Abstract
Purpose:
To study the epidemiology and clinical profile of victims of ocular trauma in an urban slum population.
Materials and Methods:
This cross-sectional study, conducted on 500 families each in three randomly selected urban slums in Delhi, collected demographic data for all members of these families, and clinical data for all those who suffered ocular trauma at any time, that required medical attention. Data was managed on SPSS 11.0.
Results:
Of 6704 participants interviewed, 163 episodes of ocular trauma were reported by 158 participants (prevalence = 2.4%, confidence interval = 2.0 to 2.7) Mean age at trauma was 24.2 years. The association between the age of participants and the history of ocular trauma was significant (P < 0.001), when adjusted for sex, education and occupation. Males were significantly more affected. Blunt trauma was the commonest mode of injury (41.7%). Blindness resulted in 11.4% of injured eyes ( P = 0.028). Of 6704 participants, 1567 (23.4%) were illiterate, and no association was seen between education status and trauma, when adjusted for sex and age at injury. A significant association was noted between ocular trauma and workplace (Chi-square = 43.80, P < 0.001), and between blindness and place (Chi-square = 9.98, P = 0.041) and source (Chi-square = 10.88, P = 0.028) of ocular trauma. No association was found between visual outcome and the time interval between trauma and first consultation (Chi-square = 0.50, P = 0.78), between receiving treatment and the best corrected visual acuity (Chi-square = 0.81, P = 0.81), and between the person consulted and blinding ocular trauma (Chi-square = 1.88, P = 0.170).
Conclusion:
A significant burden of ocular trauma in the community requires that its prevention and early management be a public health priority.
Keywords: Epidemiology, ocular trauma, urban
Ocular trauma is a major cause of preventable monocular blindness and visual impairment in the world.1,2 Despite its public health importance, there is relatively less population- based data on the magnitude and risk factors for ocular trauma, specially from developing countries.3-7 Information on minor ocular injuries requires population-based studies.6,7 Most studies are based on hospital records, but such data do not accurately indicate the population at risk. Useful as they are, they suffer from a bias towards the more serious cases of ocular trauma and underestimate the true magnitude of ocular trauma in the community.1-3,8
Urban slums constitute a major part of the population in metropolitan cities like Delhi.9 The present study was designed to study the epidemiology, clinical characteristics and health- seeking behavior following ocular trauma in an urban slum population for designing and implementing improved methods of prevention.
Materials and Methods
This cross-sectional study included administration of questionnaires and an ophthalmic examination. The sample size was calculated taking a prevalence of ocular trauma as 2.5%, a precision of 80%, confidence level of 95%, design effect of 1.5 and coverage of 85%. The sample size thus obtained was 6148. The study area comprised three randomly selected urban slums in Delhi, out of the ten at which primary eye care services are provided by our center. A map of each slum was prepared and the study explained to the local community leaders and health-related personnel. In each slum, the first 500 families were sequentially selected after a door-to-door survey. Visits were usually conducted on Sundays to try and capture the maximum residents of the household. In case a house was found locked, two further visits were paid to contact the household members.
An interview was arranged with any of the available adult members of the family, preferably, the head of the family. The informed consent form was read out in the local vernacular to the participants, and their signature or thumb impression was taken on the form. The socio-demographic information about each family was recorded. This included family size, family type, age, gender, occupation, workplace of all family members, monthly income, per capita income, and educational status of participants aged more than seven years. History of ocular trauma was taken from all available adults while, for those less than 15 years of age, the parents or guardians were interviewed about the same. Details of each episode of ocular trauma were recorded with respect to the age at which injury occurred, place and source of trauma, treatment sought and the benefit of treatment. It was specifically asked if the trauma had been sustained during the last one month. This was to facilitate estimation of the cumulative incidence of ocular trauma, as the recall during the preceding one month was likely to be reliable.
