Abstract
Aim:
To study the indications, technique and diagnostic utility of helical computed tomographic dacryocystography (CTDCG).
Materials and Methods:
Retrospective analysis of 13 patients who underwent CTDCG with subsequent surgical intervention, during the period January 2003 to December 2005, was done. Axial plain computed tomography (CT) scan was performed, followed by administration of water-soluble contrast in the conjunctival cul de sac or by cannulation of the lacrimal passages. Thin-slice helical CT with two-dimensional (2D) and three-dimensional (3D) coronal and sagittal reformation was done.
Results:
Four patients were males and 9 were females. Age range was 5 to 62 years. Seven patients presented with watering and 6 patients with a medial canthal mass. Three patients had history of trauma. CTDCG was performed by instillation technique in 10 patients and by cannulation in 3 patients. CTDCG showed mass lesion displacing the sac in 5 cases, nasolacrimal duct obstruction in 6 cases and mucocele in 2 cases. Based on the findings on CTDCG, 5 patients underwent mass excision, 7 underwent dacryocystorhinostomy and 1 patient underwent primary silicone tube intubation.
Conclusion:
Helical CTDCG is a safe and useful diagnostic tool for the lacrimal surgeon. Instillation technique is a physiological and convenient method, and cannulation is needed only in cases where adequate visualization is not achieved.
Keywords: Computed tomography dacryocystography, nonionic contrast medium
Imaging of the lacrimal system is often required in the assessment of complex lacrimal conditions such as in patients with medial canthal tumors, mid-face trauma or following sinus or lacrimal surgery. Various imaging modalities, including conventional dacryocystography (DCG), computed tomography (CT), magnetic resonance imaging (MRI) and nuclear scintigraphy, are available – each with its own advantages and limitations.1
Conventional DCG by itself is capable of demonstrating the patency as well as intrinsic pathology of lacrimal drainage system. However, it is limited in its ability to offer information extrinsic to the nasolacrimal drainage system and provides limited soft tissue detail.2
Although dacryoscintigraphy, using Technetium-99m pertechnetate solution, is a physiological study of the lacrimal drainage system, it is limited by suboptimal resolution and lack of easy availability.1
MRI scan may show the lacrimal sac as clearly as CT scan, but it does not show the canaliculi and has the same limitations as a standard CT scan in viewing canalicular pathology. Injection of gadolinium is needed to visualize the canaliculi.2 Though it can be performed without exposure to ionizing radiation or contrast by using saline for filling the lacrimal system, the test is expensive, gives poor bony details, has a long acquisition time with image degradation in case of patient movement and is not recommended as a routine examination.1,2
Plain or intravenous (IV) enhanced CT does not image the superior, inferior and the common canaliculi. They can be identified by placement of topical contrast medium either into the conjunctival sac or by cannulation of the punctum. High- resolution thin sections (1 to 2.5 mm slice thickness) CT imaging in the axial and/ or coronal plane is helpful in assessing those structures intimately associated with the nasolacrimal drainage system.2 By combining CT with DCG, the relationship between the nasolacrimal drainage system and the surrounding soft tissue and bony structures can be clearly demonstrated. It defines the lacrimal system anatomy, facilitates preoperative planning and intraoperative decision making.3
CTDCG scores better in displaying the smaller components of the lacrimal system, the superior, inferior and common canaliculi, than MRDCG.4 It is also more sensitive than MRDCG in distinguishing high-grade stenosis from total obstruction of the nasolacrimal drainage system.5
The increasing capabilities of thin-slice helical CT, with two- dimensional (2D) and three-dimensional (3D) reconstruction and shorter acquisition time, now offer excellent imaging resolution and patient compliance.
CTDCG technique was first described in detail in 2002 by Freitag et al.1 Since then, only limited reports of this technique have been described. Only few studies of CTDCG have been reported using dye instillation technique instead of the cannulation technique.4,6,7 To the best of our knowledge, no such study has been reported from India. We studied the indications, technique and diagnostic utility of helical CTDCG.
