Abstract
Objective
To compare the prevalence of underweight as calculated from Indian Academy of Paediatrics (IAP) growth curves (based on the Harvard scale) and the new WHO Child Growth Standards.
Methods
We randomly selected 806 children under 6 years of age from 45 primary anganwadi (childcare) centres in Chandigarh, Punjab, India, that were chosen through multistage stratified random sampling. Children were weighed, and their weight for age was calculated using IAP curves and WHO growth references. Nutritional status according to the WHO Child Growth Standards was analysed using WHO Anthro statistical software (beta version, 17 February 2006). The χ² test was used to determine statistical significance at the 0.05 significance level.
Findings
The prevalence of underweight (Z score less than –2) in the first 6 months of life was nearly 1.6 times higher when calculated in accordance with the new WHO standards rather than IAP growth curves. For all ages combined, the estimated prevalence of underweight was 1.4 times higher when IAP standards instead of the new WHO standards were used. Similarly, the prevalence of underweight in both sexes combined was 14.5% higher when IAP standards rather than the new WHO growth standards were applied (P < 0.001). By contrast, severe malnutrition estimated for both sexes were 3.8 times higher when the new WHO standards were used in place of IAP standards (P < 0.001).
Conclusion
The new WHO growth standards will project a lower prevalence of overall underweight children and provide superior growth tracking than IAP standards, especially in the first 6 months of life and among severely malnourished children.
Résumé
Objectif
Comparer les prévalences du déficit pondéral obtenues à partir des courbes de croissance de l’Académie Indienne de pédiatrie (reposant sur l’échelle de Harvard) et à partir des nouvelles normes OMS de croissance de l’enfant.
Méthodes
Nous avons sélectionné au hasard 806 enfants de moins de 6 ans dans 45 centres de soins pédiatriques (anganwadi) de la ville de Chandigarh, située au Punjab en Inde, par sondage aléatoire stratifié à plusieurs degrés. Ces enfants ont été pesés et on a calculé quel devait être leur poids en fonction de l’âge d’après les courbes de l’Académie Indienne de Pédiatrie et d’après les références de croissance de l’OMS. Leur état nutritionnel selon les normes OMS a été analysé à l’aide du logiciel statistique Anthro de l’OMS (version bêta du 17 février 2006). Le test du chi2 a été utilisé pour déterminer la signification statistique au niveau de significativité 0,05.
Résultats
La prévalence du déficit pondéral (score de Z < –2) au cours des 6 premiers mois de vie, déterminée à partir des normes OMS, était près de 1,6 fois supérieure à celle obtenue à partir des courbes de l’Académie de pédiatrie. Tous âges confondus, on obtenait une estimation de la prévalence du déficit pondéral 1,4 fois plus élevée en utilisant les courbes de l’Académie de Pédiatrie plutôt que les normes OMS de croissance. De même, la prévalence du déficit pondéral pour l’ensemble des deux sexes, calculée à partir des courbes de l’Académie de Pédiatrie, était supérieure de 14,5% à celle déterminée d’après les normes OMS (p < 0,001). A l’inverse, l’emploi des normes OMS conduisait à une estimation de la malnutrition sévère pour les deux sexes 3,8 fois plus élevée que l’utilisation des courbes de l’Académie de Pédiatrie (p < 0, 001).
Conclusion
Les normes OMS de croissance de l’enfant prévoiront une moindre prévalence globale du déficit pondéral chez l’enfant tout en fournissant cependant un meilleur moyen de suivi de la croissance que les courbes de l’Académie Indienne de Pédiatrie, en particulier pour les 6 premiers mois de vie et chez les enfants sévèrement malnutris.
Resumen
Objetivo
Comparar la prevalencia de la insuficiencia ponderal calculada a partir de las curvas de crecimiento de la Academia de Pediatría de la India (IAP) (basadas en la escala de Harvard) con la estimada mediante los nuevos patrones de crecimiento infantil de la OMS.
Métodos
Seleccionamos aleatoriamente a 806 niños menores de 6 años de 45 anganwadi (guarderías) de Chandigarh, Punjab, India, mediante un proceso de muestreo aleatorio estratificado multietápico. Tras pesar a los niños, se calculaba su peso para la edad utilizando las curvas de la IAP y los patrones de crecimiento de la OMS. Su estado nutricional según los patrones de crecimiento infantil de la OMS se analizó usando el software de estadística Anthro de la OMS (versión beta, 17 de febrero de 2006). Se aplicó la prueba chi-cuadrado para determinar la significación estadística a nivel de 0,05.
