Abstract
Ocular complications are known to occur as a result of human immunodeficiency virus (HIV) disease. They can be severe leading to ocular morbidity and visual handicap. Cytomegalovirus (CMV) retinitis is the commonest ocular opportunistic infection seen in acquired immune deficiency syndrome (AIDS). Though posterior segment lesions can be more vision-threatening, there are varied anterior segment manifestations which can also lead to ocular morbidity and more so can affect the quality of life of a HIV-positive person. Effective antiretroviral therapy and improved prophylaxis and treatment of opportunistic infections have led to an increase in the survival of an individual afflicted with AIDS. This in turn has led to an increase in the prevalence of anterior segment and adnexal disorders. Common lesions include relatively benign conditions such as blepharitis and dry eye, to infections such as herpes zoster ophthalmicus and molluscum contagiosum and malignancies such as squamous cell carcinoma and Kaposi′s sarcoma. With the advent of highly active antiretroviral therapy, a new phenomenon known as immune recovery uveitis which presents with increased inflammation, has been noted to be on the rise. Several drugs used in the management of AIDS such as nevirapine or indinavir can themselves lead to severe inflammation in the anterior segment and adnexa of the eye. This article is a comprehensive update of the important anterior segment and adnexal manifestations in HIV-positive patients with special reference to their prevalence in the Indian population.
Keywords: Acquired immune deficiency syndrome, anterior segment lesions, highly active antiretroviral therapy, herpes zoster ophthalmicus, human immunodeficiency virus, immune recovery uveitis, Kaposi′s sarcoma, molluscum contagiosum
Ocular complications are common in human immunod- eficiency virus (HIV)-infected individuals with at least 50–75% of infected individuals expected to develop ocular disease at some point of time during the course of the disease in the pre- highly active antiretroviral therapy (HAART) era.1,2 Opportunistic infections develop when there is a deterioration of the immune status of the individual which can be measured with the help of CD4 cell counts. Posterior segment lesions, especially cytomegalovirus (CMV) retinitis, are associated with severe visual morbidity. Corneal and anterior segment lesions affect more than 50% of all HIV patients. Ocular adnexal complications, seen in about 25% of patients, can be a sign of severe systemic immunosuppression.3 Introduction of HAART has dramatically changed the scenario of the acquired immune deficiency syndrome (AIDS) epidemic. One of the hallmarks of progressive immune deficiency is a steady decline in the absolute number of CD4+ T-lymphocytes.4 Treatment of HIV infection with these regimens seeks to inhibit progression to AIDS (defined by a CD4 cell count of <200 cells/mm3) or death. This is by reducing plasma HIV RNA to permanently low levels, reduction in the viral load and a rise in CD4 cell counts which helps in improvement in the immune status of the individual.5 With the advent of HAART, HIV and AIDS-related morbidity and mortality have drastically decreased in the developed world.6-8 Patients on HAART are less likely to be affected by blinding posterior segment infections and there has been a marked reduction even in the occurrence of anterior segment and adnexal lesions. Though not all anterior segment diseases are vision-threatening, they can modify quality of life of patients and do require immediate ophthalmic care.9 More than 90% of HIV-infected individuals live in developing nations. In developing regions like India and the African continent there has been an explosive increase in the number of people with HIV disease, contributing to more than two-thirds of the world′s population of HIV-infected individuals. It is compounded by the fact that in these areas, patients have little or no access to HAART. As of December 2005, it was estimated that 40.3 million people worldwide were infected with HIV. In addition, there were 4.9 million newly diagnosed cases in 2005.10 For many poor countries, there may be no greater or more immediate threat to public health and economic growth than HIV.11 In African populations, anterior segment and external ocular diseases, such as squamous cell carcinoma, seem to predominate among ophthalmic problems.9
HAART-led immune recovery acts like a double-edged sword. Clinical immune recovery is, in general, of great benefit to the patient. But 10–25% of people initiated on HAART, experience ″immune recovery″ or immune reconstitution inflammatory problems, the majority of which are dermatologic.12 Immune recovery or immune reconstitution inflammatory syndrome (IRIS) refers to the acute immune-mediated inflammatory response to dormant antigens that occurs when CD4 cell counts rise after treatment with HAART.13-15
HAART-mediated improvement of immune function in patients with AIDS may also alter the way the eye responds to both opportunistic infections, especially CMV and to treatment, resulting in changes in the clinical manifestations of the ocular lesions. There have been newer ocular diseases; both in the anterior and posterior segments, in these patients on HAART.7 Few of the drugs used in the management of opportunistic infections in AIDS can also cause anterior segment manifestations. The purpose of this article is to provide a comprehensive update of the important anterior segment and adnexal manifestations in HIV-positive patients with special reference to their prevalence in the Indian population.
Anterior segment manifestations in an HIV-infected individual can be grouped into those caused due to the disease itself and those related to its management.
-
Anterior segment lesions due to HIV
-
Infections
- Viral
- Bacterial
- Fungal
- Protozoal
- Others
- Neoplasia
- Others
-
-
Iatrogenic/post-treatment manifestations
- Immune recovery uveitis
- Drug-induced uveitis
Anterior segment lesions due to HIV disease
Infections
Viral diseases
Herpes zoster ophthalmicus (HZO) is caused by varicella zoster virus (VZV) which causes varicella (chicken pox) and herpes zoster (shingles). Over 90% of the population develops clinical or serologic evidence of infection with VZV by adolescence, and the prevalence is almost 100% by age 60 years.9,16
The virus usually remains latent in sensory neurons. In immunocompetent individuals, latent VZV has been detected in 65-90% of trigeminal, 50-80% of thoracic, and 70% of geniculate ganglia.9 It can reactivate in response to local surgery/trauma or in the setting of depressed cell-mediated immunity (associated with aging, malignancies such as Hodgkin′s disease/leukemia or immunosuppressive treatment).
Herpes zoster eventually occurs in 10-20% of all individuals and reactivation in the ophthalmic division of the trigeminal nerve gives rise to HZO.9
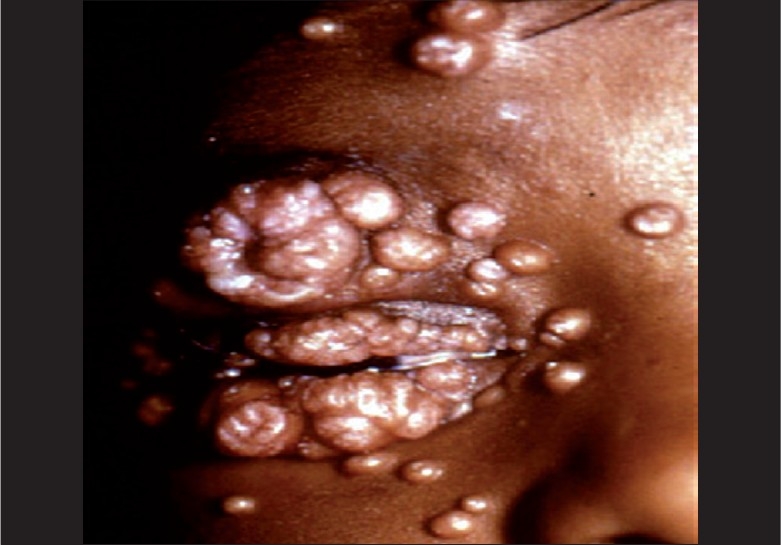
It is characterized by vesiculobullous rash over the distribution of the ophthalmic branch of the trigeminal nerve [Figure 1] and may be associated with dendritiform and stromal keratitis, conjunctivitis, blepharitis, uveitis (with secondary glaucoma), hemorrhagic hypopyon,17 scleritis, retinitis18 or encephalitis. Tissue damage can be mediated through a necrotizing vasculitis.
Figure 1.

Herpes zoster ophthalmicus in a patient with AIDS
Incidence of HZO is greater in HIV-infected individuals than in non-infected, age-adjusted populations. Approximately 5–15% of HIV-positive patients are co-infected with herpes zoster, but only half of these individuals are at risk of ocular involvement.3 It can even be an initial manifestation of HIV. Hodge and associates found that HIV-infected individuals had a relative incident risk ratio for HZO of 6.6:1, when compared to individuals who are HIV-negative.1
In immunosuppressed individuals, herpes zoster is more likely to be severe, prolonged, and can lead to viremia, which may result in visceral or neurologic infection, leading to increased morbidity and mortality.9 Herpes zoster presenting in any apparently healthy young individual (<45 years) with these characteristics and without any obvious cause of immunosuppression should be investigated for HIV. Diagnosis of HZO is mainly clinical. To confirm a clinical diagnosis, however, various tests are available, including virus cultures, Tzanck smears, polymerase chain reaction (PCR) techniques for VZV DNA, fluorescent antibody testing, and antigen detection by direct immunofluoresence.19
In immunocompetent hosts, the virus has not been recovered by culture beyond the first 48 h of the disease. VZV DNA has been detected on the ocular surface for as long as 34 days after the onset of rash and in excised corneal buttons obtained during penetrating keratoplasty up to eight years after active disease.20
Treatment of HZO in individuals with HIV disease requires aggressive initial treatment, with intravenous acyclovir, followed by a prolonged course of oral antivirals as ″maintenance therapy,″ to prevent recurrence.9 The regime is intravenous acyclovir (10 mg/kg of body weight eight-hourly for seven days followed by an oral maintenance regimen of 800 mg five times a day for at least three to six weeks). Early initiation of systemic anti-viral therapy can reduce the duration of skin lesions and ocular complications by about 50%.9,21 The most appropriate duration of treatment for HZO has not been determined for the general population, although virus has been recovered from skin lesions up to 14 days into the course of infection. In resistant cases, famciclovir can be used three times daily in 500 mg dosages as well. In cases of resistance to thymidine kinase-dependent acyclovir or famciclovir, IV foscarnet may be used.22
A recent study18 showed infection with Herpes zoster to be severe, of long duration with higher rate of complications, increased need for hospitalization and higher rates of recurrent herpes zoster in group patients. Though post-herpetic neuralgia is a very frequent complication for both groups (HIV-positive and HIV-negative) its duration is longer in HIV/AIDS patients in comparison to HIV-negative group. There was no significant difference in the severity, duration or complications of the disease among male and female patients. HIV-infected individuals with HZO should have regular fundus evaluation until complete resolution of skin vesicles to watch for retinal infection.19
In a series of young individuals with HZO, those with risk factors for HIV infection had a higher rate of ocular complications (57%) than those without risk factors (38%).23
There has also been a reported increase in the incidence of herpes zoster in patients with AIDS immediately after therapy with protease inhibitors. Martinez et al.,24 found that within a median follow-up of 64 weeks (range, 34 to 103 weeks), 14 patients (7%) had a first episode or a recurrence of herpes zoster (6.2 episodes per 100 patient-years). No episodes of zoster were diagnosed before Week 4. They noted that the risk of zoster was independent of age, sex, type of protease inhibitor and CD4 + counts and viral load at baseline and Month 1. But an increase in CD8 + lymphocyte proportion at Month 1 of > 5% (HR 32; 95% CI 8.1 to 126.4) was independently associated with the risk of herpes zoster. This will help identifying persons at risk and prophylactic antiviral therapy can be instituted in them.
