Abstract
Purpose:
To compare the prevalence of refractive errors and factors associated with spectacle use in a rural and urban south Indian population.
Materials and Methods:
Four thousand eight hundred subjects (age >39 years) each from rural and urban Tamil Nadu were enumerated for a population-based study. All participants underwent a complete ophthalmic evaluation including best-corrected visual acuity (BCVA), objective and subjective refraction. Out of 3924 rural responders 63.91% and out of 3850 urban responders 81.64% were phakic in the right eye with BCVA of 20/40 or better and were included in the study. Association of spectacle use and refractive errors with different parameters were analysed using logistic regression.
Statistical Analysis:
Chi square, t test, Chi square for trend and Pearson′s correlation coefficient were used for analysis.
Results:
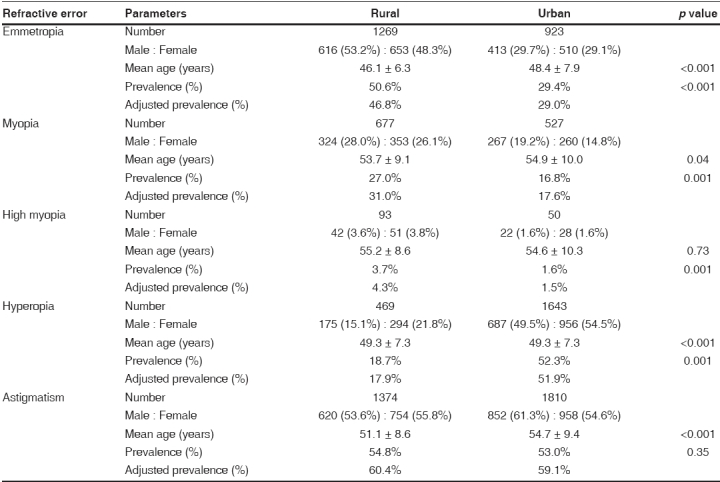
Spectacle use was significantly higher and positively associated with literacy and employment in the urban population. The age and gender-adjusted prevalence of emmetropia, myopia of spherical equivalent (SE) ≤-0.50 diopter sphere (DS), high myopia (SE ≤-5.00DS), hyperopia (SE >0.50DS) and astigmatism ≤ 0.50 diopter cylinder (DC) were 46.8%, 31.0%, 4.3%, 17.9% and 60.4% respectively in the rural population and 29.0%, 17.6%, 1.5%, 51.9%, 59.1% respectively in the urban population. The prevalence of emmetropia decreased with age (p < 0.001); prevalence of myopia and high myopia increased with age (p = 0.001) and were associated with nuclear sclerosis (p = 0.001) in both populations. Hyperopia was commoner among women than men (p = 0.001); was positively associated with diabetes mellitus (p = 0.008) in the rural population and negatively with nuclear sclerosis (p = 0.001) in both populations.
Conclusion:
Spectacle use was found to be significantly lower in the rural population. The pattern of refractive errors was significantly different between both populations.
Keywords: Astigmatism, hyperopia, myopia, population-based, refractive errors, spectacle
Uncorrected refractive error is the most frequently encountered reason for visual impairment.1,2 It has significant effects on individuals and communities, restricting some educational and occupational employment opportunities of otherwise healthy individuals. Uncorrected refractive error has been recognized as an ocular health problem by the World Health Organization while launching the Vision 2020: Right to Sight initiative, which aims to eliminate avoidable blindness by the year 2020.3 Several population-based studies have been conducted in various countries to study the prevalence of refractive errors and understand the magnitude of the problem.
The refractive status of a person above 40 years changes with age, predominantly due to the changes in the crystalline lens. Genetic and environmental influences are also believed to play a role in determining the refractive status of the eye.4-7 The rural and the urban populations of India differ from each other in several aspects such as demographic profile, the disease pattern, systemic diseases and access to ophthalmic care.8-10 The Andhra Pradesh Eye Diseases Study (APEDS) reported the prevalence of refractive errors in an urban population.11 The prevalence of refractive errors in a rural population has been reported previously by the Chennai Glaucoma Study (CGS).12 This study aims to compare the prevalence of refractive errors and report the factors associated with the use of glasses in the rural and urban adult South Indian population as part of the Chennai Glaucoma Study.
