Abstract
To describe use of a locally processed bovine pericardium (BP) to cover a large central corneal perforation following alkali injury and discuss postoperative outcome.
A 27-year-old Malay male patient presented two weeks after alkali splashed in his left eye while working. A clinical diagnosis of left central corneal ulcer with limbal ischemia following alkali injury with secondary infection was made. After failed medical therapy, we performed a Gunderson conjunctival flap under local anesthesia that retracted after one week and resulted in a large central corneal perforation with surrounding stromal thinning. The perforation was covered with a locally processed BP xenograft (Lyolemb) supplied by the National Tissue Bank, University Sains Malaysia. Nine months follow-up showed a well-taken graft without any exposure/dehiscence and minimal inflammation.
Amniotic membrane transplantation when used as a patch graft needs an urgent tectonic graft to promote corneal stability in patients with severe corneal thinning. The use of processed BP can be a viable option in treating such cases.
Keywords: Bovine pericardium, chemical injury, corneal perforation
Severe corneal ulceration might lead to descematocele formation and in turn imminent danger of perforation. Various therapeutic measures range from eye patching, bandage soft contact lenses, cyanoacrylate application,1 to surgical procedures such as tarsorrhaphy,2 conjunctival flap, amniotic membrane transplantation (AMT)3 and penetrating keratoplasty (PKP). Amniotic membrane transplantation as a patch graft needs an urgent tectonic procedure in severe corneal thinning.3
Penetrating keratoplasty is an established modality of treating large corneal perforations. Processed bovine pericardium (BP) has been widely used as a wrap for orbital implants due to its excellent suture retention and strength. It is well tolerated with minimal inflammation.4,5 Easy availability and low cost make it an alternative modality of treatment, especially if a donor cornea is not available. We report a case of large corneal perforation with surrounding stromal inflammation treated with locally processed BP.
Case Report
A 27-year-old Malay male patient presented two weeks after alkali splashed into his left eye while working. Prior to reporting to us, the patient consulted a general practitioner who prescribed some topical eye drops (details of the treatment were not available) and the eye condition worsened. Anterior segment examination revealed a central corneal ulcer (1 × 1 mm) with stromal infiltration (4 × 6 mm), limbal ischemia, normal anterior chamber depth and visual acuity of counting fingers. A gentle B-scan ruled out any posterior segment abnormality.
A clinical diagnosis of left corneal ulcer with limbal ischemia secondary to alkali injury with secondary infection was made. Culture from corneal scraping was negative. Despite intensive therapy with oral (Tab Ciprobay 500 mg twice daily, Bayer) and topical ciprofloxacin (Gutt Ciloxan 0.3% hourly, Alcon) (no topical steroids used) with other supportive therapy (Tab Vitamin C 1 g daily, Pharmaniaga), further deterioration led to formation of central corneal perforation with surrounding stromal thinning and flat anterior chamber. The visual acuity was inaccurate projection of light rays.
We performed a Gunderson conjunctival flap under local anesthesia (LA), which retracted and failed after one week. Slit-lamp examination revealed a large central corneal perforation (4 × 5 mm) with surrounding stromal thinning involving two- thirds of the cornea without any signs of infection.
In order to maintain the shape of the eyeball and due to the problem of non-availability of donor cornea, we decided to use processed BP xenograft (Lyolemb) supplied by National Tissue Bank, Universiti Sains Malaysia after obtaining the consent of the patient. A 360° peritomy was done and the graft was sutured with 7-0 polyglycolic and polylactic acids (Vicryl) to the perilimbal area with conjunctival advancement. Topical (Gutt Ciloxan 0.3% hourly, Alcon) and oral ciprofloxacin (Tab Ciprobay 500 mg twice daily, Bayer) was prescribed in the postoperative period [Figure 1]. The details of anterior segment were difficult to assess due to conjunctival advancement. Nine months follow-up showed a well-taken graft without any exposure/dehiscence and minimal inflammation [Figure 2]. Slit-lamp examination could not reveal the details of the anterior chamber and beyond due to conjunctival advancement and vision was noted as perception of light with inadequate projection of rays.
Figure 1.