In our series of 120 patients on HAART seen between 2002 and 2005, seven patients had HZO and in five of these patients the CD4 counts were more than 200 cells/cu mm (unpublished data) and in two of these patients, the counts were between 150 to 200 cells/cu mm. HZO seems to occur in patients on HAART with improvement in their immune status. In a previous study from our institute in the pre-HAART era, there was only one patient with HZO out of a series of 100 patients.25
Some patients develop severe and debilitating post-herpetic neuralgia after resolution of the oculocutaneous lesions. Post- herpetic neuralgia can be treated with analgesics and anti- inflammatory drugs such as topical lidocaine cream (5%).26 Acyclovir therapy, initiated within 72 h of onset of skin rash, also reduces the risk of post-herpetic neuralgia.27 Pain relief in severe cases may be obtained with amitryptiline (25 mg to 150 mg orally daily in slowly increasing dose). Opioids have been found to be more potent and better tolerated than tricyclic antidepressants.28 Currently, gabapentin, up to 3,600 mg per day in three divided doses, has emerged as a first-line treatment for post-herpetic neuralgia and is found to be effective for treatment of pain and sleep interference associated with this condition.29
Viral keratitis
VZV and herpes simplex virus (HSV) are the most common etiologic agents of infectious keratitis.3 Although ocular infection is usually known to occur with HSV-1, documented cases of HSV–2 ocular infection have also been reported, including an individual with AIDS who was found to have simultaneous HSV-1 and -2 infection of the cornea.30
Herpetic keratitis can cause painful and often recurrent corneal ulcerations with a characteristic branching or dendritic pattern on slit-lamp examination. Epithelial keratitis typically appears in conjunction with follicular conjunctivitis and vesicular eyelid lesions; stromal and interstitial keratitis present less frequently. HSV keratitis is usually associated with corneal scarring, iritis and raised intraocular pressure and is known to recur frequently.
VZV keratitis may be accompanied by herpes zoster ophthalmicus in 65% of individuals with HZO, dendritiform lesions occur in up to 51% cases.9 Among those with corneal involvement, neurotrophic keratitis occurs in 25% and rarely, superadded bacterial infection can occur. Both epithelial and stromal disease has been described in the absence of skin lesions, a condition named as herpetic zoster sine herpete.31,32
HIV-infected patients with HZO are more likely to experience corneal involvement than their non-infected counterparts (89% vs. 65%), and corneal perforation also has an increased incidence according to one report.3 Individuals with AIDS can develop a chronic VZV infection of the corneal epithelium. Engstrom and Holland33 were the first to describe such a case; their patient had been treated presumptively. Lesions of chronic VZV epithelial keratitis in HIV-infected individuals can be pleomorphic, often with multiple components and associated with thickened opaque epithelium. They tend to be more delicate and lacy in appearance than the discrete dendrites of HSV epithelial keratitis or the classic, broad, plaque-like VZV dendrites that have been described at the onset of HZO. Peripheral ulcerative keratitis can occur in HIV-infected patients with HZO,9 as described previously in individuals with debilitating systemic disorders.
Corneal stromal involvement has been reported infrequently in individuals with AIDS or other immunosuppressed states. It is thus possible that the T-lymphocyte dysfunction in HIV- infected individuals may actually protect them from developing HSV stromal disease.9 Punctate corneal dendritic lesions described in HIV-positive hosts do not seem to differ from those seen in immunocompetent hosts except that they may be larger and more peripherally located. The pathognomonic bulb-tipped branching pattern seen on slit-lamp examination, however, remains the same in both groups and helps confirm the clinical diagnosis.
In a series of six patients with AIDS and HSV keratitis, Young and associates34 emphasized atypical clinical features of the disease, including a predilection for marginal, as opposed to central epithelial keratitis, a relative resistance to treatment (mean healing time of three weeks compared to the two weeks typical for immunocompetent individuals); and more frequent and lengthier recurrences. Similar observations were made in a retrospective cohort study35 which compared the incidence and clinical course of HSV keratitis over a 11–year period among 1,800 patient visits of individuals who were HIV-infected and 48,200 patient visits of individuals who were not HIV-infected, and it found no difference between the groups with regard to incidence of HSV keratitis, lesion type (epithelial versus stromal), lesion location (central versus peripheral), and treatment time. The recurrence rate, however, was 2.48 times more frequent in HIV-infected individuals.
More recently, a 2003 study from Nigeria found that half of 10 healthy-appearing individuals with HZO were found to be infected with HIV.36 Confirmed HIV seropositivity was 16.7% in recurrent HSK cases as against 3.3% in the matched first-episode HSK cases in an Indian study.37
Overall recurrence rates were significantly higher amongst the HIV-positive group even among other studies. After the first episode a site of chronic latent infection is established in the cornea and immunosuppression as a result of HIV infection probably may impair those mechanisms which are normally responsible for containing such an infection in the cornea.38
Diagnosis of HSV infection is primarily clinical, but laboratory studies, including viral culture, direct fluorescent antibody tests for HSV antigens and PCR techniques for HSV DNA can help to confirm the diagnosis, especially in cases of diagnostic dilemma.9 Treatment is commonly with topical agents such as acyclovir eye ointment five times daily or vidarabine ointment 3% five times daily and cycloplegics. Debridement of the ulcer using a cotton-tip applicator may increase the healing rate.
According to Herpetic Eye Disease Study group39 long-term suppressive oral acyclovir therapy (400 mg twice daily for one year) reduces the rate of recurrent HSV epithelial keratitis and stromal keratitis. The benefit of acyclovir is greatest for patients who have experienced prior HSV stromal keratitis. Long-term suppressive oral acyclovir therapy may also benefit HIV-infected individuals with a history of HSV eye disease, in light of the increased recurrence rate of HSV keratitis in this population.9
In resistant strains, famciclovir 125 to 500 mg three times daily or foscarnet can be substituted instead of acyclovir. Bodaghi et al.,40 described a case of a young HIV-positive female with chronic keratitis not responding to acyclovir. Conventional virological methods remained inconclusive and in situ hybridization and polymerase chain reaction (PCR) rapidly confirmed the diagnosis of HSV-1 keratitis. The thymidine kinase gene sequence revealed the presence of five variations and they postulated that this gene may be associated with acyclovir resistance.
Interferon has also been used for the treatment and prevention of HSV epithelial keratitis. Patients with a history of HZO on a HAART regimen may be susceptible to immune recovery. In VZV-mediated stromal keratitis, as reported by Naseri and Margolis,41 in a patient with history of resolved HZO, T cells presumably recognized and responded to residual VZV antigens in the corneal stroma to cause the keratitis. HAART (with protease inhibitors) may potentially double the incidence of herpes zoster and related ocular involvement in AIDS patients, although treatment with nucleoside analogue reverse transcriptase inhibitors does not pose the same risk. Thus, there is an increased risk of recurrence in HIV-infected individuals and stromal keratitis as part of IRIS.
Cytomegalovirus keratitis
CMV which can be transmitted by blood, saliva, breast milk, and mucous membrane contact is usually asymptomatic in immunocompetent individuals, but can sometimes produce transient conjunctivitis. CMV retinitis is the commonest AIDS- related opportunistic infection of the eye, but rarely involves the anterior segment tissues. CMV infection of the iris has been reported in a patient with CMV retinitis.42 CMV has been reported to be associated with both epithelial and/or stromal keratitis, although both conditions are probably uncommon.9
Corneal endothelial deposits have been described in about 80% of eyes with CMV retinitis.43 These asymptomatic lesions, seen in up to 81% of cases of HIV/AIDS-related CMV retinitis appear as linear or stellate lesions and form a reticular pattern.44 Best visualized in retroillumination, they are commonly found in the inferior cornea. These deposits are known to be composed of fibrin and macrophages, with no active CMV infection. CMV has been proven, with the help of aqueous humor analysis to be the causative agent of endothelitis and anterior uveitis in immunocompetent patients.45,46
CMV has been reported to be associated with anterior uveitis with sectoral iris atrophy47 and with secondary glaucoma48 in immunocompetent individuals. Similar cases have not been found in patients with AIDS.
For immunocompromised patients of any age, restoring immunity prevents herpes virus disease, as seen in the case of CMV in AIDS patients on HAART. Specific antiviral therapy during the initial period after transplantation could prevent reactivation of HSV or CMV in seropositive recipients. Prophylaxis with antivirals against CMV and other viruses prior to clinically detectable lesions, remains controversial and the relative merits/limitations of each approach may guide the choice.49 In addition to HIV/AIDS, current antiviral therapy has been focusing primarily on herpes viruses, hepatitis viruses and influenza.50
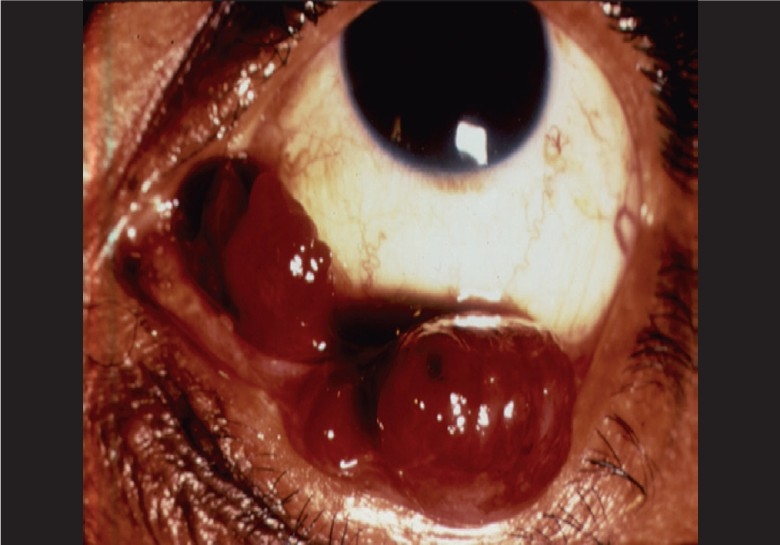
Molluscum contagiosum6
Molluscum contagiosum, caused by a large DNA pox virus, affects up to 5% of HIV-infected patients and is highly contagious. It is transmitted by direct contact and has an incubation period of six to eight weeks.9 It is seen in children and young adults.
In immunocompetent children, it is transmitted via fomites, infected clothing, bed linen, and towels. They are usually fewer in number, smaller in size and are found to be unilateral. In young adults, it is typically transmitted sexually. Children aged 0 to14 years account for 90% of molluscum contagiosum episodes.51 In HIV-positive individuals, such lesions can occur in the eyelid and conjunctiva and are characteristically larger in number and size, often confluent, bilateral and resistant to therapy [Figure 2]. Face, trunk and genitalia are commonly affected. A distribution in the chin-strap region is common in HIV-positive patients. The lash line should be examined carefully in all patients with chronic conjunctivitis so as not to miss a molluscum lesion.
Figure 2.