Each member of the family, who sustained ocular trauma at any time in his/her lifetime requiring medical care, was offered a detailed ophthalmic examination. Visual acuity (Snellen′s) was recorded, and refraction performed if pinhole vision in the injured eye was <20/20 to arrive at the best corrected visual acuity (BCVA). The anterior segment was evaluated with diffuse light, slit-lamp (Haag Streit) and a Goldmann single mirror indirect gonioscope (Volk, USA). Posterior segment was evaluated using direct and indirect ophthalmoscope (Heine, Germany) with +20 D lens. Intraocular pressure (IOP) was measured either with a hand-held applanation tonometer (Perkin′s), or noted digitally. Visual fields were tested by confrontation method. Referral to the base hospital was made as appropriate.
The data collected were suitably coded and entered into pre-designed Microsoft Access software. Data analysis was done with SPSS 11.0 Package.
Results
Of the 1500 families, 1437 (95.8%) could be contacted. A total of 6704 participants were interviewed. There were 158 participants and 163 episodes of ocular trauma (2.4%). The distribution of ocular trauma with respect to age and gender is displayed in Table 1. The association between gender and ocular trauma was significant (Chi-square = 9.59, P = 0.002).
Table 1.
Distribution of ocular trauma among participants with respect to gender and age
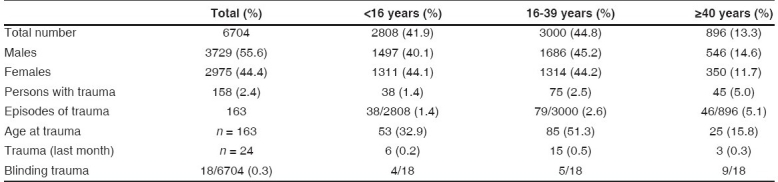
The mean age of the participants was 28.21 years (±14.6). The mean age at which ocular trauma was sustained was 24.2 years (±13.5). The association between the age of participants and the history of ocular trauma was significant (P < 0.001), when adjusted for sex, education and occupation. The association with age at ocular trauma was not significant (P = 0.944) when adjusted for sex, education and occupation. All injuries sustained at <16 years were unsupervised.
Of the 6704 participants, 1567 (23.4%) were illiterate. Of them, 38 (2.4%) reported episodes of ocular trauma. Episodes of ocular trauma was reported by 42 (2.5%) of 1694 participants who had studied up to less than the fifth standard, 36 (2.9%) of 1226 participants who had studied up to the fifth standard, 23 (3.8%) of 604 participants who had studied up to the eighth standard, and 13 (2.8%) of 467 participants who had studied up to 10th standard or higher. No significant association was seen between the education status and ocular trauma (P = 0.21), when adjusted for age at ocular injury and sex.
Of the 69 participants who had furniture-related workplaces, 10 (14.5%) sustained workplace-related ocular trauma. Similarly, five (3.5%) of 141 participants working in a metal factory, five (6.1%) of 82 participants working in driving-related occupations, and 18 (3.7%) of 489 participants working in construction-related occupations sustained ocular trauma. Of the 163 episodes, 54 (33.1%) were sustained at the workplace; in all cases no protective gear was used. Fifty-four (33.1%) episodes occurred at home, 12 (7.4%) at school, six (3.7%) on roads or by the roadside, 13 (8.0%) episodes were sustained during popular festivals, and 24 (14.7%) were games or recreation-related. Cricket (plastic ball) accounted for 19 (11.7%), ″Gilli-Danda″ four (2.5%), and kite flying one (0.6%). The association between workplace and ocular trauma was significant (Chi-square = 43.80, P< 0.001). The association between occupation and history of ocular trauma was not significant when adjusted for age and sex (P = 0.88).
One hundred and forty-two (87.1%) episodes were due to accidents, 17 (10.4%) due to alleged assault, and four (2.5%) were self-inflicted. The sources of ocular trauma are listed in Table 2.
Table 2.