Materials and Methods
Retrospective analysis of 13 patients who underwent CTDCG during the period January 2003 to December 2005 at a tertiary referral center was done. Detailed history including history of previous lacrimal surgery, trauma or sinus disease was elicited. Lacrimal system evaluation, including position and appearance of the punctum and lid, tear meniscus height evaluation, presence or absence of medial canthal mass, regurgitation on pressure on the sac or canaliculus, dye disappearance test and syringing, was performed. CTDCG was performed in patients in whom there was uncertainty as to the cause of epiphora on clinical examination or in the presence of medial canthal mass. Only those patients who underwent surgical intervention after CTDCG were included in the study to enable correlation between the CTDCG and intraoperative findings. Patients with known allergy to iodine or contrast media were precluded from undergoing the study.
Technique
The study was performed on a Siemens Esprit helical CT scanner. Three hours starvation was advised to patients requiring administration of IV contrast for evaluation of medial canthal mass. With the patient in supine position, 3-mm thick plain axial helical CT scan (4.5 millimeter table feed; 1.5 pitch) of the paranasal sinus and orbit was taken from the hard palate to the roof of the orbit to look at the bony canal, calcification or dacryolith.
CTDCG was performed by administration of contrast by cannulation or instillation in the conjunctival cul de sac. Contrast media used was iohexol (Omnipaque, G E Healthcare Systems, 300 mg iodine /ml). It is a low-osmolar, water-soluble, nonionic, iodinated contrast. It was used in 1:1 dilution, diluted with distilled water.
When the procedure was performed by instillation of contrast in the conjunctival cul de sac, one to two drops per minute, per eye, were instilled for 5 min, followed by CT scanning.
Cannulation was performed by an ophthalmologist only when the drop method failed to adequately demonstrate the lacrimal drainage system. When CTDCG was performed by cannulation, topical 0.5% proparacaine was instilled. Pre-DCG irrigation and expression of the lacrimal sac was done to flush out accumulated secretions within the duct system, which may lead to interpretive difficulties, including improper estimation of the size of the lacrimal sac or misdiagnosis of obstruction proximal to a stenosing lesion due to the retained secretions.5 Approximately 2 mm of the radiopaque contrast material was drawn into a syringe, connected to a 26 gauge lacrimal cannula with a plastic hub and tubing and the system was cleared of any air bubbles. In bilateral imaging, two cannulae and tubing with a ′Y′ connector were used. The inferior punctum was dilated with a lacrimal dilator. The lacrimal cannula was then placed into the inferior canaliculus just far enough to remain stable during the study, and the tubing was taped to the patient′s face. Care was taken to avoid placement of the cannula far into the inferior canaliculus, which may create artifacts.5 Then, 0.5 to 1.0 ml of contrast medium was injected each side. IV contrast was used in cases with medial canthal mass.
The patient was scanned in a supine position for axial imaging, and prone position for direct coronal imaging. Direct coronal imaging was done only when patient movement during the axial scanning resulted in poor quality of reformation. Two- millimeter thick helical CT with 2-mm table feed (one pitch), 130 kV, 110 mA and FOV 150 to 180 was performed with a reconstruction interval of 1 mm. The data acquired in the axial plane was reformatted into 3D and 2D coronal and oblique sagittal planes along the long axis of the lacrimal drainage apparatus.
Results
Four patients were male and nine were female. Age range was 5 to 62 years (median age 26 years). Seven patients presented with watering and six with medial canthal masses. Of the patients with medial canthal mass, two patients had firm mass and four patients had cystic mass [Table 1].
Table 1.