Molluscum contagiosum in a child with AIDS
Molluscum contagiosum is believed to be more common in persons with AIDS due to profound dysfunction of T-lymphocyte-mediated immune response, associated with HIV infection. Molluscum contagiosum lesions of the eyelid have even been reported as the initial clinical manifestation of HIV disease.52,53 It is characterized by pink or pearly white wart-like nodules on the skin. Sections of the lesions show large (20 to 30 microns) eosinophilic hyaline inclusion bodies which displace the nuclei to the margin. These bodies are composed of large numbers of virus particles, embedded in a protein matrix. Rarely, conjunctival involvement in AIDS patients can also result in nodular pink lesions.3
Treatment: Typically these lesions regress on their own in immunocompetent individuals. Treatment options include usage of topical agents like phenol and trichloroacetic acid or serial applications of liquid nitrogen. Incision with or without curettage, excision, and cryotherapy are equally effective. Despite treatment, eyelid lesions will commonly recur in patients with AIDS, usually within six to eight weeks, corresponding to the incubation period of the virus. Administration of HAART with restoration of immunity leads to complete resolution of disseminated molluscum contagiosum and limitation of infection.
Although HIV-infected individuals suffer from an aggressive form, severe inflammatory reaction is not known even in those patients with coexistent conjunctivitis. Paradoxically, the phenomenon of IRIS after treatment with HAART can also cause new presentations of molluscum contagiosum in patients without a history of the disease.54 Severe conjunctival inflammation may be noted till regression of lesions. Even though immune reconstitution does not prevent recurrence of molluscum contagiosum, newer lesions when they develop are less severe, as in immunocompetent individuals.3
Bacterial diseases
Bacterial keratitis
Several studies comparing ocular flora in immunocompromised and immunocompetent individuals have found varied results.9 Ocular flora in HIV-infected individuals is not very different from that in the general population but the risk of infection with this ″normal flora″ may be greater for severely immunosuppressed individuals.3,9 Staphylococcus aureus, Staphylococcus epidermidis and Pseudomonas aeruginosa are most frequently implicated.55 Klebsiella oxytoca, Streptococcus, Bacillus, Micrococcus, Capnocytophaga, and most recently Acanthameba species have also been shown to cause disease, with some cases of recalcitrant infection requiring keratoplasty and even evisceration of the globe.56-58 HIV-infected hosts may be predisposed towards these spontaneous bacterial keratitides because of preexisting keratoconjunctivitis sicca (KCS) and viral keratitis, which create corneal epithelial erosions allowing subsequent bacterial entry. Other risk factors predisposing to epithelial defects include the use of crack cocaine by HIV- infected individuals.9
The clinical presentation of bacterial keratitis in HIV-infected individuals differs from that in the general population. In immunosuppressed individuals, they are usually bilateral, involve multiple pathogens and carry a higher risk of perforation. There have been reports of eyes having to be eventually enucleated despite having been treated with intensive antibiotic therapy, based on in vitro sensitivities, for more than two weeks.59
Paucity of inflammation in immunosuppressed patients also contributes to delay in diagnosis and treatment. In contrast, only one eye of the 12 cases of pseudomonal corneoscleritis in immunocompetent individuals from the same institution required enucleation.
Neisseria gonorrhoeae infection is usually transmitted to the eye by accidental auto-inoculation and can be unilateral or bilateral. They cause membranous or pseudomembranous conjunctivitis with ulceration, scarring and perforation as the organism can penetrate the normal corneal epithelium. HIV infection can modify the typical host response to gonococci, resulting in more severe ocular signs and symptoms.60 Gram staining and culture helps in the identification of the etiological agent. Systemic treatment with ceftriaxone or other appropriate antibiotics must be used to treat gonococcal conjunctivitis. Topical therapy alone will be ineffective.
Protozoal diseases
Microsporidial keratitis 2
Microsporidia are spore-forming, obligate intracellular, protozoan parasites. They are known to cause gastrointestinal complications such as hepatitis, enteritis and peritonitis in patients with AIDS. Among the very few reports of human microsporidiosis reported prior to the AIDS epidemic,61 three cases had some form of immunosuppression. They occur when the CD4 + counts drop to about 100cells/cu.mm. Thirty-nine to 44% of HIV-infected individuals with diarrhoea are infected with microsporidia, in comparison to only 2.3% of HIV-infected individuals without diarrhoea.
AIDS-associated microsporidial keratoconjunctivitis is characterized by bilateral superficial punctate epithelial keratitis, white intraepithelial infiltrates, mild anterior chamber reactions, and conjunctivitis in the form of mild conjunctival follicular hypertrophy.62,63 Patients may complain of photophobia and grittiness.3 Vision loss is secondary to keratitis.
Diagnosis is by Gram or Giemsa stain and spores from conjunctival scrapings or corneal biopsies can be easily seen with Masson trichrome or Giemsa stain. Immunofluorescence and electron microscopy can help confirm the diagnosis.3 Ocular microsporidiasis should be suspected in all HIV-positive patients with persistently negative cultures for epithelial keratitis. Although HAART has been shown to alleviate and resolve microsporidial keratoconjunctivitis in HIV-positive hosts64,65 post-immune recovery-mediated microsporidial keratoconjunctivitis reactivation has also been reported.66
Treatment:67 Fumagillin 70 mg/mL eye drops are used indefinitely in HIV-positive individuals. Albendazole 400 mg twice daily orally should be used as an adjunct for the management of systemic infection.
Toxoplasmosis
Toxoplasma gondii can cause necrotizing retinochoroiditis with associated anterior uveitis as secondary phenomena, but the parasite does not extend beyond the neural retina. In contrast, severely immunosuppressed individuals with AIDS can develop a primary toxoplasmic anterior uveitis, which can occur in the absence of retinal lesions. Iris nodules with tissue destruction and severe anterior segment inflammation have been noted.68 Inflammation responds well to anti-parasitic therapy but not to corticosteroids alone.
Mycobacterial disease
Tuberculosis (TB) implies the presence of active disease from infection with the acid-fast bacillus.69 Mycobacterium tuberculosis is the commonest systemic opportunistic infection associated with AIDS even though ocular TB is not as common.70 It is important to consider it as a differential diagnosis, especially in India.
Bouza et al.17 reported an unusually high (18%) incidence of ocular tuberculosis in a cohort of 100 randomly selected tuberculosis patients examined systematically for ocular tuberculosis from 300 culture proven cases for acid fast bacilli. Eleven of these patients were HIV positive. Eleven patients had no symptoms attributable to ocular tuberculosis.
M. avium, a species of nontuberculous mycobacteria, was reported to be the cause of endophthalmitis72 with an intense inflammatory reaction and hypopyon in an individual with AIDS who had a history of disseminated M. avium infection. Prominent iris nodules caused by M. avium complex (MAC) has also been observed as the initial manifestation of panophthalmitis in an individual with AIDS.
Changed presentation in the setting of HIV disease is not known, especially in case of anterior segment lesions in TB.9 Clinical manifestations include ulcers, tubercles, granular masses or pedunculated polypoid tumors.9 Patients may present with localized nodule in the eyelid simulating chalazion. Orbital and lacrimal gland involvement by M. tuberculosis leads to localized granuloma73 though unusually they can present as a conjunctival mass.70
Infection of the iris can present either with or without iris nodules. TB is also a known cause of uveitis, although it is uncommon, even among those with systemic TB.71 Presentations of ocular tuberculosis in HIV-infected individuals is also similar. An association between corneal phlyctenulosis74 and tuberculoprotein hypersensitivity is suggested by both epidemiologic and experimental studies, although it is rarely seen in patients with pulmonary TB.
TB may cause interstitial keratitis with stromal infiltration. Interstitial keratitis secondary to TB may be associated with uveitis. It may occur as an isolated finding or in association with scleritis. Sclerokeratitis can be seen with peripheral stromal inflammation in a triangular fashion associated with localized scleritis. Localized lesions are focal elevated nodules of the sclera that may undergo necrosis leading to scleromalacia and scleral perforation if untreated. Diffuse scleritis is less common than localized nodular scleritis.
M. tuberculosis infection of the conjunctiva may involve the palpebral, bulbar, or forniceal conjunctiva. Tuberculous conjunctivitis is a very rare condition in the developed world. In recalcitrant cases of chronic red eye,75 a definitive diagnosis requires the identification of Mycobacterium tuberculosis organisms in conjunctival biopsy specimens, either through microscopic detection of acid-fast bacilli or through more sensitive culture techniques. Keratoconjunctivitis may occur in association with cutaneous TB.76 While intraocular disease is mostly a secondary infection, cutaneous TB is almost always primary.77
Tuberculosis can present as a granulomatous type of anterior uveitis, even in HIV-infected individuals and the inflammatory reaction correlates with the level of CD4 cell counts.
Treatment: Systemic anti-tuberculous therapy (ATT) with drugs such as isoniazid, rifampin, pyrazinamide and ethambutol is important as pulmonary or other foci of disease may coexist. Modified DOTS regimen (Directly Observed Treatment Short course) is the recommended regime in India. Specific ocular treatment should be instituted along with ATT. There have been reports of scleral TB responding favorably to additional topical (every 2 h) and subconjunctival (every three days) streptomycin sulfate along with ATT9 with healing of the lesion. In individuals with HIV infection, therapy may require longer duration and additional drugs. Newer drugs have also been incorporated in the ATT group of drugs, especially in the newer setting of multidrug-resistant TB, particularly in case of HIV-infected individuals. These include quinolones, newer rifamycins like rifabutin and macrolides antibiotics.
Fungal infections
In the general population, fungal corneal ulcers are rare in the absence of preceding trauma, ocular surface disease or corticosteroid therapy while HIV/AIDS patients can develop spontaneous fungal infections. In developed countries, Candida and cryptococci are the most prevalent ocular fungal pathogens among HIV-positive hosts. Candida causes anterior segment keratitis. Cryptococci commonly triggers posterior segment pathology although they can sometimes cause conjunctivitis, limbal infection and iris granulomas.78 Cryptococcus albidus causing scleral ulceration has been reported.79 Histoplasma and Pneumocystis can also cause anterior segment manifestations9 but are not as commonly reported from India. Fungal keratitides have a more acute and protracted course in the HIV/AIDS population, and are more likely to result in bilateral disease with corneal perforation.80 Hence, culture or biopsy of lesions is important for HIV-infected patients with ocular surface infections, to differentiate between bacterial and fungal etiology.
