Abstract
Post-penetrating keratoplasty (post-PK) glaucoma is an important cause of irreversible visual loss and graft failure. The etiology for this disorder is multifactorial, and with the use of new diagnostic equipment, it is now possible to elucidate the exact pathophysiology of this condition. A clear understanding of the various mechanisms that operate during different time frames following PK is essential to chalk out the appropriate management algorithms. The various issues with regard to its management, including the putative risk factors, intraocular pressure (IOP) assessment post-PK, difficulties in monitoring with regard to the visual fields and optic nerve evaluation, are discussed. A step-wise approach to management starting from the medical management to surgery with and without metabolites and the various cycloablative procedures in cases of failed filtering procedures and excessive perilimbal scarring is presented. Finally, the important issue of minimizing the incidence of glaucoma following PK, especially through the use of oversized grafts and iris tightening procedures in the form of concomitant iridoplasty are emphasized. It is important to weigh the risk-benefit ratio of any modality used in the treatment of this condition as procedures aimed at IOP reduction, namely trabeculectomy with antimetabolites, and glaucoma drainage devices can trigger graft rejection, whereas cyclodestructive procedures can not only cause graft failure but also precipitate phthisis bulbi. Watchful expectancy and optimal time of intervention can salvage both graft and vision in this challenging condition.
Keywords: Glaucoma, penetrating keratoplasty, iridoplasty, trabeculectomy
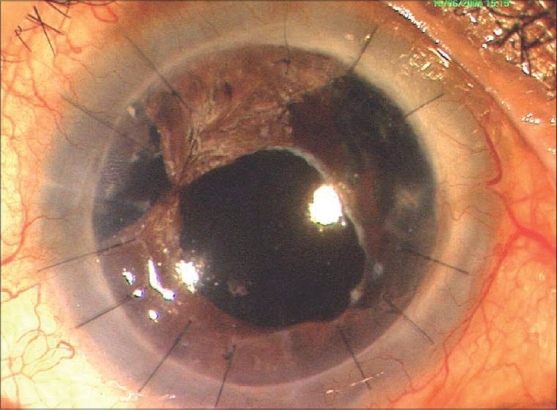
Glaucoma following penetrating keratoplasty (PK) is one of the most common cause for irreversible visual loss1 and the second leading cause for graft failure2 [Fig. 1] after rejection. Post-PK glaucoma is a significant clinical problem because of its frequency of occurrence, difficulty in diagnosis and monitoring, and complexity of management.3 An increase in intraocular pressure (IOP) at any time after PK leads to a significant endothelial cell loss, with dire consequences as the endothelial reserve is already low. Timely diagnosis of post-PK glaucoma with initiation of appropriate treatment is mandatory to preserve optimal graft clarity and optic nerve head function.2
Figure 1.
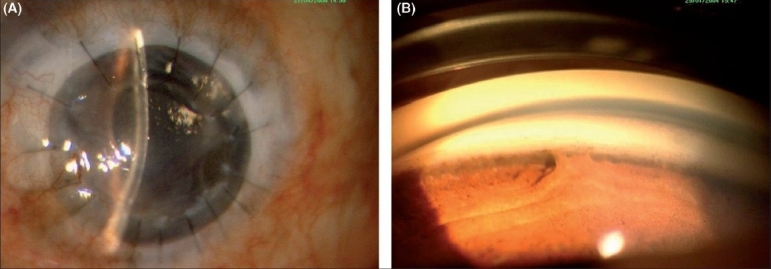
(A) Graft corneal edema due to peripheral anterior synechiae (PAS) and secondary glaucoma. (B) PAS - gonioscopic view
Post-PK glaucoma is defined as an elevated IOP greater than 21 mmHg, with or without associated visual field loss or optic nerve head changes. Diagnostic difficulty arises due to errors in tonometry recordings of a thick or astigmatic corneal graft.4 In addition, it is often not possible to assess adequately the optic nerve and visual field before surgery or in the immediate post- operative period because of preoperative media opacification and post-operative corneal distortion with high astigmatism, respectively.4
It was only in the 1960s, with the development of instruments that allowed routine monitoring of IOP after PK, that the problem of post-PK glaucoma was recognized. In 1969, Irvine and Kaufman5 first reported the high incidence of increased IOP following PK. They reported a mean maximum pressure of 40 mmHg in aphakic transplants and 50 mmHg in combined transplants and cataract extraction in the immediate post- operative period. Since then, various authors have reported the incidence of glaucoma following PK to be from 9 to 31% in the early post-operative period3,6,7 and from 18 to 35% in the late post-operative period.1,8
The purpose of the present review is to highlight the magnitude of the problem. The etiology, risk factors, diagnostic assessment and management options are reviewed and the prognosis as reported in the literature is highlighted. A PubMed/Medline search using keywords like penetrating keratoplasty and glaucoma, or glaucoma following PK was done over the last 30 years. The search was limited to articles in English. For articles in other languages, only the abstract in English was taken for reference.
Etiology
Risk factors for glaucoma in patients undergoing PK include:
Indications for PK and associated rates of chronic post-PK glaucoma
Goldberg et al.3 reported a 29% incidence of increased IOP in the early post-operative period and 30% in the late post-operative period in patients with aphakic bullous keratopathy. They reported that the incidence of increased IOP is higher in patients with repeat grafts, both in the early (45%) and late post-operative phase (52%) and those with pre-existing glaucoma (71% of all patients with pre-existing glaucoma developed elevated IOP in the early post-operative course).3 Kirkness et al.9 reported a higher incidence of glaucoma in patients undergoing PK following corneal perforation, especially those following suppurative keratitis, due to peripheral anterior synechia (PAS) formation and secondary angle closure. As seen in Table 1, the rates of chronic glaucoma after PK differ significantly based on the indication for PK (from a low of 0-12% for keratoconus to a high of 75% after infectious keratitis).