Profile of patients who underwent computed tomographic dacryocystography
Syringing was patent in 4 of these 6 patients with a medial canthal mass. In the 7 cases without a medial canthal mass, syringing was patent in 2. Three patients had history of trauma, of which 1 patient (patient no. 5) had sac surgery twice elsewhere, with persistence of symptoms. Ten patients underwent CTDCG with the drop technique, with contrast instillation in the conjunctival cul de sac. Three patients underwent cannulation and injection of contrast into the lacrimal drainage system, since the instillation technique failed to demonstrate the dye in the lacrimal passages in these patients. Bilateral DCG was performed in 1 of the 3 patients evaluated by cannulation technique and in 7 of the 10 patients who underwent instillation technique CTDCG. High-quality images with sharp delineation of the lacrimal drainage system were obtained in all cases, including the normal passages [Fig. 1]. Patient no. 2 presented with a medial canthal mass, and CTDCG demonstrated smooth displacement of the canaliculi due to the mass and a patent lacrimal drainage system [Fig. 2] CTDCG showed mass lesion displacing the sac in 5 cases, nasolacrimal duct obstruction in 6 cases and mucocele in 2 cases [Table 2]. CTDCG in patient no. 5 showed fracture of inferior orbital rim with displaced fragment of bone and also fractures involving maxillary sinus, nasal and zygomatic bones. The sac was distended and laterally displaced with no flow into the nasolacrimal duct (NLD) [Fig. 3]. In patient no. 8, CTDCG showed ill-defined soft tissue thickening in the medial canthal area with a hyperdense lesion suggestive of foreign body or bony fragment. There was irregular opacification of the sac with proximal NLD obstruction [Fig. 4].
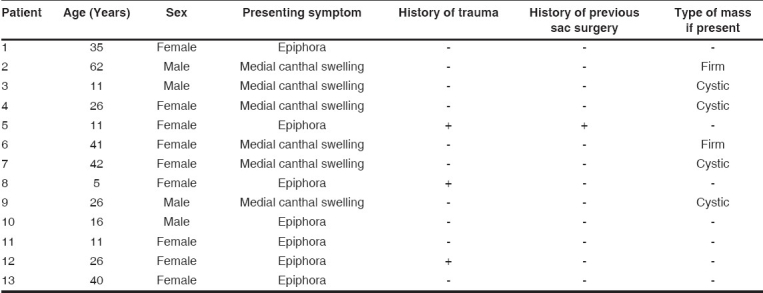
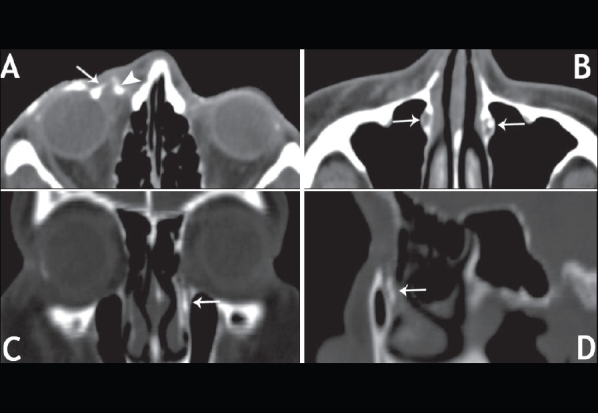
Figure 1.
Computed tomographic dacryocystography demonstrating normal lacrimal drainage system [(A - axial scan) and (B - reformatted coronal scan) showing lacrimal sac filled with contrast (arrow); (C - reformatted sagittal) showing contrast-filled sac (arrowhead) and contrast in the nasolacrimal duct (arrow); (D - reformatted coronal scan) showing contrast in superior and inferior canaliculi (arrow), sac (arrowhead) and nasolacrimal duct (curved arrow)]
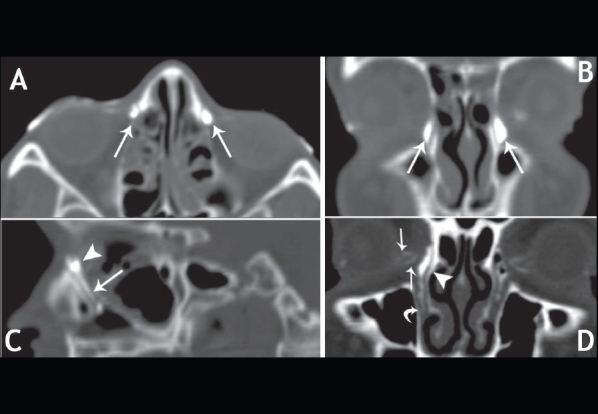
Figure 2.