Spirochaetal infections
Treponema pallidum: Ocular syphilis caused by Treponema pallidum tends to present with more aggressive, severe and relapsing manifestations in HIV-positive hosts as compared with immunocompetent hosts.81-83 It is frequently the presenting symptom of co-infection with HIV. All patients with syphilis should be evaluated for HIV and vice versa, as syphilis may follow a more aggressive course in individuals who are concurrently infected with HIV. Disruption of the mucosal epithelial barrier in syphilitic ulcers, which contain mononuclear cells (targets of HIV infection) may be the mechanism by which syphilis increases the risk of HIV acquisition.9 Anterior segment manifestations of syphilis include chancres of the conjunctiva (primary syphilis), conjunctivitis (secondary syphilis) and gummata (late syphilis). Conjunctivitis can be granulomatous and histologically similar to sarcoidosis.9
It is the most common bacterial cause of uveitis in HIV- positive hosts with an incidence of 0.6%. It tends to be more severe and consists of panuveitis in conjunction with anterior uveitis.82,83 Eighty-five per cent of HIV-positive patients with ophthalmic syphilis have coexisting neurosyphilis, and hence all patients must undergo cerebrospinal fluid analysis to rule out neurosyphilis when syphilitic uveitis is first diagnosed.84 The diagnosis of syphilis involves a good clinical history in addition to serologic screening and confirmatory tests such as the rapid plasma reagin or fluorescent treponemal antibody absorbent tests, respectively. Direct examination using darkfield microscopy or biopsy of suspicious lesions can be performed if results are uncertain.85 Isolated episcleritis and scleritis are uncommon during any stage of the disease, but when present, are usually features of secondary or late syphilis.86
Treatment of ocular syphilis is similar to that of neurosyphilis. The most effective treatment involves high-dose IV penicillin G 12 to 24 million units/d for 14 days.87,88 Because of the high rate of relapse, HIV-positive patients are recommended to have extensive follow-up subsequently at least for two years.
Anterior uveitis2: Anterior uveitis may be rarely associated with HIV disease, especially as part of a CMV retinitis (CMVR) or a syphilitic panuveitis. Symptomatic anterior uveitis is rare in HIV-positive patients.88 Uveitis associated with CMVR is seen rarely. More severe anterior chamber inflammation may be seen with toxoplasmic or syphilitic retinochoroiditis/ panuveitis,89 or rarely in other infectious retinitis such as acute retinal necrosis.
HIV itself has been isolated from tears, conjunctiva, cornea, aqueous humor, iris, sclera, vitreous humor and retina, and has been suspected as a cause of intraocular inflammation occasionally, in the absence of other pathogens.9
″Multifocal punctate retinal infiltrates,″ an unusual inflammatory condition, which can have associated anterior segment inflammation, may also be a direct effect of HIV infection.90 Diagnosis requires slit-lamp examination, and therapy is primarily directed at identifying an infectious etiology. Topical steroids are often employed but must be used with caution and in combination with appropriate antimicrobial therapy.
Other adnexal infectious lesions
Preseptal cellulitis
Staphylococcus aureus is the most common cause of cutaneous and systemic bacterial infection in HIV-positive patients. It is found in the nasal mucosa in more than twice91 the number of HIV patients when compared to normal individuals. Treatment is similar to that in immunocompetent individuals.
Abscess in the eyelid
Infections of the eyelid and conjunctiva are rare in patients with AIDS. Dermal abscesses due to staphylococci, acid-fast bacilli and CMV have been reported in molluscum lesions in patients with AIDS indicating the tendency of such lesions to acquire secondary infection.53,92 Diagnosis is by smear and culture.
Treatment: Topical and systemic antibiotics.
Neoplasms
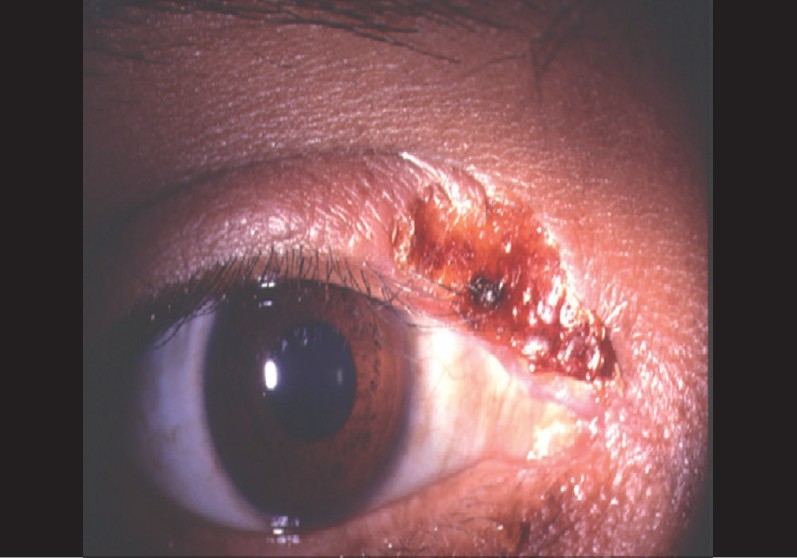
Kaposi′s sarcoma of the eyelid and the conjunctiva
Kaposi′s sarcoma (KS) is a highly vascular mesenchymal tumor that appears as multiple purple-to-red nodules on the skin and mucous membranes31 [Figure 3]. It occurs in 30% of all AIDS patients in the US. In approximately 10-20% of individuals with HIV-associated KS, the tumor involves the eyelids, conjunctiva and in rare cases, the orbit. KS can be an initial manifestation of AIDS. Kaposi′s sarcoma of the eyelid and conjunctiva is rare in the Indian subcontinent possibly due to the rarity of the probable causative agent, human herpes virus 8. The appearance of KS on the eyelids is similar to the lesions elsewhere on the skin. It can mimic a chalazion and can be seen in the upper or lower lids. Conjunctival lesions93,94 may be seen in any part of the palpebral or bulbar conjunctiva but are usually more common in the inferior fornix. Kaposi′s sarcoma in the conjunctiva can be mistaken for a subconjunctival hemorrhage or pyogenic granuloma.4
Figure 3.
Kaposi's sarcoma in a patient with AIDS
Histologically, KS can resemble an angioma, hemangioma, lymphangioma or granulation tissue. It has a complex arrangement of capillary channels and vascular spaces (″slits″) without endothelium.9 Malignant spindle cells are arranged around these incomplete vascular spaces. The spindle- shaped interstitial cells are of vascular endothelial origin, with vacuolated cytoplasm which may demonstrate mitotic activity.95 Dugel and associates96 have classified adnexal KS lesions clinically and histopathologically into three stages. Stage I and II lesions are flat (less than 3 mm in height), patchy and of less than four months duration; Stage III lesions are nodular, greater than 3 mm in height and greater than four months in duration. This staging may have prognostic value regarding the course of disease and response to therapy.97
Treatment: KS does not invade the eye and treatment is not necessary if it is asymptomatic and is cosmetically acceptable. The principal goal of therapy in this population is palliation when disease is disfiguring, painful, or interfering with function. Local measures are often used for patients with minimal cutaneous KS.9 However, if it causes discomfort either through a mass effect, secondary corneal change or if it is disfiguring, then treatment can be planned. Under these circumstances, it may be treated by cryotherapy, surgical excision (if the lesion is small), radiation and/or chemotherapy.
Radiation therapy11 is effective in treating the eyelid and conjunctival lesions but can lead to loss of lashes, irritation, conjunctivitis, conjunctival keratinization, cicatricial ectropion and retinopathy.
Systemic agents are warranted for patients with advanced disease such as extensive cutaneous disease, visceral disease or lymphedema. Intralesional vinblastin or interferon alpha12 have known to produce good results. Associated systemic KS is best treated with systemic chemotherapy. Anterior segment fluorescein angiography can be helpful in demarcating the 1 to 2 mm tumor-free zone during surgery. Magnetic resonance imaging can be helpful in the diagnosis and follow-up of patients after treatment.98
Widespread success of HAART in treating AIDS-related primary KS has definitely reduced the need for other management options too, controlling the disease such as chemotherapy or irradiation.99
Immune reconstitution inflammatory syndrome-related complications causing lethal KS have been reported. Early intervention with a limited course of systemic chemotherapy (while still maintaining a HAART regimen) is successful in treating the flare-ups100,101
Squamous cell carcinoma of conjunctiva
SCC is the third most common neoplasm associated with HIV after KS and lymphoma.3 The eyelid and conjunctiva are seldom a site of initial presentation in the developed world though they can be the first presenting sign of AIDS in up to 50% of African patients though it is not as common in the Indian population102-104 [Figure 4]. Africans are more at risk due to the increased prevalence of the human papilloma virus.
Figure 4.

Squamous cell carcinoma as an initial manifestation of AIDS
When the tumor is found at the limbus, gonioscopy has to be performed to rule out intraocular extension.2 Most commonly noted clinical characteristics of conjunctival SCC are corneal overriding (90%), fast growth rates (with a rate of 1mm in 83%), tumors larger than 1 cm (17%), changes in conjunctival color (66%), and nasal locations (66%).3
Twenty percent of benign pterygia may harbour SCC/ Carcinoma in situ and hence pathology review should be done for all conjunctival lesions. HIV testing should be carried out in all cases of conjunctival tumors for patients living in high-risk areas as it may be the first sign of HIV-positivity.104
Treatment: Wide excision with frozen section monitoring of the margins. HAART has been known to cause complete regression of invasive conjunctival SCC in an HIV-positive patient,105 which raises the possibility of antiviral therapy as an alternative to radical surgery.
Cutaneous and conjunctival lymphoma2
Non-Hodgkin′s lymphoma (NHL) accounts for 3.5–5% of AIDS-defining illnesses9 and tends to be of a higher grade of malignancy in HIV patients106 and can affect eyelids and conjunctiva. NHL should be suspected in all HIV patients of any age who have prominent vitreous cells, with or without subretinal exudation. Intraocular lymphoma usually is seen with CD4 cell counts of less than 50 cells/ml. Intraocular lymphoma can also cause anterior chamber reactions.107,108 Primary NHL has also been found in eyelids of patients with AIDS, presenting as rapidly enlarging erythematous lesions.109 Lid swelling, ptosis, proptosis, gaze palsies and ophthalmoplegia have been reported.110 NHL can mimic keratoconjunctivitis sicca. Hence any AIDS patient with dry eye, especially if unresponsive to therapy, should be viewed with suspicion, more so, if it is unilateral and/or the patient has associated systemic symptoms such fever, malaise or weight loss.2
Treatment: Radiotherapy and/or chemotherapy such as vinblastin. Interferon alpha has also been used as part of treatment modality.
Bacillary angiomatosis
Bacillary angiomatosis (BA)111,112 is the vascular proliferative form of infection with Bartonella organisms. Bacillary angiomatosis was first described in 1983 in a patient infected with the HIV. Subsequently, it has been described in patients following organ transplants and in other immunocompromised persons. Patients with HIV disease are at increased risk of developing BA when their CD4 T-cell count <200 cells/cu.mm. It can mimic KS and is important that this entity is differentiated from the more lethal KS.
Other manifestations
Keratoconjunctivitis sicca (KCS)
Dry eye occurs in 20–38.8% of HIV-positive hosts in the later stages of AIDS.3 It is thought to be due to lymphocytic infiltration of the lacrimal gland. Afflicted individuals are more susceptible to bacterial keratitis and abnormalities in the composition of the tear film are typically present.113 Etiology is multifactorial and is due to the combined effects of HIV- mediated inflammatory destruction of primary and accessory lacrimal glands and to the direct conjunctival damage due to the HIV virus itself.112 The virus is also postulated to play a significant role in spontaneous corneal thinning and perforation which is observed in some infected patients.114-116 Contrary to its effect on many other ocular HIV/AIDS-related diseases, HAART has not played a part in significantly reducing the prevalence of KCS.3
Management options include artificial tears, long-acting lubricants and punctal occlusion in severe cases.
