Abstract
Xeroderma pigmentosum (XP) is an autosomal recessive genetic disorder of DNA repair in which the body′s normal ability to repair damage caused by ultraviolet light is deficient. This leads to a 1000-fold increased risk of cutaneous and ocular neoplasms. Ocular neoplasms occurring in XP in order of frequency are squamous cell carcinoma, basal cell carcinoma and melanoma. Malignant melanomas occur at an early age in patients with XP. We report a case of XP with massive orbital melanoma in an eight-year-old boy which is unique due to its amelanotic presentation confirmed histopathologically.
Keywords: Amelanotic, malignant melanoma, orbit, xeroderma pigmentosum
Xeroderma pigmentosum (XP) is a rare genetic disease characterized by defective repair of DNA damage.1 Inheritance is autosomal recessive and consanguinity of parents is common.2 Ocular involvement is reported in 91% of cases.2 Epibulbar neoplasms are found in 11% of XP patients and in order of frequency are predominantly squamous cell carcinoma followed by basal cell carcinoma and melanoma.3 We report a case of an orbital amelanotic malignant melanoma in XP. Detailed search on MEDLINE could not find any such case reported earlier in the literature.
Case Report
An eight-year-old male presented with decrease in vision, photophobia, blepharospasm and lacrimation of the right eye and loss of vision with large orbital mass of the left eye since last one year. Multiple freckle-like pigmented macules on sun-exposed parts of the body were evident since one year of age. Parents had three males and one female child, only one male child developed a similar skin condition and the remaining three children were healthy. There was a history of consanguinity.
Cutaneous examination showed hyperpigmented freckle- like and hypopigmented macules all over the body. A hypopigmented growth was present on the right ala of the nose and just above the right eyebrow on its lateral aspect. No lymphadenopathy or organomegaly was detected.
On ocular examination, the visual acuity of the right eye could not be assessed as the child was uncooperative. The right upper lid and lower lid showed hyperpigmented freckle-like and hypopigmented macules similar to the rest of the body. Further, the right eye showed lower lid ectropion and a macular corneal opacity involving the entire cornea [Figure 1A]. Iris and lens details were not clear. In the left eye a large orbital reddish yellow mass with irregular outer surface of 5.0 cm×6.0 cm was present. No other ocular structure could be identified and both eyelids were also lost [Figure 1B].
Figure 1A.

(A) Lower lid ectropion and macular corneal opacity in right eye of a xeroderma pigmentosum patient one year back.
Figure 1B.

(B) A large orbital growth in the left eye of a xeroderma pigmentosum patient
Routine investigations (hemoglobin, total leucocyte count, differential leucocyte count, erythrocyte sedimentation rats, renal function test, liver function test, urine routine and microscopic, X-ray chest, electrocardiogram, bleeding time and clotting time) were normal. Magnetic resonance imaging (MRI) of the left orbit showed a heterogeneous mass of the left orbit involving and replacing the globe with loss of its contour. The mass was extending anteriorly and protruding beyond the anterior margin of the orbit forming polypoidal growth. Posteriorly, there was involvement of extraocular muscles and optic nerve with no evidence of extension beyond the bony orbit or intracranial spread.
Skin biopsy confirmed the diagnosis of XP. Biopsy of the growth on the right ala of the nose and lateral aspect of the right eyebrow showed cutaneous basal cell carcinoma.
A total exentration of the orbital mass was carried out. On gross examination a single irregular soft tissue mass of 5.0 × 6.0 × 4.0 cm with focal areas of hemorrhage was seen. On histopathlogical examination, sections from the excised tumor tissue exhibited features consistent with a mixed spindle cell and epitheloid cell melanoma. The predominant tumor cell type was epitheloid cell type and the tumor cells were largely amelanotic [Figure 2].
Figure 2.
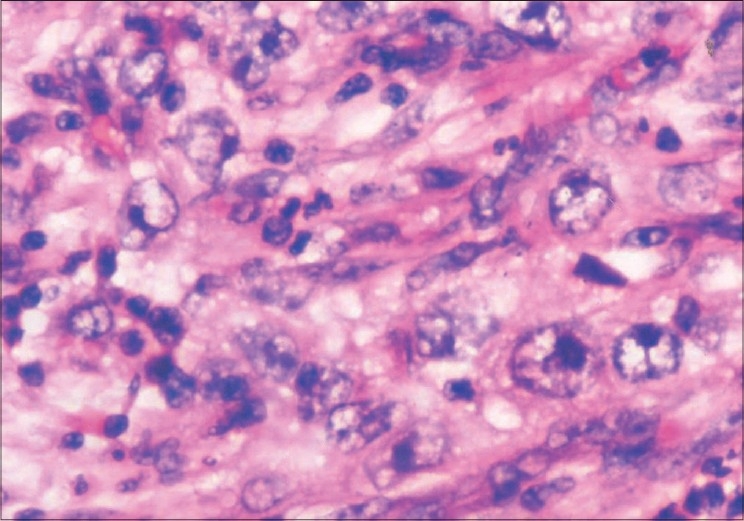
Photomicrograph showing sheet of plump epitheloid tumor cells with large nuclei and prominent nucleoli. Melanin is absent in tumor cells (H&E, ×400)
Based on the above-mentioned features a diagnosis of XP with an amelanotic melanoma of the orbit was confirmed.