Computed tomographic dacryocystography of patient no. 2 showing (A) contrast in superior and inferior canaliculi (white arrow), compressed and medially displaced contrast-filled sac (black arrow) and medial canthal mass (black arrowhead); (B) showing contrast in the inferior meatus (arrow)
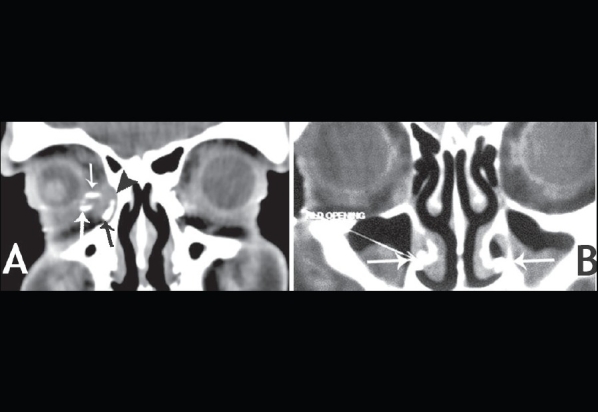
Table 2.
Findings on clinical and computed tomographic dacryocystography evaluation of lacrimal drainage system
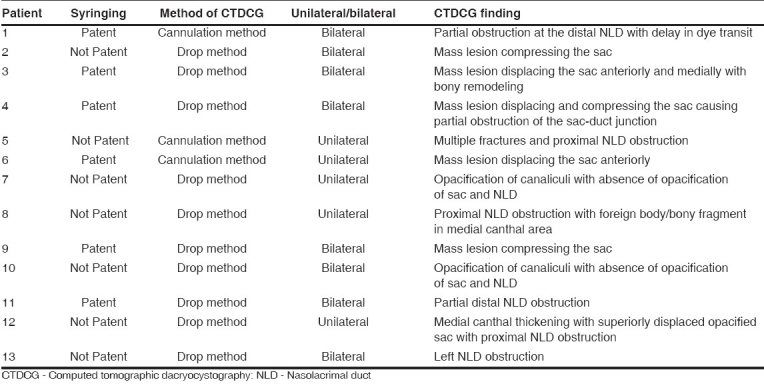
Figure 3.

(A) showing photograph of patient no. 5; (B) three-dimensional CT scan showing multiple facial fractures (black arrows); (C) Computed tomographic dacryocystography showing proximal nasolacrimal duct obstruction with contrast in superior and inferior canaliculi (upper arrow), sac (lower arrow) and absence of contrast in the nasolacrimal duct
Figure 4.
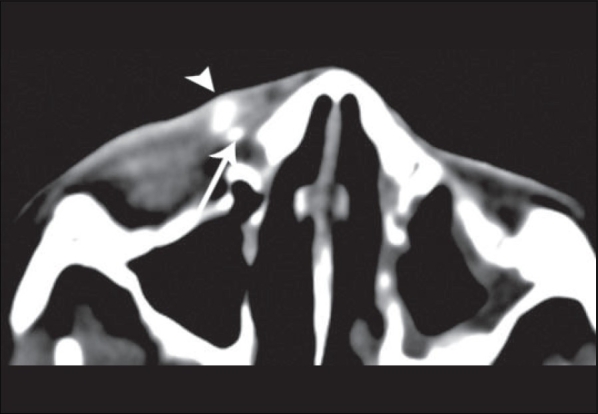
Computed tomographic dacryocystography of patient no. 8 showing superiorly displaced opacified lacrimal sac (arrowhead) and foreign body/ bony fragment in medial canthal area (arrow)
Five patients underwent mass excision by medial orbitotomy, and seven underwent dacryocystorhinostomy (DCR). One patient (patient no. 11) with partial NLD obstruction on CTDCG with findings of delayed dye appearance into the inferior meatus underwent primary silicone tube intubation. Histopathology of the excised mass revealed inclusion cyst in two patients, and one each had apocrine cyst, benign reactive hyperplasia and lymphoma [Table 3].