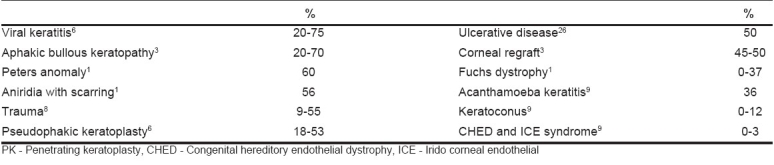
Table 1.
Indications for penetrating keratoplasty and associated rates of chronic post-PK glaucoma
Pathophysiology
Pathophysiology of post-PK glaucoma is multifactorial [Table 2] and may be related to distortion of the angle with collapse of the trabecular meshwork, suturing technique, post-operative inflammation, use of corticosteroids, PAS formation and pre-existing glaucoma. Olson and Kaufman,8 using a mathematical model, proposed that the elevated IOP following PK in an aphakic patient might be the result of angle distortion secondary to a compressed tissue in the angle. Edema and inflammation after surgery lead to further compromise in the trabecular meshwork function, and the situation is further aggravated by angle distortion. Factors that contribute to angle distortion include tight suturing, long bites (more compressed tissue), larger trephine sizes, smaller recipient corneal diameter and increased peripheral corneal thickness. The following surgical variables reduce angle compression:
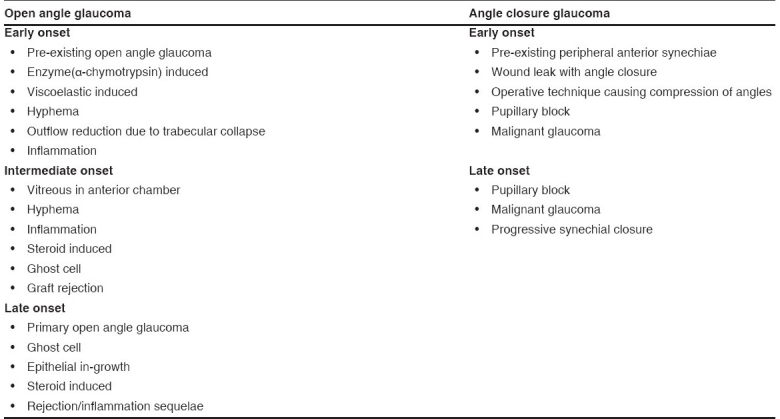
Table 2.
Mechanisms of increased intraocular pressure after penetrating keratoplasty
Less tight sutures
Deep sutures
Short sutures
Suture bites equal on either side of wound
Smaller sized grafts
Donor corneas larger than that of the recipient
Thinner recipient corneas
Larger overall corneal diameter
On the other hand, Zimmerman et al.10 proposed that mechanical collapse of the trabecular meshwork in aphakic grafts is the main problem leading to glaucoma. They postulated that the trabeculum needs posterior fixation afforded by the ciliary body-lens support system and an anterior support afforded by the Descemet′s membrane. In aphakia, the posterior support is relaxed with the removal of the lens. After PK, the Descemet′s membrane is incised, which leads to a relaxation of the anterior support. Both these factors lead to a partial trabecular collapse and obstruction of aqueous outflow. Supporting this theory, Zimmerman et al.11 reported that oversized donor buttons (0.5 mm larger than the host bed) in aphakic patients reduced the incidence of glaucoma. The effect was more obvious when an 8-mm donor button was used in a 7.5-mm host bed. Retained viscoelastic material is another important cause for increased IOP in the early post-operative period, especially with the use of sodium hyaluronate 2.3% (Healon 5) or Healon GV (1.4%) and its combination with chondroitin sulfate (Viscoat) used during PK. One has to be cautious when these high viscosity agents are used because they can clog the trabecular meshwork, leading to a severe post-operative IOP spike. Complete removal must be done at the end of surgery.
The main cause for late post-PK glaucoma is synechial angle closure with the degree of synechial closure strongly correlated with the need for surgery.12 A floppy atrophic iris may also lead to a higher incidence of PAS formation, which can be prevented by iris suturing or iridoplasty.13
Diagnosis
Accurate measurement of IOP, assessment of visual fields and neuroretinal structures are often not possible before PK due to the primary corneal disease. This often leads to an inability to diagnose pre-existing glaucomatous optic neuropathy. Following PK, changes in corneal thickness, post-operative astigmatism and refractive changes often preclude reliable post- operative assessment of IOP, disc and visual field. Extra time needs to be devoted for such patients with the main emphasis on stereoscopic optic nerve head evaluation under mydriasis. Gonioscopy may be performed to view the site and extent of PAS [Fig. 1]. The ideal way is to take disc photographs at the first examination and serially repeat them at least once a year to detect if there is any progression of the glaucomatous optic neuropathy.
The diagnosis of post-PK glaucoma is primarily based on IOP measurements in the early post-operative period, and on IOP, optic disc change and progressive visual field changes in the late post-operative period. IOP in the early post- operative period, when the corneal surface is irregular, can be measured with the Mackay-Marg electronic applanation tonometer,14 the pneumatic applanation tonometer, the tono-pen, or recently the dynamic contour tonometer (DCT), independent of the corneal thickness. If the graft surface is smooth with an intact epithelium and regular mires can be obtained, then Goldmann applanation can be used to measure the IOP. Marked corneal astigmatism causes an elliptical fluorescein pattern. To obtain an accurate reading with the Goldmann applanation tonometer, the clinician should rotate the prism so that the red mark on the prism holder is set at the least curved meridian of the cornea (along the negative axis). Alternately, two pressure readings, taken 90 degrees apart, can be averaged. The accuracy of applanation tonometry is reduced in certain situations, such as corneal edema, scars, blood staining, or any condition that thickens or alters the corneal elasticity.15 Corneal epithelial edema and stromal edema predispose to inaccurately low readings, whereas pressure measurements taken over a corneal scar will be falsely high. While measuring IOP with Goldmann applanation tonometer that is standardized for a central corneal thickness (CCT) of 520 µ, overestimation of IOP may occur due to an increase in the corneal thickness.