Whitish tissue underneath sutures indicating bovine pericardium graft with limbal ischemia one-week postoperatively
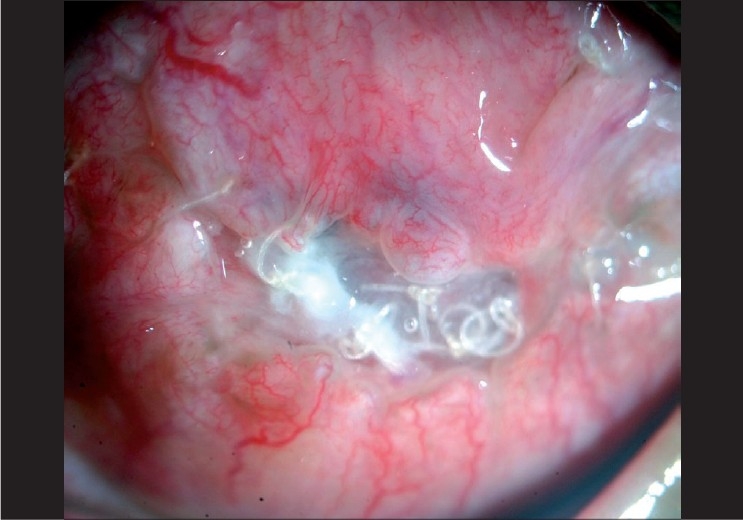
Figure 2.

A well-taken bovine pericardium graft with early symblepharon and minimal inflammation nine-months postoperatively
Discussion
Conjunctival flap is unlikely to seal large corneal perforations associated with corneal melting following chemical injury. Efficacy of AMT alone or with glue in treating small corneal perforation has been well established but found unable to promote corneal stability in patients with severe corneal thinning and therefore, an additional urgent tectonic procedure has to be undertaken.3 Non-availability of donor cornea poses a considerable problem in some countries.
Processed BP is a tough lyophilised collagen sheet used as a surgical armamentarium in wrapping orbital implants.4,5 It renders the material antigenically inert and adds to its strength, pliability and longevity.5 It has been shown to be well tolerated with minimal inflammation in animal studies.4 Although theoretic concerns about prion disease can be raised, no evidence of this problem has been reported from over 90,000 human implantations.6 Devron reported no significant ophthalmic reactions due to this xenograft in his cases of orbital implants.7
At the National Tissue bank, Universiti Sains Malaysia, the procured pericardium sheet was washed using chemical agent (sterile phosphate buffer at pH 7.4) and frozen to −40°C. It was then freeze-dried and packaged in double-layer plastic bag. The processed BP was radio-sterilized at 2.5 mega rads using gamma radiation and was then ready for use.8 We used this locally processed BP in our case. Nine months follow-up showed good results.
To our knowledge, there has been no reported case using BP in corneal perforation. Its use in complicated ocular surface diseases such as large corneal perforation with corneal melting can be promising. Its use needs to be further studied more extensively as an alternative graft material in large corneal perforations.
References
- 1.Webster RG, Slansky HH, Refojo MF, Dohlman CH. The use of adhesive for closure of corneal perforations. Arch Ophthalmol. 1968;80:705–9. doi: 10.1001/archopht.1968.00980050707004. [DOI] [PubMed] [Google Scholar]
- 2.Azuara-Blanco A, Pillai CT, Dua HS. Amniotic membrane transplantation for ocular surface reconstruction. Br J Ophthalmol. 1999;83:399–402. doi: 10.1136/bjo.83.4.399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prabhasawat P, Tesavibul N, Komolsuradej W. Single and multilayer amniotic membrane transplantation for persistent corneal epithelial defect with and without stromal thinning and perforation. Br J Ophthalmol. 2001;85:1455–63. doi: 10.1136/bjo.85.12.1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.DeBacker CM, Dutton JJ, Proia AD, Holck DE, Stone T. Bovine pericardium versus homologous sclera as wrapping materials for hydroxyapatite ocular implants: an animal study. Ophthalmic Plastic Reconstr Surg. 1999;15:312–6. doi: 10.1097/00002341-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Mehta JS, Franks WA. The sclera, the prion and the ophthalmologist. Br J Ophthalmol. 2002;86:587–92. doi: 10.1136/bjo.86.5.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holt TA, Phillips J. Bovine spongiform encephalopathy. BMJ. 1988;296:1581–2. doi: 10.1136/bmj.296.6636.1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Devron HC. Early wound dehiscence with use of hydroxyapatite orbital implant covered with calf pericardium. Br J Ophthalmol. 2001;85:627–8. doi: 10.1136/bjo.85.5.625c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abdullah J, Rushdan A, Hamzah M, Arif AR, Rani A. Use of bovine xenograft in reconstruction of traumatic anterior cranial fossa bone defects involving the frontal sinus. Ann Transplant. 1999;4:28–31. [PubMed] [Google Scholar]


