Abstract
Purpose:
To study the optic disc topographic measurements of normal Indian eyes using optical coherence tomography (OCT).
Materials and Methods:
One hundred and fifty eyes selected randomly from 150 normal Indian subjects of both sex and various age groups underwent optic disc imaging with the OCT using the fast optic disc protocol.
Results:
Mean ± standard deviation of the optic disc topographic measurements were: disc area 2.63 ± 0.55 mm2, cup area 0.87 ± 0.45 mm2, neuroretinal rim area 1.78 ± 0.55 mm2 and cup to disc area ratio 0.33 ± 0.15. There was no significant difference in the measurements between males and females. There was no significant correlation with respect to age and refractive errors ranging from -5.0 to +3.0 diopters of spherical equivalent.
Conclusion:
Our study provides a normative database for the various optic disc topographic measurements and its variations with age, sex and refractive error in normal Indian eyes using OCT.
Keywords: Normal Indian eyes, optic disc topographic measurements, optical coherence tomography
Introduction
Assessment of the optic disc is of utmost importance not only for the diagnosis of optic nerve anomalies, glaucoma and neuro- ophthalmologic diseases but also for their follow-up.1,2 Several imaging methods are currently employed in clinical practice to obtain quantitative stereometric and volumetric information of the optic disc.3,4
Optical coherence tomography (OCT) is a noninvasive, non-contact, imaging technique which provides in vivo cross- sectional images of the optic nerve and retina. Low-coherence interferometry is used to resolve the distances of reflective structures in the eye. It also enables quantitative assessment of the retinal nerve fiber layer (RNFL) thickness.5,6
Evaluation of the optic disc by various methods has been reported for the Indian population.6-8 A normative database for the optic nerve head analysis using OCT in normal Indian eyes is not available. The purpose of this study was to assess the optic disc topographic measurements in normal Indian eyes using OCT.
Materials and Methods
This study included 156 normal subjects selected randomly from the outpatients allotted to two of us for examination (SD/SB). With informed consent, all subjects were subjected for disc evaluation with the Optical Coherence Tomograph (Stratus OCT™,3, Carl Zeiss Meditec, Dublin, CA). All patients who met the inclusion criteria described below were enrolled in this study.
Each study participant underwent complete ophthalmologic examination including a medical history review, best- corrected visual acuity (Snellen′s visual acuity), slit-lamp examination, intraocular pressure measurement (non-contact pneumotonometry) and dilated fundus examination.
The inclusion criteria were refraction within ±5.0 diopters of spherical equivalent, intraocular pressure ≤21 mm Hg, no family history of glaucoma, no systemic illnesses, no anterior or posterior segment pathology and no history of lasers or intraocular surgery.
Normal-appearing disc, cup and neuroretinal rim (disc anomalies, features of glaucomatous disc and other pathologies of the disc were excluded) on careful examination of the optic disc with 90D-aided stereoscopic slit-lamp indirect ophthalmoscopy, intraocular pressure of ≤21 mm Hg and best- corrected visual acuity of 20/30 or more were the criteria for classifying the optic disc to be normal.
The images were selected on the basis of image quality. Six subjects were excluded from the study due to poor resolution in six eyes produced by the OCT machine (the OCT image poor in red and yellow color).
After making the above exclusions, 150 eyes of 150 subjects (15 to 67 years) consisting of 68 males and 82 females selected randomly using the simple random numbers table, were stratified for sex, age and refractive error.
On the day of the hospital visit, the randomly selected eyes underwent optic disc imaging with the Stratus OCT™ (Software version 4.0.1) using the fast optic disc protocol. This protocol acquires six 4.0 mm radial scans. These line scans are arranged like the spokes of a wheel centered in the middle of the disc. For all scans, internal fixation was used as it provides a higher degree of reproducibility.
Images were automatically analyzed by the software. The OCT imaging and quality assessment of the scans were done by one examiner (SD). Focused ocular fundus video image, an adequate signal strength (>7) and the presence of linear scans centered on the disc were requirements for acceptable quality.