Conjunctivitis
Non-specific, culture-negative conjunctivitis has been reported to be seen in less than 1% of patients with HIV.2 Rarely cytomegalovirus or cryptococcus can be the causative organism. Grams stain and culture need to be done before labeling it as non-infective. Biopsy is indicated in unresponsive cases.
Trichomegaly
Acquired trichomegaly or hypertrichosis2 have been described, especially in the late stages. Exact cause is not known although drug toxicity,117 elevated viral load have been suggested to play a role. It has to be treated if annoying or if cosmetically unacceptable.
Conjunctival microvasculopathy
Seventy to eighty per cent patients have some form of asymptomatic conjunctival microvascular changes. These include segmental vascular dilatation and narrowing, microaneurysm formation, comma-shaped vascular fragment and visible granularity to the flowing blood column (sludging).2 These are seen more commonly near the inferior limbus and have a good correlation with the occurrence of retinal microvasculopathy. Exact cause is not known. It is postulated to be due to increased plasma viscosity, endothelitis or immune complex deposition. No treatment is required
Angle closure glaucoma2
Acute angle closure glaucoma has been described in association with uveal effusion118 syndrome in patients infected with HIV. Cause of angle closure glaucoma is not known. Intraocular inflammation is minimal but can be severe in case of primary choroidal inflammation with secondary exudative retinal detachment. B-scan ultrasonography and ultrasound biomicroscopy helps in clinching the diagnosis. Treatment includes cycloplegics, corticosteroids, aqueous suppressants, hyperosmolar agents and surgical drainage of suprachoroidal fluid.
Atopic Dermatitis
Atopic dermatitis has a prevalence of approximately 10% in the general population and can be the first ocular manifestation in some individuals after HIV infection.9 Treatment of atopic eyelid disease in both HIV-infected and HIV-negative individuals consists of topical corticosteroids.
Blepharitis
Blepharitis is more common and more serious in HIV-infected individuals. Blepharitis and an eyelid ulcer have been reported as the initial manifestations of HIV disease92 [Figure 5]. New-onset chronic relapsing episodes of blepharitis, which began months to years after starting indinavir therapy have also been reported. These patients presented with retinoid effects such as desquamative or erosive chelitis, mucocutaneous xerosis, alopecia, asteatotic eczema, paronychia, and ingrown nails.119
Figure 5.
A patient of ulcerative blepharitis with AIDS
Iatrogenic and post-treatment manifestations
Immune recovery uveitis
The clinical picture of HIV-associated eye disease has changed dramatically since the introduction of HAART.8 Although direct infectious destruction of tissue is less severe, inflammatory infiltration is augmented, and this gives rise to a situation that is open to misinterpretation. Before the introduction of protease inhibitors, patients with CMV retinitis typically had CD4 T-lymphocyte counts less than 50 cells/cu.mm with minimal intraocular inflammation.120,121 Significant intraocular inflammation has now been reported in some patients with CMV retinitis who have had improved immune function with HAART [Figure 6]. Immune recovery uveitis, which involves mainly the anterior uvea and vitreous, is often associated with a marked disturbance of visual function.122,123 Hence it is important to identify early the occurrence of this phenomenon in patients on HAART on their path to immune recovery. Prompt treatment with anti-inflammatory therapy including steroids prevents vision loss due to immune recovery uveitis.
Figure 6.
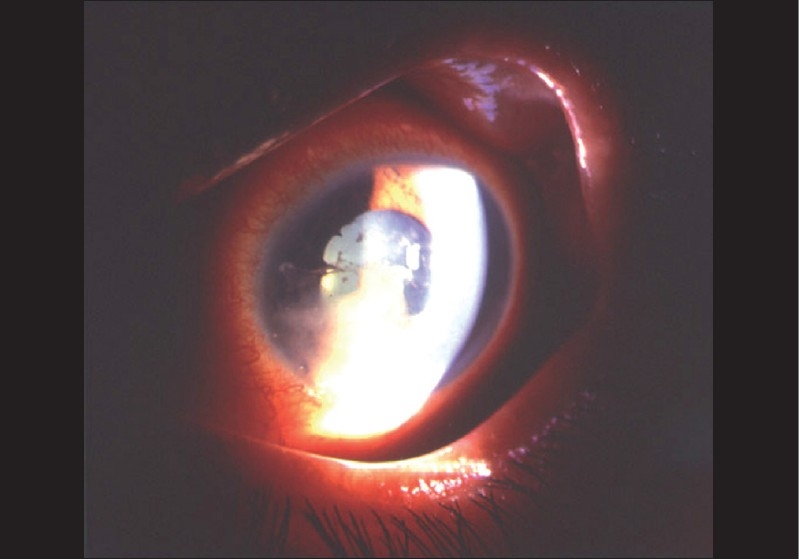
Severe anterior uveitis with hypopyon in case of immune recovery uveitis with AIDS on protease inhibitor
Drug-induced uveitis
Another group of new diseases has been attributed to the toxic effects of drugs, i.e. of Rifabutin124 and Cidofovir.125 In both instances, a predominantly anterior form of uveitis develops, which is characterized by a discrepancy between clinical symptoms and morphological changes; the former condition is distinguished by severe pain, and the latter by marked inflammation.
Certain autoimmune syndromes (such as Reiter′s syndrome) may also be associated with iridocyclitis. Rare occurrences of an anterior uveitis secondary to sarcoidosis126 in a patient infected with HIV have been reported.
Symptomatic anterior uveitis in HIV-positive patients has been described by Verma et al.127 They reported 12 cases with varied etiology. They concluded that HIV-positive patients with symptoms of uveitis do not have active CMV retinitis and the ophthalmologist must search for other causes such as TB or lymphoma in those with granulomatous uveitis or herpes zoster in those with non-granulomatous uveitis.
Stevens-Johnson syndrome (SJS)
HIV-infected individuals are frequently exposed to many medications, especially drugs such as nevirapine, which are capable of causing hypersensitivity or toxic reactions. Altered cell-mediated immunity may also lead to increased risk of SJS as a response to infectious agents as well. Associated dry eye may aggravate the problems associated with SJS in HIV- infected individuals.9
Corneal phospholipidoses2
Vortex keratopathy or corneal phospholipidosis can be caused by antivirals such as ganciclovir, acyclovir or atovaquone, a drug used in the treatment of toxoplasmosis. Patients may be asymptomatic or may complain of a mild irritation, foreign body sensation or photophobia. Characteristic whorl-like pattern of gray white opacities is seen at the level of the corneal epithelium.
Summary
Anterior segment manifestations in the eye in HIV-infected individuals are varied. They can be vision-threatening. More commonly, they can affect the quality of life which ultimately hampers the rehabilitation of the individual which is the ultimate goal. Multiple pathogens can be found in the same individual. They can give a definitive clue to HIV-related systemic disorder. As is the case with other lesions, even anterior segment and adnexal manifestations in these patients may have atypical presentations. They may present with minimal inflammatory reactions and thus every clinician should be aware of such atypical manifestations.
In India, viral infections, such as herpes zoster, herpes simplex and molluscum contagiosum are more common. Patients with herpetic eye disease in AIDS may need long-term maintenance prophylaxis therapy. Herpes zoster ophthalmicus is seen relatively more commonly in the HAART era in India.
HAART has definitely reduced the frequency of rare malignancies such as KS and SCC though ocular KC is not commonly seen in India. There are not many studies regarding the prevalence of other anterior segment manifestations in HIV-infected individuals in India.
Patients on HAART can develop severe inflammatory reaction due to immune recovery phenomenon which can cause severe ocular morbidity. Hence it is important that ophthalmologists be aware of this emerging new phenomenon so that it is managed appropriately.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Hodge WG, Seif SR, Margolis TP. Ocular opportunistic infection incidences among patients who are HIV positive compared to patients who are HIV negative. Ophthalmology. 1998;105:895–900. doi: 10.1016/S0161-6420(98)95033-3. [DOI] [PubMed] [Google Scholar]
- 2.Kestelyn PG, Cunningham ET., Jr HIV-AIDS and blindness. Bull World Health Organ. 2001;79:208–13. [PMC free article] [PubMed] [Google Scholar]
- 3.Adnexal and anterior segment manifestations of HIV-AIDS. Int Ophthalmol Clin. 2007;47:15–32. doi: 10.1097/IIO.0b013e318036bcc4. [DOI] [PubMed] [Google Scholar]
- 4.Meyer D. Eye signs that alert the clinician to a diagnosis of AIDS. SADJ. 2005;60:386–7. [PubMed] [Google Scholar]
- 5.Kahraman G, Krepler K, Franz C, Ries E, Maar N, Wedrich A, et al. Seven years of HAART impact on ophthalmic management of HIV-infected patients. Ocul Immunol Inflamm. 2005;13:213–8. doi: 10.1080/09273940490912443. [DOI] [PubMed] [Google Scholar]
- 6.Kirk O, Mocroft A, Lundgren JD EuroSIDA-studiet. Decline in AIDS and death rates in the EuroSIDA study: An observational study. Ugeskr Laeger. 2004;166:2572–6. [PubMed] [Google Scholar]
- 7.Mesaric B, Lisic M, Kniewald T, Ugrinovic N, Begovac J. Ocular manifestations in patients with human immunodeficiency virus infection before and after the introduction of highly active antiretroviral therapy. Lijec Vjesn. 2005;127:123–8. [PubMed] [Google Scholar]
- 8.Arruda RF, Muccioli C, Belfort R., Jr Ophthalmological findings in HIV infected patients in the post-HAART (Highly Active Anti-retroviral Therapy) era, compared to the pre-HAART era. Rev Assoc Med Bras. 2004;50:148–52. doi: 10.1590/s0104-42302004000200029. [DOI] [PubMed] [Google Scholar]
- 9.Jeng BH, Holland GN, Lowder CY, Deegan WF, 3rd, Raizman MB, Meisler DM. Anterior segment and external ocular disorders associated with human immunodeficiency virus disease. Surv Ophthalmol. 2007;52:329–68. doi: 10.1016/j.survophthal.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 10. [last accessed on 2006 May 13]. Available from: http://www.unaids.org-epi-2005-doc-report_pdf.asp.