Discussion
Xeroderma pigmentosum was first described in 1874 by Hebra et al.4 In 1882, Kaposi coined the term XP for the condition, referring to its characteristic as dry, pigmented skin. It is a hereditary condition with an incidence of 1:250000 live births.5 Being an autosomal recessive disease, parental consanguinity plays an important role in XP. It was noted in 40% of cases in a study6 while Kraemer′s series reported it in 31% of cases.3 Xeroderma pigmentosum is characterized by photosensitivity, pigmentary changes, premature aging, photophobia and malignant tumor development in sun-exposed mucocutaneous and ocular structures.3 Among the ocular tissues, the lids, conjunctiva and cornea are predominantly affected because they are exposed to ultraviolet radiation from sunlight.3 The case reported by us has almost all the above-mentioned features of XP. Ocular surface neoplasms, including squamous cell carcinoma, basal cell carcinoma and melanoma, occur with a predilection for the limbal area.3 Squamous cell carcinoma is the commonest of all, occurring in up to 13% of patients.2,7 El Hafnawi et al.,2 reported four cases of melanocytic lesions affecting the eye, two of which were considered malignant. One was a conjunctival melanoma, the second was an advanced melanoma affecting the whole orbit and base of skull. The case reported by us is also an advanced orbital melanoma similar to the case mentioned above, the only difference being amelanosis in our case, which is a rare occurrence. Vivian et al.,8 also reported ocular melanomas of the conjunctiva and choroid, originating from an area of melanosis. Nakajima et al.,9 in a series of malignant melanomas from many sites reported three pigmented primary choroidal melanomas. Johnson et al.,10 have also described a patient with malignant melanoma of the iris while Kraemer et al.,3 have reported two choroidal melanomas from 830 reported cases of XP.
Many researchers have reported several cases of ocular melanomas but none have discussed amelanosis in ocular melanoma. To our knowledge this is the first ever case of advanced orbital amelanotic melanoma reported so far. Treatment of such cases in addition to medical treatment is complete excision of tumor and genetic counseling.
Acknowledgments
Hyderabad Eye Research Foundation
Footnotes
Presentation at a meeting: A part was presented as poster in Annual Conference of Oculoplastic Association of India. December 14th -16th, 2007. Hyderabad.
References
- 1.Mseddi M, Sellami D, Elloumi Y, Aloulou Y, Kammoun B, Turki H, et al. Ophthalmologic manifestations of the xeroderma pigmentosum. Tunis Med. 2006;84:542–4. [PubMed] [Google Scholar]
- 2.El-Hafrawi H, Mortada A. Ocular manifestations of xeroderma pigmentosum. Br J Dermatol. 1965;77:261–76. doi: 10.1111/j.1365-2133.1965.tb14641.x. [DOI] [PubMed] [Google Scholar]
- 3.Kraemer KH, Lee M, Scotto J. Xeroderma Pigmentosum-cutaneous, ocular and neurologic abnormalities in 830 published cases. Arch Dermatol. 1987;123:241–80. doi: 10.1001/archderm.123.2.241. [DOI] [PubMed] [Google Scholar]
- 4.Hebra F, Kaposi M. On diseases of the skin including exanthemata. New Sydenham Soc. 1874;61:252–8. [Google Scholar]
- 5.Robbin JH, Kraemer KH, Lutzner MA, Festoff BW, Coon HP. Xeroderma pigmentosum: An inherited disease with sun sensitivity, multiple cutaneous neoplasms and abnormal DNA repair. Ann Intern Med. 1974;80:221–48. doi: 10.7326/0003-4819-80-2-221. [DOI] [PubMed] [Google Scholar]
- 6.Goyal JL, Rao VA, Srinivasan R, Agarwal K. Oculocutaneous manifestations in xeroderma pigmentosa. Br J Ophthalmol. 1994;78:295–7. doi: 10.1136/bjo.78.4.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reese AB, Wilber IE. The eye manifestations of xeroderma pigmentosum. Am J Ophthalmol. 1943;26:901–11. [Google Scholar]
- 8.Vivian AJ, Ellison DW, McGile JI. Ocular melanomas in xeroderma pigmentosum. Br J Ophthalmol. 1993;77:597–8. doi: 10.1136/bjo.77.9.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nakajima T, Watanabi S, Sato Y, Kameya T, Shinosato Y, Ishihara K. Immuno-histochemical demonstration of S-100 protein in malignant melanoma and pigmented naevus and its diagnostic application. Cancer. 1982;50:912–8. doi: 10.1002/1097-0142(19820901)50:5<912::aid-cncr2820500519>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- 10.Johsnon M, Skuta G, Kinkaid M, Nelson C, Wolter J. Malignant melonoma of the iris in xeroderma pigmentosum. Arch Ophthalmol. 1989;107:402–7. doi: 10.1001/archopht.1989.01070010412036. [DOI] [PubMed] [Google Scholar]