Materials and Methods
The Chennai Glaucoma Study was a population-based cross- sectional study to estimate the prevalence of glaucoma in a rural and urban South Indian population. The rural study area13-16 comprised a total population of 22,000 people residing in 27 villages spread over Thiruvallur and Kancheepuram districts of Tamil Nadu. The urban sample was identified by a multistage sampling procedure. The city was divided into 10 corporation zones comprising 155 divisions. One division was randomly selected from each of the 10 zones and five divisions were randomly picked from those 10 divisions.
Twenty-two per cent of the population was above the age of 40 years as per the 1991 Census of India report.13-16 Based on this distribution, 4840 subjects aged 40 years or more were expected in our study area. Four thousand eight hundred persons were enumerated each in rural and urban areas. In the urban area, a simple random sample of 960 each from the five selected divisions was enumerated.17
The study was conducted between June 2001 and May 2004. Written informed consent was obtained from all subjects and the study was performed in accordance with the tenets of the Declaration of Helsinki. The study was approved by the institutional review board, Vision Research Foundation, Chennai. All subjects underwent a complete ophthalmic examination including a detailed history of ophthalmic and systemic problems, measurement of best-corrected visual acuity using the modified ETDRS chart (Light House Low Vision Products, New York, NY, USA), applanation tonometry, gonioscopy, grading of lens opacities using LOCS II,18 fundus examination, optic disc and fundus photography and random blood sugar estimation.
Monocular visual acuity was determined with current spectacle prescription if any. Pinhole acuity was assessed in eyes with presenting visual acuity less than 20/20 (logMAR 0.0). Streak retinoscopy (Beta 200, Heine, Germany) and subjective refraction were performed on all subjects. The best-corrected visual acuity was ascertained and recorded. Refraction data were based on the subjective refraction. Only the right eye of phakic subjects with best-corrected visual acuity better than or equal to 20/40 (logMAR 0.3) were included for analysis.17
A detailed history on present spectacle use and the type of spectacle was ascertained from all subjects participating in the study. Subjects who had completed at least primary education were classified as literates.19 Occupation was classified as daily wage, employed (private/government/self-employed/business), retired and professionals.
Emmetropia was defined as a spherical equivalent between -0.50 diopter sphere (DS) and +0.50 DS.12,20 Myopia was defined as a spherical equivalent lesser than -0.50 DS and spherical equivalent lesser than - 5.00 DS was classified as high myopia.11,12,20-24 Hyperopia was defined as spherical equivalent greater than +0.50DS.11,12,20-24 Astigmatic correction was prescribed in the minus cylinder format and astigmatism was defined as a cylindrical error less than -0.50 diopter cylinder (DC) in any axis.11,12,20-24 Astigmatism was defined as with the rule if the axis lay within 15° on either side of the horizontal meridian, against the rule if the axis lay within 15° on either side of the vertical meridian and oblique astigmatism if the axis lay between 15° to 75° or between 105° to 165°.12,21 Significant nuclear sclerosis was defined as nuclear opalescence of N2 or more with the LOCS II grading system.18 Diabetes mellitus was detected based on previous history and/or random blood sugar level greater than 200 mg/dl.25
Data analysis was carried out using SPSS Version 13 (SPSS Inc, Chicago, IL). Significance was assessed at the P < 0.05 levels for all parameters. Categorical variables between groups were compared using Chi square test or Fisher′s exact test; t test was used for continuous variables. Trends with age were analyzed using Chi square analysis for trend. Pearson′s coefficient of correlation was used to compare subjective and objective refraction and right and left eye refraction. Multivariate analyses were performed using logistic regression.
Results
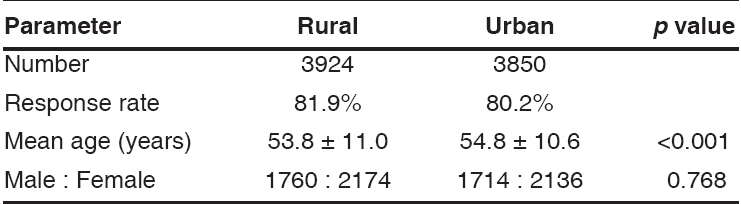
A total of 7774 subjects (3924 rural, 3850 urban) responded to the study. The urban population was significantly older than the rural population. The demographics of the participants from the rural and urban populations are shown in Table 1.