The Stratus OCT extrapolates between the scans to provide measurements throughout the optic nerve head. For optic disc topography, the automated determination of the disc margin as the end of the retinal pigment epithelium (RPE) was used for this analysis. The straight blue line which connects the edges of the RPE represents the disc diameter. The cup diameter is denoted by a parallel red line constructed 150 µm anterior to the disc diameter. Structures below the red line are defined as the cup and structures above the red line, the neuroretinal rim [Fig. 1].
Figure 1.
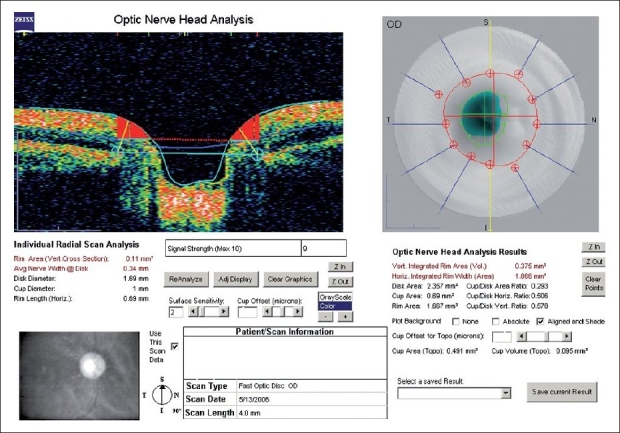
Optic nerve head analysis with OCT
Previous reports estimate the mean morphometric optic disc size of 2.58 ± 0.65 mm2 in the Indian population.8 Expecting to get optic disc area results with significant difference (d) of 0.5 mm2, power of 80% (Zb = 0.842) and significance level of 0.01 (Za = 2.576) was used to determine the sample size. The sample size was determined using the formula n = 2(Za + Zb)2 S2/d2. Considering the standard deviation (S) of 0.65, the minimum sample size calculated was 40.
Student′s t test for independent variables was used to compare the results of different sex. Descriptive analyses including mean values and standard deviation (SD) of the optic disc parameters were performed. Ninety-five per cent confidence intervals for each optic disc parameter were calculated. Pearson′s correlation coefficient and linear regression analysis was done to determine the effect of age on optic disc parameters. Statistical significance was shown if P < 0.05. Statistical analyses were done using SPSS Version 10.0.
Results
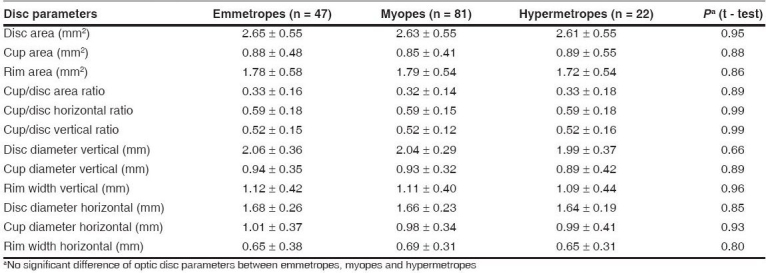
One hundred and fifty eyes of 150 subjects were studied with respect to their sex, age and refractive error. There were 68 (45.3%) males and 82 (54.7%) female subjects with mean age of 32.09 ± 11.54 years (range, 15 to 67). There were 81 (54.0%) myopic, 47 (31.3%) emmetropic and 22 (14.7%) hypermetropic eyes with refraction ranging from -5.0 to +3.0 diopters of spherical equivalent. The mean optic disc parameters are detailed in Table 1. There was no statistical difference regarding the sex [Table 1]. However, there was statistical correlation between the age and some optic disc parameters [Table 2]. There was no statistical difference between the refractive errors for the various optic disc parameters [Table 3].
Table 1.
