Abstract
A 54-year-old diabetic female presented with orbital abscess and corneal infiltrate 3 days after deep posterior subtenon triamcinolone acetonide injection in her right eye. This was administered immediately after focal laser photocoagulation for diabetic macular edema. The orbital abscess and corneal infiltrate responded to systemic and topical antibiotics.
Keywords: Diabetes mellitus, orbital abscess, subtenon triamcinolone
Posterior subtenon injections of corticosteroids have been widely used for treatment of cystoid macular edema following uveitis and intraocular surgeries. They are increasingly used nowadays for the management of diabetic macular edema.1 The main advantage is maximum concentration at the macula which is the desired site of action with minimal side-effects. We herein report of a case of orbital abscess following deep posterior subtenon triamcinolone injection.
Case Report
A 54-year-old female patient presented to us with pain, swelling of lids of the right eye (RE) associated with intense chemosis and congestion of the conjunctiva. She was a known diabetic since 20 years and a hypertensive since 15 years. She had received posterior subtenon triamcinolone 20 mg injection with a 20-gauge veinflow canula in her RE immediately following focal laser treatment 3 days back for diabetic macular edema. At presentation her vision in RE was hand movement close to face (HMCF) and the same in the left eye (LE). Intraocular pressure could not be measured in RE due to massive lid edema. It was recorded as 14 mmHg in LE. The RE revealed lid edema with erythema [Fig. 1A]. The temperature of the overlying skin was raised but there was no palpable mass. The conjunctiva was congested and chemosed. Extraocular movements were limited in all directions of gaze in RE. In LE the movements were full in all directions. On forcibly lifting the upper lid of RE there was frank white tenacious discharge from the site of subtenon injection along with necrosis of the surrounding conjunctiva and peripheral corneal infiltrate [Fig. 1B]. Pupillary reaction was normal. Posterior segment examination showed proliferative diabetic retinopathy (PDR) with clinically significant macular edema (CSME) in both eyes.
Figure 1A.

(A) Swelling and erythema of right lid at presentation
Figure 1B.

(B) Note the area of corneal infiltrate alongwith conjunctival infection and discharge from the site of injection
Microbiological investigation of the discharge and infiltrate showed the presence of gram-positive cocci in clusters but no growth was observed on culture. Her fasting blood sugar was 284 mg% at presentation. Thereafter she was started on insulin infusion along with intravenous ciprofloxacin 500 mg twice daily, vancomycin 1 g twice a day and metrogyl 80 mg twice daily along with topical moxifloxacin 0.3% six times a day and atropine thrice a day. She had previously received injection cefazolin and ciprofloxacin elsewhere for 1 day. Computed tomography (CT) of head was consistent with diagnosis of orbital abscess [Fig. 1C] with no involvement of optic nerve. There was no evidence of intracranial involvement.
Figure 1C.