In cases with complete tarsorrhaphy, the IOP can be estimated by digital palpation,16 although new tonometers that measure IOP through the lid (Proview Phosphene Tonometer) are available. In such cases, measuring the IOP in the normal eye using the Goldmann applanation tonometer and then performing digital palpation gives a better estimate of the IOP.
Ultrasound biomicroscopy
Ultrasound biomicroscopy is useful to assess the angle and establish the cause for post-PK glaucoma, especially in eyes with a failed graft where anterior segment details are not clearly visible. The extent of irido-corneal adhesions, location of intraocular lens (IOL), phakic/aphakic status, anterior chamber (AC) depth, angle width and corneal thickness can be determined with this technology. Moreover, UBM can be of use to the anterior segment surgeon by providing preoperative data regarding the anterior segment anatomy, especially with regard to the presence of irido-corneal adhesions and to guide the surgeon regarding extra precautions to be taken in such areas to prevent or minimize inadvertent iris damage during PK. It also aids the glaucoma surgeon in planning the site for trabeculectomy or a glaucoma drainage device (GDD).
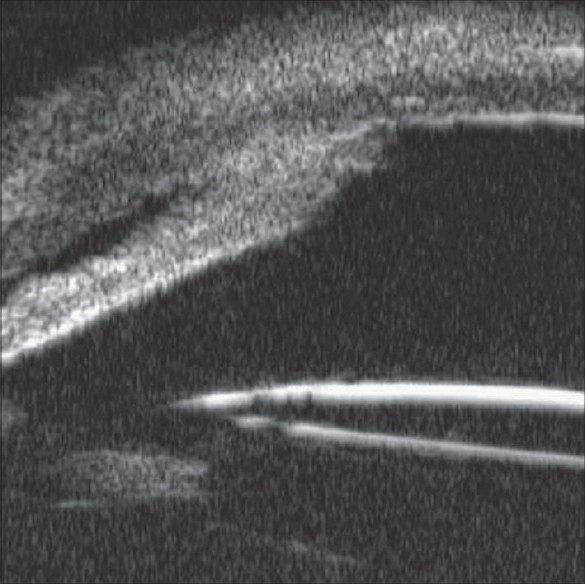
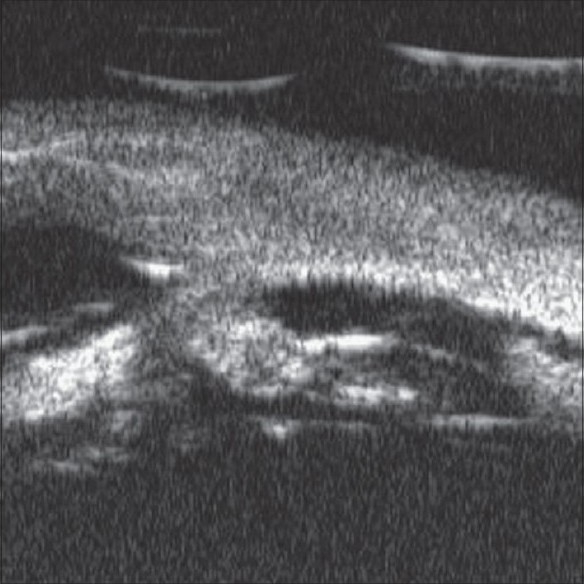
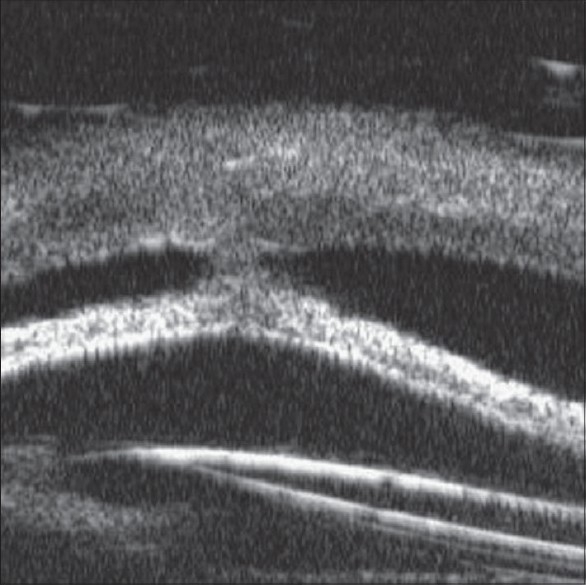
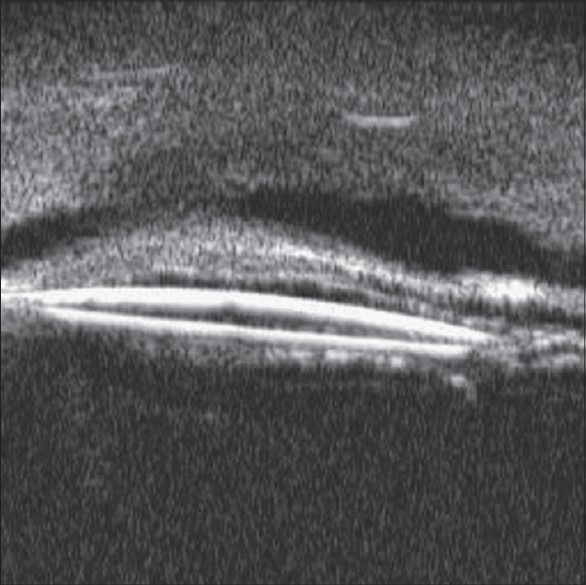
In a UBM study undertaken by the lead investigator,17 UBM findings in 31 eyes with post keratoplasty glaucoma were reported. Indication for keratoplasty, lens status, intraocular pressure at the time of presentation, and the time of diagnosis of glaucoma were noted. The mean intraocular pressure was 35.5 ± 5.8 mm Hg (range, 26-52 mm Hg). The mean time of follow-up after penetrating keratoplasty was 6.97 ± 2.98 months (range, 2-16 months). Of the 31 patients, 11 had undergone penetrating keratoplasty for therapeutic purposes (infectious keratitis), whereas the remaining 20 had undergone keratoplasty for optical reasons. Fourteen (45.1%) patients were pseudophakic, 13 (41.9%) were aphakic, and 4 (12.9%) were phakic. The types of synechiae noted on the UBM included peripheral anterior synechiae in 30/31 (96.7%) eyes [Fig. 2], synechiae at the graft host junction in 13/31 (41.93%) eyes [Fig. 3], both peripheral anterior synechiae and graft. Host junction synechiae in 12/31 (38.7%) eyes [Fig. 4], central irido-corneal synechiae in 6/31 (19.3%) eyes [Fig. 5], and intraocular lens iris synechiae in 3/31 (9.6%) eyes. [Fig. 6]. This study concluded that secondary angle closure caused by anterior synechiae formation is one of the important causes for PPKG in eyes with opaque grafts. UBM, therefore, serves as a useful tool for anterior segment evaluation in such cases and can help in planning the site for glaucoma filtering surgeries and drainage devices.
