Abstract
A 35-year-old male with a history of chikungunya fever, presented with diminution of vision in the right eye of one-week duration. His best corrected visual acuity (BCVA) was counting fingers 2 meters and 20/20 (Snellens) in the right and left eyes respectively. A diagnosis of neuroretinitis was made in the right eye while left eye showed features of retinitis. ELISA (serum) and polymerase chain reaction (aqueous) were positive for herpes simplex virus. The lesions did not show any response to antiviral or steroid treatment and appeared to be self-limiting. At five months follow-up, lesions had resolved well with BCVA of 20/120 and 20/20 in the right and left eyes respectively.
Keywords: Bilateral, chikungunya, retinitis
Chikungunya fever is caused by an alphavirus transmitted to humans by the bite of infected mosquitoes belonging to the genus Aedes.1 Large scale outbreaks of the fever due to the chikungunya fever in south India have been reported recently. We report an interesting case of bilateral retinitis following serologically proven chikungunya fever.
Case Report
A 35-year-old male presented with diminution of vision in the right eye of one-week duration. He was symptomatically treated for serologically proven chikungunya fever three weeks back. On examination, his best corrected visual acuity (BCVA) was counting fingers 2 meters and 20/20 (Snellens) in the right and left eyes respectively. Relative afferent pupillary defect was noted in the right eye. Slit-lamp examination showed a quiet anterior segment and 1 + vitreous cells (Grading: Kimura and colleagues)2 in both eyes. Intraocular pressures were normal. Fundus examination of the right eye showed areas of retinitis and hemorrhages in the posterior pole and hyperemia and blurring of the disc margins (neuroretinitis). In the left eye, a patch of retinitis was seen nasal to the optic disc [Fig. 1A and B]. Fundus fluorescein angiography showed areas of capillary nonperfusion corresponding to the retinitis lesions [Fig. 2A and B] and optical coherence tomography (Stratus version 4, Zeiss, Germany) showed areas of retinal destruction [Fig. 3]. Laboratory investigations included an ESR of 38mm/h, normal hematological and rheological parameters, coagulation profile, blood sugar, liver and renal function, urine analysis and chest X-ray. VDRL test for syphilis and Mantoux test were negative. ELISA showed IgM and IgG positivity for herpes simplex and only IgG positivity for cytomegalovirus and Varicella Zoster viruses. ELISA for HIV and toxoplasma were negative. Aqueous tap was positive for herpes simplex virus. He was started on intravenous acyclovir 1500 mg/m2/day. As the lesions continued to progress [Fig. 4A and B] in both eyes, oral steroids in a dosage of 1 mg/kg body weight were added after four days along with oral acyclovir and intravitreal ganciclovir 2000 micrograms in 0.05 ml in both eyes. Oral acyclovir was stopped after 10 days while the steroids were tapered over four weeks. At the end of four weeks, there was no further deterioration in vision or appearance of any new lesions. At the last follow-up (five months), the retinal lesions had healed well [Fig. 5] and his BCVA was 20/120 and 20/20 in the right and left eyes respectively.
Figure 1A.

Fundus photograph of the right eye showing active retinitis
Figure 1B.

Fundus photograph of left eye showing active retinitis
Figure 2A.
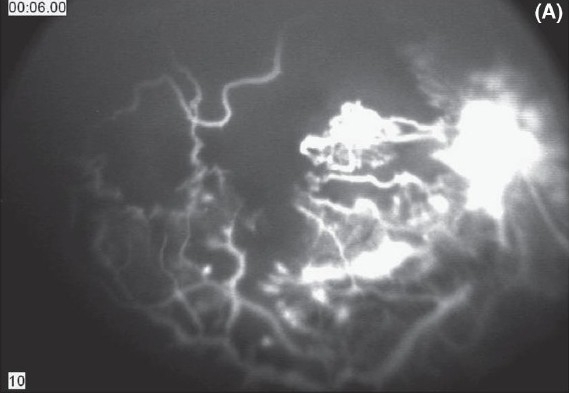
Fluorescein angiogram showing areas of capillary nonperfusion in the right eye
Figure 2B.
