Abstract
Aims:
There are few reports on 25-gauge transconjunctival sutureless vitrectomy (TSV) in cases of pseudophakic retinal detachment. We conducted this study to report the anatomic and functional outcomes of 25-gauge TSV in the treatment of primary pseudophakic retinal detachment (RD).
Design:
Prospective, interventional case series.
Materials and Methods:
Fifteen eyes of 15 patients with RD after cataract surgery with phacoemulsification were evaluated. Primary pseudophakic RDs with macular detachment and proliferative vitreoretinopathy Stage B or less were included in the study. Pars plana vitrectomy with the 25-gauge TSV system, perfluorocarbon liquid injection followed by air exchange, endolaser photocoagulation and sulfur hexafluoride gas (20%) injection were applied to all eyes.
Results:
Mean follow-up time was 9.2 months (range, six to 12 months). Retinal reattachment with a single operation was achieved in 93% of eyes and with additional surgery, the retina was reattached in 100% of eyes. Preoperative visual acuity was less than 20/200 in all eyes (range, hand motions to 20/400). Postoperative visual acuity was 20/40 or better in eight eyes (53%) and between 20/50 and 20/200 in seven eyes (47%). No severe hypotony was encountered and no sutures were required to close the scleral and conjunctival openings. Postoperative complications were macular pucker in one eye (7%) and cystoid macular edema in another eye (7%).
Conclusions:
Primary 25-gauge TSV system appears to be an effective and safe procedure in the treatment of uncomplicated pseudophakic RD.
Keywords: 25-gauge pars plana vitrectomy, pseudophakic retinal detachment, transconjunctival sutureless vitrectomy
Retinal detachment (RD) is one of the serious complications of cataract surgery that threatens visual acuity and occurs in approximately 0.4-1.0% of eyes after cataract surgery with phacoemulsification. 1,2,3 Scleral buckling surgery and primary pars plana vitrectomy (PPV) with or without scleral buckling are the most commonly used techniques in the treatment of pseudophakic RD. 4,5,6,7,8,9 The advent of new microsurgical instruments, wide-angle viewing apparatus and perfluorocarbon liquids have (PFCL) increased the scope of primary PPV in the treatment of pseudophakic RD.
The recent evolution in the PPV technique with minimal invasive surgery and faster patient recovery is 25-gauge transconjunctival sutureless vitrectomy (TSV). 10 Several authors have reported successful anatomic and visual outcomes with 25-gauge TSV in eyes with different vitreoretinal disorders. 11,12,13,14,15 However, there is limited experience in pseudophakic RD. The purpose of this study was to report the preliminary results of 25-gauge TSV in the management of primary pseudophakic RD.
Materials and Methods
In this prospective study, we evaluated the visual and anatomic outcomes of primary PPV with the 25-gauge TSV system in 15 eyes of 15 patients with pseudophakic RD between May 2004 and September 2005. Inclusion criteria were RD occurring after cataract extraction with phacoemulsification and posterior chamber intraocular lens (IOL) implantation; macular detachment; proliferative vitreoretinopathy (PVR) Grade A or B.16 Exclusion criteria were PVR greater than Grade B; anterior chamber IOL; presence of giant retinal tear; presence of posteriorly dislocated lens fragments; a history of any other intraocular surgery except cataract extraction. Eyes that had been operated due to traumatic and congenital cataracts were excluded as well. The possible merits and risks of the treatment were explained to the patients and an informed consent was obtained in accordance with the Helsinki Declaration prior to inclusion in the study.
Baseline preoperative data included age, sex, duration of macular detachment, best-corrected Snellen visual acuity, slit-lamp biomicroscopy examination, applanation tonometry and detailed fundus examination (using non-contact and contact lenses). Axial length measurements were obtained from the patients′ medical records.