Distribution of ocular trauma with respect to source of trauma
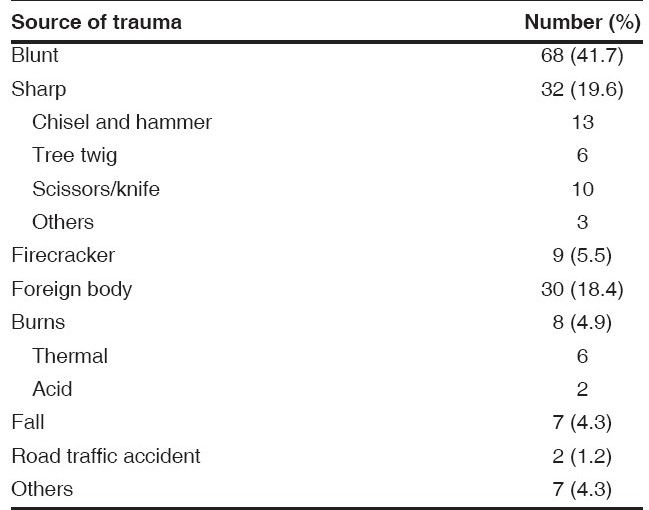
Blindness, defined as BCVA of less than 20/200 in the affected eye, was seen in 18 of the 158 eyes with trauma (11.4%). Half were affected before 12 years and 100% by 40 years (mean 24.24 ± 13.30 years). Blinding trauma was sustained by nine (24.3%) of 37 participants during recreational or sports activity, six (11.5%) of 52 participants at home, and three (5.9%) of 51 participants at work. All participants who sustained ocular trauma either at school or by the roadside had BCVA > 20/200. Blunt objects were implicated in eight (44.4%) eyes, firecracker injury and sharp objects in four (22.2%) eyes each, and foreign body and fall in one (5.6%) eye each. A significant association was seen between blindness and the place of ocular trauma (Chi-square = 9.98, P = 0.041), blindness and the source of trauma (Chi-square = 10.88, P = 0.028), the age at presentation of blinding trauma and the number of participants (Chi- square = 20.95, P< 0.001).
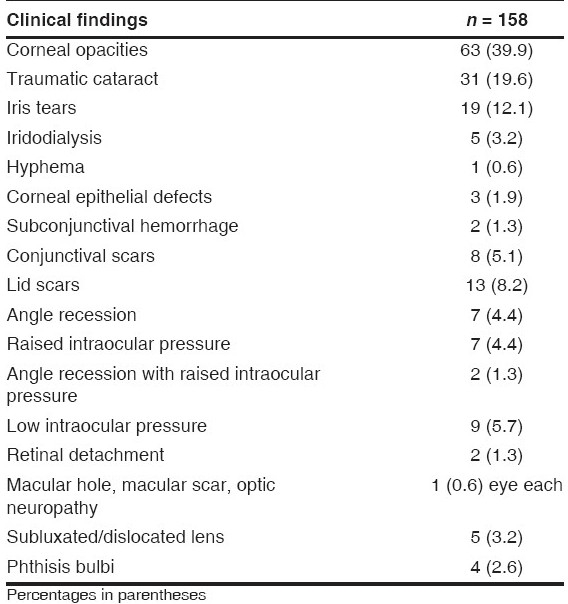
Clinical findings in eyes with ocular trauma are listed in Table 3. Blindness resulted from phthisis (n = 4), corneal scars (n = 6), cataract (n = 3), retinal detachment (n = 2), and macular scar, hyphema and optic neuropathy in one eye each.
Table 3.
Clinical findings in the eyes with ocular trauma
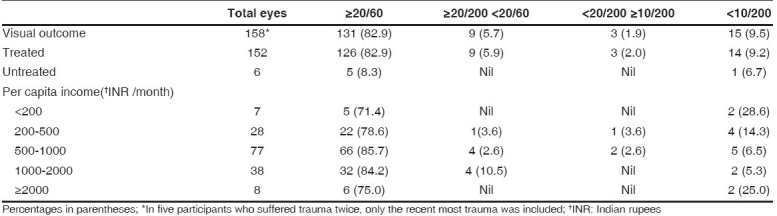
No significant association was found between visual outcome and the time interval between the trauma and first consultation (Chi-square = 0.50, P = 0.78). One participant never consulted anyone.