(C) CT scan of orbit shows proptosis, hypoechoic lesion with hyperechoic borders localized in preseptal tissues and anterior orbit with surrounding preseptal soft tissue swelling extending nasally and temporally
Over the next 3 days there was very little improvement. At this moment oral linazolid 500 mg twice a day was added to the drug regimen suspecting methicillin and vancomycin-resistant Staphylococcus aureus. There was remarkable improvement in the ensuing 48 h. Lid edema reduced considerably along with decrease in conjunctival chemosis and congestion. Extraocular movements improved and the discharge was seemingly much less than before. The above treatment continued for a period of 7 days. At 3 weeks follow-up all parameters were normal except for adjacent conjunctival and corneal scarring [Fig. 1D]. Visual acuity improved to 20/200. There was no restriction of ocular movements.
Figure 1D.
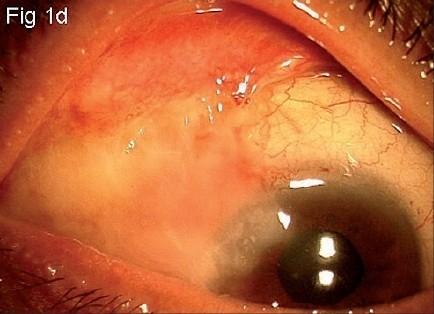
(D) Right eye showing area of conjunctival scarring and adjacent corneal opacity at 3 weeks follow-up
Discussion
Subtenon injections of steroids are commonly used in the treatment of macular edema associated with diabetes and uveitis. In general, patients with recalcitrant macular edema do not respond to focal laser treatment and require adjunctive subtenon injection of steroid. Complications though rare include inadvertent intravascular injection, globe perforation, cataract formation, ptosis, orbital fat atrophy or allergic reaction.2 Bakri et al. injected posterior subtenon triamcinolone in patients at least 3 months after laser treatment with minimal side-effects.3 Transient rise in intraocular pressure was observed in three eyes and ptosis in two eyes. In another study by Javadzadeh et al., a similar protocol for treating recalcitrant diabetic macular edema was followed.1 Only two cases in their series developed focal conjunctival necrosis over the site of injection. Orbital cellulitis has been seen after anterior subtenon injection of local anesthetic agent for cataract surgery.4 Recently, Oh et al. reported a case of periocular abscess which presented 1 month following posterior subtenon injection of triamcinolone and panretinal photocoagulation.5
Asymptomatic orbital abscess presenting 3 weeks following posterior subtenon injection of triamcinolone has been reported.6 However, acute orbital abscess is a previously unrecognized complication of this procedure. Our case highlights the fact that posterior subtenon triamcinolone injection should preferably be avoided at the same time as laser photocoagulation. Coupling solution used during focal laser treatment may have contaminated the conjunctival sac causing localized infection. Uncontrolled diabetes may have also contributed. It is well known that after posterior subtenon injection of anesthetic solution, nearly 50% of the solute resides in the orbital tissues anterior to the globe equator.7 In such a situation injection of deep posterior subtenon corticosteroid may have created a similar tract for the infection to present as an orbital abscess.
References
- 1.Javadzadeh A. The effect of posterior subtenon methyllprednisolone acetate in refractory diabetic macular oedema: A prospective non randomized interventional case series. BMC Ophthalmol. 2006;6:15–29. doi: 10.1186/1471-2415-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dafflon ML, Tran VT, Guex-Crosier Y, Herbort CP. Posterior sub- tenon′s steroid injections for the treatment of posterior ocular inflammation: Indications, efficacy and side effects. Graefes Arch Clin Exp Ophthamol. 1999;237:289–95. doi: 10.1007/s004170050235. [DOI] [PubMed] [Google Scholar]
- 3.Bakri SJ, Kaiser PK. Posterior subtenon triamcinolone acetonide for refractory diabetic macular edema. Am J Ophthalmol. 2005;139:290–4. doi: 10.1016/j.ajo.2004.09.038. [DOI] [PubMed] [Google Scholar]
- 4.Dahlmann AH, Appaswamy S, Headon MP. Orbital cellulitis following sub-tenon′s anaesthesia. Eye. 2002;16:200–1. doi: 10.1038/sj.eye.6700055. [DOI] [PubMed] [Google Scholar]
- 5.Oh IK, Baek S, Huh K, Oh J. Periocular abscess caused by Pseudallescheria boydii after a posterior subtenon injection of triamcinolone acetonide. Graefes Arch Clin Exp Ophthalmol. 2007;245:164–6. doi: 10.1007/s00417-006-0325-3. [DOI] [PubMed] [Google Scholar]
- 6.Engelman CG, Palmer JD, Jose S. Orbital abscess following subtenon triamcinolone injection. Arch Ophthalmol. 2004;122:654–5. doi: 10.1001/archopht.122.4.654. [DOI] [PubMed] [Google Scholar]
- 7.Niemi-Murola L, Krootila K, Kivisaari R, Kangasmaki A, Kivisaari L, Maunuksela EL. Localization of local anesthetic solution by magnetic resonance imaging. Ophthalmology. 2004;111:342–7. doi: 10.1016/j.ophtha.2003.05.026. [DOI] [PubMed] [Google Scholar]