Figure 2.
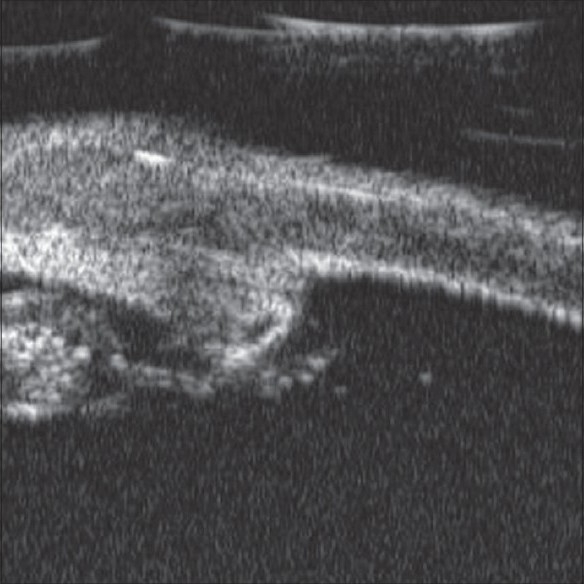
PAS on ultrasound biomicroscopy (UBM) (copyright owner Lippincott, Williams and Wilkins, 2008)
Figure 3.
Graft host junction (GH Jn) synechia on UBM (copyright owner Lippincott, Williams and Wilkins, 2008)
Figure 4.
Both PAS and GH Jn synechiae (copyright owner Lippincott, Williams and Wilkins, 2008)
Figure 5.
Central iris corneal synechia with ACIOL tilt (copyright owner Lippincott, Williams and Wilkins, 2008)
Figure 6.
IOL iris synechia (copyright owner Lippincott, Williams and Wilkins, 2008)
Management
Management of post-PK glaucoma (Appendix) is a complex issue and requires an insight into the pathophysiology leading to elevated IOP. It is important to take appropriate steps during surgery for primary prevention of this blinding disorder.
Prophylaxis
Preoperative factors
Pre-existing glaucoma is a major risk factor for post-operative glaucoma and graft failure and is especially difficult to treat in aphakic and pseudophakic eyes.18-20 Reinhard et al.19 estimated the 3-year graft survival rate in patients with a pre-operative history of glaucoma to be 71%, in contrast to 89% without such a history. A high incidence of graft failure has been reported if a glaucoma operation is performed following the PK.21 Some studies therefore suggest treating the glaucoma with mitomycin-C trabeculectomy22 or with a GDD23 combined with the PK surgery.
Intraoperative factors
During surgery, use of following procedures may reduce the risk for post-PK glaucoma: one-mm oversize donor button,11,24,25 deep bites,10 goniosynechiolysis, iridoplasty (iris tightening procedure) - [Fig. 7] in cases of a floppy iris,13 viscoelastic removal at the end of surgery, and careful wound closure to prevent post-operative wound leaks.
Figure 7.
PK with concomitant iridoplasty (courtesy of Dr. Namrata Sharma, Dr. R.P. Centre)
Post-operative factors
Post-operatively, judicious use of topical steroids controls the inflammation and prevents PAS formation. Cycloplegics keep the pupil mobile and prevent pupillary block glaucoma. The IOP must be monitored as long-term use of steroid therapy can lead to secondary open angle glaucoma.
Medical management
Use of topical medications to control IOP is still the first-line treatment of post-PK glaucoma. The following medications can be used:
Beta adrenergic blockers (timolol and betaxolol), alpha- 2-adrenergic agonists (brimonidine), miotics (pilocarpine), prostaglandin analogs (latanoprost, travoprost, and bimatoprost), and carbonic anhydrase inhibitors (acetazolamide and methazolamide).
Beta adrenergic blocking agents and adrenergic agonists act by decreasing aqueous humor production having no effect on outflow pathways. Adrenergic agents are rarely used in current practice, as they are not very effective and cause chronic conjunctival inflammation. Brimonidine tartarate 0.2% or 0.15% with purite preservative can be used (thrice daily as monotherapy and twice daily as combination therapy). Apraclonidine (0.5%) is a potent vasoconstrictor and is useful both to prevent AC bleeding during the operation and to treat resultant IOP spikes post-operatively from such a bleed. Miotics have little effect in the presence of angle closure caused by PAS and are no longer recommended.
Systemic carbonic anhydrase inhibitors are very useful as a short-term therapy in the early post-operative period to control the IOP. Long-term therapy is limited by serious side effects such as tinnitus, nausea, gastrointestinal disturbances, paresthesias, fatigue, depression, anorexia, weight loss, nephrolithiasis, and blood dyscrasias.26 Topical carbonic anhydrase inhibitors (dorzolamide and brinzolamide) should be used with caution as they also suppress the carbonic anhydrase enzyme in the corneal endothelium and long-term use can lead to graft decompensation.27,28 Although these groups of drugs can be safely used in healthy grafts with good endothelial reserve, their use for a long period of time should be avoided in cases with marginal endothelial reserve.