- 11.Belfort R., Jr The ophthalmologist and the global impact of the AIDS epidemic: LV Edward Jackson Memorial lecture. Am J Ophthalmol. 2000;129:1–8. doi: 10.1016/s0002-9394(99)00428-6. [DOI] [PubMed] [Google Scholar]
- 12.Ratnam I, Chiu C, Kandala NB, Easterbrook PJ. Incidence and risk factors for immune reconstitution inflammatory syndrome in an ethnically diverse HIV type 1-infected cohort. Clin Infect Dis. 2006;42:418–27. doi: 10.1086/499356. [DOI] [PubMed] [Google Scholar]
- 13.French MA, Price P, Stone SF. Immune restoration disease after antiretroviral therapy. AIDS. 2004;18:1615–27. doi: 10.1097/01.aids.0000131375.21070.06. [DOI] [PubMed] [Google Scholar]
- 14.Cooney EL. Clinical indicators of immune restoration following highly active antiretroviral therapy. Clin Infect Dis. 2002;34:224–33. doi: 10.1086/323898. [DOI] [PubMed] [Google Scholar]
- 15.Jabs DA, Bartlett JG. AIDS and Ophthalmology: A period of transition. Am J Ophthalmol. 1997;124:227–33. doi: 10.1016/s0002-9394(14)70789-5. [DOI] [PubMed] [Google Scholar]
- 16.Liesegang TJ. Varicella-zoster virus eye disease. Cornea. 1999;18:511–31. [PubMed] [Google Scholar]
- 17.Biswas J, Samanta TK, Madhavan HN, Kumarasamy N, Solomon S. Acute panuveitis with haemorrhagic hypopyon as a presenting feature of acquired immunodeficiency syndrome (AIDS) Indian J Ophthalmol. 2000;48:311–2. [PubMed] [Google Scholar]
- 18.Sellitti TP, Huang AJ, Schiffman J, Davis JL. Association of herpes zoster ophthalmicus with acquired immunodeficiency syndrome and acute retinal necrosis. Am J Ophthalmol. 1993;116:297–301. doi: 10.1016/s0002-9394(14)71346-7. [DOI] [PubMed] [Google Scholar]
- 19.Sharvadze L, Tsertsvadze T, Gochitashvili N, Bolokadze N, Dolmazashvili E. Peculiarities of herpes zoster in immunocompetent and immunocompromised hosts. Georgian Med News. 2006;141:50–3. [PubMed] [Google Scholar]
- 20.Zaal MJ, Volker-Dieben HJ, Wienesen M, D′Amaro J, Kijlstra A. Longitudinal analysis of varicella-zoster virus DNA on the ocular surface associated with herpes zoster ophthalmicus. Am J Ophthalmol. 2001;131:25–9. doi: 10.1016/s0002-9394(00)00652-8. [DOI] [PubMed] [Google Scholar]
- 21.Severson EA, Baratz KH, Hodge DO, Burke JP. Herpes zoster ophthalmicus in Olmsted County, Minnesota: Have systemic antivirals made a difference? Arch Ophthalmol. 2003;121:386–90. doi: 10.1001/archopht.121.3.386. [DOI] [PubMed] [Google Scholar]
- 22.Biswas J, Fogla R, Gopal L, Narayana KM, Banker AS, Kumarasamy N, et al. Current approaches to diagnosis and management of ocular lesions in human immunodeficiency virus positive patients. Indian J Ophthalmol. 2002;50:83–96. [PubMed] [Google Scholar]
- 23.Sandor EV, Millman A, Croxson TS, Mildvan D. Herpes zoster ophthalmicus in patients at risk for the acquired immune deficiency syndrome (AIDS) Am J Ophthalmol. 1986;101:153–5. doi: 10.1016/0002-9394(86)90585-4. [DOI] [PubMed] [Google Scholar]
- 24.Martinez E, Gatell J, Moran Y, Aznar E, Buira E, Guelar A, et al. High incidence of herpes zoster in patients with AIDS soon after therapy with protease inhibitors. Clin Infect Dis. 1998;27:1510–3. doi: 10.1086/515019. [DOI] [PubMed] [Google Scholar]
- 25.Biswas J, Madhavan HN, George AE, Kumarasamy N, Solomon S. Ocular lesions associated with HIV infection in India: A series of 100 consecutive patients evaluated at a referral center. Am J Ophthalmol. 2000;129:9–15. doi: 10.1016/s0002-9394(99)00415-8. [DOI] [PubMed] [Google Scholar]
- 26.Kost RG, Straus SE. Postherpetic neuralgia-pathogenesis, treatment and prevention. N Engl J Med. 1996;35:32–42. doi: 10.1056/NEJM199607043350107. [DOI] [PubMed] [Google Scholar]
- 27.Vander SM, Carrasco D, Lee P, Tyring SK. Reduction of postherpetic neuralgia in herpes zoster. J Cutan Med Surg. 2001;5:409–16. doi: 10.1007/s102270000024. [DOI] [PubMed] [Google Scholar]
- 28.Raja SN, Haythornthwaite JA, Pappagallo M, Clark MR, Travison TG, Sabeen S, et al. Opioids versus antidepressants in postherpetic neuralgia: A randomized, placebo-controlled trial. Neurology. 2002;59:1015–21. doi: 10.1212/wnl.59.7.1015. [DOI] [PubMed] [Google Scholar]
- 29.Rowbotham M, Harden N, Stacey B, Bernstein P, Magnus-Miller L. Gabapentin for the treatment of postherpetic neuralgia: A randomized controlled trial. JAMA. 1998;280:1837–42. doi: 10.1001/jama.280.21.1837. [DOI] [PubMed] [Google Scholar]
- 30.Charles NC, Akhtar S. Herpes simplex types 2 membranous conjunctivitis in acquired immune deficiency syndrome. Ophthal Pract. 2002;20:342–4. [Google Scholar]
- 31.Intraocular inflammation and uveitis. USA: American Academy of Ophthalmology; 2005-2006. Basic and clinical science course; pp. 241–62. [Google Scholar]
- 32.Silverstein BE, Chandler D, Neger R, Margolis TP. Disciform keratitis: A case of herpes zoster sine herpete. Am J Ophthalmol. 1997;123:254–5. doi: 10.1016/s0002-9394(14)71044-x. [DOI] [PubMed] [Google Scholar]
- 33.Engstrom RE, Holland GN. Chronic herpes zoster virus keratitis associated with the acquired immunodeficiency syndrome. Am J Ophthalmology. 1988;105:556–8. doi: 10.1016/0002-9394(88)90252-8. [DOI] [PubMed] [Google Scholar]
- 34.Young TL, Robin JB, Holland GN, Hendricks RL, Paschal JF, Engstrom RE, Jr, et al. Herpes simplex keratitis in patients with acquired immune deficiency syndrome. Ophthalmology. 1989;96:1476–9. doi: 10.1016/s0161-6420(89)32706-0. [DOI] [PubMed] [Google Scholar]
- 35.Hodge WG, Margolis TP. Herpes simplex virus keratitis among patients who are positive or negative for human immunodeficiency virus: An epidemiologic study. Ophthalmology. 1997;104:120–4. doi: 10.1016/s0161-6420(97)30351-0. [DOI] [PubMed] [Google Scholar]
- 36.Owoeye JF, Ademola-Popoola DS. Herpes zoster infection and HIV seropositivity among eye patients-University of Ilorin Teaching Hospital experience. West Afr J Med. 2003;22:136–8. doi: 10.4314/wajm.v22i2.27933. [DOI] [PubMed] [Google Scholar]
- 37.Pramod NP, Hari R, Sudhamathi K, Ananadakannan K, Thyagarajan SP. Influence of human immunodeficiency virus status on the clinical history of herpes simplex keratitis. Ophthalmologica. 2000;214:337–40. doi: 10.1159/000027516. [DOI] [PubMed] [Google Scholar]
- 38.Hendricks RL. An immunologist′s view of the herpes simplex keratitis. Cornea. 1997;16:503–6. [PubMed] [Google Scholar]
- 39.Herpetic Eye Disease Study Group. Oral acyclovir for herpes simplex virus eye disease: Effect on prevention of epithelial keratitis and stromal keratitis. Arch Ophthalmol. 2000;118:1030–6. [PubMed] [Google Scholar]
- 40.Bodaghi B, Mougin C, Michelson S, Agut H, Dighiero P, Offret H, et al. Acyclovir-resistant bilateral keratitis associated with mutations in the HSV-1 thymidine kinase gene. Exp Eye Res. 2000;71:353–9. doi: 10.1006/exer.2000.0886. [DOI] [PubMed] [Google Scholar]
- 41.Naseri A, Margolis TP. Varicella zoster virus immune recovery stromal keratitis in a patient with AIDS. Br J Ophthalmol. 2001;85:1390–1. doi: 10.1136/bjo.85.11.1384h. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cheng L, Rao NA, Keefe KS, Avila CP, Jr, Macdonald JC, Freeman WR. Cytomegalovirus iritis. Ophthalmic Surg Lasers. 1998;29:930–2. [PubMed] [Google Scholar]
- 43.Walter KA, Coulter VL, Palay DA, Taravella MJ, Grossniklaus HE, Edelhauser HF. Corneal endothelial deposits in patients with cytomegalovirus retinitis. Am J Ophthalmol. 1996;121:391–6. doi: 10.1016/s0002-9394(14)70435-0. [DOI] [PubMed] [Google Scholar]
- 44.Brody JM, Butrus SI, Laby DM, Ashraf MF, Rabinowitz AI, Parenti DM. Anterior segment findings in AIDS patients with cytomegalovirus retinitis. Graefes Arch Clin Exp Ophthalmol. 1995;233:374–6. doi: 10.1007/BF00200488. [DOI] [PubMed] [Google Scholar]
- 45.Chee SP, Bacsal K, Jap A, Se-Thoe SY, Cheng CL, Tan BH. Corneal endotheliitis associated with evidence of cytomegalovirus infection. 2007;114:798–803. doi: 10.1016/j.ophtha.2006.07.057. [DOI] [PubMed] [Google Scholar]
- 46.Koizumi N, Yamasaki K, Kawasaki S, Sotozono C, Inatomi T, Mochida C, et al. Cytomegalovirus in aqueous humor from an eye with corneal endotheliitis. Am J Ophthalmol. 2006;141:564–5. doi: 10.1016/j.ajo.2005.09.021. [DOI] [PubMed] [Google Scholar]
- 47.Markomichelakis NN, Canakis C, Zafirakis P, Marakis T, Mallias I, Theodossiadis G. Cytomegalovirus as a cause of anterior uveitis with sectoral iris atrophy. Ophthalmology. 2002;109:879–82. doi: 10.1016/s0161-6420(02)00961-2. [DOI] [PubMed] [Google Scholar]
- 48.van Boxtel LA, van der Lelij A, van der Meer J, Los LI. Cytomegalovirus as a cause of anterior uveitis in immunocompetent patients. Ophthalmology. 2007;114:1358–62. doi: 10.1016/j.ophtha.2006.09.035. [DOI] [PubMed] [Google Scholar]
- 49.Fillet AM. Prophylaxis of herpesvirus infections in immunocompetent and immunocompromised older patients. Drugs Aging. 2002;19:343–54. doi: 10.2165/00002512-200219050-00003. [DOI] [PubMed] [Google Scholar]