Twenty-four participants out of the 158, sustained ocular trauma to one eye each in the preceding one month. These included 18 males and six females. Of these, 13 (54.2%) participants had consulted an ophthalmologist, while six (25.0%) had consulted a general practitioner. Blunt trauma was responsible for seven (29.2%) episodes, sharp objects for three (12.5%), foreign bodies for nine (37.5%), and thermal burns for three (12.5%) episodes.
One hundred and thirty-nine (85.3%) episodes were treated with eye drops and/or oral drugs, and surgery performed in 18 (11.0%). Hospitalization was required in nine (5.7%) cases (mean = 1.8 days). The mean number of days off work was 1.26 days. Of six untreated episodes, five were reported in the last one month. An ophthalmologist was consulted in 110 (67.8%) episodes, following which 92 (83.6%) reported some benefit, 16 (14.5%) reported none and two (1.3%) were unsure of any. In 43 episodes in which a general practitioner was consulted, benefit was reported in seven (16.3%) and none in 36 (83.7%). In four episodes others were consulted, and benefit was reported in one (25%) and none in three (75%).
The association between having received treatment and the BCVA was not significant (Chi-square = 0.81, P = 0.81) [Table 4]. Blinding ocular trauma was seen in 13 (12.3%) of 106 participants who consulted an ophthalmologist, and four (25%) of 16 participants who consulted a non-ophthalmologist. Of the four participants who consulted others, two (50%) had blinding trauma. There was no association between the person consulted and blinding ocular trauma (Chi-square = 1.88, P = 0.170).
Table 4.
Distribution of best corrected visual acuity after ocular trauma with respect to treatment status per capita income
Discussion
The prevalence of ocular trauma in our study (2.4%) is lower than in other studies (3.97%).6 The cumulative lifetime prevalence of ocular trauma at ≥40 years has been reported as 4.5%, 14.4% and 21.1%.1,3,4 The estimated cumulative incidence risk of ocular trauma in our study is 4.3% based on reported ocular trauma in the preceding month. The reported annual incidence is 1.6%, and 980 per 100,000.4,5 The reported cumulative prevalence of visual impairment (VA< 20/40) due to ocular trauma is 8.5 per 1000 persons.5 Blinding ocular trauma in our study (0.3%) is lower than that reported as 0.60%, and 7.3 per 1000 people.4,6
The association between the age of participants and history of ocular trauma indicates the cumulative lifetime occurrence of ocular trauma. Differences could be related to recall bias, where older episodes of ocular trauma may have been underreported, while those episodes of ocular trauma significant enough to require treatment may have been recollected more often.
Hospital-based studies report lower figures for annual incidence of ocular trauma and annual incidence of hospitalized ocular trauma.5 A population-based study reported an annual incidence of 9.75 injuries per 1000 adults, significant enough to require treatment.5 A rural population (4.5%) may have a higher prevalence as compared to an urban one (3.97%).6,7 Our study also found men, children and young adults to be more prone to ocular trauma. Unskilled and semi-skilled workers, and lower socioeconomic classes, such as laborers, had a higher prevalence of ocular trauma, consistent with previous reports.4,6 In contrast, data from developed countries indicate that the highest rates of eye injuries are for communication (1.4%), and tradespersons (1.8%).3 Racial differences have also been noted.1
In our study, the majority of ocular injuries were sustained at work and home, and blunt trauma (41.7%) was more commonly implicated than sharp objects (19.6%).2 While this is consistent with some, others have found injuries by sharp objects, such as arrows, to be more common.3,4,7 Consultation with an ophthalmologist (74.2%) was similar to that reported by others, but the source of treatment is not significantly correlated with blindness, as noted previously.7 Of note is that even in developed countries, no treatment was sought for as high as 18% of the injuries, of which 9% turned out to be visually impairing or blinding.1
Our study did not corroborate the reported decreased risk of ocular trauma in literates, but it corroborated a decline in incidence of eye injury in late adulthood.2,7 We noted a lower incidence of sports-related (22.7%) ocular trauma than others (>50%), and also a lower prevalence of ocular trauma (32.9%) in the younger age group of <16 years as compared to reports of 47% for those below 17 years.6 Ocular trauma due to sports or recreational activities have worse visual outcomes, as do firecracker injuries.