Resultados
La prevalencia de insuficiencia ponderal (Z < -2) en los primeros 6 meses de vida fue casi 1,6 veces mayor cuando se calculó mediante los patrones de la OMS que cuando se emplearon las curvas de crecimiento de la IAP. Para todas las edades combinadas, la prevalencia estimada de insuficiencia ponderal fue 1,4 veces mayor con los patrones de la IAP que con los de la OMS. Análogamente, la prevalencia de insuficiencia en los dos sexos considerados conjuntamente fue un 14,5% superior cuando se emplearon los patrones de la IAP que cuando se usaron los patrones de crecimiento de la OMS (p < 0,001). En cambio, la malnutrición grave estimada para los dos sexos fue 3,8 veces mayor con las curvas de la OMS que con las de la IAP (p < 0,001).
Conclusión
Los patrones de crecimiento de la OMS arrojan una menor prevalencia de insuficiencia ponderal global entre los niños y han de permitir realizar un mejor seguimiento del crecimiento que los patrones de la IAP, sobre todo durante los seis primeros meses de vida y entre los niños con malnutrición grave.
ملخص
الغرض
استهدفت هذه الدراسة المقارنة بين معدل انتشار الوزن المنخفض، المحسوب على أساس منحنيات النمو المحددة من قِبَل الأكاديمية الهندية لطب الأطفال (المستندة إلى مقياس هارفارد)، وبين المعدل المحسوب وفقا لمعايـير منظمة الصحة العالمية الجديدة لنمو الطفل.
الطريقة
تم انتقاء 806 أطفال دون السادسة من العمر، بطريقة عشوائية، من 45 مركزاً لرعاية الأطفال في تشانديغرا، بولاية البنجاب، بالهند، تم اختيارها بطريقة أخذ العينات الطباقية العشوائية. وتم وزن الأطفال، وحساب وزنهم بالنسبة إلى العمر باستخدام منحنيات النمو الخاصة بالأكاديمية الهندية لطب الأطفال ومراجع النمو الخاصة بمنظمة الصحة العالمية. وتم تحليل الحالة التغذوية وفقاً لمعايـير منظمة الصحة العالمية لنمو الأطفال، وذلك باستخدام برنامج Anthro الإحصائي الخاص بمنظمة الصحة العالمية (النسخة بيتا، 17 شباط/فبراير 2006). واستُخدم اختبار X² لتحديد مدى الأهمية الإحصائية عند مستوى اعتداد 0.05.
النتائج
كان معدل انتشار نقص الوزن (حرز Z أقل من -2) في الأشهر الستة الأولى من العمر أعلى من معدلات النمو الخاصة بالأكاديمية الهندية لطب الأطفال حوالي 1.6 مرة، وذلك عند حسابها وفقاً لمعايـير منظمة الصحة العالمية. وبالنسبة لجميع الأعمار مجتمعة، كان معدل الانتشار التقديري لنقص الوزن أعلى بنسبة 1.4 مرة عند استخدام معايـير الأكاديمية الهندية لطب الأطفال بدلاً من معايـير منظمة الصحة العالمية. وبالمثل، كان معدل انتشار نقص الوزن لدى الجنسين أعلى بنسبة 14.5% عند تطبيق معايـير الأكاديمية الطبية بدلاً من معايـير النمو الخاصة بمنظمة الصحة العالمية (عند نسبة احتمال P < 0.001). وبالمقارنة مع ذلك، كان سوء التغذية الوخيم التقديري للجنسين أعلى بنسبة 3.8 مرة عند استخدام معايـير منظمة الصحة العالمية بدلاً من معايـير الأكاديمية الهندية (عند نسبة احتمال P < 0.001).
الاستنتاج
من شأن معايـير النمو الخاصة بمنظمة الصحة العالمية أن تظهر معدلات انتشار أقل لنقص الوزن العام بين الأطفال، وأن تـتـتبّع النمو بشكل أفضل من معايـير الأكاديمية الهندية، ولاسيَّما في الأشهر الستة الأولى من العمر ولدى الأطفال المصابين بسوء التغذية الوخيم.