Optic disc parameters - variations with sex [Mean ± SD (95% CI)]
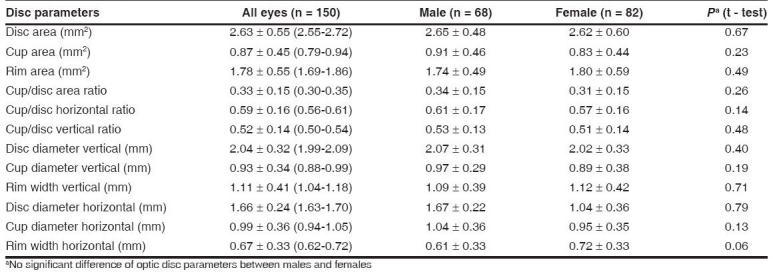
Table 2.
Optic disc parameters - changes with respect to age [Mean (SD)]
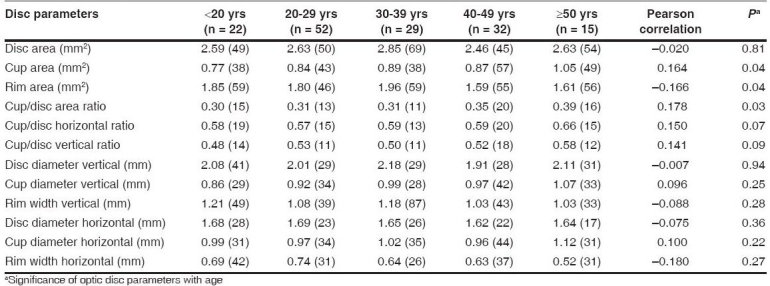
Table 3.
Optic disc parameters - variations with refractive error (range, -5.0 to +3.0 diopters) [Mean ± SD]
Optic disc: Mean optic disc area was 2.63 ± 0.55 mm2. Mean horizontal disc diameter (1.66 ± 0.24 mm) was significantly (P < 0.01) smaller than the mean vertical disc diameter (2.04 ± 0.32 mm). The shape of the optic disc was vertically oval in the majority of eyes, with the vertical disc diameter being greater than the horizontal disc diameter in 132 eyes (88.0%). The horizontal disc diameter was greater than the vertical disc diameter in 15 eyes (10.0%). In three eyes (2.0%), the vertical disc diameter and the horizontal disc diameter were equal.
Neuroretinal rim: Mean neuroretinal rim area was 1.78 ± 0.55 mm2. It was significantly and positively correlated with the size of the disc (r = 0.64, P < 0.01). There was a significant negative correlation between the rim area and cup area (r = -0.42, P < 0.01). Mean vertical rim width (1.11 ± 0.41 mm) was significantly (P < 0.01) greater than the mean horizontal rim width (0.67 ± 0.33 mm).
Optic cup: Mean cup area was 0.87 ± 0.45 mm2. It had significant positive correlation with the optic disc size (r = 0.41, P < 0.01). The horizontal cup diameter was greater than the vertical cup diameter, indicating a horizontally oval shape of the cup. However, there was no statistically significant difference between the horizontal cup diameter and the vertical cup diameter (P = 0.12)
Cup to disc ratio: The mean horizontal cup/disc ratio was 0.59 ± 0.16 and mean vertical cup/disc ratio was 0.52 ± 0.14. The mean cup/disc area ratio was 0.33 ± 0.15. The cup/disc area ratio had significant positive correlation with the optic disc area (r = 0.05, P < 0.01).
Discussion
Currently, there are several instruments available for the analysis of the optic nerve head, in order to detect early glaucomatous damage, even before functional field loss is detectable. The OCT provides an assessment of the optic nerve head by passing a near - infrared illumination (840 nm) beam into the eye and studying its reflectivity patterns by computer-assisted software. Although OCT has been introduced in India, the normative profile of various disc parameters is not established for the Indian population.