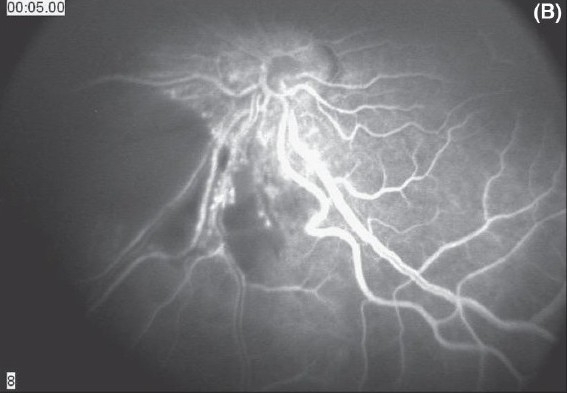
Fluorescein angiogram showing areas of capillary nonperfusion in the left eye
Figure 3.
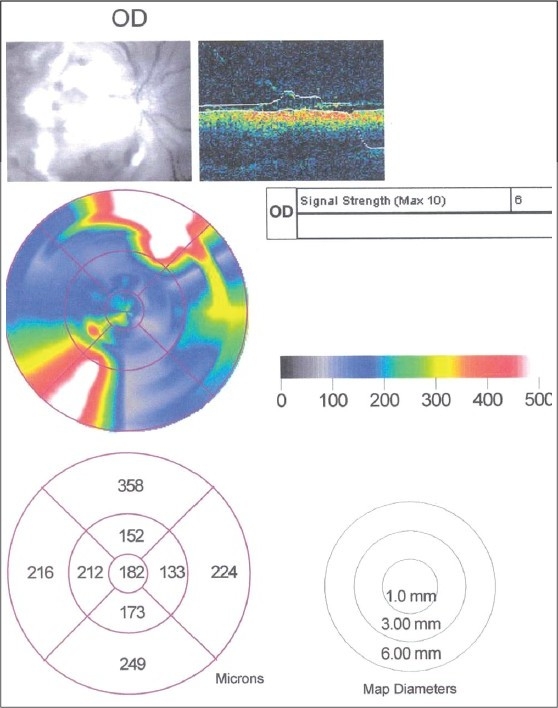
Optical coherence tomogram of the right eye showing areas of retinal destruction
Figure 4A.
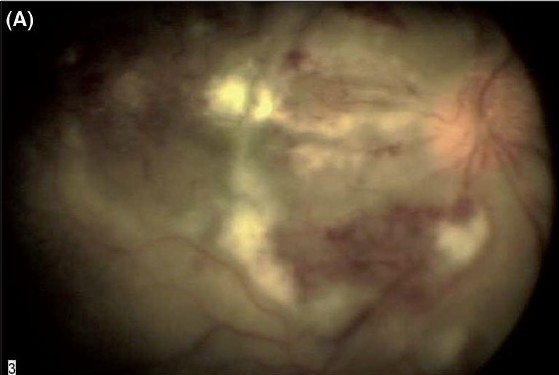
Fundus photograph of the right eye showing progression of retinitis
Figure 4B.

Fundus photograph of left eye showing progression of retinitis
Figure 5.