Prostaglandin analogs can also be used to decrease IOP by increasing uveoscleral outflow and can be used in conjunction with beta blockers. Preservatives, such as benzalkonium chloride (BAC; 0.01%) used in majority of topical antiglaucoma medication, have a toxic effect on corneal epithelium and one should try and use preservative free unims for long-term therapy.
When using topical drugs to lower the IOP, one has to keep in mind the side effects that are peculiar to them in the setting of post-PK glaucoma. Beta adrenergic blockers can lead to superficial punctate keratopathy, exacerbation of dry eye, and corneal anesthesia all of which by themselves can be detrimental to the state of the graft. Alpha-2-adrenergic agonist drugs can lead to allergic periocular reactions, besides superficial punctate keratopathy and dry eyes. The use of miotics in this setting is discouraged, because they promote breakdown of blood aqueous barrier, thus stimulating graft rejection and increasing the risk of retinal detachment, particularly in aphakes. The prolonged use of topical carbonic anhydrase inhibitors can lead to graft decompensation in the presence of borderline corneal endothelial status. Finally, the prostaglandin analogs should also be used with caution as they may lead to uveitis, cystoid macular edema (CME) in aphakia and pseudophakia, and reactivation of herpes simplex keratitis in patients grafted with a previous history of healed herpetic keratitis. The use of adrenergic agents like epinephrine, dipivefrin is also discouraged in the modern day management of these patients because of their potential corneal epithelial toxicity, exacerbation of CME in aphakes, pseudophakes and promotion of conjunctival inflammation thereby making future surgical intervention all the more difficult.
In cases of steroid responsive glaucoma, the dose of steroid drops may be tapered to the minimum required. Alternatively, stronger steroid drops can be replaced by steroids that have less tendency to increase IOP such as topical fluorometholone, loteprednol, and rimexolone. Cyclosporine A 0.5-2.0% topical drops four times daily can be substituted for steroids and this can also help to control the IOP.29
Surgical management
The following options are available:
Laser trabeculoplasty
Laser iridoplasty/iridotomy
Trabeculectomy with antimetabolites
GDDs
Laser trabeculoplasty
Argon laser trabeculoplasty (ALT) can be used if the angle is open. Recommended settings are a 50-µ spot size, 0.1-sec duration, and 600-900 mW of power.30 The laser is aimed at the junction of the pigmented and non-pigmented trabecular meshwork and the end point is minimal blanching or bubble formation. Complications are post-operative IOP spikes and uveitis, which can trigger graft rejection. It is imperative to give post-laser topical steroids at an increased frequency (two to four hourly) to minimize the chances of triggering graft rejection. ALT may be indicated in patients with open angles, clear grafts, and moderately elevated IOP (20-25 mmHg) on glaucoma medications. Diode laser trabeculoplasty and selective laser trabeculoplasty may also be used.
Laser iridotomy may be performed with an Nd:YAG (neodymium:yttrium-aluminium-garnet) laser, if a pupillary block is suspected. Gonioplasty can be done for PAS, which has been present for less than one year.
Trabeculectomy
Conventional trabeculectomy is usually not effective due to dense perilimbal scarring and fibrosis with an increased risk of failure. The failure rate is further increased in aphakic eyes where it is mandatory to do a vitrectomy to prevent any vitreous from blocking the trabeculectomy ostium. Antimetabolites (5-fluorouracil and mitomycin-C) must be used in these patients to inhibit the fibroblastic response.22,31 Five milligrams of 5 FU in 0.1 cc is given daily as a subconjunctival injection in the immediate post-operative period for 7-10 days.31 Apart from the inconvenience of daily injections, 5-FU injections are associated with a high rate of corneal epithelial toxicity and therefore should be used with caution in patients with post-PK glaucoma.
Mitomycin-C application (0.2-0.4 mg applied for 1-4 min subconjunctival or sub-scleral) has significantly improved the success rate of filtering surgery for glaucoma.31
The reported success rate in IOP control with mitomycin trabeculectomy in patients with post-PK glaucoma is 67-91% and that of graft failure is 12-18%.32,33 Intraoperative care must be taken to prevent shallowing of AC to minimize endothelial loss, and mitomycin-C should be thoroughly washed off prior to entry into the AC.
Glaucoma drainage devices
Glaucoma drainage devices create an alternate aqueous pathway by channeling aqueous from the AC through a long tube to an equatorial plate that promotes bleb formation. In 1987, Kirkness was the first to report the use of GDD in post- PK glaucoma.34 Although the use of GDDs appears to control glaucoma in a high percentage of patients in all published series (71-96%, with an average of 84.8%), it appears to be associated with a high incidence of graft failure in the range of 10-51% (average 36.2%).33,37-39 The risk of graft rejection may be increased after GDD surgery, because the drainage tube may provide a conduit for retrograde passage of inflammatory cells into the AC. It is important to note that the risk of graft rejection following the insertion of any GDD whether valved or non-valved is similar. This implies that other mechanisms besides passage of inflammatory cells into the AC through the tube may play a role. Inflammation caused by the surgical procedure itself may lead to post-surgical uveitis and breakdown of blood aqueous barrier, triggering graft rejection.
The etiology of graft failure probably is multifactorial. The presence of underlying chronic inflammation, extensive PAS, and multiple previous surgeries may compromise the graft. It has been seen that most corneal transplants undergo a 60% reduction in the central endothelial cell count during the first two post-operative years after implant surgery.35 The complication associated with GDDs like shallow AC with iris/ tube graft endothelial touch might accelerate the process leading to graft failure. Meticulous surgery should be done to avoid the complication of flat AC and tube endothelial touch. The use of high-dose steroids for 3-6 months in the post-operative phase may help in controlling and suppressing inflammation. Other complications include conjunctival erosion, prolonged hypotony, tube endothelial touch, tube obstruction, tube failure, retinal detachment, tube plate extrusion, epithelial down growth, and infection.
