twa et al.24 showed that the difference in the comparison of posterior corneal surface curvature before and after LASIK was 0.60D measured by Orbscan System.24
Recently, Nishimura et al.21 demonstrated that the posterior corneal curvature, peripheral corneal thickness, ACD and ACV were consistent post-LASIK showing that backward shifting of the peripheral posterior corneal surface due to corneal swelling after LASIK did not occur. Cairns et al.27 however had shown the forward shifting of the posterior cornea by 21.3 µm. This dissimilarity adds to concern over the accuracy of posterior corneal surface analysis in post-LASIK eyes using Orbscan. Whether this shift is a genuine physical ectasia or merely a potential artifact in the Orbscan measurements or in the assumption for analysis is uncertain.21 The "apparent (reported) depth" on Orbscan may thus be an underestimate.
Du et al. also reported that the pre and post-LASIK central ACD depth was lower as measured by Orbscan than by A-scan ultrasonography although this had no clinical significance.28 The measurement of ACD from Pentacam was found to be repeatable in normal subjects.29 The 95% LoA was within ±0.1 mm. The intra-observer CR for ACD in our analysis was 2.68% and LoA was ±0.37 mm in normal subjects while in post-LASIK eyes CR was 0.98% and LoA ±0.12 mm.
The excellent repeatability of the anterior and posterior corneal surfaces indicates that Pentacam provides reliable information as regards the curvature of anterior and posterior cornea, pachymetry and anterior chamber dimensions after LASIK, though the accuracy of these measurements have not been measured in the present study.
In conclusion, Pentacam is a non-contact, quick, repeatable, easy to use instrument which makes it a potentially versatile tool for studying the corneal thickness, anterior and posterior curvature in post-LASIK patients.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Barkana Y, Gerber Y, Elbaz U, Schwartz S, Ken-Dror G, Avni I, et al. Central corneal thickness measurement with the Pentacam Scheimpflug system, optical low-coherence reflectometry pachymeter and ultrasound pachymetry. J Cataract Refract Surg. 2005;31:1729–35. doi: 10.1016/j.jcrs.2005.03.058. [DOI] [PubMed] [Google Scholar]
- 2.Lackner B, Schmidinger G, Skorpik C. Validity and repeatability of anterior chamber depth measurements with pentacam and orbscan. Optom Vis Sci. 2005;82:858–61. doi: 10.1097/01.opx.0000177804.53192.15. [DOI] [PubMed] [Google Scholar]
- 3.O′Donnell C, Maldonado-Codina C. Agreement and repeatability of central thickness measurement in normal corneas using ultrasound pachymetry and the OCULUS Pentacam. Cornea. 2005;24:920–4. doi: 10.1097/01.ico.0000157422.01146.e9. [DOI] [PubMed] [Google Scholar]
- 4.Iskander NG, Anderson Penno E, Peters NT, Gimbel HV, Ferensowicz M. Accuracy of Orbscan pachymetry measurements and DGH ultrasound pachymetry in primary laser in situ keratomileusis and LASIK enhancement procedures. J Cataract Refract Surg. 2001;27:681–5. doi: 10.1016/s0886-3350(01)00820-3. [DOI] [PubMed] [Google Scholar]
- 5.Prisant O, Calderon N, Chastang P, Gatinel D, Hoang-Xuan T. Reliability of pachymetric measurements using Orbscan after excimer refractive surgery. Ophthalmology. 2003;110:511–5. doi: 10.1016/S0161-6420(02)01298-8. [DOI] [PubMed] [Google Scholar]
- 6.Miyata K, Tokunaga T, Nakahara M, Ohtani S, Nejima R, Kiuchi T, et al. Residual bed thickness and corneal forward shift after laser in situ keratomileusis. J Cataract Refract Surg. 2004;30:1067–72. doi: 10.1016/j.jcrs.2003.09.046. [DOI] [PubMed] [Google Scholar]
- 7.Maruoka S, Nawa Y, Masuda K, Ueda T, Hara Y, Uozato H. Underestimation of corneal thickness by orbscan after myopic correction. J Cataract Refract Surg. 2005;31:1854. doi: 10.1016/j.jcrs.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 8.British Standards Institution. London: HMO; 1994. Accuracy (trueness and precision) of measurement methods and results: General principles and definitions. BS ISO 5725 part 1. [Google Scholar]
- 9.British Standards Institution. London: HMO; 1994. Accuracy (trueness and precision) of measurement methods and results: Basic methods for the determination of repeatability and reproducibility of a standard measurement method. BS ISO 5725 part 2. [Google Scholar]
- 10.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]