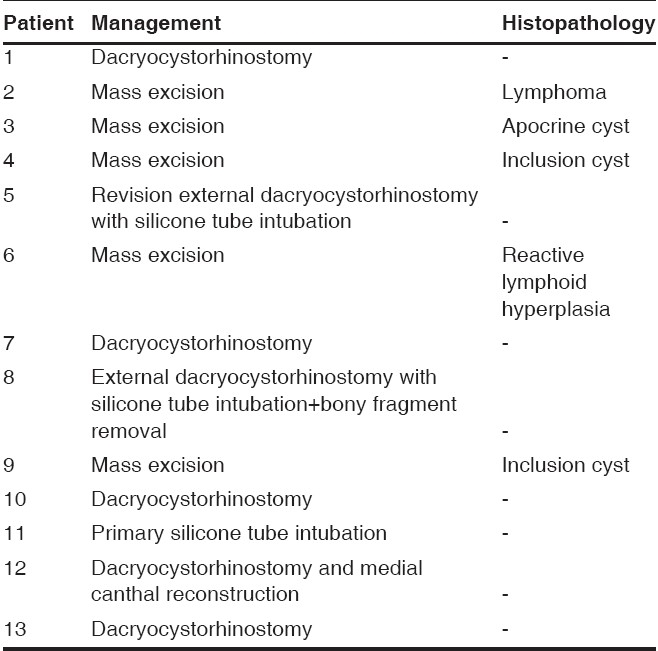
Table 3.
Surgical management of patients who underwent computed tomographic dacryocystography and findings on histopathology of mass lesions excised
Discussion
By combining CT scan with DCG, the relationship between the nasolacrimal drainage system and the surrounding soft tissue and bony structures is delineated better. Performing the CT scan prior to use of lacrimal contrast is important in delineating calcifications such as dacryoliths and for accurate evaluation of bony injuries and is recommended in all cases.
CTDCG is indicated in investigating patients with epiphora after the clinical examination suggests a mechanical obstruction. It helps to (l) describe the level of the obstruction; (2) evaluate whether the obstruction is complete or incomplete, intrinsic or extrinsic to the duct and (3) determine the cause of the obstruction. The suspected obstruction may be associated with various clinical conditions, including congenital obstructions, supernumerary canaliculi, lacrimal fistula or diverticula, concretions (dacryoliths), neoplastic or inflammatory processes or post-treatment changes.5 CTDCG offers maximum information to allow the appropriate choice of treatment in these cases. In our study, seven patients presented with watering and without a medial canthal mass. The cause and exact site of obstruction was clearly identified with the help of CTDCG in these patients. The DCG findings correlated well with intraoperative findings.
In patients with failed DCR, the location of the bony opening, soft tissue scarring, bony regrowth, secondary stenosis of the canaliculi,8 synechia between the ostium and nasal septum can be imaged by CTDCG.5 Similarly, anatomic variations in the nasal cavity, turbinates or nasal septum and the possibility of encountering ethmoid sinus air cells during DCR can be noted. CTDCG best shows the relationship of surgical clips, sutures and fixation plates to the nasolacrimal sac or the osteotomy site. Only one patient in our study had history of DCR in the past (patient no. 5). This patient was found to have a residual sac with proximal NLD obstruction along with facial fractures on CTDCG [Fig. 3]. She underwent a successful DCR surgery with silicone tube intubation.