Table 1.
Demographics of rural and urban participants
Three thousand five hundred and nine (89.4%) rural subjects and 3513 (91.3%) urban subjects were phakic in the right eye. Results were analyzed for 2508 (71.5%) rural and 3143 (89.5%) urban subjects whose best-corrected visual acuity in the right eye was 20/40 or better. One thousand one (25.5%) rural subjects were excluded from analysis due to poor vision, 921 (92.0%) due to cataract (LOCS II grade ≥ N2/C3/P2) and the remaining 80 (28 emmetropes, 41 myopes, 11 hyperopes) due to other ocular diseases precluding accurate subjective or objective refraction. In the urban population of the 368 (9.6%) subjects excluded due to poor vision, 330 (89.7%) were due to cataract and the remaining 38 (12 emmetropes, four myopes, eight high myopes, 14 hyperopes) were due to other ocular diseases.
No significant difference was seen between mean objective and subjective refraction in both rural and urban populations (p = 0.06 and 0.49 respectively). Good correlation was seen in subjective refraction between right eye and left eye in both rural and urban populations (Pearson′s correlation: 0.80 and 0.91 respectively). The mean refractive error was -0.56 DS in the rural and +0.40 DS in the urban population. The median refractive error in the rural and urban populations was 0.00 DS and 0.50 DS respectively.
The urban population was significantly older than the rural population (p < 0.001). The demographics of the analyzed population and of all refractive error groups are shown in Tables 2 and 3. There was no significant difference in the proportion of men and women among the rural and urban populations in any of the refractive error groups.
Table 2.
Demographics of the analyzed populations
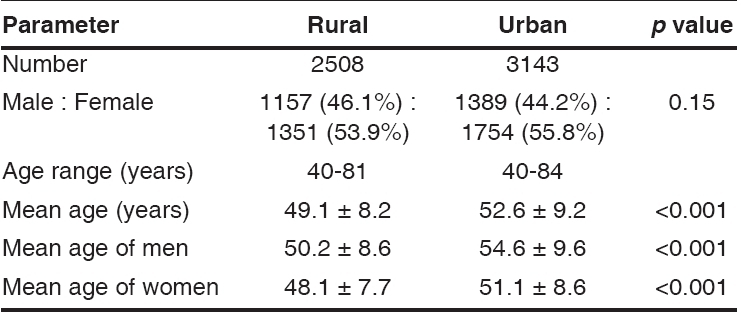
Table 3.
Comparison of refractive error groups in rural and urban populations
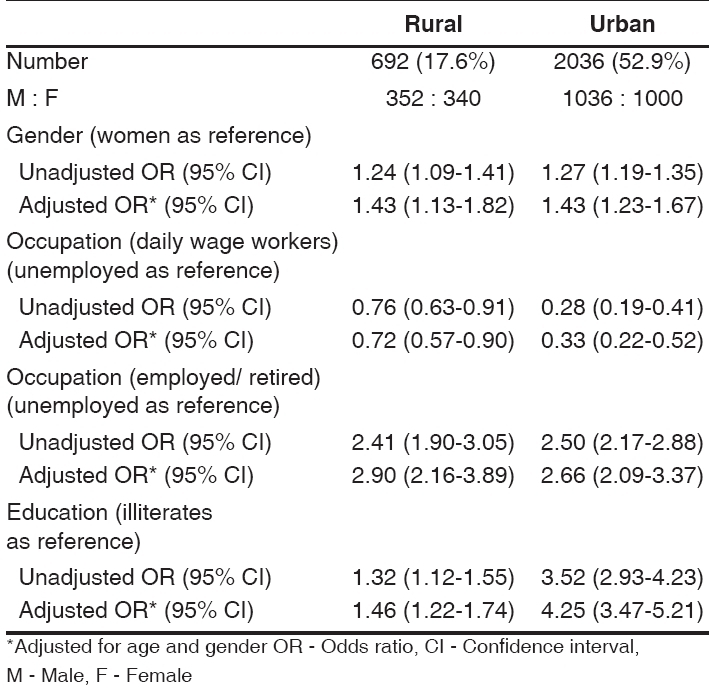
Of the analyzed rural and urban population 17.6% and 52.9% used glasses respectively. There was no significant difference in the proportion of men and women using glasses between both populations. Among spectacle users, the majority of the urban population used bifocal spectacles while more rural people used single vision spectacles either for distance or near vision. Spectacle use was found to increase with increasing age and men were more likely to use glasses in all age groups in both populations [Fig. 1]. In both the rural and the urban populations, daily wage earners were less likely to use glasses (OR: 0.72, 95% CI: 0.57 to 0.90 OR: 0.33, 95% CI: 0.22 to 0.52 respectively) while those employed, professionals or retired were more likely to use glasses. (OR: 2.90, 95% CI: 2.16 to 3.89 OR: 2.66, 95% CI: 2.09 to 3.37 respectively).