Introduction
Eighty percent of the world’s undernourished children live in 20 countries, with India being home to nearly 60 million children who are underweight.1 The National Family Health Survey (NFHS) in India reported the prevalence of underweight among children younger than 3 years in 2005–2006 to be nearly 46%, a figure representing only a marginal decline from the rates recorded in 1992–1993 (51%) and 1998–1999 (47%).2–5
Weight for age is the most widely used index for assessment of undernutrition in clinical practice and the only one used by the Integrated Child Development Services (ICDS) programme in India. The ICDS programme uses its vast network of primary childcare centres and workers – known as anganwadi workers – to monitor children’s growth by weighing at monthly intervals.6 Weight is then plotted for each child on Indian Academy of Paediatrics (IAP) growth charts, which are based on Harvard growth standards.7
In April 2006, WHO released new references for assessing growth and development in children from birth to 5 years. These references, known as the WHO Child Growth Standards, replaced the National Center for Health Statistics (NCHS)/WHO international growth reference (hereafter referred to as NCHS standards), which had certain limitations. In February 2007, the Ministry of Women and Child Development (nodal ministry for the ICDS programme) and the Ministry of Health and Family Welfare in India agreed to a changeover from the IAP growth curves in use at the time to WHO child growth curves. It is, therefore, important to assess whether using the latter will lead to changes in the estimated prevalence of underweight and, if so, how much of a change.8
In this study, we aim to compare the prevalence of underweight as calculated using IAP standards with the WHO Child Growth Standards and discuss the implications for child health programmes in India.
Methods
India has 28 states and nine union territories. Chandigarh is one union territory where health indicators are better than the Indian average.9 The population of Chandigarh was 900 635 at the time of the 2001 census, with projections from the National Commission on Population suggesting 1.16 million inhabitants by 2007.10 Children in the 0–6-year age group make up about 12.8% of the total population.
The ICDS programme’s central objective is to reduce child mortality and to achieve optimal physical, mental and psychosocial development for India’s children. The programme takes a multisectoral approach to child well-being, as it incorporates health, education and nutrition interventions through a network of anganwadi centres at the community level. At these centres, primary childcare workers and their helpers provide eight key services to pregnant women, children aged 0–6 years and lactating mothers.
Supplementary feeding, immunization, health check-ups and referrals, as well as health and nutrition education are offered to women. For children, micronutrient supplementation, growth monitoring, immunization, health check-ups with timely referrals and informal preschool education are provided.6 In Chandigarh these services are offered through a comprehensive network of three ICDS projects covering 329 primary childcare centres that have been running since 1979.
Study design and sampling
Multistage stratified random sampling was used to select anganwadi centres. We included 15% of all centres from each ICDS project area, with a probability of being selected proportional to the number of centres in three area types – urban, rural and urban slum – that we categorized using the data from the Department of Social Welfare, Chandigarh. Thus, a total of 45 anganwadi centres were selected: eight urban, 16 rural and 21 in urban slums. A cross-sectional household survey was conducted by the six field investigators (who all had graduate-level qualifications and health-related field experience) in the entire catchment area of each primary childcare centre. We calculated to record all beneficiaries, both registered and unregistered. We trained the field investigators in data collection and in the weighing of children before pilot testing.
We calculated that a sample size of 769 children younger than 6 years was needed to ascertain underweight prevalence, assuming a 5% prevalence of severe underweight (with worst acceptable result of 3.5%) and a 0.05 significance level. To recruit the required number of children, we randomly chose 10% of registered beneficiaries from the attendance register of the selected anganwadi centres and 10% of unregistered beneficiaries identified in the survey area. Unregistered children were included because the research was part of an overall evaluation of the ICDS programme and was thus intended to provide a complete picture of undernutrition prevalence in the state.
Children are categorized in the attendance register by sex and age group: 0–6 months, 6 months to 3 years and 3–6 years. The age groups make it possible to recognize the needs and services specific to each stratum. For example, the mothers of exclusively breastfed (0–6 months) children are provided with supplementary nutrition. Children aged 6 months to 3 years are given supplementary nutrition directly, and those in the 3–6-year age group receive informal preschool education as well as supplementary nutrition. Furthermore, children aged 6 months to 3 years are known to be at higher risk of developing underweight as a result of certain inappropriate cultural weaning practices (such as delayed weaning and the restriction of certain foods) and of higher rates of infection than breastfed children. Registered beneficiaries were randomly selected from attendance registers with a selection probability proportional to the number of children in each sex category and age group. Overall, 806 children were recruited for the study; 441 of them were registered in the ICDS programme and 365 were not.