- 50.Rottinghaus ST, Whitley RJ. Current non-AIDS antiviral chemotherapy. Exp Rev Anti Infect Ther. 2007;5:217–30. doi: 10.1586/14787210.5.2.217. [DOI] [PubMed] [Google Scholar]
- 51.Pannell RS, Fleming DM, Cross KW. The incidence of molluscum contagiosum, scabies and lichen planus. Epidemiol Infect. 2005;133:985–91. doi: 10.1017/S0950268805004425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Leahey AB, Shane JJ, Listhaus A, Trachtman M. Molluscum contagiosum eyelid lesions as the initial manifestation of acquired immunodeficiency syndrome. Am J Ophthalmol. 1997;124:240–1. doi: 10.1016/s0002-9394(14)70791-3. [DOI] [PubMed] [Google Scholar]
- 53.Biswas J, Therese L, Kumarasamy N, Solomon S, Yesudian P. Lid abscess with extensive molluscum contagiosum in a patient with acquired immunodeficiency syndrome. Indian J Ophthalmol. 1997;45:234–6. [PubMed] [Google Scholar]
- 54.Ratnam I, Chiu C, Kandala NB, Easterbrook PJ. Incidence and risk factors for immune reconstitution inflammatory syndrome in an ethnically diverse HIV type 1-infected cohort. Clin Infect Dis. 2006;42:418–27. doi: 10.1086/499356. [DOI] [PubMed] [Google Scholar]
- 55.Moraes HV., Jr Ocular manifestations of HIV-AIDS. Curr Opin Ophthalmol. 2002;13:397–403. doi: 10.1097/00055735-200212000-00010. [DOI] [PubMed] [Google Scholar]
- 56.Aristimuno B, Nirankari VS, Hemady RK, Rodrigues MM. Spontaneous ulcerative keratitis in immunocompromised patients. Am J Ophthalmol. 1993;115:202–8. doi: 10.1016/s0002-9394(14)73924-8. [DOI] [PubMed] [Google Scholar]
- 57.Hansen B, Kronborg G. Acanthamoeba keratitis in a non-contact lens wearer with human immunodeficiency virus. Scand J Infect Dis. 2003;35:207–9. doi: 10.1080/003655400310000157. [DOI] [PubMed] [Google Scholar]
- 58.Tandon R, Vajpayee RB, Gupta V, Vajpayee M, Satpathy G, Dada T. Polymicrobial keratitis in an HIV-positive patient. Indian J Ophthalmol. 2003;51:87–8. [PubMed] [Google Scholar]
- 59.Nanda M, Pflugfelder SC, Holland S. Fulminant pseudomonal keratitis and scleritis in human immunodeficiency virus-infected patients. Arch Ophthalmol. 1991;109:503–5. doi: 10.1001/archopht.1991.01080040071029. [DOI] [PubMed] [Google Scholar]
- 60.Lau RK, Goh BT, Estreich S, Cox SN, Levy I. Adult gonococcal keratoconjunctivitis with AIDS. Br J Ophthalmol. 1990;74:52. doi: 10.1136/bjo.74.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Bryan RT. Microsporidiosis as an AIDS-related opportunistic infection. Clin Infect Dis. 1995;21:S62–5. doi: 10.1093/clinids/21.supplement_1.s62. [DOI] [PubMed] [Google Scholar]
- 62.Friedberg DN, Stenson SM, Orenstein JM, Tierno PM, Charles NC. Microsporidial keratoconjunctivitis in acquired immunodeficiency syndrome. Arch Ophthalmol. 1990;108:504–8. doi: 10.1001/archopht.1990.01070060052047. [DOI] [PubMed] [Google Scholar]
- 63.Lowder CY, McMahon JT, Meisler DM, Dodds EM, Calabrese LH, Didier ES, et al. Microsporidial keratoconjunctivitis caused by septata intestinalis in a patient with acquired immunodeficiency syndrome. Am J Ophthalmol. 1996;121:715–7. doi: 10.1016/s0002-9394(14)70642-7. [DOI] [PubMed] [Google Scholar]
- 64.Carr A, Marriott D, Field A, Vasak E, Cooper DA. Treatment of HIV-1-associated microsporidiosis and cryptosporidiosis with combination antiretroviral therapy. Lancet. 1998;351:256–61. doi: 10.1016/S0140-6736(97)07529-6. [DOI] [PubMed] [Google Scholar]
- 65.Martins SA, Muccioli C, Belfort R, Jr, Castelo A. Resolution of microsporidial keratoconjunctivitis in an AIDS patient treated with highly active antiretroviral therapy. Am J Ophthalmol. 2001;131:378–9. doi: 10.1016/s0002-9394(00)00810-2. [DOI] [PubMed] [Google Scholar]
- 66.Gajdatsy AD, Tay-Kearney ML. Microsporidial keratoconjunctivitis after HAART. Clin Exp Ophthalmol. 2001;29:327–9. doi: 10.1046/j.1442-9071.2001.00443.x. [DOI] [PubMed] [Google Scholar]
- 67.Benson CA, Kaplan JE, Masur H, Pau A, Holmes KK, CDC Treating opportunistic infections among HIV-infected adults and adolescents: Recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association. MMWR Recomm Rep. 2004;53:1–112. [PubMed] [Google Scholar]
- 68.Cano-Parra JL, Diaz-LLopis ML, Cordoba JL, Gobernado ML, Navea AL, Menezo JL. Acute iridocyclitis in a patient with AIDS diagnosed as toxoplasmosis by PCR. Ocul Immunol Inflamm. 2000;8:127–30. [PubMed] [Google Scholar]
- 69.Helm CJ, Holland GN. Ocular tuberculosis. Surv Ophthalmol. 1993;38:229–56. doi: 10.1016/0039-6257(93)90076-j. [DOI] [PubMed] [Google Scholar]
- 70.Babu RB, Sudharshan S, Kumarasamy N, Therese KL, Biswas J. Ocular tuberculosis in acquired immunodeficiency syndrome. Am J Ophthalmol. 2006;142:413–8. doi: 10.1016/j.ajo.2006.03.062. [DOI] [PubMed] [Google Scholar]
- 71.Bouza E, Merino P, Munoz P, Sanchez-Carrillo C, Yáñez J, Cortés C. Ocular tuberculosis: A prospective study in a general hospital. Medicine (Baltimore) 1997;76:53–61. doi: 10.1097/00005792-199701000-00005. [DOI] [PubMed] [Google Scholar]
- 72.Cohen JI, Saragas SJ. Endophthalmitis due to Mycobacterium avium in a patient with AIDS. Ann Ophthalmol. 1990;22:47–51. [PubMed] [Google Scholar]
- 73.Gopal L, Rao SK, Biswas J, Madhavan HN, Agarwal S. Tuberculous granuloma managed by full thickness eye wall resection. Am J Ophthalmol. 2003;135:93–4. doi: 10.1016/s0002-9394(02)01858-5. [DOI] [PubMed] [Google Scholar]
- 74.Valentina C, Mircla C. Phlyctenular keratoconjunctivitis and lymph node tuberculosis. Ophthalmologia. 1999;48:15–8. [PubMed] [Google Scholar]
- 75.Jennings A, Bilous M, Asimakis P, Maloof AJ. Mycobacterium tuberculosis presenting as chronic red eye. Cornea. 2006;25:1118–20. doi: 10.1097/01.ico.0000240097.99536.82. [DOI] [PubMed] [Google Scholar]
- 76.Singal A, Aggarwal P, Pandhi D, Rohatgi J. Cutaneous tuberculosis and phlyctenular keratoconjunctivitis: A forgotten association. Indian J Dermatol Venereol Leprol. 2006;72:290–2. doi: 10.4103/0378-6323.26726. [DOI] [PubMed] [Google Scholar]
- 77.Dinning WJ, Marston S. Cutaneous and ocular tuberculosis: A review. J Royal Soc Med. 1985;78:576–81. doi: 10.1177/014107688507800711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Muccioli C, Belfort Junior R, Neves R, Rao N. Limbal and choroidal Cryptococcus infection in the acquired immunodeficiency syndrome. Am J Ophthalmol. 1995;120:539–40. doi: 10.1016/s0002-9394(14)72677-7. [DOI] [PubMed] [Google Scholar]
- 79.Garelick JM, Khodabakhsh AJ, Lopez Y, Bamji M, Lister M. Scleral ulceration caused by cryptococcus albidus in a patient with acquired immune deficiency syndrome. Cornea. 2004;23:730–1. doi: 10.1097/01.ico.0000126322.13143.7b. [DOI] [PubMed] [Google Scholar]
- 80.Acharya NR, Cunningham ET., Jr Corneal, anterior segment, and adnexal manifestations of human immunodeficiency virus. Int Ophthalmol Clin. 1998;38:161–77. doi: 10.1097/00004397-199803840-00015. [DOI] [PubMed] [Google Scholar]
- 81.McLeish WM, Pulido JS, Holland S, Culbertson WW, Winward K. The ocular manifestations of syphilis in the human immunodeficiency virus type 1-infected host. Ophthalmology. 1990;97:196–203. doi: 10.1016/s0161-6420(90)32605-2. [DOI] [PubMed] [Google Scholar]
- 82.Becerra LI, Ksiazek SM, Savino PJ, Marcus DK, Buckley RM, Sergott RC, et al. Syphilitic uveitis in human immunodeficiency virus-infected and non infected patients. Ophthalmology. 1989;96:1727–30. doi: 10.1016/s0161-6420(89)32657-1. [DOI] [PubMed] [Google Scholar]
- 83.Musher DM, Hamill RJ, Baughn RE. Effect of human immunodeficiency virus (HIV) infection on the course of syphilis and on the response to treatment. Ann Intern Med. 1990;113:872–81. doi: 10.7326/0003-4819-113-11-872. [DOI] [PubMed] [Google Scholar]
- 84.Aldave AJ, King JA, Cunningham ET., Jr Ocular syphilis. Curr Opin Ophthalmol. 2001;12:433–41. doi: 10.1097/00055735-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 85.Hall CS, Klausner JD, Bolan GA. Managing syphilis in the HIV- infected patient. Curr Infect Dis Rep. 2004;6:72–81. doi: 10.1007/s11908-004-0027-0. [DOI] [PubMed] [Google Scholar]
- 86.Moloney G, Branley M, Kotsiou G, Rhodes D. Syphilis presenting as scleritis in an HIV-positive man undergoing immune reconstitution. Clin Experiment Ophthalmol. 2004;32:526–8. doi: 10.1111/j.1442-9071.2004.00871.x. [DOI] [PubMed] [Google Scholar]
- 87.Hall CS, Klausner JD, Bolan GA. Managing syphilis in the HIV- infected patient. Curr Infect Dis Rep. 2004;6:72–81. doi: 10.1007/s11908-004-0027-0. [DOI] [PubMed] [Google Scholar]
- 88.Rosberger DF, Heinemann MH, Friedberg DN, Holland GN. Uveitis associated with human immunodeficiency virus infection. Am J Ophthalmol. 1998;125:301–5. doi: 10.1016/s0002-9394(99)80135-4. [DOI] [PubMed] [Google Scholar]
- 89.Doris JP, Saha K, Jones NP, Sukthankar A. Ocular syphilis: The new epidemic. Eye. 2006;20:703–5. doi: 10.1038/sj.eye.6701954. [DOI] [PubMed] [Google Scholar]