There are two types of GDDs, which can be used: (i) valved - offers resistance to out flow (Ahmed valve; Krupin implant); (ii) valveless - no resistance to out flow (Molteno implant, Baerveldt implant). The advantages of the valved devices, especially that of the Ahmed glaucoma valve,36 is the ease of insertion and low incidence of hypotony in the immediate post-operative phase. However, the Ahmed valve is associated with a high incidence of increased IOP - hypertensive phase (as much as 80%), 1-3 months after the operation, which may need needling and 5-FU injections.36 On the other hand, GDDs with a larger surface area, such as the double-plate Molteno and Baerveldt implant, appear to exhibit a lesser incidence of the hypertensive phase and may achieve slightly lower IOPs in the long term. The overall success rate and other complications, including corneal decompensation, appear to be similar among all GDDs.37-39
It is preferred to use the Ahmed glaucoma valve in patients with mild-to-moderate glaucomatous optic nerve damage and larger surface area devices, such as the double-plate Molteno and the Baerveldt implant, which are associated with more significant pressure reduction in patients with more advanced optic nerve damage.
Cyclodestructive procedures
Cyclodestructive procedures aim to control the IOP by decreasing aqueous humor production by destroying part of the ciliary body. Cyclocryotherapy, transscleral cyclophotocoagulation with diode or krypton laser are the various procedures that can be performed on patients with intractable post-PK glaucoma. Since conventional filtering surgeries and GDDs have a high failure rate, cyclophotocoagulation is a widely adopted procedure, because it is non-invasive and can be done as a low-cost outpatient procedure.
Cyclocryotherapy has been a principal mode of treatment of post-PK glaucoma. The glaucoma cryoprobe is placed for 1 min, 1.5 mm behind the corneoscleral limbus. A total of 6-8 applications are made with equidistant spots, involving the inferior 180° or 270° circumference of the globe at a temperature of −60°C to −80°C. Two to three clock-hours of the superior quadrant of the globe should be left untreated to allow for a future filtering surgery procedure. The treatment can be repeated if indicated. Complications of this procedure include uveitis, immediate rise in IOP, graft failure, corneal decompensation, macular edema, cataract, vitreous hemorrhage, and phthisis bulbi.
Nd:YAG laser cyclophotocoagulation40 involves the use of 15 evenly spaced burns, placed 1-1.5 mm from the limbus for 180° with a Nd:YAG laser.37 The recommended mean energy level is 4.0-9.0 J. Post-operative pain medication and topical steroids are indicated. Low energy settings are preferred in patients previously treated with cyclocryotherapy or filtering procedure to avoid hypotony. Repeated applications may be necessary before adequate control is achieved.
Diode laser cyclophotocoagulation41 utilizes a semiconductor diode laser with a wave length of 810 nm, has lower scleral transmission than the Nd:YAG laser (1064 nm) but greater absorption by melanin. As semiconductor diodes have solid-state construction, they have the advantage of portability, durability, and smaller size as compared with Nd:YAG lasers. The recommended power settings with the diode laser are 1250-2000 mW, with a 2-sec exposure time. An initial power setting of 1500 mW is increased or decreased by 250-mW increments until it is 250 mW below that producing an audible popping sound. Complications include decrease in the Snellen visual acuity (22-56%), graft failure (11-65%), persistent hypotony (5-10%), anterior uveitis, epithelial defects, and loss of vision, severe pain, phthisis bulbi, hyphema, hypotony, intractable pain, sympathetic ophthalmia, scleral thinning, and vitreous hemorrhage. It is recommended to avoid the 3 and 9 o′clock positions to spare the ciliary nerves.
Transpupillary argon laser photocoagulation42 is another modality that can be used. It has been seen that transpupillary argon laser photocoagulation of the ciliary process can reduce IOP in direct proportion to the number of ciliary processes ablated. The technique requires a Goldmann three-mirror lens. The laser is set at 50-100 µm spot size for a duration of 0.1-0.2 sec and with a power of 1000 mW. Hemostasis is obtained with repeated application of the laser with larger (200 µm) spot size, 0.2-sec duration, and lower power (250 mW). Ciliary processes are ablated one at a time. A limiting factor of transpupillary argon laser cyclophotocoagulation is the visualization of the processes requiring widely dilated pupil and specialized contact lens. Endoscopic cyclophotocoagulation43 is another technique that can be used.
Prognosis of Post-PK Glaucoma
Two things that are important in managing a case of post-PK glaucoma are the influence of glaucoma on graft survival and the effect of glaucoma in causing permanent irreversible visual loss. There is uniform agreement in literature regarding adverse outcomes on both of the above accounts. A study from our center based on a retrospective review of 747 PKs reported only 50% graft clarity over the study period18 and further worse only 19% of eyes could retain a visual acuity of 20/60 or better despite medical and surgical measures to control the glaucoma. One thing that needs to be kept in the mind while managing a case of post-PK glaucoma is that the PAS formation is progressive over time and that IOP control might worsen over long-term follow-up. Therefore, long-term vigilance is required in taking care of such eyes. Another issue that is important is the effect of any intervention on triggering graft rejection and subsequently graft failure. Kwon et al.,39 in their 3-year retrospective study, documented 44% graft rejection and non-immunologic causes of graft failure following insertion of GDDs in such eyes. Shah et al.41 determined the visual outcome after diode laser cyclophotocoagulation in 28 eyes with at least 6-month follow-up. They documented stable baseline visual acuity in 17 of the 28 (61%) patients and worsening in eight of the 28 (28%) patients.