Figure 1.
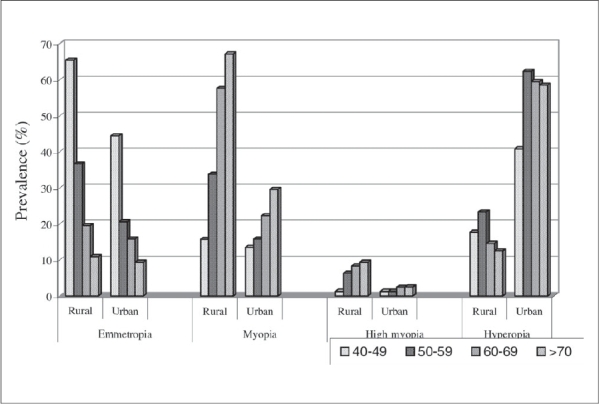
Prevalence of refractive errors in each group in rural and urban populations
In the rural population a subset of six villages concentrated on cottage industry with embroidery as their primary occupation. Villagers in these areas were more likely to wear glasses than the agricultural villages (OR: 1.61, 95% CI: 1.36 to 1.91). Among the spectacle users, they were more likely to use either single vision spectacles for near vision or bifocals (OR: 5.14, 95% CI: 3.31 to 7.98; OR: 1.39, 95% CI: 1.10 to 1.74 respectively).
Literacy was found to be positively associated with spectacle use in both the rural (OR: 1.46, 95% CI: 1.22 to 1.74) and the urban populations (OR: 4.25, 95% CI: 3.47 to 5.21). Among the refractive error groups, use of glasses was found to be more common among hyperopes, in both rural (32.0%) and urban (64.9%) population [Table 4].
Table 4.
Use of specatacles
The prevalence of emmetropia differed significantly between the two populations (p < 0.001) with the urban population showing significantly fewer emmetropes when compared to the rural population. Both populations showed a significant decreasing trend of emmetropia with age (p < 0.001). No association was noted between gender and emmetropia in both rural and urban populations.
The prevalence of myopia was also found to be significantly different in both populations (p = 0.001). The myopic rural and urban populations were found to be significantly older than the entire population (p < 0.001). Myopia was found to be significantly associated with nuclear sclerosis (p < 0.001). Table 5 gives the distribution of significant nuclear sclerosis in each age group in both the populations. The age-adjusted Odds Ratio (OR) for nuclear sclerosis and myopia was 11.80 (95% CI: 9.01 to 15.46), and 8.35 (95% CI: 6.19 to 11.28) for the rural and urban population respectively. The prevalence of myopia in both populations showed a significant increasing trend with age (p < 0.001). After adjustment for nuclear sclerosis there was a significant negative trend seen between myopia and age (p = 0.005, age-adjusted OR: 0.98, 95% CI: 0.97 to 0.99). There was no significant difference noted in the prevalence of the myopia between genders in the rural population (p = 0.31). In the urban population it was found that men were more likely to be myopic (p = 0.005, age-adjusted OR: 1.34, 95% CI: 1.10 to 1.64). Myopia was not significantly associated with diabetes mellitus in both rural and urban population (p = 0.98 and 0.41 respectively).
Table 5.
Comparison of nuclear sclerosis among myopes and non-myopes
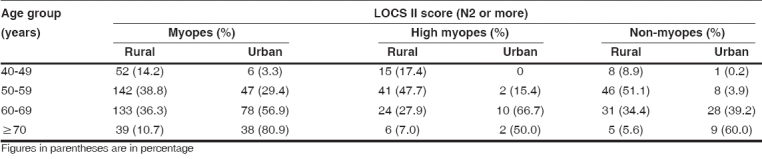
The prevalence of high myopia was also significantly higher in the rural population (p = 0.001); there was no significant difference in the mean age between the two populations (p = 0.73), however, the mean age of high myopes in both populations was significantly higher than the entire population (p = 0.001). The prevalence of high myopia was found to significantly increase with age in the rural population (chi square for trend p = 0.001). However, though increasing trend of the prevalence with age was seen in the urban population, it was not found to be significant (p = 0.07). There was no significant association noted between gender and high myopia in both populations.