In the present study, we found no significant difference between males and females with respect to the various optic disc parameters. Males had a larger, however not significantly (P = 0.67) larger, disc area than females. Similar findings have been reported by Jonas et al.8 The Rotterdam study, one of the largest epidemiological studies on the morphology of the optic nerve head in white people, had demonstrated that the mean optic disc area is on an average 3.2% larger in men than in women.9
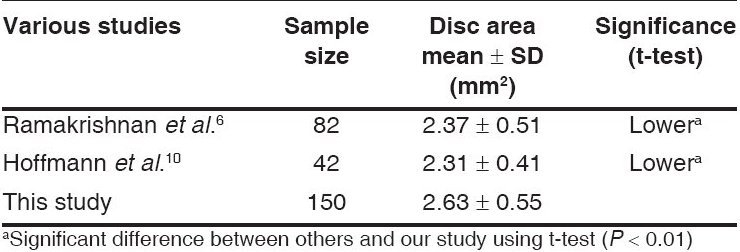
The optic disc area measurement in this study was larger than the optic disc measurements reported by Ramakrishnan et al.6 and Hoffmann et al.,10 who like us had used the Stratus OCT to assess the optic disc topography. The statistically significant difference in measurements may be attributed to the larger sample size of our study [Table 4]. Discrepancy in measurements could also be due to the fact that in our study, the analysis was done entirely by the software, whereas in the study by Ramakrishnan et al.,6 the end of the RPE/choriocapillaries reflection was detected manually in certain cases.
Table 4.
Comparison of mean disc area in various studies
A linear correlation between the disc size and the cup to disc area ratio has been reported earlier.11 The increase in the cup to disc area ratio for each millimeter increase in the disc diameter was 0.27 in the Blue Mountain Eye Study.12 In the current study, the increase in the cup to disc area ratio for each millimeter increase in the disc diameter was 0.08.
Decline in RNFL thickness owing to the loss of ganglion cells with age has been demonstrated with the help of OCT13 and histopathological studies.14 With this RNFL loss, one expects the neuroretinal rim area to decrease and the cup area to increase, as confirmed in this study.
In our study, the spherical equivalent of refraction ranged from -5.0 to +3.0 diopters. For this range of refraction, we found no significant difference in the various optic disc parameters. This finding was also seen in the study by Jonas et al.,8 where the range of refraction was -4.5 to +2.5 diopters. Jonas has shown that the optic disc size depends on the refractive error with an increase in highly myopic eyes beyond - 8 diopters and a decrease in highly hyperopic eyes beyond +4 diopters.15
The normative database commercially available with the Stratus OCT neither provides information on ethnic differences within its data groups nor does it provide information with numerical data. Our study therefore provides a normative database for the various optic disc topographic measurements and its variations with sex, age and refractive error in normal Indian eyes using OCT.
However, the limitation of this study is that it is biased towards the younger age group. Further investigation with a larger sample size and an older age group who are more prone to disc changes may be required.
Conclusion
Our study provides a normative database for the various optic disc topographic measurements and its variations with sex, age and refractive error in normal Indian eyes using OCT. The development of the three-dimensional Spectral Domain (Fourier Domain) OCT which gives faster and more accurate results could be used to substantiate these findings.
Acknowledgments
The authors would like to thank Mr. R. Ezhil for his assistance with the statistical part of the study.
