Abstract
We report a case of a choroidal neovascular membrane (CNVM) following ocular penetration during peribulbar anesthesia in a 55- year-old male patient. A combination of photodynamic therapy with intravitreal bevacizumab led to resolution of the persistent CNVM.
Keywords: Bevacizumab, choroidal neovascular membrane, penetrating ocular injury, peribulbar anesthesia, photodynamic therapy
Peribulbar anesthesia is an established technique of anesthesia for ocular surgeries.1 Ocular penetration and its complications following peribulbar anesthesia have often been reported in the literature.2,3
We are unaware of previous reports of a choroidal neovascular membrane (CNVM) following penetrating ocular injury due to peribulbar anesthesia and its response to standard photodynamic therapy (PDT) along with intravitreal anti- vascular endothelial growth factor (VEGF) agents.
Case Report
A 55-year-old male patient presented to us with history of sudden onset metamorphopsia in the left eye. He was operated in the same eye four months back for vitreous hemorrhage secondary to ocular penetration following peribulbar anesthesia for cataract surgery (both the surgeries were done elsewhere). He was a known case of open angle glaucoma under treatment with timolol maleate 0.5% eye drops twice a day and dorzolamide eye drops thrice a day over the past three years.
On examination, the best-corrected visual acuity in the right eye was finger counting (FC) three feet, <N36 and in the left eye was 20/120, N18. The intraocular pressure (IOP) was 14 mmHg in either eye with applanation tonometer. Fundus examination showed retinal pigment epithelium (RPE) atrophy at the macula in the right eye and a large scar running across the macula bordered by fluid and hemorrhage at its distal end in the left [Fig. 1]. There was an advanced glaucomatous optic neuropathy (cup disc ratio - 0.9:1 with pale neuro-retinal rim) in either eye.
Figure 1.

Fundus examination of the left eye shows a large scar running across the macula bordered by fluid and hemorrhage at its distal end. Inset: Fundus fluorescein angiography of the left eye shows a linear hypofluorescence running across the macula corresponding to the needle tract through the retinal pigment epithelium. At its distal end was found a hyperfluorescent area with leakage suggestive of a choroidal neovascular membrane
On fundus fluorescein angiography (FFA) of the left eye, there was a linear hypofluorescence running across the macula corresponding to the needle tract through the RPE. At its distal edge was found a hyperfluorescent area with leakage suggestive of a CNVM [Fig. 1, inset]. Patient was subjected to standard fluence PDT for the same. There was persistence of CNVM one month following PDT [Fig. 2, left]. At this point of time patient was subjected to combination therapy of a standard fluence PDT with intravitreal bevacizumab (2.5 mg/0.1 ml, Off-label) injection immediately after the PDT, which was uneventful. Six months following the treatment visual acuity had stabilized to 20/60, N12 with no leakage on FFA [Fig. 2, right].
Fig. 2, left.
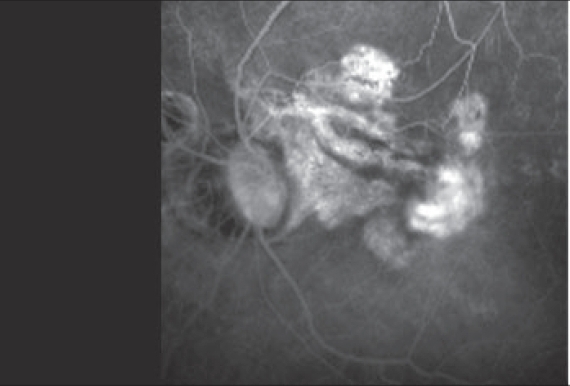
Left: Fundus fluorescein angiography of the left eye shows persistent leakage from the choroidal neovascular membrane (after first photodynamic therapy)
Fig. 2, right.

Right: Fundus fluorescein angiography of the left eye at the last visit shows absence of leakage from the choroidal neovascular membrane
Discussion
Globe penetration is a less common complication of peribulbar anesthesia (0.006%).1,2,4 This incidence is likely to be higher in patients with high myopia owing to the increased axial length as in our patient.5 However, as the cataract surgery was done elsewhere the exact technique and sequence of events was not known.
The presumed etiology of CNVM, due to ocular perforation during peribulbar anesthesia, can be postulated by the development of vitreous hemorrhage immediately after the cataract surgery and the relation of the CNVM with the needle tract on FFA. PDT is an established treatment for predominantly classic CNVM following age related macular degeneration (ARMD). Photodynamic therapy seems to be effective against CNVM due to choroidal rupture following blunt trauma.6
Intravitreal bevacizumab (Genentech) has been found successful in the treatment of a wide variety of ocular pathologies including CNVM of varied etiologies.7 It was chosen in our patient (who had advanced glaucoma) because of lesser propensity to elevate IOP compared to triamcinolone acetate. As the effect of bevacizumab would have been short-lived in a vitrectomized eye a combined treatment was preferred over monotherapy.
Thus, CNVM following ocular penetration is a rare but sight-threatening complication of peribulbar anesthesia. A combination therapy of PDT with intravitreal bevacizumab seems to be an effective therapy.
References
- 1.David DB, 2nd, Mandel MR. Efficacy and complication rate of 16,224 consecutive peribulbar blocks: A prospective multicenter study. J Cataract Refract Surg. 1994;20:327–37. doi: 10.1016/s0886-3350(13)80586-x. [DOI] [PubMed] [Google Scholar]
- 2.Puri P, Verma D, McKibbin M. Management of ocular perforations resulting from peribulbar anaesthesia. Indian J Ophthalmol. 1999;47:181–3. [PubMed] [Google Scholar]
- 3.Lingam G, Badrinath SS, Parikh S, Chawla G. Retinal detachment secondary to ocular perforation during retrobulbar anaesthesia. Indian J Ophthalmol. 1995;43:13–5. [PubMed] [Google Scholar]
- 4.Kumar CM. Orbital regional anaesthesia: Complications and their prevention. Indian J Ophthalmol. 2006;54:77–84. doi: 10.4103/0301-4738.25826. [DOI] [PubMed] [Google Scholar]
- 5.Gadkari Salil S. Evaluation of 19 cases of inadvertent globe perforation due to periocular injections. Indian J Ophthalmol. 2007;55:103–7. doi: 10.4103/0301-4738.30702. [DOI] [PubMed] [Google Scholar]
- 6.Mehta HB, Shanmugam MP. Photodynamic therapy of a post traumatic choroidal neovascular membrane. Indian J Ophthalmol. 2005;53:131–2. doi: 10.4103/0301-4738.16180. [DOI] [PubMed] [Google Scholar]
- 7.Bashshur ZF, Bazarbachi A, Schakal A, Haddad ZA, El Haibi CP, Noureddin BN. Intravitreal bevacizumab for the management of choroidal neovascularization in age-related macular degeneration. Am J Ophthalmol. 2006;142:1–9. doi: 10.1016/j.ajo.2006.02.037. [DOI] [PubMed] [Google Scholar]