- 11.Liu Z, Huang AJ, Pflugfelder SC. Evaluation of corneal thickness and topography in normal eyes using the Orbscan corneal topography system. Br J Ophthalmol. 1999;83:774–8. doi: 10.1136/bjo.83.7.774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Iskander NG, Peters NT, Penno EA, Gimbel HV. Postoperative complications in laser in situ keratomileusis. Curr Opin Ophthalmol. 2000;11:273–9. doi: 10.1097/00055735-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Gimbel HV, Anderson Penno EE, Peters NT, Iskander G. LASIK complications; Prevention and management. 2nd ed. Thorofare, NJ: Slack; 2001. pp. 93–116. [Google Scholar]
- 14.Chakrabarti HS, Craig JP, Brahma A, Malik TY, McGhee CN. Comparison of corneal thickness measurements using ultrasound and Orbscan slit-scanning topography in normal and post-LASIK eyes. J Cataract Refract Surg. 2001;27:1823–8. doi: 10.1016/s0886-3350(01)01089-6. [DOI] [PubMed] [Google Scholar]
- 15.Miyata K. Reply to letter by ACK Cheng. J Cataract Refract Surg. 2004;30:2251–2. doi: 10.1016/j.jcrs.2004.08.027. [DOI] [PubMed] [Google Scholar]
- 16.Nawa Y, Masuda K, Ueda T, Hara Y, Uozato H. Evaluation of apparent ectasia of posterior surface of the cornea after keratorefractive surgery. J Cataract Refract Surg. 2005;31:571–3. doi: 10.1016/j.jcrs.2004.05.050. [DOI] [PubMed] [Google Scholar]
- 17.Boscia F, La Tegola MG, Alessio G, Sborgia C. Accuracy of Orbscan optical pachymetry in corneas with haze. J Cataract Refract Surg. 2002;28:253–8. doi: 10.1016/s0886-3350(01)01162-2. [DOI] [PubMed] [Google Scholar]
- 18.Snook RK. Pachymetry and true topography using the Orbscan system. In: Gills JP, Sanders DR, editors. Corneal topography; the State of the Art. Thorofare, NJ: Slack Inc; 1995. pp. 89–103. [Google Scholar]
- 19.Sanchis-Gimeno JA, Lleo-Perez A, Casanova J, Alonso L, Rahhal SM. Inter-observer variability of central corneal thickness measurements using non-contact specular microscopy after laser in situ keratomileusis. Clin Exp Optom. 2004;87:15–8. doi: 10.1111/j.1444-0938.2004.tb03140.x. [DOI] [PubMed] [Google Scholar]
- 20.Kawana K, Tokunaga T, Miyata K, Okamoto F, Kiuchi T, Oshika T. Comparison of corneal thickness measurements using Orbscan II, non-contact specular microscopy and ultrasonic pachymetry in eyes after laser in situ keratomileusis. Br J Ophthalmol. 2004;88:466–8. doi: 10.1136/bjo.2003.030361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nishimura R, Negishi K, Saiki M, Arai H, Shimizu S, Toda I, et al. No forward shifting of posterior corneal surface in eyes undergoing LASIK. Ophthalmology. 2007;114:1104–10. doi: 10.1016/j.ophtha.2006.09.014. [DOI] [PubMed] [Google Scholar]
- 22.Quisling S, Sjoberg S, Zimmerman B, Goins K, Sutphin J. Comparison of Pentacam and Orbscan IIz on posterior curvature topography measurements in keratoconus eyes. Ophthalmology. 2006;113:1629–32. doi: 10.1016/j.ophtha.2006.03.046. [DOI] [PubMed] [Google Scholar]
- 23.Pallikaris IG, Kymionis GD, Astyrakakis NI. Corneal ectasia induced by laser in situ keratomileusis. J Cataract Refract Surg. 2001;27:1796–802. doi: 10.1016/s0886-3350(01)01090-2. [DOI] [PubMed] [Google Scholar]
- 24.Twa MD, Roberts C, Mahmoud AM, Chang JS. Response of the posterior corneal surface to laser in situ keratomileusis for myopia. J Cataract Refract Surg. 2005;31:61–71. doi: 10.1016/j.jcrs.2004.09.032. [DOI] [PubMed] [Google Scholar]
- 25.Wang Z, Chen J, Yang B. Posterior corneal surface topographic changes after laser in situ keratomileusis are related to residual corneal bed thickness. Ophthalmology. 1999;106:406–10. doi: 10.1016/S0161-6420(99)90083-0. [DOI] [PubMed] [Google Scholar]
- 26.Baek TM, Lee KH, Kagaya F, Tomidokoro A, Amano S, Oshika T. Factors affecting the forward shift of posterior corneal surface after laser in situ keratomileusis. Ophthalmology. 2001;108:317–20. doi: 10.1016/s0161-6420(00)00502-9. [DOI] [PubMed] [Google Scholar]
- 27.Cairns G, Ormonde SE, Gray T, Hadden OB, Morris T, Ring P, et al. Assessing the accuracy of Orbscan II post-LASIK: Apparent keratectasia is paradoxically associated with anterior chamber depth reduction in successful procedures. Clin Experiment Ophthalmol. 2005;33:147–52. doi: 10.1111/j.1442-9071.2005.00975.x. [DOI] [PubMed] [Google Scholar]
- 28.Du ZY, Zhang DY, Zheng Q, Chen Y, Guo H, Yin HM. An analysis of measurement error in Orbscan topography system. Zhonghua Yan Ke Za Zhi. 2003;39:36–40. [PubMed] [Google Scholar]
- 29.Lam AK, Chan R, Woo GC, Pang PC, Chiu R. Intra-observer and inter-observer repeatability of anterior eye segment analysis system (EAS-1000) in anterior chamber configuration. Ophthalmic Physiol Opt. 2002;22:552–9. doi: 10.1046/j.1475-1313.2002.00074.x. [DOI] [PubMed] [Google Scholar]