All operations were performed by an experienced surgeon (AY) under local anesthesia. The microcannulae (DORC International, Zuidland, Holland) were inserted transconjunctivally with the help of the insertion trocars in the inferotemporal, superotemporal and superonasal quadrants. The overlying conjunctiva was pulled aside with forceps during the entrance of the insertion trocar in order to avoid the alignment between conjunctival and scleral incisions. The infusion cannula was placed in the inferotemporal quadrant and plugs were used to temporarily close the other entry sites. A cutting rate of 1500 cuts per min and a vacuum level of 500mmHg were used during PPV. The bottle height was set at 40cm. Peripheral vitreous was removed during PPV. Peripheral manipulations were performed by using wide-angle viewing system with scleral depression by an assistant. Following PPV, the infusion line was removed while the microcannula was held in place with forceps. A PFCL (perfluoro-n-octane) was then injected slowly up to the anterior break to flatten the retina. The infusion line was replaced and switched to air to perform a complete PFCL-air exchange. A viscoelastic solution (Sodium Hyaluronate 1%) was injected into the anterior chamber through a paracentesis to avoid air passage to the anterior chamber. Endolaser photocoagulation was applied around the retinal break(s) and to the 360° peripheral retina (three to four rows of burns posterior to the vitreous base) under air. Then, the superonasal microcannula was removed and sulfur hexafluoride gas (20%) was injected through the infusion line. After removing the superotemporal microcannula, the inferotemporal microcannula and infusion line were removed en bloc while injecting gas. The conjunctiva overlying the sclerotomy was slightly displaced to disrupt the alignment between both entry sites and an antibiotic and corticosteroid combination was injected into the subconjunctival space. The viscoelastic solution was left in the anterior chamber at the end of the operation. The prone position was maintained for five days postoperatively.
Patients were examined postoperatively at one day, one week, one month, three months, six months and every six months thereafter. Each postoperative examination included determination of best-corrected Snellen visual acuity, slit-lamp examination, applanation tonometry and fundus examination. Main outcome measures were: retinal reattachment rate, visual acuity, intraocular pressure (IOP) and intraoperative and postoperative complications.
Results
Of 15 patients, 10 were men and five were women. Mean age was 65 years (range, 42 to 78 years). Mean follow-up time was 9.2 months (range, six to 12 months). Preoperative characteristics, visual and anatomic outcomes of patients are shown in Table 1. Preoperative visual acuity was hand motions (HM) in 11 eyes (73%), 20/400 in three eyes (20%) and 20/800 (7%) in one eye. Mean duration of macular detachment was 5.9 days (range, one to 21 days). Anterior vitrectomy with sulcus-fixated IOL implantation had been performed in six eyes (40%) with posterior capsule rupture and vitreous loss complicating the phacoemulsification procedure. The remaining nine eyes (60%) had intact posterior capsule. Mean axial length was 24.5±2.3 mm and two eyes had pathologic myopia with an axial length of 29 and 30 mm. None of the eyes had had neodymium:YAG (Nd:YAG) laser capsulotomy.
Table 1.
Preoperative characteristics, visual and anatomic outcomes of patients
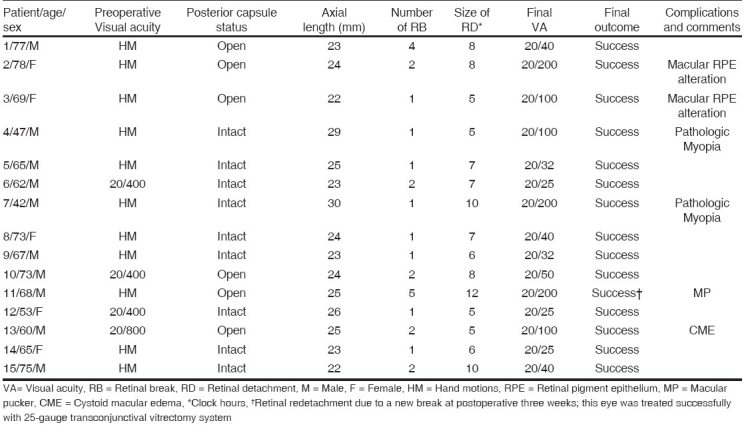
Single operation success was achieved in 14 (93%) of 15 eyes. In one eye, retinal redetachment due to a new break, which was observed at postoperative three weeks, was successfully treated with reoperation using the 25-gauge TSV system. Final visual acuity was better than preoperative visual acuity in all eyes. Postoperative visual acuity was 20/40 or better in eight eyes (53%) and between 20/50 and 20/200 in seven eyes (47%). Mean IOP was 10.4 mmHg (range, 7 to 16) before the operation, 11.8 mmHg (range, 8 to 20) at day one and 17.1 mmHg (range, 10 to 27) at month one after the operation.
No major intraoperative complications were encountered and conversion to conventional 20-gauge PPV was not required in any eye. Intraocular manipulations were easily performed and no sutures were required to close the scleral and conjunctival openings. No clinically significant intraocular inflammation was observed in the postoperative period due to the viscoelastic solution left in the anterior chamber. Postoperative complications were macular pucker in one eye (7%) and cystoid macular edema in another eye (7%).