The prevalence of hyperopia was significantly higher in the urban population (p = 0.001). The mean age of hyperopes was significantly higher in the urban population. The prevalence of hyperopia in the rural population increased till 60 years and then decreased (chi square for trend p = 0.74). Though chi square for trend in the urban population showed a significant increase in prevalence with age (p < 0.001), a similar trend of increasing prevalence till 60 years and then a decrease was seen.
Women were found to have a significantly higher prevalence of hyperopia than men in both the rural and urban population (p = 0.001). This significance remained even after adjusting for age. The age-adjusted OR for hyperopia among women in the rural population was found to be 1.33 (95% CI: 1.11 to 1.59, p = 0.002) and 1.43 (95% CI: 1.24 to 1.66, p < 0.001) in the urban population. Hyperopia showed a significant negative association with nuclear sclerosis in both cohorts. The age- adjusted OR was 0.098 (95% CI: 0.06 to 0.14, p < 0.001) and 0.14 (95% CI: 0.11 to 0.19, p < 0.001) for the rural and urban population respectively. Hyperopia was found to have a significant positive association with diabetes mellitus in the rural population (p = 0.008, age-adjusted OR: 1.55, 95% CI: 1.12 to 2.14). However, no association was noted between hyperopia and diabetes in the urban population.
The prevalence of astigmatism did not vary significantly between both the populations (p = 0.35). The prevalence of against the rule astigmatism was found to significantly increase with age in the rural and urban populations (p = 0.006 and p < 0.001 respectively) and with the rule significantly decreased with age (p = 0.001 and p < 0.001 respectively) in both populations.
Analyzing the complaints of decrease in vision among the non spectacle users 82.5% of uncorrected presbyopes who needed only near vision correction in the rural cohort and 97.15% of those in the urban cohort complained of decreased vision. On analyzing any degree of uncorrected refractive error greater than +/- 0.5D: 85% of those with uncorrected mild and moderate hyperopia complained of decreased vision. For mild, moderate and high myopia these figures were 87.2%, 87.5% and 90% respectively for the rural cohort. For the urban population these figures were 96.5%, 95% and 100% for mild, moderate and severe myopia and 97.3%, 99.1% and 100% for corresponding grades of hyperopia.
Discussion
Dandona et al., have reported the prevalence of refractive errors in an urban south Indian population that included children and adults.11 The prevalence of refractive errors in the rural south Indian adult population has been reported previously by the Chennai Glaucoma Study (CGS).12 This study, which is also a part of the population-based study of glaucoma, compares the prevalence of refractive errors between rural and urban south Indian populations.
Spectacle use was found to be more common among the urban population than the rural population. This could be due to increased availability and accessibility of eye care services in these areas. Spectacle use was also found to be more common among employed people and literates, which is similar to the findings reported by Dandona et al.26 Spectacle use was found to increase with age in both populations probably due to the onset of lenticular myopia or need for spectacles after cataract surgery. Factors that were associated with spectacle use were related to literacy, those from the rural cohort were less likely to use bifocal spectacles possibly related to lower education levels. However, need-based use was seen in the rural population which is reflected in the higher prevalence of near vision correction among those who were employed in embroidery as a cottage industry and the lower prevalence in both populations among daily wage earners who were predominantly involved in manual labor.
Eighty-three per cent of the rural and 97.15% of the urban cohort with uncorrected presbyopes complained of decreased vision. Among non spectacle users even mild degrees of uncorrected refractive error were responsible for noticeable visual impairment among the majority of rural and almost all urban subjects.
The prevalence of emmetropia was found to be significantly different between the two populations. This could probably be due to earlier onset of lenticular myopia in the rural population causing a myopic shift thereby decreasing the expected hyperopic refractive error towards myopia or emmetropia.