All children selected were weighed with the help of a Salter weighing machine (Salter England Model No. 235 6S, United Nations Children’s Fund), which has a range of 25 kg with an accuracy to 100 g. Standard precautions were taken while weighing the children,11 who were categorized according to different grades of malnutrition using the IAP classification and the WHO Child Growth Standards of weight for age: underweight was defined as a Z score less than –2, and severe underweight as a Z score less than –3.
Data analysis
The data collected during the survey were converted to electronic format with the use of the Enter suite from Epi Info version 3.2 (Centers for Disease Control and Prevention, Atlanta, GA, United States of America). We graded malnutrition according to IAP classification using growth charts from the ICDS programme. Frequency counts and simple proportions were computed. Anthropometric data were also entered in WHO Anthro 2005 software (beta version, 17 February 2006), and weight-for-age Z scores were computed for boys and girls separately by age groups.12,13 Data from children under 5 years of age were analysed separately for underweight by IAP cut-off levels, and a comparison with the prevalence derived by using WHO Z scores was carried out. Children having grade III and IV malnutrition according to IAP standards were classified as severely underweight.
Quality control
To safeguard the quality of weight measurements and data collection by field investigators, 10% of all weight measurements and data forms were repeated by a field supervisor on a random basis, and two sets of recordings were matched for interobserver agreement. In the case of a discrepancy in recorded weight, another measurement was made by both the field investigator and the supervisor, and the mean of the two measurements was used if a discrepancy persisted. Written informed consent was obtained from the mothers of all study participants.
Results
Between 15 April 2007 and 31 July 2007, data were collected from children registered at eight urban (17.8%), 16 rural (35.5%) and 21 urban slum (46.7%) anganwadi centres in Chandigarh. Overall, 806 children aged under 6 years were recruited, and 737 (91.4%) of them were younger than 5 years.
According to the IAP classification, around half the children (50.2%) under 5 years were underweight. When the WHO Child Growth Standards were applied, the prevalence of underweight was seen to rise from birth up to age 36 months and to decline thereafter before rising again from 48–60 months. This age-related trend in the prevalence of underweight was statistically significant (P = 0.02) (Table 1).
Table 1. Nutritional status in children 0–5 years of age in Chandigarh, India, according to WHO Child Growth Standards and IAP standards.
| Age in months | Underweighta |
Severe underweightb |
|||||
|---|---|---|---|---|---|---|---|
| WHO | IAP | Difference | WHO | IAP | Difference | ||
| % (95% CI) | % | (WHO – IAP) | % (95% CI) | % | (WHO – IAP) | ||
| 0–5 | 22.0 (13.6–29.2) | 14.1 | 7.9 | 7.9 (1.7–14) | 2.4 | 5.5 | |
| 6–11 | 31.4 (19.8–43) | 38.7 | –7.3 | 10.0 (2.3–17.7) | 1.3 | 8.7 | |
| 12–23 | 34.3 (26.1–42.4) | 56 | –21.7* | 13.3 (7.4–19.2) | 7.8 | 5.5 | |
| 24–35 | 43.6 (35.3–51.9) | 49.6 | –6 | 15.4 (9.3–21.6) | 2.8 | 12.6* | |
| 36–47 | 37.3 (28.8–45.9) | 49.6 | –12.3** | 10.4 (4.3–16) | 1.4 | 9* | |
| 48–60 | 40.3 (32.2–48.3) | 59.2 | –18.9* | 15.6 (9.5–21.6) | 2.6 | 13* | |
| Overall | 35.7 (32.2–39.2) | 50.2 | –14.5* | 12.7 (10.2–15.2) | 3.3 | 9.4* | |
*P < 0.001, **P < 0.05. CI, confidence interval; IAP, Indian Academy of Paediatrics. a Z score < –2. b Z score < –3.