Footnotes
Presented in part at the Tamil Nadu Ophthalmic Conference, Pondicherry, August 2006
Source of Support: Donation of the OCT Facility by M/s TEXTAN Chemicals (P) Ltd, Chennai and M/s Deccan Overseas Exports (P) Ltd. Chennai
Conflict of Interest: None declared
References
- 1.Caprioli J, Miller JM. Optic disc rim area is related to disc size in normal subjects. Arch Ophthalmol. 1987;105:1683–5. doi: 10.1001/archopht.1987.01060120081030. [DOI] [PubMed] [Google Scholar]
- 2.Garway-Heath DF, Hitchings RA. Quantitative evaluation of the optic nerve head in early glaucoma. Br J Ophthalmol. 1998;82:352–61. doi: 10.1136/bjo.82.4.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Weinreb RN. Assessment of optic disc topography for diagnosing and monitoring glaucoma. Arch Ophthalmol. 1998;116:1229–31. doi: 10.1001/archopht.116.9.1229. [DOI] [PubMed] [Google Scholar]
- 4.Blumenthal EZ, Williams JM, Weinreb RN, Girkin CA, Berry CC, Zangwill LM. Reproducibility of nerve fiber layer thickness by use of optical coherence tomography. Ophthalmology. 2000;107:2278–82. doi: 10.1016/s0161-6420(00)00341-9. [DOI] [PubMed] [Google Scholar]
- 5.Mistlberger A, Liebmann JM, Greenfield DS, Pons ME, Hoh ST, Ishikawa H, et al. Heidelberg retina tomography and optical coherence tomography in normal, ocular hypertensive and glaucomatous eyes. Ophthalmology. 1999;106:2027–32. doi: 10.1016/S0161-6420(99)90419-0. [DOI] [PubMed] [Google Scholar]
- 6.Ramakrishnan R, Kader Mohideen Abdul, Budde Wido M. Optic disc morphometry with optical coherence tomography: Comparison with planimetry of fundus photographs and influence of parapapillary atrophy and pigmentary conus. Indian J Ophthalmol. 2005;53:187–91. doi: 10.4103/0301-4738.16678. [DOI] [PubMed] [Google Scholar]
- 7.Sekhar GC, Prasad K, Dandona R, John RK, Dandona L. Planimetric optic disc parameters in normal eyes: A population based study in South India. Indian J Ophthalmol. 2001;49:19–23. [PubMed] [Google Scholar]
- 8.Jonas JB, Thomas R, George R, Berenshtein E, Muliyil J. Optic disc morphology in South India: The Vellore Eye Study. Br J Ophthalmol. 2003;87:189–96. doi: 10.1136/bjo.87.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ramrattan RS, Wolfs RC, Hofmann A, de Jong PT. Determinants of optic disk characteristics in a general population: The Rotterdam Study. Ophthalmology. 1999;106:1588–96. doi: 10.1016/S0161-6420(99)90457-8. [DOI] [PubMed] [Google Scholar]
- 10.Hoffmann EM, Bowd C, Medeiros FA, Boden C, Grus FH, Bourne RR, et al. Agreement among 3 optical imaging methods for the assessment of optic disc topography. Ophthalmology. 2005;112:2149–56. doi: 10.1016/j.ophtha.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 11.Haley PR, Mitchell P, Smith W, Wang JJ. Relationship between cup-disc ratio and optic disc diameter: The Blue Mountain Eye Study. Aust NZJ Ophthalmol. 1997;25:S99–101. doi: 10.1111/j.1442-9071.1997.tb01771.x. [DOI] [PubMed] [Google Scholar]
- 12.Crowston JG, Hopley CR, Healey PR, Lee A, Mitchell P Blue Mountain s Eye Study. The effect of optic disc diameter on vertical cup to disc ratio percentiles in a population based cohort: The Blue Mountains Eye Study. Br J Ophthalmol. 2004;88:766–70. doi: 10.1136/bjo.2003.028548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramakrishnan R, Mittal S, Ambatkar S, Kader MA. Retinal nerve fibre layer thickness measurements in normal Indian population by optical coherence tomography. Indian J Ophthalmol. 2006;54:11–5. doi: 10.4103/0301-4738.21608. [DOI] [PubMed] [Google Scholar]
- 14.Mikelberg FS, Drance SM, Yidegiligne HM, White VA, Schulzer M. Relation between optic nerve axon number and axon diameter to scleral canal area. Ophthalmology. 1991;98:60–3. doi: 10.1016/s0161-6420(91)32341-8. [DOI] [PubMed] [Google Scholar]
- 15.Jonas JB. Optic disk size correlated with refractive error. Am J Ophthalmol. 2005;139:346–8. doi: 10.1016/j.ajo.2004.07.047. [DOI] [PubMed] [Google Scholar]