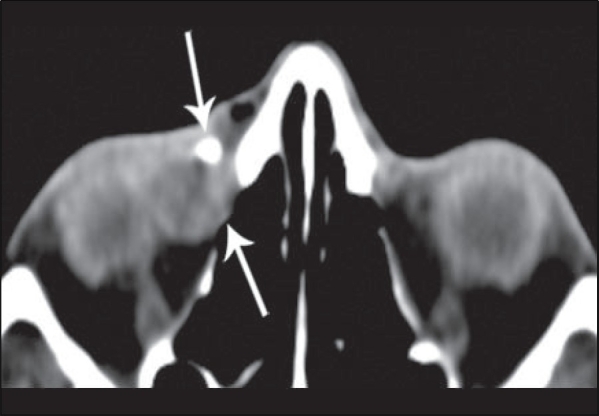
In patients with lacrimal outflow symptoms after trauma, CTDCG offers additional benefits of more exact localization of the lacrimal drainage system fractures, bone displacements, location of previously placed miniplates, wire or silastic sheets. In our study, three patients had history of trauma, of which one patient (patient no. 5) had sac surgery twice elsewhere with persistence of symptoms. CTDCG in this patient showed multiple facial fractures with proximal NLD obstruction. Another patient with history of trauma showed proximal NLD obstruction with suspected medial canthal foreign body or bony fragment on CTDCG (patient no. 8). She was found to have bony fragment in the medial canthal area, which was removed intraoperatively during DCR. Patient no. 12 with history of trauma showed medial canthal thickening with superiorly displaced opacified sac and proximal NLD obstruction on CTDCG [Fig. 5]. She underwent successful DCR with medial canthal reconstruction.
Figure 5.
Computed tomographic dacryocystography of patient no. 12 showing superiorly displaced opacified lacrimal sac on the right side (arrowhead) with medial canthal thickening on axial section (A); arrow showing contrast in the canaliculus; (B - axial scan), (C - reformatted coronal scan) and (D - reformatted sagittal scan) showing contrast in the nasolacrimal duct in the patent left side and absence of contrast in the right nasolacrimal duct (arrow)
All patients presenting with an inferomedial orbital mass lesion are candidates for CTDCG. The information about the exact relationship of the mass to the sac, the possible nature of the mass and secondary effects on the lacrimal system offered by CTDCG helps in making treatment decisions. In our study, six patients presented with medial canthal masses. The possible nature, location, extent and secondary effects on the sac and canaliculi were well seen on CTDCG. Five patients had mass excision and one underwent DCR for lacrimal sac mucocele [Fig. 6]. On histopathology of the excised mass, findings suggested inclusion cyst (two patients); and apocrine cyst, benign reactive hyperplasia and lymphoma (one patient each).
Figure 6.
Computed tomographic dacryocystography of patient no. 7 showing contrast in the conjunctiva (upper arrow) and non-opacified enlarged sac (lower arrow)
The etiology of functional nasolacrimal duct obstruction (FNLDO) and its relation to sinonasal disease has also been better appreciated on a CTDCG.5 None of the patients in our study had associated sinusitis or nasal pathology, unlike the landmark study by Freitag et al.1 where 50% of the studied patients had some degree of sinus disease.
CTDCG is contraindicated in pregnant women and in patients with a known allergy to iodine. Also, we do not recommend CTDCG in cases with acute dacryocystitis, due to reasons related to patient comfort in undergoing the procedure as also the extensive soft tissue edema and possible masking of important diagnostic radiological signs. Children and uncooperative patients require sedation for this procedure. Four of the patients in our study were children, the youngest being 5 years of age (patient no. 8). With appropriate preparation, all of them underwent successful CTDCG by instillation method, except one patient (Patient no. 3) who needed cannulation and underwent the same without any complications.
Though oil-based contrast media fill the NLDS better, are less irritating, are undiluted with tears and offer better opacification, they have potential disadvantages. Extravasation can lead to severe granulomatous inflammation,5 especially in post-traumatic and post-inflammatory cases. Their higher viscosity makes instillation in the conjunctiva impractical. Residual fluid in the sac causes oil-based contrast media to form globules, giving a false impression of a polycystic sac or diverticula.5 Water-soluble contrast is safe and effective;5 and hence we used iohexal, a water-soluble dye, in our study. The patient may complain of slight dryness,6 burning or irritation of the eye due to contrast, which is short lived.5 None of our patients had such complaints. The contrast has an unpleasant taste but is safe to swallow.5
Instillation of contrast in the conjunctiva gives better patient comfort, tolerance, acceptance and ease of procedure, is more physiological and avoids artifacts due to the cannula placement. It also eliminates risk of iatrogenic injury from cannulation or injection of contrast medium and does not require trained personnel for cannulation. It can be performed in children without sedation. In our study, 10 of the 13 patients underwent CTDCG by instillation technique, cannulation being needed only in 3 patients due to inadequate visualization of contrast in the lacrimal drainage system following instillation study.