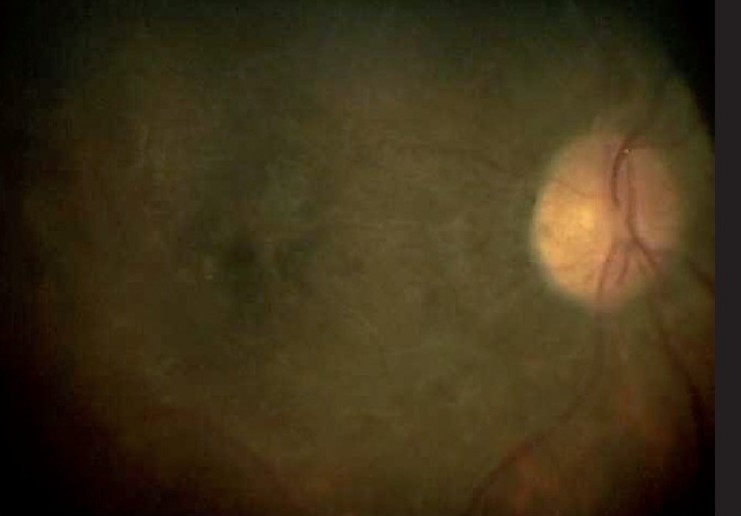
Fundus photograph of the right eye showing resolved retinitis
Discussion
Ocular manifestations in chikungunya fever are rare and include retroorbital pain, conjunctivitis and choroiditis, (Medline search).3 We report an interesting case of bilateral retinitis in a patient with serologically proven chikungunya fever. As no reports of retinitis after chikungunya fever were available in the literature at the time of examination, tests were done to rule out an infective etiology. ELISA and the PCR results of the serum and the aqueous sample respectively were positive for herpes simplex virus.4-6 As a result, he was started on intravenous acyclovir. As symptoms continued to progress in spite of intravenous acyclovir, an ongoing immune-mediated reaction following the fever was a possibility. Role of corticosteroids and immunosuppression in viral fever is controversial. As a result, he received oral steroids (1 mg/kg body wt) under cover of antivirals. There was no immediate improvement of the retinitis with the above treatment. However, there was no further worsening of the retinitis either. The lesions were self-limiting and took over six to eight weeks to resolve completely.
Retrospectively, the interval between the onset of visual symptoms and the systemic manifestations of chikungunya fever in our patient was three weeks. This delay favors the hypothesis that the ocular lesions could be an immune- mediated process rather than a direct viral infection. There may also be an aberrant immune response triggered by the virus resulting in development of autoantibodies against the retina.7 However, in our case, it is difficult to explain the PCR and ELISA positivity to herpes simplex virus and non- responsiveness to antiviral treatment. As this is an isolated case report, it is difficult to postulate the mechanism involved in the development of retinitis.
This report highlights the findings and course of bilateral retinitis in a patient with chikungunya fever.
References
- 1.Calisher CH, Shope RE, Brandt W, Casals J, Karabatsos N, Murphy FA, et al. Proposed antigenic classification of registered arboviruses I: Togaviridae, alphavirus. Intervirology. 1980;14:229–32. doi: 10.1159/000149190. [DOI] [PubMed] [Google Scholar]
- 2.Kimura SJ, Thygeson P, Hogan MJ. Signs and symptoms of uveitis: II, Classification of the posterior manifestations of uveitis. Am J Ophthalmol. 1959;47:171–6. doi: 10.1016/s0002-9394(14)78240-6. [DOI] [PubMed] [Google Scholar]
- 3.Chanana B, Azad RV, Nair S. Bilateral macular choroiditis following chikungunya virus infection. Eye. 2007;21:1020–1. doi: 10.1038/sj.eye.6702863. [DOI] [PubMed] [Google Scholar]
- 4.Madhavan HN, Priya K. The diagnostic significance of enzyme linked immunosorbent assay for herpes simplex, varicella zoster and cytomegalovirus retinitis. Indian J Ophthalmol. 2003;51:71–5. [PubMed] [Google Scholar]
- 5.Grover R, Ratho RK, Gupta V, Mahajan RC, Gupta A. Role of viral serology in the diagnosis of acute retinal necrosis syndrome. Indian J Pathol Microbiol. 2002;45:269–71. [PubMed] [Google Scholar]
- 6.de Boer JH, Verhagen C, Bruinenberg M, Rothova A, de Jong PT, Baarsma GS, et al. Serologic and polymerase chain reaction analysis of intraocular fluids in the diagnosis of infectious uveitis. Am J Ophthalmol. 1996;121:650–8. doi: 10.1016/s0002-9394(14)70631-2. [DOI] [PubMed] [Google Scholar]
- 7.Lim WK, Mathur R, Koh A, Yeoh R, Chee SP. Ocular manifestations of dengue fever. Ophthalmology. 2004;111:2057–64. doi: 10.1016/j.ophtha.2004.03.038. [DOI] [PubMed] [Google Scholar]