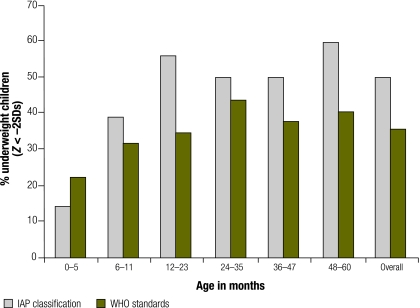
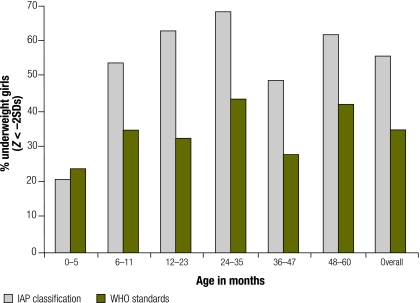
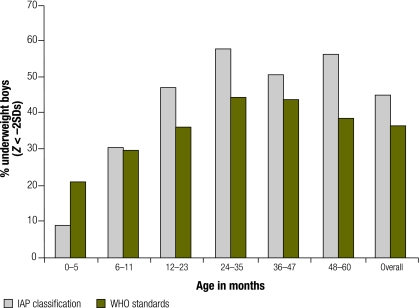
A comparison of overall prevalence of underweight across different age groups (using new WHO standards and IAP standards) revealed consistently higher estimates in all age groups by the IAP standard, except in the first half of infancy. The prevalence of underweight in the first 6 months of life was nearly 1.6 times higher when calculated with WHO Child Growth Standards compared with IAP growth curves (Table 1, Fig. 1 and Fig. 2). For children of all ages combined, the prevalence of underweight was 1.4 times higher when IAP standards rather than the new WHO standards were used, with the absolute difference being 14.5% (P < 0.001). IAP standards also produced lower estimates of malnutrition prevalence in girls under 6 months (P = 0.05), as shown in Fig. 3 and Fig. 4.
Fig. 1.
Underweight in children under 5 years of age in Chandigarh, India, using WHO Child Growth Standards versus IAP standards
IAP, Indian Academy of Paediatrics; SD, standard deviation.
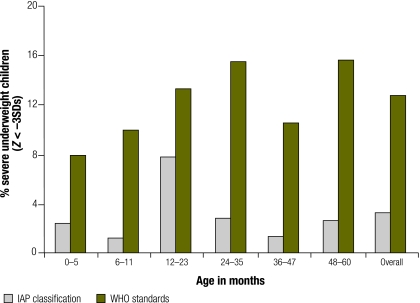
Fig. 2.
Severe underweight in children under 5 years of age in Chandigarh, India, using WHO Child Growth Standards versus IAP standards
IAP, Indian Academy of Paediatrics; SD, standard deviation.
Fig. 3.
Underweight in girls under 5 years of age in Chandigarh, India, using WHO Child Growth Standards versus IAP standards
IAP, Indian Academy of Paediatrics; SD, standard deviation.
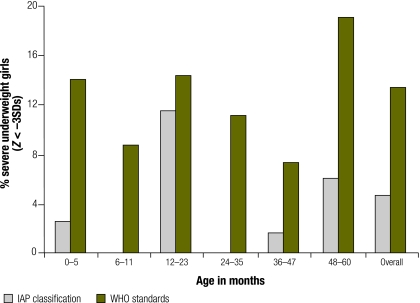
Fig. 4.
Severe underweight in girls under 5 years of age in Chandigarh, India, using WHO Child Growth Standards versus IAP standards
IAP, Indian Academy of Paediatrics; SD, standard deviation.
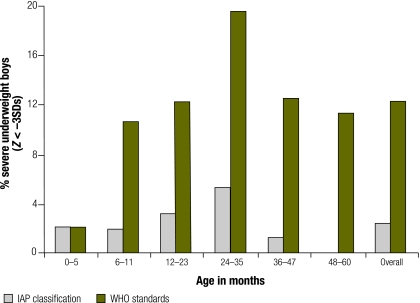
By contrast, overall estimates for severe malnutrition were 3.8 times higher using the new WHO standards rather than IAP standards (P < 0.001). This pattern was repeated within each age stratum and for both sexes (Table 1; Fig. 1, Fig. 2, Fig. 3, Fig 4, Fig. 5 and Fig. 6).
Fig. 5.
Underweight in boys under 5 years of age in Chandigarh, India, using WHO Child Growth Standards versus IAP standards
IAP, Indian Academy of Paediatrics; SD, standard deviation.
Fig. 6.
Severe underweight in boys under 5 years of age in Chandigarh, India, using WHO Child Growth Standards versus IAP standards
IAP, Indian Academy of Paediatrics; SD, standard deviation.