Discussion
In this prospective study, retinal reattachment with a single operation using 25-gauge TSV was achieved in 93% of eyes with pseudophakic RD and with additional surgery, the retina was reattached in 100% of eyes. In the peer-reviewed literature (Medline search), only two eyes have been reported to be treated with 25-gauge TSV for pseudophakic RD. 13 These eyes have been successfully treated. Single operation and final anatomic success with primary 20-gauge PPV have been reported in 63 to 98% and 92 to 100% of eyes with pseudophakic RD, respectively. 5,6,8,9,17,18 In addition, our single operation and final success rates compare favorably with the anatomic outcomes of other surgical procedures used in the management of pseudophakic RD [Table 2].4,5,6,7,9,18,19,20,21,22,23 Therefore, our preliminary results suggest that 25-gauge TSV may be an alternative surgical procedure in the treatment of selected cases of pseudophakic RD.
Table 2.
Anatomic and visual outcomes of scleral buckle, pneumatic retinopexy and primary 20-gauge pars plana vitrectomy with or without 360° encirclement in the management of pseudophakic retinal detachment
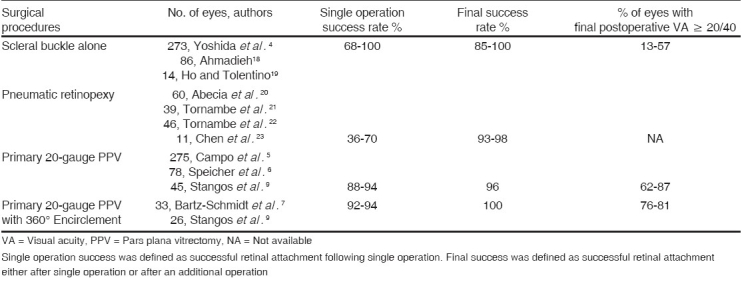
In the present study, visual acuity was 20/40 or better in eight eyes (53%) and between 20/50 and 20/200 in seven eyes (47%). In recent studies in which primary 20-gauge PPV was performed in the treatment of pseudophakic RD, visual acuity of 20/40 or better has been reported in 11 to 88% of eyes. 5,6,8,17,18 Our visual results are also comparable with the visual outcomes of other surgical procedures used in the management of pseudophakic RD [Table 2]. 4,5,6,7,9,18,19,20,21,22,23 There are several advantages of 25-gauge TSV over conventional 20-gauge PPV including less operation time, absence of suture-related irritation or local inflammatory reaction at the sclerotomy sites, absence of limbal stem cell damage due to conjunctival dissection, insignificant corneal surface and astigmatic changes in the early postoperative period, faster postoperative recovery and increased patient comfort. 11,13,15,24 In addition, the potential advantages of 20-gauge PPV without scleral buckling over conventional scleral buckling are expected to be the advantages of 25-gauge TSV. These are less operation time, accurate diagnosis of breaks, controlled drainage of subretinal fluid and no postoperative axial length changes. Therefore, if a primary PPV is appropriate in the management of pseudophakic RD, it may be logical to perform it with a 25-gauge TSV system.
Anterior or posterior capsular fibrosis, small capsulorrhexis, cortical remnants, poor pupillary dilation, small IOL diameter, formation of moisture droplets on the posterior surface of the IOL and optical aberrations secondary to IOL itself make the PPV more difficult in pseudophakic eyes, when compared with the primary RD. 25,26 The indication of 25-gauge TSV can be extended to pseudophakic RD and favorable outcomes may be obtained by paying special attention to the above issues.