Conclusion
Uncontrolled IOP after PK is one of the leading causes of graft failure and visual loss in this patient population. It is mandatory that the IOP is monitored on a regular basis after corneal transplantation and aggressively treated if found high. Any patient with pre-existing glaucoma must be carefully evaluated prior to the corneal transplants. Optimal surveillance and aggressive medical and surgical management can salvage both graft and vision in these already compromised eyes.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Foulks GN. Glaucoma associated with penetrating keratoplasty. Ophthalmology. 1987;94:871–4. doi: 10.1016/s0161-6420(87)33542-0. [DOI] [PubMed] [Google Scholar]
- 2.Wilson SE, Kaufman HE. Graft failure after penetrating keratoplasty. Surv Ophthalmol. 1990;34:325–56. doi: 10.1016/0039-6257(90)90110-h. [DOI] [PubMed] [Google Scholar]
- 3.Goldberg DB, Schanzlin DJ, Brown SI. Incidence of increased intraocular pressure after keratolasty. Am J Ophthalmol. 1981;92:372–7. doi: 10.1016/0002-9394(81)90527-4. [DOI] [PubMed] [Google Scholar]
- 4.Ayyala RS. Penetrating keratoplasty and glaucoma. Surv Ophthalmol. 2000;45:91–105. doi: 10.1016/s0039-6257(00)00141-7. [DOI] [PubMed] [Google Scholar]
- 5.Irvine AR, Kaufman HE. Intraocular pressure following penetrating keratoplasty. Am J Ophthalmol. 1969;68:835–44. doi: 10.1016/0002-9394(69)94577-2. [DOI] [PubMed] [Google Scholar]
- 6.Karesh JW, Nirankari VS. Factors associated with glaucoma after penetrating keratoplasty. Am J Ophthalmol. 1983;96:160–4. doi: 10.1016/s0002-9394(14)77783-9. [DOI] [PubMed] [Google Scholar]
- 7.Chien AM, Schimdt CM, Cohen E. Glaucoma in the immediate post operative period after penetrating keratoplasty. Am J Ophthalmol. 1993;115:711–4. doi: 10.1016/s0002-9394(14)73636-0. [DOI] [PubMed] [Google Scholar]
- 8.Olson RJ, Kaufman HE. A mathematical description of causative factors and prevention of elevated intraocular pressure after keratoplasty. Invest Ophthalmol Vis Sci. 1977;16:1085–92. [PubMed] [Google Scholar]
- 9.Kirkness CM, Moshegov C. Post keratoplasty glaucoma. Eye. 1988;2:19–26. doi: 10.1038/eye.1988.130. [DOI] [PubMed] [Google Scholar]
- 10.Zimmerman TJ, Krupin T, Grodzki W. the effect of suture depth on outflow facility in penetrating keratoplasty. Arch Ophthalmol. 1978;96:505–6. doi: 10.1001/archopht.1978.03910050273018. [DOI] [PubMed] [Google Scholar]
- 11.Zimmerman TJ, Olson RJ, Waltman S, Kaufman H. Transplant size and elevated intraocular pressure: Postkeratoplasty. Arch Ophthalmol. 1978;96:2231–3. doi: 10.1001/archopht.1978.03910060533012. [DOI] [PubMed] [Google Scholar]
- 12.Lass JH, Pavan-Langston D. Timolol therapy in secondary angle closure glaucoma post penetrating keratoplasty. Ophthalmology. 1979;86:54–9. doi: 10.1016/s0161-6420(79)35545-2. [DOI] [PubMed] [Google Scholar]
- 13.Cohen EJ, Kenyon KR, Dohlmam CH. Iridoplasty for prevention of post keratoplasty angle closure glaucoma. Ophthalmic Surg. 1982;13:994–6. [PubMed] [Google Scholar]
- 14.McMillan F, Forster RK. Comparison of MacKay-Marg, Goldmann and Perkins′ tonometers in abnormal corneas. Arch Ophthalmol. 1975;93:420–4. doi: 10.1001/archopht.1975.01010020434007. [DOI] [PubMed] [Google Scholar]
- 15.Doughty MJ, Zaman ML. Human corneal thickness and its impact on intraocular measures: A review and meta-analysis approach. Surv Ophthalmol. 2000;44:367–408. doi: 10.1016/s0039-6257(00)00110-7. [DOI] [PubMed] [Google Scholar]
- 16.Rubinfeld RS, Cohen EJ, Laibson PR. The accuracy of finger tension for estimating intraocular pressure after penetrating keratoplasty. Ophthalmic Surg Lasers. 1998;29:213–5. [PubMed] [Google Scholar]
- 17.Dada T, Aggarwal A, Vanathi M, Gadia R, Panda A, Gupta V, et al. Ultrasound biomicroscopy in opaque grafts with post-penetrating keratoplasty glaucoma. Cornea. 2008;27:402–5. doi: 10.1097/ICO.0b013e31816373c5. [DOI] [PubMed] [Google Scholar]
- 18.Sihota R, Sharma N, Panda A, Aggarwal HC, Singh R. Post penetrating keratoplasty glaucoma: Risk factors, management and visual outcome. Aust NZJ Ophthalmol. 1998;26:305–9. doi: 10.1111/j.1442-9071.1998.tb01334.x. [DOI] [PubMed] [Google Scholar]
- 19.Reinhard T, Kallmann C, Cepin A. The influence of glaucoma history on raft survival after penetrating keratoplasty. Graefes Arch Clin Exp Ophthalmol. 1997;235:553–7. doi: 10.1007/BF00947083. [DOI] [PubMed] [Google Scholar]
- 20.Yamagami S, Suzuki Y, Tsuru T. Risk factors for graft failure in penetrating keratoplasty. Acta Ophthalmol Scand. 1996;74:584–8. doi: 10.1111/j.1600-0420.1996.tb00740.x. [DOI] [PubMed] [Google Scholar]
- 21.Kirkness CM, Steele AD, Ficker LA. Coexistent corneal disease and glaucoma managed by either drainage surgery and subsequent keratoplasty or combined drainage surgery and penetrating keratoplasty. Br J Ophthalmol. 1992;76:146–52. doi: 10.1136/bjo.76.3.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Figuerido RS, Araujo SV, Cohen EJ. Management of coexisting corneal disease and glaucoma by combined penetrating keratoplasty and trabeculectomy with mitomycin C. Ophthalmic Surg Lasers. 1996;27:903–9. [PubMed] [Google Scholar]