The prevalence of myopia in the rural population was found to be 26.99%. Myopia in the rural population was found to significantly increase with age, which is similar to the finding reported by Dandona et al.11 and the Barbados eye study.24 Since the majority of our rural population was agricultural workers, increased exposure to ultraviolet radiation from the sun causing earlier aging of the crystalline lens could be the reason for increased prevalence of nuclear sclerosis and consequently myopia in the rural population.7
The prevalence of myopia in the urban population was found to be 16.77%. The prevalence of myopia was found to be significantly lesser in the urban than the rural population. The urban prevalence of myopia is similar to the prevalence reported by several other population-based studies (APEDS,11 Baltimore,23 Rotterdam,27 Melbourne VIP28). Early nuclear sclerosis is known to induce index myopia due to changes in the refractive index of the central nucleus. Nuclear sclerosis was found to be significantly associated with myopia in both the rural and the urban populations. However, significant nuclear sclerosis was found to be more prevalent in the rural than in the urban population. The prevalence of myopia was found to significantly increase with age in the urban population. After adjustment for nuclear sclerosis, the prevalence was found to decrease with age, similar to reports from other western countries.21-24 Myopia was found to be more common among urban men than women. This male preponderance has been reported earlier in a study of Caucasians and in the Bangladeshi population.29,30
The prevalence of hyperopia in the rural population was 18.70%. The prevalence of hyperopia in the rural population was found to increase till 60 years of age and then decrease which was similar to the finding reported by the Barbados eye study.24 The prevalence of hyperopia was found to be significantly higher among women. Diabetes was found to be significantly positively associated with hyperopia in the rural population.12
The prevalence of hyperopia was significantly higher in the urban population (52.27%) than in the rural population. The decreased prevalence of hyperopia in the rural population could be due to the influence of lens causing early nuclear sclerosis and hence an associated myopic shift. The urban population showed an increasing trend of hyperopia with age similar to the findings reported by APEDS11 and several other studies.21-23 Hyperopia prevalence was found to be significantly higher among women than men in the urban population as seen in the rural. This female preponderance has also been reported in several other studies.11,22,24,29 Women have been reported to have shorter axial length than men in a subset of our population,31 which could explain the increased prevalence of hyperopia among women in our study.
The prevalence of astigmatism was found to be 54.78% in the rural population and 53.03% in the urban population. The prevalence in both populations was found to significantly increase with age as reported by studies in the South East Asian populations.20,32 Against the rule astigmatism was found to be predominant in both populations similar to the finding reported by the Blue Mountains eye study21 and the APEDS.11 The prevalence of against the rule astigmatism significantly increased with age and with the rule astigmatism significantly decreased with age in both populations. One of the postulated reasons is increased lid laxity with age causing flattening of the vertical corneal meridian thereby decreasing with the rule astigmatism and increasing against the rule astigmatism with age.11,33-35
In conclusion, 70.63% of the urban population and 49.40% of the rural population had refractive errors, while only 59.40% in urban and 17.20% in the rural population used refractive correction. Prevalence of spectacle use was significantly lower in the rural population. This is a substantial proportion of the population that has correctable visual impairment and is not using glasses. The difference in usage pattern between both populations could be related to differences in the penetration of ophthalmic services or differences in perceived need for the use of glasses. The other finding was that the pattern of refractive errors was different for both cohorts - this could largely be explained by the emmetropization of the rural population secondary to lenticular myopia. Early nuclear lenticular changes significantly influence the pattern of refractive errors in the rural population. It potentially leads to emmetropization of the hyperopic error and increased index myopia.