Theoretical risks of the TSV system were postoperative vitreous incarceration leading to anterior vitreoretinal traction and late period retinal tear or detachment, endophthalmitis and hypotony. Postoperative RD (2.2 to 2.9%), relative hypotony with an IOP of 6 to 9 mmHg (16.9 to 22.8%), shallow choroidal detachment (3.8%), endophthalmitis have been reported in studies, in which 25-gauge TSV was performed for different vitreoretinal disorders. 11,13,14,15,27 Retinal redetachment (7%) due to a new break, macular pucker (7%) and cystoid macular edema (7%) were the postoperative complications encountered in our series. Despite peripheral vitreous removal which increases the risk of postoperative hypotony, an IOP of less than 8mmHg and choroidal detachment were not observed in any eye. This may be due to the injection of a viscoelastic solution (sodium hyaluronate 1% in our series) into the anterior chamber and also due to the use of intravitreal gas injection. The viscoelastic solution left in the anterior chamber at the end of the operation may have prevented postoperative hypotony by decreasing the aqueous outflow. In addition, Shimada et al. have reported that postoperative hypotony incidence is significantly lower in eyes that received intraocular fluid air/gas exchange than the eyes that did not. 12 Residual peripheral vitreous, which is pushed towards the sclerotomies by intravitreal gas may serve as a plug and prevent leakage, even in eyes with peripheral vitreous removal. The primary limitations of this study are the small number of patients, selection of cases without severe PVR and lack of comparison with other surgical procedures used in the management of pseudophakic RD. In addition, we did not measure the surgical time to compare 25-gauge TSV with 20-gauge PPV. In conclusion, primary 25-gauge TSV system appears to be effective and safe in the management of uncomplicated pseudophakic RD. Faster postoperative recovery and increased patient comfort make this surgical procedure a good alternative to other procedures used in the management of pseudophakic RD. Further studies comparing the 25-gauge TSV system to other surgical procedures with a large number of patients and long follow-up are required.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Haddad WM, Monin C, Morel C, Larricart P, Quesnot S, Ameline B, et al. Retinal detachment after phacoemulsification: A study of 114 cases. Am J Ophthalmol. 2002;133:630–8. doi: 10.1016/s0002-9394(02)01347-8. [DOI] [PubMed] [Google Scholar]
- 2.Javitt JC, Tielsch JM, Canner JK, Kolb MM, Sommer A, Steinberg EP. National outcomes of cataract extraction. Increased risk of retinal complications associated with Nd:YAG laser capsulotomy. The Cataract Patient Outcomes Research Team. Ophthalmology. 1992;99:1487–97. doi: 10.1016/s0161-6420(92)31775-0. [DOI] [PubMed] [Google Scholar]
- 3.Olsen G, Olson RJ. Update on a long-term, prospective study of capsulotomy and retinal detachment rates after cataract surgery. J Cataract Refract Surg. 2000;26:1017–21. doi: 10.1016/s0886-3350(00)00304-7. [DOI] [PubMed] [Google Scholar]
- 4.Yoshida A, Ogasawara H, Jalkh AE, Sanders RJ, McMeel JW, Schepens CL. Retinal detachment after cataract surgery. Surgical results. Ophthalmology. 1992;99:460–5. doi: 10.1016/s0161-6420(92)31952-9. [DOI] [PubMed] [Google Scholar]
- 5.Campo RV, Sipperley JO, Sneed SR, Park DW, Dugel PU, Jacobsen J, et al. Pars plana vitrectomy without scleral buckle for pseudophakic retinal detachments. Ophthalmology. 1999;106:1811–6. doi: 10.1016/S0161-6420(99)90353-6. [DOI] [PubMed] [Google Scholar]
- 6.Speicher MA, Fu AD, Martin JP, Von Fricken MA. Primary vitrectomy alone for repair of retinal detachments following cataract surgery. Retina. 2000;20:459–64. doi: 10.1097/00006982-200009000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Bartz-Schmidt KU, Kirchhof B, Heimann K. Primary vitrectomy for pseudophakic retinal detachment. Br J Ophthalmol. 1996;80:346–9. doi: 10.1136/bjo.80.4.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lois N, Wong D. Pseudophakic retinal detachment. Surv Ophthalmol. 2003;48:467–87. doi: 10.1016/s0039-6257(03)00083-3. [DOI] [PubMed] [Google Scholar]
- 9.Stangos AN, Petropoulos IK, Brozou CG, Kapetanios AD, Whatham A, Pournaras CJ. Pars-plana vitrectomy alone vs vitrectomy with scleral buckling for primary rhegmatogenous pseudophakic retinal detachment. Am J Ophthalmol. 2004;138:952–8. doi: 10.1016/j.ajo.2004.06.086. [DOI] [PubMed] [Google Scholar]