Discussion
The ICDS programme in India uses IAP standards for monitoring the growth of children aged under 6 years. All major national surveys carried out in India by the National Nutrition Monitoring Bureau,14 the National Family Health Survey1,2 and the District Level Household Survey have used IAP standards to estimate the prevalence of undernutrition. Furthermore, in clinical settings weight for age is a widely used indicator, and most clinicians use IAP standards.
However, we observed substantial discrepancies in underweight prevalence estimates when using IAP versus WHO Child Growth Standards. This could be explained by the fact that the new WHO standards are based on data from predominantly breastfed infants of a heterogeneous sample of children from developing and developed countries, whereas IAP standards are based on Harvard unisex tables of height and weight for age derived from predominantly formula-fed infants of North European descent. Furthermore, the data used for the new WHO standards were collected with a much greater frequency of weight recording in the first year of life than were data for the Harvard standards, allowing the dynamic growth in the first 12 months to be captured15,16 Use of new WHO standards resulted in a higher prevalence of underweight in the first half of infancy, which correlates with the 26% rate of low-birth-weight infants in our study.
A review of data from the District Level Household Survey in India shows that the reported 10% rate of undernutrition in the 0–3-month age group as assessed by IAP norms is unrealistically low considering the 30% prevalence of low birth weight in the country. Thus, the new WHO growth standards are more accurate than IAP standards for the period of infancy. Furthermore, IAP standards led to an overestimated prevalence of undernutrition among girls in particular (by 21.2% compared with WHO standards), an effect that can be explained by the use of unisex Harvard standards as compared with sex-specific WHO growth curves. Thus, the new WHO standards show a smaller gender bias in underweight prevalence than the IAP growth curves.
The IAP normal (≥ 80% of the Harvard median) is well below the median by the new WHO standards in the first 6 months of life, but it is above the median by such standards by 12 months of age and remains higher thereafter.17 Another study comparing NCHS and WHO growth standards reported that healthy breastfed infants followed the WHO standards’ weight-for-age mean Z-score, while appearing to falter on the NCHS standards from age 2 months onwards.18 Underweight rates increased during the first 6 months and thereafter decreased when based on the new WHO standards.
The new WHO standards have the advantage of being based on the growth of a heterogeneous sample of breastfed infants from six countries, including India. Furthermore, they were drawn up with frequent fortnightly growth monitoring to capture the dynamics of child growth in early infancy and with robust statistical methods that did not exist when IAP standards were developed.15
The Ministry of Women and Child Development (responsible for the ICDS programme) and the Ministry of Health and Family Welfare in India have endorsed the WHO Child Growth Standards and have drawn timelines for the changeover from the currently used IAP growth curves to the new WHO child growth curves.19 However, this change should be preceded by appropriate training of staff of all levels from the two departments, perhaps in joint training sessions. The training of ICDS programme staff presents another opportunity to bolster services and provide greater impetus to the key activity of growth monitoring. Furthermore, the logistics surrounding the increased demand for supplementary nutrition in view of the greater number of severely underweight children need to be adequately addressed. Focusing on these issues will also provide an opportunity for severely malnourished children to receive more attention.
The establishment of growth curves modelled on the physical progress of breastfed children brings the tools used to assess growth into line with national feeding guidelines that recommend breastfeeding as the optimum source of nutrition during infancy.20–22
WHO growth standards may project a lower overall prevalence of underweight in children in India, as we have found to be the case in Chandigarh. However, we believe that growth tracking with the new WHO standards is far superior to the current practice of using IAP standards, especially in the first 6 months of life, in girls and in severely malnourished children. Data, from previous demographic surveys that have been computed using IAP standards, need to be revisited using the new WHO standards for realistic tracking of the nutritional goals set by the Government of India.
We recommend that professional bodies such as the IAP, the Indian Association of Preventive and Social Medicine, the Indian Public Health Association and the Indian Medical Association endorse the use of the new WHO Child Growth Standards for the monitoring of the growth and development of children in clinical and public health practice in India. ■
Footnotes
Funding: The study was funded by the Women and Child Development Corporation, Chandigarh Administration. The funding agency had no role in the design of the study, data collection or report writing. It had no access to study data during or after the course of the research.
Competing interests: None declared.