- 23.Rapuano CJ, Schimdt CM, Cohen EJ. Results of alloplastic tube shunt procedures before, during, or after penetrating keratoplasty. Cornea. 1995;14:26–32. [PubMed] [Google Scholar]
- 24.Bourne WM, Davison JA. The effects of oversize donor buttons on post operative intraocular pressure and corneal curvature in aphakic penetrating keratoplasty. Ophthalmology. 1982;89:242–6. doi: 10.1016/s0161-6420(82)34809-5. [DOI] [PubMed] [Google Scholar]
- 25.Vajpayee RB, Dada T, Ray M, Tandon R, Sethi A, Turaka K. Oversized corneal grafts for corneal opacities with iridocorneal adhesions. Ophthalmology. 2001;108:2026–8. doi: 10.1016/s0161-6420(01)00772-2. [DOI] [PubMed] [Google Scholar]
- 26.Epstein DL, Bramsen T, Sperling S. Carbonic anhydrase inhibitor side effects. Serum chemical analysis. Arch Ophthalmol. 1977;95:1378–82. doi: 10.1001/archopht.1977.04450080088009. [DOI] [PubMed] [Google Scholar]
- 27.Konowal A, Morrison JC, Brown SV. Irreversible corneal decompensation in patients treated with dorzolamide. Am J Ophthalmol. 1999;127:403–6. doi: 10.1016/s0002-9394(98)00438-3. [DOI] [PubMed] [Google Scholar]
- 28.Fraunfelder FT. Drugs used primarily in Ophthalmology. In: Mever SM, editor. Drug induced Ocular side effects and Drug interactions. Philadelphia: Lea and Febiger; 1989. pp. 476–7. [Google Scholar]
- 29.Perry HD, Donnenfeld ED, Kanellopoulos AJ, Grossman GA. Topical cyclosporine A in the management of postkeratoplasty glaucoma. Cornea. 1997;16:284–8. [PubMed] [Google Scholar]
- 30.Van meter WS, Allen RC, Waring CO. Laser trabeculoplasty for glaucoma in aphakia and pseudophakic eyes after penetrating keratoplasty. Arch Ophthalmol. 1988;106:185–8. doi: 10.1001/archopht.1988.01060130195023. [DOI] [PubMed] [Google Scholar]
- 31.Skuta GI, Beeson CC, Higginbotham EJ. Intraoperative mitomycin C versus post operative 5-flurouracil in high risk glaucoma filtration surgery. Ophthalmology. 1992;99:438–44. doi: 10.1016/s0161-6420(92)31951-7. [DOI] [PubMed] [Google Scholar]
- 32.Chowers I, Ticho U. Mitomycin-C in combined or two stage procedure trabeculectomy followed by penetrating keratoplasty. J Glaucoma. 1999;8:184–7. [PubMed] [Google Scholar]
- 33.Ayyala RS, Pieroth L, Vinals AF. Comparison of mitomycin C trabeculectomy, glaucoma drainage device implantation and laser neodymium YAG cyclophotocoagulation in the management of intractable glaucoma after penetrating keratoplasty. Ophthalmology. 1998;105:1550–6. doi: 10.1016/S0161-6420(98)98046-0. [DOI] [PubMed] [Google Scholar]
- 34.Kirkness CM. Penetrating keratoplasty, glaucoma and silicon drainage tubing. Dev Ophthalmol. 1987;14:161–5. doi: 10.1159/000414385. [DOI] [PubMed] [Google Scholar]
- 35.Bates AK, Hiorns RW, Cheng H. Modeling of changes in the corneal endothelium after cataract surgery and penetrating keratoplasty. Br J Ophthalmol. 1992;76:32–5. doi: 10.1136/bjo.76.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ayyala RS, Zurakowski D, Smith JA. A clinical study of Ahmed valve implant in advanced glaucoma. Ophthalmology. 1998;105:1968–76. doi: 10.1016/S0161-6420(98)91049-1. [DOI] [PubMed] [Google Scholar]
- 37.Abdulla Al-Torbak. Graft survival glaucoma outcome after simultaneous penetrating keratoplasty and Ahmed glaucoma valve implant. Cornea. 2003;22:194–7. doi: 10.1097/00003226-200304000-00002. [DOI] [PubMed] [Google Scholar]
- 38.Sidoti PA, Mosny AY, Ritterband DC, Seeder JA. Pars plana tube insertion of glaucoma drainage implants and penetrating keratoplasty in patients with coexisting glaucoma and corneal disease. Ophthalmology. 2001;108:1050–8. doi: 10.1016/s0161-6420(01)00583-8. [DOI] [PubMed] [Google Scholar]
- 39.Kwon YH, Taylor JM, Hong S, Honkanen RA, Zimmerman MB, Alward WL, et al. Long term results of eyes with penetrating keratoplasty and glaucoma drainage tube implant. Ophthalmology. 2001;108:272–8. doi: 10.1016/s0161-6420(00)00496-6. [DOI] [PubMed] [Google Scholar]
- 40.Threlkeld AB, Shields MB. Noncontact transscleral Nd: YAG cyclophotocoagulation for glaucoma after penetrating keratoplasty. Am J Ophthalmol. 1995;120:569–76. doi: 10.1016/s0002-9394(14)72203-2. [DOI] [PubMed] [Google Scholar]
- 41.Shah P, Lee GA, Kirwan JK, Bunce C, Bloom PA, Ficker LA, et al. Cyclodiode photocoagulation for refractory glaucoma after penetrating keratoplasty. Ophthalmology. 2001;108:1986–91. doi: 10.1016/s0161-6420(01)00767-9. [DOI] [PubMed] [Google Scholar]
- 42.Holz HA, Lim MC. Glaucoma lasers: A review of the newer techniques. Curr Opin Ophthalmol. 2005;16:89–93. doi: 10.1097/01.icu.0000156991.52256.56. [DOI] [PubMed] [Google Scholar]
- 43.Endoscopic cyclophotocoagulation. Br J Ophthalmol. 2002;86:1434–8. doi: 10.1136/bjo.86.12.1434. [DOI] [PMC free article] [PubMed] [Google Scholar]