In a patent system, the contrast medium will immediately drain from lacrimal sac into the nose and nasopharynx. A delay in dye appearance is interpreted as partial obstruction and was seen in two patients (patient no. 1 and patient no. 11). Both underwent successful DCR operation.
Initial or subsequent cannulation of the superior punctum may be appropriate when there is difficulty with cannulation of the inferior punctum or when further assessment is required following the initial injection through the inferior punctum. None of our patients needed cannulation of the superior punctum.
Routine bilateral DCG may be justified by the relative ease of the procedure; the lack of additional radiation, since the contralateral orbit is frequently included in the field of study; and the frequent finding of abnormalities in the clinically ′asymptomatic′ side.5 Bilateral simultaneous injection allows comparative study of flow characteristics through the nasolacrimal duct system. However, bilateral DCG for unilateral pathology may cause iatrogenic insult to the non-involved tear duct system during cannulation.5 Bilateral studies were performed in 7 of 10 cases of instillation technique and 1 of 3 cases of cannulation technique. We did not find any abnormalities on imaging lacrimal drainage systems where symptoms of epiphora or a medial canthal mass were not associated. We feel that performance of bilateral CTDCG as a routine in patients with unilateral symptoms must be avoided – particularly if cannulation, with its attendant risks, is needed.
Helical CT has several advantages over conventional CT. The volume data acquisition with thin (less than 1 mm) overlapping sections with helical CT allows superior quality of coronal, sagittal [Fig. 7] and 3D reconstruction, which obviates the need for direct coronal scanning, thereby reducing the total radiation exposure and scanning time.4 Also, direct coronal scanning requires neck hyperextension in prone position, and there may be artifacts from dental fillings, which are avoided by coronal reformation.4 The shorter acquisition time (less than 20 to 30 sec) with helical CT allows the study to be done in children without sedation, ensures patient cooperation and avoids image degradation due to patient movement.4,7 Reconstruction of 3D images using a connectivity algorithm can be obtained, and the lacrimal system can be viewed in relationship to the adjacent orbital and facial skeleton [Fig. 8].1,7
Figure 7.
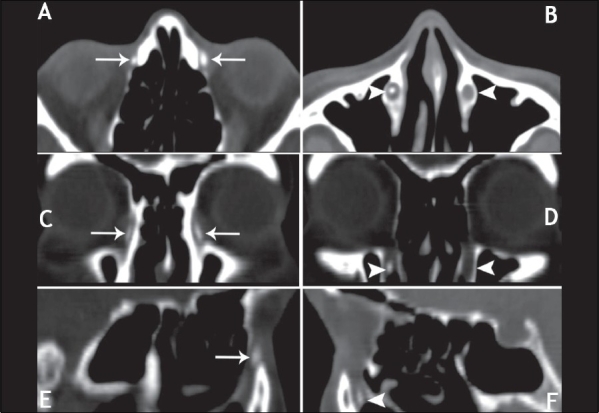
Computed tomographic dacryocystography of patient no. 13 showing lacrimal sac filled with contrast (arrow) in (A - axial scan), (C - reformatted coronal scan) and (E - reformatted sagittal scan); and (B - axial scan), (D - reformatted coronal scan) and (F - reformatted sagittal scan) showing presence of contrast in the patent right nasolacrimal duct and absence of contrast in the nasolacrimal duct on the left side (arrowhead)
Figure 8.