Footnotes
Source of Support: Chennai Willingdon Corporate Foundation
Conflict of Interest: None declared
References
- 1.Dandona R, Dandona L. Refractive error blindness. Bull World Health Organ. 2001;79:237–43. [PMC free article] [PubMed] [Google Scholar]
- 2.Dandona L, Dandona R, Naduvilath TJ, McCarthy CA, Srinivas M, Mandal P, et al. Burden of moderate visual impairment in an urban population in Southern India. Ophthalmology. 1999;106:497–504. doi: 10.1016/S0161-6420(99)90107-0. [DOI] [PubMed] [Google Scholar]
- 3.Magnitude and causes of visual impairment. World Health Organization [homepage on the internet] Available from: http://www.who.int/mediacentre/factsheets/fs282/en/
- 4.Saw SM, Chua WH, Wu HM, Yap E, Chia KS, Stone RA. Myopia: Gene-environment interaction. Ann Acad Med Singapore. 2000;29:290–7. [PubMed] [Google Scholar]
- 5.Saw SM. A synopsis of the prevalence rates and environmental risk factors for myopia. Clin Exp Optom. 2003;86:289–94. doi: 10.1111/j.1444-0938.2003.tb03124.x. [DOI] [PubMed] [Google Scholar]
- 6.Guggenheim JA, Hill C, Yam TF. Myopia, Genetics and ambient lighting at night in a UK sample. Br J Ophthalmol. 2003;87:580–2. doi: 10.1136/bjo.87.5.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dong X, Ayala M, Lofgren S, Soderberg PG. Ultraviolet radiation- induced cataract: Age and Maximum acceptable dosage. Invest Ophthalmol Vis Sci. 2003;44:1150–4. doi: 10.1167/iovs.02-0541. [DOI] [PubMed] [Google Scholar]
- 8.Ramachandran A, Snehalatha C, Dharmaraj D, Viswanathan M. Prevalence of glucose intolerance in Asian Indians: Urban-rural difference and significance of upper body adiposity. Diabetes Care. 1992;10:1348–55. doi: 10.2337/diacare.15.10.1348. [DOI] [PubMed] [Google Scholar]
- 9.Reddy KS, Prabhakaran D, Shah P, Shah B. Differences in body mass index and waist:hip ratios in north Indian rural and urban populations: The International Association for the Study of Obesity. Obes Rev. 2002;3:197–202. doi: 10.1046/j.1467-789x.2002.00075.x. [DOI] [PubMed] [Google Scholar]
- 10.Rao GN. Ophthalmology in India. Arch Ophthalmol. 2000;118:1431–2. doi: 10.1001/archopht.118.10.1431. [DOI] [PubMed] [Google Scholar]
- 11.Dandona L, Dandona R, Naduvilath TJ, Srinivas M, McCarthy CA, Rao GN. Refractive errors in an urban population in Southern India: The Andhra Pradesh Eye Diseases Study. Invest Ophthalmol Vis Sci. 1999;40:2810–8. [PubMed] [Google Scholar]
- 12.Raju P, Ramesh S Ve, Arvind H, George R, Baskaran M, Pradeep GP, et al. Prevalence of refractive errors in a rural South Indian population. Invest Ophthalmol Vis Sci. 2004;45:4268–72. doi: 10.1167/iovs.04-0221. [DOI] [PubMed] [Google Scholar]
- 13.Census of India 1991, District census handbook, Chengelpet MGR district. Series 23 (Part XII -B) New Delhi: Government of India; 1991. pp. 214–343. [Google Scholar]
- 14.Census of India 1991: Religion (Table C-9), District census handbook, Chengelpet MGR district. Series 23 (Part IV B - (ii) New Delhi: Government of India; 1991. pp. 22–9. [Google Scholar]
- 15.Census of India 1991, District census handbook, Chengelpet MGR district, New Delhi. Series 23 (Part IV A, C Series) New Delhi: Government of India; 1991. pp. 25–54. [Google Scholar]
- 16.Census of India 1991, Social and Cultural Tables (Table C-6), District census handbook, Chengelpet MGR district, New Delhi. Part IV. New Delhi: Government of India; 1991. pp. 56–60. [Google Scholar]
- 17.Arvind H, Paul PG, Raju P, Baskaran M, George R, Balu S, et al. Methods and design of Chennai glaucoma study. Ophthalmic Epidemiol. 2003;10:337–48. doi: 10.1076/opep.10.5.337.17320. [DOI] [PubMed] [Google Scholar]
- 18.Chylac LT, Leske MC, McCarthy D, Khu P, Kashiwagi T, Sperdito R. Lens Opacities Classification System II (LOCS II) Arch Ophthalmol. 1989;107:991–7. doi: 10.1001/archopht.1989.01070020053028. [DOI] [PubMed] [Google Scholar]