References
- 1.Bryce J, Coitinho D, Darnton-Hill I. Pinsturp-Anderson P for the Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: effective action at national level. Lancet. 2008;371:510–26. doi: 10.1016/S0140-6736(07)61694-8. [DOI] [PubMed] [Google Scholar]
- 2.International Institute of Population Sciences. National Family Health Survey –1 Mumbai: IIPS, ORC Macro; 1993. [Google Scholar]
- 3.International Institute of Population Sciences. National Family Health Survey –2 Mumbai: IIPS, ORC Macro; 1998. [Google Scholar]
- 4.National Family Health Survey –3 factsheet. Available from: http://health.nic.in/factsheets%20pdf/IN.pdf
- 5.Gragnolati M, Bredenkamp C, Gupta MD, Lee YK, Shekhar M. ICDS and persisting undernutrition. Econ Polit Wkly. 2006;41:1193–201. [Google Scholar]
- 6.Ghosh S. Integrated Child Development services programme - need for reappraisal. Indian Pediatr. 1997;34:911–8. [PubMed] [Google Scholar]
- 7.Nutrition Sub-Committee of the Indian Academy of Paediatrics Report. Indian Pediatr. 1972;9:360. [Google Scholar]
- 8.Garza C. de Onis M for the Multicentre Growth Reference Group. Rationale for developing a new international growth reference. Food Nutr Bull. 2004;25(suppl):S5–14. doi: 10.1177/15648265040251S102. [DOI] [PubMed] [Google Scholar]
- 9.Registrar General of India. Sample Registration System Bulletin. Available from: http://www.censusindia.gov.in/Vital_Statistics/SRS_Bulletins/SRS_Bulletins_links/SRS_Bulletin-October-2006.pdf [accessed on 19 December 2008].
- 10.Planning Commission Government of India. Population projections 2001-2025 New Delhi: Government of India; 2006. [Google Scholar]
- 11.Jelliffe DB. The assessment of nutritional status of a community Geneva: World Health Organization; 1996 (Monograph Series No. 53). [PubMed] [Google Scholar]
- 12.WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development Geneva: World Health Organization; 2006. Available from: http://www.who.int/childgrowth/standards/Technical_report.pdf [accessed on 19 December 2008].
- 13.Physical status: the use and interpretation of anthropometry Geneva: World Health Organization; 1995 (WHO Technical Report Series No. 854). [PubMed]
- 14.National Nutrition Monitoring Bureau. NNMB reports1979-2002 Hyderabad: National Institute of Nutrition; 2003. [Google Scholar]
- 15.Garza C, de Onis M, Victoria CG, Onyango AW, Frongillo EO, Martines J. The Multicentre Growth Reference Study: planning, study design and methodology. Food Nutr Bull. 2004;25(suppl):S15–26. doi: 10.1177/15648265040251S103. [DOI] [PubMed] [Google Scholar]
- 16.WHO Multicentre Growth Reference Study Group WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr Suppl. 2006;450:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x. [DOI] [PubMed] [Google Scholar]
- 17.Ramachandran P. Adoption of WHO Child Growth Standards (2006) – issues and implications NFI Bulletin 2007;28:1-6. Available from: http://nutritionfoundationofindia.res.in/pdfs/Apr2007.pdf [accessed on 19 December 2008].
- 18.De Onis M, Onyango AW, Borghi E, Garza C, Yang H. Comparison of WHO Child Growth Standards and National Centre for Health Statistics/ WHO international growth standards: implication for child health programmes. Public Health Nutr. 2006;9:942–7. doi: 10.1017/PHN20062005. [DOI] [PubMed] [Google Scholar]
- 19.Indian Ministry of Health and Family Welfare. Recommendations. National workshop on adoption of new WHO Child Growth Standards, New Delhi, India, 8-9February2007
- 20.Gartner LM, Morton J, Lawrence RA, Naylor AJ, O’Hare D, Schanler RJ, et al. Breastfeeding and the use of human milk. Pediatrics. 2005;115:496–506. doi: 10.1542/peds.2004-2491. [DOI] [PubMed] [Google Scholar]
- 21.Fifty-fourth World Health Assembly. Resolution WHO 54.2, Infant and young child nutrition Geneva: World Health Organization; 2001. [Google Scholar]
- 22.The optimal duration of exclusive breastfeeding: report of an expert consultation Geneva: World Health Organization; 2002. [Google Scholar]