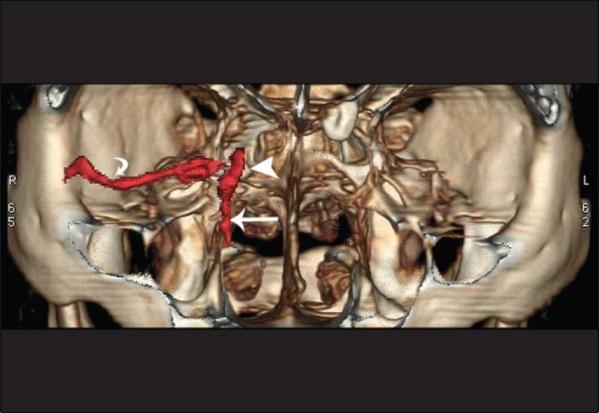
Three-dimensional helical computed tomographic dacryocystography showing lacrimal drainage system (red) and its relationship to the surrounding facial skeleton. Contrast in the conjunctival cul de sac (curved arrow), in the lacrimal sac (arrowhead) and in the nasolacrimal duct (arrow)
We believe that CTDCG is useful in the assessment of complex lacrimal problems such as in patients with medial canthal tumors, mid-face trauma or following sinus or lacrimal surgery.2 Instillation technique is noninvasive, obviating the need for cannulation of the lacrimal passage and its attendant risks, thereby enhancing the safety and usefulness of this investigative modality.
Conclusion
CTDCG is a useful diagnostic tool in clinically challenging cases of lacrimal system abnormality. It defines the lacrimal system anatomy accurately, facilitates preoperative planning and intraoperative decision-making. Instillation of nonionic, water- soluble contrast in the conjunctival cul de sac is a physiologic, simple and sensitive method to evaluate lacrimal obstruction. We propose it as a first step, catheterization being used only in the absence of opacification after instillation. Helical CT with its volume data acquisition capability, shorter acquisition time, with high-resolution coronal, sagittal and 3D reconstruction offers advantage over conventional CT scan.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Freitag SK, Woog JJ, Kousoubris PD, Curtin HD. Helical computed tomographic dacryocystography with three-dimensional reconstruction: A new view of the lacrimal drainage system. Ophthal Plast Reconstr Surg. 2002;18:121–32. doi: 10.1097/00002341-200203000-00006. [DOI] [PubMed] [Google Scholar]
- 2.Hurwitz JJ, Edward Kassel EE, Jaffer N. The Lacrimal System. In: Hurwitz JJ, editor. Computed Tomography and Combined CT-Dacryocystography (CT-DCG) New York: Raven Press; 1996. pp. 83–5. [Google Scholar]
- 3.Ashenhurst M, Jaffer N, Hurwitz JJ, Corin SM. Combined computed tomography and dacryocystography for complex lacrimal problems. Can J Ophthalmol. 1991;26:27–31. [PubMed] [Google Scholar]
- 4.Caldemeyer KS, Stockberger SM, Broderick LS. Topical contrast-enhanced CT and MR dacryocystography: Imaging the lacrimal drainage apparatus of healthy volunteers. AJR Am J Roentgenol. 1998;171:1501–4. doi: 10.2214/ajr.171.6.9843278. [DOI] [PubMed] [Google Scholar]
- 5.Kassel EE, Schatz CJ. Lacrimal apparatus. In: Som PM, Curtin HD, editors. Head and Neck Imaging. 4th ed. pp. 655–733. [Google Scholar]
- 6.Zinreich SJ, Miller NR, Freeman N, Glorioso W, Rosenbaum AE. Computed tomographic dacryocystography using topical contrast media for lacrimal system visualization. Orbit. 1990;9:79–87. [Google Scholar]
- 7.Moran CC, Buckwalter K, Caldemeyer KS, Smith RR. Helical CT with topical water-soluble contrast media for imaging of the lacrimal drainage apparatus. AJR Am J Roentgenol. 1995;164:995–6. doi: 10.2214/ajr.164.4.7726064. [DOI] [PubMed] [Google Scholar]
- 8.Gokcek A, Argin MA, Altintas AK. Comparison of failed and successful dacryocystorhinostomy by using computed tomographic dacryocystography findings. Eur J Ophthalmol. 2005;15:523–9. [PubMed] [Google Scholar]