- 19.Paul PG, George R, Baskaran M, Arvind H, Madanraj V, Augustian J, et al. A comparison of participants and non-participants in the Chennai glaucoma study-rural population. Ophthalmic Epidemiol. 2005;12:125–32. doi: 10.1080/09286580590932798. [DOI] [PubMed] [Google Scholar]
- 20.Wong TY, Foster PJ, Hee J, Pin Ng Tze, Tielsch JM, Chew SJ, et al. Prevalence and risk factors of refractive errors in adult Chinese in Singapore. Invest Ophthalmol Vis Sci. 2000;41:2486–94. [PubMed] [Google Scholar]
- 21.Attebo K, Ivers RQ, Mitchell P. Refractive errors in an older population: The Blue Mountains eye study. Ophthalmology. 1999;106:1066–72. doi: 10.1016/S0161-6420(99)90251-8. [DOI] [PubMed] [Google Scholar]
- 22.Wang Q, Klein BE, Klein R, Moss SE. Refractive status in the Beaver Dam eye study. Invest Ophthalmol Vis Sci. 1994;35:4344–47. [PubMed] [Google Scholar]
- 23.Katz J, Tielsch JM, Sommer A. Prevalence and risk factors for refractive errors in an adult inner city population. Invest Ophthalmol Vis Sci. 1997;38:334–40. [PubMed] [Google Scholar]
- 24.Wu SY, Nemesure B, Leske MC. Refractive errors in a black adult population: The Barbados eye study. Invest Ophthalmol Vis Sci. 1999;40:2179–84. [PubMed] [Google Scholar]
- 25.Lamb EJ, Day AP. New diagnostic criteria for diabetes mellitus:are we any further forward? Ann Clin Biochem. 2000;37:588–92. doi: 10.1258/0004563001899889. [DOI] [PubMed] [Google Scholar]
- 26.Dandona R, Dandona L, Kovai V, Giridhar P, Prasad Mudigonda N, Srinivas M. Population-based study of speactacle use in Southern India. Indian J Ophthalmol. 2002;50:145–55. [PubMed] [Google Scholar]
- 27.The Eye Diseases Prevalence Research Group. The prevalence of refractive errors among adults in the United States, Western Europe and Australia. Arch Ophthalmol. 2004;122:495–505. doi: 10.1001/archopht.122.4.495. [DOI] [PubMed] [Google Scholar]
- 28.Wensor M, McCarty CA, Taylor HR. Prevalence and risk factors of myopia in Victoria, Australia. Arch Ophthalmol. 1999;117:658–63. doi: 10.1001/archopht.117.5.658. [DOI] [PubMed] [Google Scholar]
- 29.Hyams S, Pokotilo E, Shkruko G. Prevalence of refractive errors in adults over 40: A survey of 8102 eyes. Br J Ophthalmol. 1977;61:428–32. doi: 10.1136/bjo.61.6.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rupert RA, Brendan PD, Syed MA, Deen MN, Gordon JJ. Prevalence of refractive error in Bangladeshi adults: Results of the National Blindness ND Low vision survey of Bangladesh. Ophthalmology. 2004;111:1150–60. doi: 10.1016/j.ophtha.2003.09.046. [DOI] [PubMed] [Google Scholar]
- 31.George R, Paul PG, Baskaran M, Ramesh S Ve, Raju P, Arvind H, et al. Ocular Biometry in occludable angles and angle closure glaucoma: A population based survey. Br J Ophthalmol. 2003;87:399–402. doi: 10.1136/bjo.87.4.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Saw SM, Gazzard G, Koh D, Farook M, Widjaja D, Lee J, et al. Prevalence rates of refractive errors in Sumatra, Indonesia. Invest Ophthalmol Vis Sci. 2002;43:3174–80. [PubMed] [Google Scholar]
- 33.Gudmundsdottir E, Jonasson F, Jonsson V, Stefansson E, Sasaki H, Sasaki K, et al. ″With the rule″ astigmatism is not the rule in the elderly. Acta Ophthalmol Scand. 2000;78:642–6. doi: 10.1034/j.1600-0420.2000.078006642.x. [DOI] [PubMed] [Google Scholar]
- 34.Pensyl CD, Harrison RA, Simpson P, Waterbor JW. Distribution of astigmatism among Sioux Indians in South Dakota. J Am Opto Assoc. 1997;68:425–31. [PubMed] [Google Scholar]
- 35.Goss DA. Meridional analysis of with-the-rule astigmatism in Oklahoma Indians. Optom Vis Sci. 1989;66:281–7. doi: 10.1097/00006324-198905000-00005. [DOI] [PubMed] [Google Scholar]