- 10.Fujii GY, De Juan E, Jr, Humayun MS, Pieramici DJ, Chang TS, Awh C, et al. A new 25-gauge instrument system for transconjunctival sutureless vitrectomy surgery. Ophthalmology. 2002;109:1807–13. doi: 10.1016/s0161-6420(02)01179-x. [DOI] [PubMed] [Google Scholar]
- 11.Fujii GY, De Juan R, Jr, Humayun MS, Chang TS, Pieramici DJ, Barnes A, et al. Initial experience using the transconjunctival sutureless vitrectomy system for vitreoretinal surgery. Ophthalmology. 2002;109:1814–20. doi: 10.1016/s0161-6420(02)01119-3. [DOI] [PubMed] [Google Scholar]
- 12.Shimada H, Nakashizuka H, Mori R, Mizutani Y. Expanded indications for 25-gauge transconjunctival vitrectomy. Jpn J Ophthalmol. 2005;49:397–401. doi: 10.1007/s10384-004-0214-4. [DOI] [PubMed] [Google Scholar]
- 13.Lakhanpal RR, Humayun MS, de Juan E, Jr, Lim JI, Chong LP, Chang TS, et al. Outcomes of 140 consecutive cases of 25-gauge transconjunctival surgery for posterior segment disease. Ophthalmology. 2005;112:817–24. doi: 10.1016/j.ophtha.2004.11.053. [DOI] [PubMed] [Google Scholar]
- 14.Ibarra MS, Hermel M, Prenner JL, Hassan TS. Longer-term outcomes of transconjunctival sutureless 25-gauge vitrectomy. Am J Ophthalmol. 2005;139:831–6. doi: 10.1016/j.ajo.2004.12.002. [DOI] [PubMed] [Google Scholar]
- 15.Yanyali A, Celik E, Horozoglu F, Oner S, Nohutcu AF. 25-Gauge transconjunctival sutureless pars plana vitrectomy. Eur J Ophthalmol. 2006;16:141–7. doi: 10.1177/112067210601600123. [DOI] [PubMed] [Google Scholar]
- 16.The classification of retinal detachment with proliferative vitreoretinopathy . Ophthalmology. 1983;90:121–5. doi: 10.1016/s0161-6420(83)34588-7. [DOI] [PubMed] [Google Scholar]
- 17.Brazitikos PD, Androudi S, Christen WG, Stangos NT. Primary pars plana vitrectomy versus scleral buckle surgery for the treatment of pseudophakic retinal detachment: A randomized clinical trial. Retina. 2005;25:957–64. doi: 10.1097/00006982-200512000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Ahmadieh H, Moradian S, Faghihi H, Parvaresh MM, Ghanbari H, Mehryar M, et al. Anatomic and visual outcomes of scleral buckling versus primary vitrectomy in pseudophakic and aphakic retinal detachment: six-month follow-up results of a single operation--report no. 1. Ophthalmology. 2005;112:1421, 9. doi: 10.1016/j.ophtha.2005.02.018. [DOI] [PubMed] [Google Scholar]
- 19.Ho PC, Tolentino FI. Retinal detachment following extracapsular cataract extraction and posterior chamber intraocular lens implantation. Br J Ophthalmol. 1985;69:650–3. doi: 10.1136/bjo.69.9.650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abecia E, Pinilla I, Olivan JM, Larrosa JM, Polo V, Honrubia FM. Anatomic results and complications in a long-term follow-up of pneumatic retinopexy cases. Retina. 2000;20:156–61. [PubMed] [Google Scholar]
- 21.Tornambe PE, Hilton GF, Brinton DA, Flood TP, Green S, Grizzard WS, et al. Pneumatic retinopexy. A two-year follow-up study of the multicenter clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology. 1991;98:1115–23. [PubMed] [Google Scholar]
- 22.Tornambe PE, Hilton GF The Retinal Detachment Study Group. Pneumatic retinopexy. A multicenter randomized controlled clinical trial comparing pneumatic retinopexy with scleral buckling. Ophthalmology. 1989;96:772, 84. doi: 10.1016/s0161-6420(89)32820-x. [DOI] [PubMed] [Google Scholar]
- 23.Chen JC, Robertson JE, Coonan P, Blodi CF, Klein ML, Watzke RC, et al. Results and complications of pneumatic retinopexy. Ophthalmology. 1988;95:601–6. doi: 10.1016/s0161-6420(88)33134-9. [DOI] [PubMed] [Google Scholar]
- 24.Yanyali A, Celik E, Horozoglu F, Nohutcu AF. Corneal topographic changes after transconjunctival (25-gauge) sutureless vitrectomy. Am J Ophthalmol. 2005;140:939–41. doi: 10.1016/j.ajo.2005.05.042. [DOI] [PubMed] [Google Scholar]
- 25.Eaton AM, Jaffe GJ, McCuen BW, 2nd, Mincey GJ. Condensation on the posterior surface of silicone intraocular lenses during fluid-air exchange. Ophthalmology. 1995;102:733–6. doi: 10.1016/s0161-6420(95)30961-x. [DOI] [PubMed] [Google Scholar]
- 26.Yoshida A, Ogasawara H, Jalkh AE, Sanders RJ, McMeel JW, Schepens CL. Retinal detachment after cataract surgery. Predisposing factors. Ophthalmology. 1992;99:453–9. doi: 10.1016/s0161-6420(92)31953-0. [DOI] [PubMed] [Google Scholar]
- 27.Taylor SR, Avlward GW. Endophthalmitis following 25-gauge vitrectomy. Eye. 2005;19:1228–9. doi: 10.1038/sj.eye.6701737. [DOI] [PubMed] [Google Scholar]