- 90.Levinson RD, Vann R, Davis JL, Friedberg DN, Tufail A, Terry BT, et al. Chronic multifocal retinal infiltrates in patients infected with human immunodeficiency virus. Am J Ophthalmol. 1998;125:312–24. doi: 10.1016/s0002-9394(99)80137-8. [DOI] [PubMed] [Google Scholar]
- 91.Tschachler E, Bergstresser PR, Stingl G. HIV-related skin diseases. Lancet. 1996;348:659–63. doi: 10.1016/S0140-6736(96)01032-X. [DOI] [PubMed] [Google Scholar]
- 92.Biswas J, Madhavan HN, Kumarasamy N, Solomon S. Blepharitis and lid ulcer as initial ocular manifestations in acquired immunodeficiency syndrome (AIDS) patients. Indian J Ophthalmol. 1997;45:233–4. [PubMed] [Google Scholar]
- 93.Schmid K, Wild T, Bolz M, Horvat R, Jurecka W, Zehetmayer M. Kaposi′s sarcoma of the conjunctiva leads to a diagnosis of acquired immunodeficiency syndrome. Acta Ophthalmol Scand. 2003;81:411–3. doi: 10.1034/j.1600-0420.2003.00105.x. [DOI] [PubMed] [Google Scholar]
- 94.Corti M, Solari R, de Carolis L, Corraro R. Eye involvement in AIDS-related Kaposi sarcoma. Enferm Infect Microbiol Clin. 2001;19:3–6. doi: 10.1016/s0213-005x(01)72539-6. [DOI] [PubMed] [Google Scholar]
- 95.Rutgers JL, Wieczorek R, Bonetti F, Kaplan KL, Posnett DN, Friedman-Kien AE, et al. The expression of endothelial cell surface antigens by AIDS-associated Kaposi′s sarcoma: Evidence for a vascular endothelial cell origin. Am J Pathol. 1986;122:493–9. [PMC free article] [PubMed] [Google Scholar]
- 96.Dugel PU, Gill PS, Frangieh GT, Rao NA. Ocular adnexal Kaposi′s sarcoma in acquired immunodeficiency syndrome. Am J Ophthalmol. 1990;110:500–3. doi: 10.1016/s0002-9394(14)77872-9. [DOI] [PubMed] [Google Scholar]
- 97.Dugel PU, Gill PS, Frangieh GT, Rao NA. Treatment of ocular adnexal Kaposi′s sarcoma in acquired immune deficiency syndrome. Ophthalmology. 1992;99:1127–32. doi: 10.1016/s0161-6420(92)31841-x. [DOI] [PubMed] [Google Scholar]
- 98.Scheschonka A, Mösch M, Krieglsteiner S, Turowski B, Zanella FE. Pre- and post treatment MR imaging in AIDS-related Kaposi sarcoma of the conjunctiva and lacrimal gland. AJNR Am J Neuroradiol. 2003;24:1327–9. [PMC free article] [PubMed] [Google Scholar]
- 99.International Collaboration on HIV and Cancer. Highly active antiretroviral therapy and incidence of cancer in human immunodeficiency virus-infected adults. J Natl Cancer Inst. 2000;92:1823–30. doi: 10.1093/jnci/92.22.1823. [DOI] [PubMed] [Google Scholar]
- 100.Crane HM, Deubner H, Huang JC, Swanson PE, Harrington RD. Fatal Kaposi′s sarcoma-associated immune reconstitution following HAART initiation. Int J STD AIDS. 2005;16:80–3. doi: 10.1258/0956462052932647. [DOI] [PubMed] [Google Scholar]
- 101.Connick E, Kane MA, White IE, Ryder J, Campbell TB. Immune reconstitution inflammatory syndrome associated with kaposi sarcoma during potent antiretroviral therapy. Clin Infect Dis. 2004;39:1852–5. doi: 10.1086/426078. [DOI] [PubMed] [Google Scholar]
- 102.Muccioli C, Belfort R, Burnier M, Rao N. Squamous cell carcinoma of the conjunctiva in a patient with the acquired immune deficiency syndrome. Am J Ophthalmol. 1996;121:94–6. doi: 10.1016/s0002-9394(14)70541-0. [DOI] [PubMed] [Google Scholar]
- 103.Fogla R, Biswas J, Krishnakumar S, Madhavan HN, Kumarasamy N, Solomon S. Squamous cell carcinoma of the conjunctiva as initial presenting sign in a patient with acquired immunodeficiency syndrome (AIDS) due to human immunodeficiency virus type-2. Eye. 2000;14:246–7. doi: 10.1038/eye.2000.65. [DOI] [PubMed] [Google Scholar]
- 104.Porges Y, Groisman GM. Prevalence of HIV with conjunctival squamous cell neoplasia in an African provincial hospital. Cornea. 2003;22:1–4. doi: 10.1097/00003226-200301000-00001. [DOI] [PubMed] [Google Scholar]
- 105.Holkar S, Mudhar HS, Jain A, Gupta M, Rogstad KE, Parsons MA, et al. Regression of invasive conjunctival Squamous carcinoma in an HIV-positive patient on antiretroviral therapy. Int J STD AIDS. 2005;16:782–3. doi: 10.1258/095646205774988028. [DOI] [PubMed] [Google Scholar]
- 106.Sandler AS, Kaplan L. AIDS lymphoma. Curr Opin Oncol. 1996;8:377–85. doi: 10.1097/00001622-199609000-00008. [DOI] [PubMed] [Google Scholar]
- 107.Espana-Gregori E, Hernandez M, Menezo-Rozalen JL, Diaz-Llopis M. Metastatic anterior chamber non-Hodgkin lymphoma in a patient with acquired immunodeficiency syndrome. Am J Ophthalmol. 1997;124:243–5. doi: 10.1016/s0002-9394(14)70793-7. [DOI] [PubMed] [Google Scholar]
- 108.Rivero ME, Kuppermann BD, Wiley CA, Garcia CR, Smith MD, Dreilinger A, et al. Acquired immunodeficiency syndrome-related intraocular B-cell lymphoma. Arch Ophthalmol. 1999;117:616–22. doi: 10.1001/archopht.117.5.616. [DOI] [PubMed] [Google Scholar]
- 109.Goldberg SH, Fieo AG, Wolz DE. Primary eyelid non- Hodgkin′s lymphoma in a patient with acquired immunodeficiency syndrome. Am J Ophthalmol. 1992;113:216–7. doi: 10.1016/s0002-9394(14)71545-4. [DOI] [PubMed] [Google Scholar]
- 110.Matzkin DC, Slamovits TL, Rosenbaum PS. Simultaneous intraocular and orbital non-Hodgkin lymphoma in the acquired immune deficiency syndrome. Ophthalmology. 1994;101:850–5. doi: 10.1016/s0161-6420(94)31248-6. [DOI] [PubMed] [Google Scholar]
- 111.Batard ML, Cheret A, Muller P, Sarrouy J, Mareel A, Lamaury I. Bacillary angiomatosis associated with AIDS. Ann Dermatol Venereol. 2006;133:498–9. doi: 10.1016/s0151-9638(06)70950-4. [DOI] [PubMed] [Google Scholar]
- 112.Ormerod LD, Dailey JP. Ocular manifestations of cat-scratch disease. Curr Opin Ophthalmol. 1999;10:209–16. doi: 10.1097/00055735-199906000-00010. [DOI] [PubMed] [Google Scholar]
- 113.Matui R, Nussenblatt R, de Smet MD. Prevalance of tear hyposecretion and vitamin A deficiency in patients with AIDS. Invest Ophthalmol Vis Sci. 1994;35:1308. [Google Scholar]
- 114.Moraes HV., Jr Ocular manifestations of HIV-AIDS. Curr Opin Ophthalmol. 2002;13:397–403. doi: 10.1097/00055735-200212000-00010. [DOI] [PubMed] [Google Scholar]
- 115.Akpek EK, Haddad RS, Winkelstein JA, Gottsch JD. Bilateral consecutive central corneal perforations associated with hypogammaglobulinemia. Ophthalmology. 2000;107:123–6. doi: 10.1016/s0161-6420(99)00005-6. [DOI] [PubMed] [Google Scholar]
- 116.Raina UK, Sharma V, Jain S, Arora R, Mehta DK. Peripheral corneal thinning and silent corneal perforation in an HIV seropositive case. Acta Ophthalmol Scand. 2004;82:246–7. doi: 10.1111/j.1600-0420.2004.00150f.x. [DOI] [PubMed] [Google Scholar]
- 117.Graham DA, Sires BS. Acquired trichomegaly associated with acquired immunodeficiency syndrome. Arch Ophthalmol. 1997;115:557–8. doi: 10.1001/archopht.1997.01100150559025. [DOI] [PubMed] [Google Scholar]
- 118.Nash RW, Lindquist TD. Bilateral angle-closure glaucoma associated with uveal effusion: Presenting sign of HIV infection. Surv Ophthalmol. 1992;36:255–8. doi: 10.1016/0039-6257(92)90094-a. [DOI] [PubMed] [Google Scholar]
- 119.Lozano F, Leon EM, Mira JA, Corzo JE, Gómez-Mateos JM. Relapsing blepharitis in patients under highly active antiretroviral therapy including indinavir. AIDS. 2004;18:354–6. doi: 10.1097/00002030-200401230-00038. [DOI] [PubMed] [Google Scholar]
- 120.Robinson MR, Reed G, Csaky KG, Polis MA, Whitcup SM. Immune recovery uveitis in patients with cytomegalovirus retinitis taking highly active anti retroviral therapy. Am J Ophthalmol. 2000;130:49–56. doi: 10.1016/s0002-9394(00)00530-4. [DOI] [PubMed] [Google Scholar]
- 121.Nguyen QD, Kempen JH, Bolton SG, Dunn JP, Jabs DA. Immune recovery uveitis in patients with AIDS and cytomegalovirus retinitis after highly active antiretroviral therapy. Am J Ophthalmol. 2000;129:634–9. doi: 10.1016/s0002-9394(00)00356-1. [DOI] [PubMed] [Google Scholar]
- 122.Karavellas MP, Azen SP, Macdonald JC, Shufelt CL, Lowder CY, Plummer DJ, et al. Immune recovery vitritis and uveitis in AIDS: Clinical predictors, sequelae and treatment outcomes. Retina. 2001;21:1–9. doi: 10.1097/00006982-200102000-00001. [DOI] [PubMed] [Google Scholar]
- 123.Kempen JH, Min YI, Freeman WR, Holland GN, Friedberg DN, Dieterich DT, et al. Risk of immune recovery uveitis in patients with AIDS and cytomegalovirus retinitis. Ophthalmology. 2006;113:684–94. doi: 10.1016/j.ophtha.2005.10.067. [DOI] [PubMed] [Google Scholar]
- 124.Tseng AL, Walmsley Rifabutin-associated uveitis. Ann Pharmacother. 1995;29:1149–55. doi: 10.1177/106002809502901114. [DOI] [PubMed] [Google Scholar]
- 125.Davis JL, Taskintuna I, Freeman WR, Weinberg DV, Feuer WJ, Leonard RE. Iritis and hypotony after treatment with intravenous cidofovir for cytomegalovirus retinitis. Arch Ophthalmol. 1997;115:733–7. doi: 10.1001/archopht.1997.01100150735008. [DOI] [PubMed] [Google Scholar]
- 126.Lee AK, Chronister CL. Sarcoidosis-related anterior uveitis in a patient with human immunodeficiency virus. J Am Optom Assoc. 1999;70:384–90. [PubMed] [Google Scholar]
- 127.Verma S, Hughes JD, Mabey D, Graham EM. Symptomatic anterior uveitis in an HIV-positive patient. Int J STD AIDS. 1999;10:268–74. doi: 10.1258/0956462991913925. [DOI] [PubMed] [Google Scholar]