In our study, the persons who sustained ocular trauma at their workplace used no protective gear. It is essential that protective equipment be used in all such instances for the prevention of ocular injuries.
Our study indicates a significant burden of ocular trauma in the urban slum population of Delhi in India, which has not been previously reported. The lifetime prevalence of ocular trauma is higher than for diseases like glaucoma, age-related macular degeneration, or diabetic retinopathy.7 The fact that treatment, even by an ophthalmologist, did not significantly influence the final visual outcome, makes it imperative that preventive eye care programs consider ocular trauma in the population as a priority. Public health education aimed at increasing awareness among parents, guardians and school teachers regarding the need for supervision of children, and institution of prevention programs, especially for vulnerable groups, is urgently needed in order to reduce ocular morbidity due to ocular trauma.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Katz J, Tielsch JM. Lifetime prevalence of ocular injuries from the Baltimore Eye Survey. Arch Ophthalmol. 1993;111:1564–8. doi: 10.1001/archopht.1993.01090110130038. [DOI] [PubMed] [Google Scholar]
- 2.Schein OD, Hibberd P, Shingleton BJ, Kunzweiler T, Frambach DA, Seddon JM, et al. The spectrum and burden of ocular injury. Ophthalmology. 1988;95:300–5. doi: 10.1016/s0161-6420(88)33183-0. [DOI] [PubMed] [Google Scholar]
- 3.McCarty CA, Fu CL, Taylor HR. Epidemiology of ocular trauma in Australia. Ophthalmology. 1999;106:1847–52. doi: 10.1016/S0161-6420(99)90361-5. [DOI] [PubMed] [Google Scholar]
- 4.Wong TY, Klein BE, Klein R. TThe prevalence and 5-Year incidence of ocular trauma. The Beaver Dam Eye Study. Ophthalmology. 2000;107:2196–202. doi: 10.1016/s0161-6420(00)00390-0. [DOI] [PubMed] [Google Scholar]
- 5.Glynn RJ, Seddon JM, Berlin BM. The incidence of eye injuries in New England adults. Arch Ophthalmol. 1988;106:785–9. doi: 10.1001/archopht.1988.01060130855039. [DOI] [PubMed] [Google Scholar]
- 6.Dandona L, Dandona R, Srinivas M, John RK, McCarty CA, Rao GN. Ocular trauma in an urban population in southern India: The Andhra Pradesh Eye Disease Study. Clin Exp Ophthalmol. 2000;28:350–6. doi: 10.1046/j.1442-9071.2000.00334.x. [DOI] [PubMed] [Google Scholar]
- 7.Nirmalan PK, Katz J, Tielsch JM, Robin AL, Thulasiraj RD, Krishnadas R, et al. Ocular trauma in a rural south Indian population: The Aravind Comprehensive Eye Survey. Ophthalmology. 2004;111:1778–81. doi: 10.1016/j.ophtha.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 8.Wong TY, Tielsch JM. A population based study on the incidence of severe ocular trauma in Singapore. Am J Ophthalmol. 1999;128:345–51. doi: 10.1016/s0002-9394(99)00167-1. [DOI] [PubMed] [Google Scholar]
- 9. [[cited on 2006 Aug 20]]. Available from: http://www.censusindianet/results/slum1html/


